Abstract
Purpose
We determined whether baseline urodynamic study variables predict failure after midurethral sling surgery.
Materials and Methods
Pre-operative urodynamic study variables and post operative continence status were analyzed from women participating in a randomized trial comparing retropubic to transobturator midurethral sling. Objective failure was defined by positive standardized stress test, or 15 ml or greater on 24-hour pad test, or re-treatment for stress urinary incontinence (SUI). Subjective failure criteria were self-reported stress symptoms, or leakage on 3-day diary, or retreatment for stress urinary incontinence. Logistic regression assessed associations between covariates and failure controlling for treatment group and clinical variables. Receiver operator curves were constructed for relationships between objective failure and measures of urethral function.
Results
Objective continence outcomes were available at 12 months from 565 of 597 (95%) women. Treatment failed in 260 (245 subjective criteria, 124 by objective criteria). No urodynamic variable was significantly associated with subjective failure on multivariate analysis. Valsalva leak point pressure (VLPP) and maximum urethral closure pressure (MUCP) were the only urodynamic variables consistently associated with objective failure on multivariate analysis. No specific cut-point was determined for predicting failure for VLPP or MUCP by ROC; the lowest quartile (VLPP <86 cm H2O; MUCP <45 cm H2O) conferred an almost two fold increased odds of objective failure regardless of sling route [OR 2.23 (1.20– 4.14) for VLPP and OR 1.88 (1.04–3.41)] for MUCP.
Conclusions
Women with either a VLPP or MUCP in the lowest quartile are nearly 2-fold more likely to experience SUI one year after transobturator or retropubic MUS.
Keywords: urinary stress incontinence, urodynamics, maximum urethral closure pressure, leak point pressure, surgery
Introduction
Urodynamic testing is often performed before surgery for stress urinary incontinence to try to predict which women are at greater risk of failure, or to recommend one type of procedure over another. For many years, in women with a maximum urethral closure pressure (MUCP) < 20 cm H2O, a sling procedure rather than a Burch colposuspension, was recommended.[1] It is not known whether this measure or other urodynamic measures predict results of midurethral sling (MUS) surgeries. Smaller studies to date have drawn mixed conclusions about whether the retropubic or transobturator approach has a greater failure risk in women with poor urethral function.
In this planned secondary analysis of the Trial Of MidUrethral Sling (TOMUS) trial we determined whether certain preoperative urodynamic findings predict objective or subjective failure after MUS surgery.
Materials and Methods
Methods [2] and primary results [3] for the TOMUS randomized equivalence trial that compared retropubic (RMUS) to transobturator (TMUS) midurethral slings have been previously described. Briefly, eligible women had pure or predominant stress incontinence symptoms for at least three months, a positive urinary stress test at a bladder volume of 300 mL or less, and were planning surgery.
Institutional Review Board approval was obtained at all participating sites and an independent data and safety monitoring board monitored the study.
Urodynamics
All patients underwent preoperative urodynamic testing according to ICS Guidelines[4] and according to a standardized research protocol. The details and specifics of the non-instrumented uroflowmetry (NIF), filling cystometry (CMG), and a pressure flow study (PFS) have been previously published. [5]
Urethral profilometry
The difference between the urodynamic protocol used in this TOMUS trial and our previously published urodynamic protocol [5] is that urethral profilometry was added and therefore a triple lumen (7 French) catheter instead of a dual lumen (7 French) catheter was utilized for testing. After NIF, but before CMG, Urethral pressure profiles (UPP) were performed in the supine position with perfusion[6] using a flow restrictor at 0.5 ml/min. Three UPP withdrawals at 1 mm/sec were performed measuring functional urethral length (FUL) and maximum urethral closure pressure (MUCP); the subject had to have at least 2 valid profilometries (FUL ≤ 50 mm) for MUCP/ FUL data inclusion. The physicians who performed surgery in the trial were blinded to all the urodynamic measurements and results. The term “delta” is used when the urodynamic measure is the difference from baseline.
Primary outcomes of objective and subjective success status were assessed 12 months post randomization. [3] An objective failure was defined as a positive stress test, or a positive pad test, or retreatment for stress incontinence. A subjective failure was defined as reported stress-type UI symptoms ‘sometimes’ or more often on the Medical Epidemiological and Social Aspects of Aging (MESA) [7] questionnaire, or leakage on a 3-day voiding diary, or retreatment for stress incontinence.
