Abstract
AIM
To compare the regularity and accuracy of laser in situ keratomileusis (LASIK) flaps created by the Ziemer FEMTO LDV “Classic” (Ziemer “Classic”) and Ziemer FEMTO LDV Crystal Line femtosecond laser (Ziemer Crystal Line).
METHODS
Fourier-domain optical coherence tomography (RTVue OCT) was used to measure the morphology of 200 LASIK flaps of 100 consecutive patients created with the Ziemer Classic (100 flaps) or the Ziemer Crystal Line (100 flaps) at one week postoperatively. Flap thickness was evaluated at 36 specified measurement points on each flap. For all procedures with both lasers, the nominal flap thickness was 110µm.
RESULTS
The mean flap thickness of the Ziemer Crystal Line group (102.49±2.68µm) was thinner than that of the Ziemer Classic group (107.65±5.09µm) (P