The Fourteen urodynamic measures investigated as continuous variables included: VLPP, MUCP, FUL, first desire, strong desire, MCC, vesical compliance, detrusor compliance, NIF Qmax, PFS Qmax, delta pves@Qmax, delta pabd@Qmax, delta pdet @Qmax and PVR after NIF. Three categorical urodynamic parameters investigated included were urodynamic stress incontinence (yes/no), detrusor overactivity (yes/no) and point at which patient leaked (leaked with Valsalva, leaked with cough at MCC only, or did not leak). Receiver operator curves (ROC) were constructed for the relationships between objective failure and VLPP as well as MUCP. Outcomes for women with the lowest quartiles versus higher values for VLPP and MUCP were compared.
Logistic regression assessed the association between each proposed covariate and failure, controlling for treatment group. Models were fit separately for objective and subjective failure. Preliminary multivariable models including treatment group (regardless of significance) were constructed including any covariates having p-values <0.05. To assess whether urodynamic variables were independently associated with outcome after controlling for clinical variables, in the final model we controlled for significant clinical variables that would be readily available to the clinician at the time of treatment planning (age and concomitant surgery). Because VLPP and MUCP correlate with each other and the aim was to obtain estimates of VLPP unadjusted by MUCP (and vice versa), separate multivariable analysis was performed for each of these variables. To assess whether the relationships found between the urodynamic measures and failure differed according to treatment group (retropubic or transobturator), interactions of treatment by covariate were considered relevant. A 5% two-sided significance level was used.
Results
A total of five hundred ninety seven women were randomly assigned to receive either a retropubic sling (298 women) or a transobturator sling (299 women). Baseline clinical characteristics and the primary outcomes have been previously reported. [3] The primary outcome measures were assessed in 95% (565/597) of randomized subjects at 12 months with 46% (260) having any treatment failure (Table 1). More women had treatment failure by subjective vs objective criteria (245 vs. 124) and only 15 women had failure by objective measures only. Table 1 summarizes the failure results and urodynamic measures in this population.
Table 1.
Treatment, Failure, and Preoperative Urodynamic Characteristics of Women Enrolled in the TOMUS trial
| Total No. |
||
|---|---|---|
| Treatment | 597 | |
| TMUS | 299 (50.1) | |
| RMUS | 298 (49.9) | |
| Objective failure | 559 | |
| Yes | 124 (22.2) | |
| No | 435 (77.8) | |
| Subjective failure | 564 | |
| Yes | 245 (43.4) | |
| No | 319 (56.6) | |
| Any failure (objective and/or subjective) | 565 | |
| Yes | 260 (46.0) | |
| No | 305 (54.0) | |
| Urodynamic stress incontinence (USI) | 589 | |
| Yes | 505 (85.7) | |
| No | 84 (14.3) | |
| Detrusor overactivity (DO) | 589 | |
| Yes | 70 (11.9) | |
| No | 519 (88. 1) | |
| At what point did the patient leak | 589 | |
| Leakage w/ Valsalva | 418 (71.0) | |
| Leakage w/ cough at MCC only | 87 (14.8) | |
| No leakage | 84 (14.3) | |
| VLPP (cm H2O) (atmospheric reference) | 119 (42) | 372 |
| MUCP (cm H2O) | 68 (33) | 539 |
| FUL (mm) | 32 (8) | 539 |
| First desire (cc) | 117 (80) | 586 |
| Strong desire (cc) | 227 (118) | 585 |
| MCC (cc) | 351(123) | 589 |
| NIF Qmax (cc/s) | 25 (12) | 550 |
| PFS Qmax (cc/s) | 22 (11) | 556 |
| pves @Qmax (cm H2O) | 56 (26) | 401 |
| pabd@Qmax (cm H2O) | 37 (27) | 401 |
| Delta pdet @ Qmax (cm H2O) | 19 (13) | 401 |
| PVR at NIF (cc) | 24 (42) | 502 |
| Vesical compliance (cc/cm H2O) | 68 (127) | 513 |
| Detrusor compliance (cc/cm H2O) | 53 (144) | 496 |
Frequency (%) for categorical variables and Mean (SD) for continuous variables
Urodynamic Measures and Objective and Subjective Success
When we performed logistic regression analysis assessing the association between each proposed urodynamic measure and subjective failure, controlling for treatment group, no significant association was found for thirteen continuous urodynamic measures (VLPP, MUCP, FUL, first desire, strong desire, MCC, vesical compliance, detrusor compliance, NIF Qmax, PFS Qmax, delta pves@Qmax, delta pabd@Qmax, and PVR after NIF) and for three categorical urodynamic measures (urodynamic stress incontinence (yes/no), detrusor overactivity (yes/no) and point at which patient leaked (leaked with Valsalva, leaked with cough at MCC only, or did not leak). Delta pdet@Qmax was the only variable significantly associated with subjective failure, but this did not remain significant on multivariate analysis after controlling for treatment group, concomitant surgery, age, VLPP, MUCP, and delta pabd @Qmax. There were no significantly increased odds of subjective failure with VLPP (OR 0.96, CI 0.91–1.01), or MUCP (OR 0.98, 0.93–1.03).
Therefore, all results presented subsequently in this study pertain to objective failure only. On the bivariate analysis for predicting objective failure of the 17 urodynamic variables evaluated the only measures that had p values < 0.05 were: USI, VLPP, MUCP, delta pabd@Qmax and delta pdet@Qmax.
Urodynamic Stress Incontinence (USI)
Of the 565 women with objective outcomes, the presence or absence of USI could be determined in 551 (98%). Of these women 14% (76/551) did not leak during urodynamic testing, 15% (84/549) leaked only with cough at MCC, and 71% (391/551) leaked with Valsalva efforts. In bivariate analysis the objective failure rate in women with USI (110/475, 23%) was nearly twice that of women without USI (9/76, 12%, OR 2.26, CI 1.09–4.67).
Detrusor Overactivity
Of evaluable women 12% (64/551) had detrusor overactivity (DO); of these, 27% (17/62) had objective failure compared to 21% (103/487) of women without DO (OR 1.42, 0.78–2.56). A similar non-significant group difference was found when evaluating subjective failure (49% vs. 42%, OR 1.34, CI 0.79–2.27) in the subjects with DO versus subjects without DO, respectively.
Urethral Function Measures
VLPP’s were obtained in 94% (348/372) of the subjects who leaked with Valsalva efforts, but only 63% (348/5519) of the overall group had VLPP measures, primarily because many subjects did not leak with Valsalva effort. In contrast, 94% of subjects with objective outcomes (504/539) had valid and plausible urethral profilometry measures. On bivariate analysis, for every 10 cm H2O increase in VLPP there was a 7% reduction in objective failure rate (OR 0.93, 0.87–0.99), and for every 10 cm H20 increase in MUCP there was a 12% decrease in objective failure rate (OR 0.88, 0.81–0.95).
Urethral function measures - dichotomous analysis
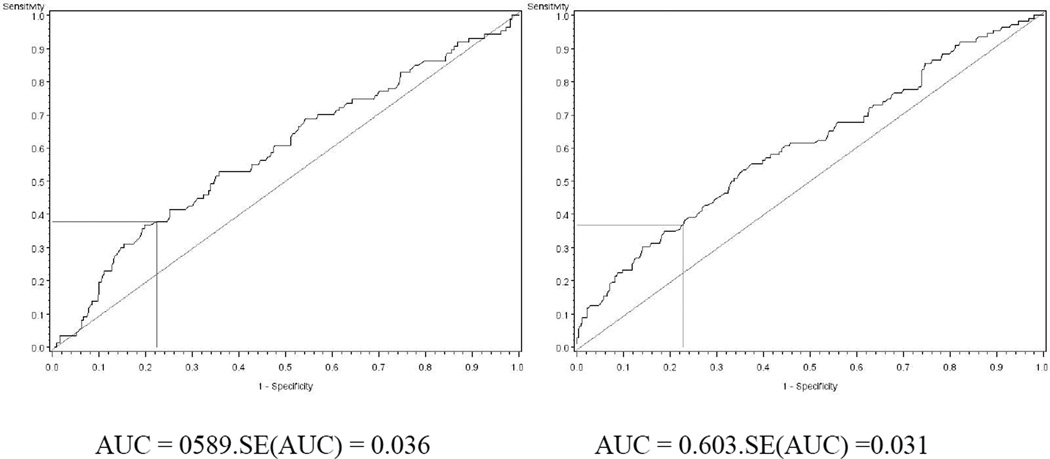
VLPP and MUCP values were normally distributed in our population. ROC analyses were performed to determine if there were any obvious threshold values or cut-points for VLPP’s and MUCP (Figure 1). There were no obvious cut-points with both high sensitivity and high specificity for failure for either VLPP or MUCP.
Figure 1.
Receiver Operator Curves (ROC) for objective failure for VLPP and MUCP values. Horizontal and vertical lines in the lower left of each part depict the sensitivity and 1-specificity when using lower quartile cut-points for the urethral function values (86 cm H2O for VLPP, 45 cm H2O for MUCP).
Since common usage of urethral function measures is to compare the very worst values (lowest) group with the upper values group and without an obvious cut-point by ROC analysis, an analysis was performed comparing the lowest quartile of these values with the upper three quartiles. For VLPP, the lowest quartile (that is, the value below which 25% of the population fell) corresponded to a pves < 86 cm H20 measured with atmospheric pressure as the reference and zeroed to the symphysis with the patient standing. The mean pves at start of fill for these standing subjects was 36 cm H20 and therefore this lower quartile cut-off for VLPP is an approximate delta VLPP or of 50 cm H20. For MUCP, the lowest quartile corresponded to a value of 45 cm H20, which reflects the higher values obtained with water perfusion technology.[8] Higher objective failure rates were associated with lower quartile VLPP or MUCP values compared to upper three quartile values for both surgical procedures (Figure 2). An interaction analysis was performed to determine whether subjects with lower quartile VLPP’s or lower quartile MUCP’s had significantly better results in one treatment group more than another. From a logistic regression model considering VLPP or MUCP, treatment group, and their interaction, the p-value for the interaction between VLPP and treatment group is 0.64, and the p-value for the interaction between MUCP and treatment group is 0.19. These non-significant p-values for the interaction terms suggest that the higher objective failure rates associated with lower quartile MUCP or VLPP are applicable to both the retropubic and transobturator MUS approaches.
Figure 2.
Objective failure rates of retropubic and transobturator mid urethral sling procedures. In each part failure rates are stratified by urethral function measures in upper 3 quartiles (light gray) or lower quartile (dark gray). Error bars represent ± 1 standard error. Low VLPP is associated with higher objective failure rates (p=0.003), which holds for both treatment groups (interaction between treatment and VLPP not significant, p= 0.64). Low MUCP is associated with higher objective failure rates (p=0.003), whilch holds for both treatments groups (interaction between treatment and MUCP not significant, p=0.19).
Multivariate analysis
Table 2 shows the results of the multivariate analysis which includes controlling for age and concomitant surgery which were the only two significant clinical predictors of objective failure (data not shown) that would be commonly available to a clinician evaluating a woman for stress incontinent surgery. For these models VLPP and MUCP were treated independently.
Table 2.
Odds ratio of objective failure in the VLPP and MUCP multivariable models
| Variable | VLPP | MUCP | ||
|---|---|---|---|---|
| OR (95% CI) | p- value |
OR (95% CI) | p- value |
|
|
VLPP VLPP≤25th percentile vs. VLPP >25th percentile |
2.23 (1.20–4.14) | 0.011 | – | – |
|
MUCP MUCP≤25th percentile vs. MUCP>25th percentile |
– | – | 1.87 (1.02–3.41) | 0.04 |
| Delta pabd@Qmax | 1.09 (0.98–1.21) | 0.10 | 1.10 (0.99–1.22) | 0.08 |
| Delta pdet@Qmax | 0.82 (0.63–1.08) | 0.15 | 0.79 (0.61–1.02) | 0.07 |
|
USI Yes, did leak vs. No, did not leak |
– | – | 5.20 (1.16–23.44) | 0.03 |
| Treatment: TMUS vs. RMUS | 1.27 (0.71–2.28) | 0.43 | 1.19 (0.69–2.04) | 0.54 |
| Concomitant Surgery: No vs. Yes | 1.11 (0.55–2.23) | 0.78 | 1.48 (0.75–2.92) | 0.26 |
| Age(/10years) | 1.31 (1.01–1.71) | 0.04 | 1.37 (1.07–2.92) | 0.01 |
The VLPP model is unadjusted but MUCP and the MUCP model is unadjusted by VLPP. Both models control for delta PabdQmax, delta PdetQmax, USI, treatment group, and the clinical variables of concomitant surgery and age, except that the VLPP model does not adjust for USI since all subjects with VLPP’s by definition have USI.
VLPP, MUCP, USI and possibly delta pdet@Qmax (significant in one of two analyses) remain significant predictive variables in multivariate analysis. The odds ratio of objective faiture for women with USI compared to those without USI was 5.2 but the CI was large (1.16 – 23.44_. Having a lower quartile VLPP or MUCP conferred an almost two fold increase in odds of objective failure.
Discussion
We observed that women with more severe urethral dysfunction, defined as the lowest quartile VLPP or MUCP, are at a nearly 2-fold increased risk of objective failure one year after a retropubic or transobturator MUS. This increased risk of failure with lower VLPP or MUCP values was not significantly more for the transobturator procedure compared to the retropubic procedure.
Most prior studies which have evaluated the association between urodynamic factors and SUI surgery failure were retrospective, included an inadequate sample size, failed to control for confounding factors, or lacked standardized evaluation and validated outcome measures. In an RCT of the Burch colposuspension vs. the fascial pubovaginal sling, pre-operative VLPP, presence or absence of DO or USI failed to predict stress incontinence failure, although there was a trend toward a lower success rate in women without USI.[9].
It has been suggested that patients with poor urethral function have better success rates with retropubic than transobturator MUS because the vector forces provided by a retropubic sling may be more compressive than that provided by a transobturator sling. Thus knowledge of poor urethral function pre-operatively may be important when selecting the surgical technique. Most studies of retropubic slings have shown that measures of VLPP and MUCP were not associated with surgical success rates. [10–13] A recent metanalysis confirmed that urethral function did not predict outcome of MUS, regardless of approach. [14] In a randomized surgical trial of transobturator and retropubic MUS, Barber et al. reported that VLPP, considered either as a continuous or dichotomous variable (<60 cm/H2O) was not associated with failure of either procedure after one year. [15] Similarly, Costantini et al noted no increased relative risk of surgical failure when comparing transobturator or retropubic MUS based on VLPP or MUCP findings. [16] However, some studies have shown that low MUCP and/or VLPP were associated with increased failure with the transobturator route. [11][17] [18] [19] [20] [21]Schierlitz et al. randomized women with poor urethral function (MUCP ≤ 20 cm H20 and /or delta VLPP of ≤ 60 cm/H20) to retropubic or transobturator procedures. [22]Postoperative USI at 6 months was less in the retropubic (21%) than the transobturator groups (45%) (p= 0.004).
On unadjusted analysis that for every 10 cm H2O increase in VLPP there was a 7% reduction in the objective failure rate, and for every 10 cm H2O increase in MUCP there was a 12% reduction in the objective failure rate. Previous reports have evaluated dichotomous variables often using pre-established, somewhat arbitrary cut-points such as VLPP of < 60 cm H20 or MUCP of < 20 cm H2[11, 15, 18–21] [22] [23] [24] Using (ROC) we found no obvious cut-point that demonstrated both high sensitivity and specificity for objective surgical failure for either VLPP or MUCP. Therefore, we chose to compare the lowest quartile of VLPP and MUCP with the upper three quartiles. Having a lower quartile VLPP or MUCP confers an almost two fold increase in odds of objective failure. The interaction analysis shows that the higher failure rates associated with lower quartile MUCP or VLPP are applicable to both the retropubic and transobturator procedures.
Although inspection of the MUCP data in figure 2 may suggest a trend that subjects with lower quartile MUCP may have significantly lower failure rates with a retropubic than a transobturator procedure, the most appropriate statistical analysis to test this significance is an interaction analysis which quantifies whether there is a different relationship between MUCP and objective failure for the treatment groups. This analysis did not reach significance. (p=0.19). Thus our findings suggest that measures of MUCP or VLPP should not be used to select the route of MUS. We acknowledge that our study was not specifically designed to address surgical treatment outcomes in only subjects with low VLPP and/or low MUCP, and although we had 150 subjects with lower quartile VLPP and MUCP values, we may still be underpowered to detect a clinically meaningful interaction with treatment for these subjects.
Contrary to the trend noted in the SISTEr trial, subjects with USI in this trial had a higher failure rate than those without USI. Perhaps subjects who leak on stress test, but not during urodynamics, have better urethral function, and are less likely to leak on postoperative stress testing, which could explain why this finding was found for objective but not for subjective failure. However, given the discrepant results in two trials and the large CI of this result, we are reluctant to place much emphasis on this finding. The discrepant results may be related to the more strict definition of objective failure in TOMUS, slightly different populations, different sling placement, or the relatively small number of patients without USI in both these studies.
Similar to what we reported previously in the SISTEr trial [9], the presence of DO was not associated with an increased risk of objective or subjective failure in this study, despite the fact that increased urge symptoms and increased urge bother were associated with surgical failure in both trials. [25]This may reflect our SUI dominant patient population, the complexity of urinary urgency symptoms and its poor correlation with DO, or the limitations of the small number of patients with DO in both these studies.
The delta pPabd@Qmax (a measure of straining with voiding) was associated with increased odds of objective failure on univariate analysis but not in multivariable analysis. An increased delta pdet@Qmax (perhaps measuring increased urethral resistance to urine flow) was the only variable significantly associated with subjective and objective failure in univariate analysis and was still significant in the MUCP multivariable analysis but not in the VLPP multivariable analysis. The significance of these inconclusive findings is unclear.
A limitation of any study evaluating a large number of factors or dichotomous categorization of values with no clear cut points on ROC analysis is false positive findings. We chose to evaluate seventeen different urodynamic variables and possible associations with both subjective and objective failure a priori,; false positive results are possible. We acknowledge that choosing slightly different cut-off values could result in slightly different results, which are why we have refrained from repetitive cut point analysis. The strengths of this study include the multicenter design with a variety of urology and urogynecology surgeons, surgeons blinded to urodynamic results, the use of clearly defined validated outcome measures, a high rate of ascertainment of the primary outcome at 12 months, and the standardized urodynamic testing.
Conclusion
Women in the lowest quartile for either VLPP or MUCP are at an almost two fold increase in odds to experience objective failure for either retropubic or transobturator procedures one year after surgery. We did not find evidence that the retropubic or transobturator approaches had significantly different objective failure rates in women with the lowest quartile of VLPP or MUCP measures.
Acknowledgments
This work was performed in Urinary Incontinence Treatment Network which was funded by the NIH/NIDDK and the list of investigators and the grant numbers can be found in the acknowledgements.
References
- 1.Sand PK, et al. The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol. 1987;69(3 Pt 1):399–402. [PubMed] [Google Scholar]
- 2.UITN. The Trial Of Mid-Urethral Slings(TOMUS: Design and Methodology. The Journal of Applied Research. 8(1):1–13. [PMC free article] [PubMed] [Google Scholar]
- 3.Richter HE, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 362(22):2066–2076. doi: 10.1056/NEJMoa0912658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schafer W, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21(3):261–274. doi: 10.1002/nau.10066. [DOI] [PubMed] [Google Scholar]
- 5.Nager CW, et al. Reference urodynamic values for stress incontinent women. Neurourol Urodyn. 2007;26(3):333–340. doi: 10.1002/nau.20348. [DOI] [PubMed] [Google Scholar]
- 6.Griffiths D, et al. Standardization of terminology of lower urinary tract function: pressure-flow studies of voiding, urethral resistance, and urethral obstruction. International Continence Society Subcommittee on Standardization of Terminology of Pressure-Flow Studies. Neurourol Urodyn. 1997;16(1):1–18. doi: 10.1002/(sici)1520-6777(1997)16:1<1::aid-nau1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 7.Herzog AR, Diokno AC, Fultz NH. Urinary incontinence: medical and psychosocial aspects. Annu Rev Gerontol Geriatr. 1989;9:74–119. doi: 10.1007/978-3-662-40455-3_3. [DOI] [PubMed] [Google Scholar]
- 8.Wang AC, Chen MC. A comparison of urethral pressure profilometry using microtip and double-lumen perfusion catheters in women with genuine stress incontinence. Bjog. 2002;109(3):322–326. doi: 10.1111/j.1471-0528.2002.01001.x. [DOI] [PubMed] [Google Scholar]
- 9.Nager CW, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in selected women. J Urol. 2008;179(4):1470–1474. doi: 10.1016/j.juro.2007.11.077. [DOI] [PubMed] [Google Scholar]
- 10.Rezapour M, Falconer C, Ulmsten U. Tension-Free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)--a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S12–S14. doi: 10.1007/s001920170005. [DOI] [PubMed] [Google Scholar]
- 11.Meschia M, et al. Tension-free vaginal tape: analysis of risk factors for failures. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(4):419–422. doi: 10.1007/s00192-006-0161-3. [DOI] [PubMed] [Google Scholar]
- 12.Rardin CR, KN, Miklos J, Rosenblatt PL, Moore RD, Strohsnitter WC. Outcomes of tension-free vaginal tape in women with intrinsic sphincter deficiency with or without urethral hypermobility. J Pelvic Med Surg. 2005;11:321–327. [Google Scholar]
- 13.Clemons JL, LaSala CA. The tension-free vaginal tape in women with a non-hypermobile urethra and low maximum urethral closure pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(7):727–732. doi: 10.1007/s00192-006-0231-6. [DOI] [PubMed] [Google Scholar]
- 14.Latthe PM, Foon R, Toozs-Hobson P. Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. Bjog. 2007;114(5):522–531. doi: 10.1111/j.1471-0528.2007.01268.x. [DOI] [PubMed] [Google Scholar]
- 15.Barber MD, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008;199(6):666, e1–e7. doi: 10.1016/j.ajog.2008.07.050. [DOI] [PubMed] [Google Scholar]
- 16.Costantini E, et al. Preoperative MUCP and VLPP did not predict long-term (4-year) outcome after transobturator mid-urethral sling. Urol Int. 2009;83(4):392–398. doi: 10.1159/000251177. [DOI] [PubMed] [Google Scholar]
- 17.Miller JJ, et al. Is transobturator tape as effective as tension-free vaginal tape in patients with borderline maximum urethral closure pressure? Am J Obstet Gynecol. 2006;195(6):1799–1804. doi: 10.1016/j.ajog.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Hsiao SM, Chang TC, Lin HH. Risk factors affecting cure after mid-urethral tape procedure for female urodynamic stress incontinence: comparison of retropubic and transobturator routes. Urology. 2009;73(5):981–986. doi: 10.1016/j.urology.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Rechberger T, et al. The clinical effectiveness of retropubic (IVS-02) and transobturator (IVS-04) midurethral slings: randomized trial. Eur Urol. 2009;56(1):24–30. doi: 10.1016/j.eururo.2009.02.038. [DOI] [PubMed] [Google Scholar]
- 20.Jeon MJ, et al. Surgical therapeutic index of tension-free vaginal tape and transobturator tape for stress urinary incontinence. Gynecol Obstet Invest. 2008;65(1):41–46. doi: 10.1159/000107491. [DOI] [PubMed] [Google Scholar]
- 21.Gungorduk K, et al. Which type of mid-urethral sling procedure should be chosen for treatment of stress urinary incontinance with intrinsic sphincter deficiency? Tension-free vaginal tape or transobturator tape. Acta Obstet Gynecol Scand. 2009;88(8):920–926. doi: 10.1080/00016340903100354. [DOI] [PubMed] [Google Scholar]
- 22.Schierlitz L, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008;112(6):1253–1261. doi: 10.1097/AOG.0b013e31818db391. [DOI] [PubMed] [Google Scholar]
- 23.Porena M, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol. 2007;52(5):1481–1490. doi: 10.1016/j.eururo.2007.04.059. [DOI] [PubMed] [Google Scholar]
- 24.Houwert RM, et al. Predictive value of urodynamics on outcome after midurethral sling surgery for female stress urinary incontinence. Am J Obstet Gynecol. 2009;200(6):649, e1–e12. doi: 10.1016/j.ajog.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 25.Richter HE, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Urol. 2008;179(3):1024–1030. doi: 10.1016/j.juro.2007.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]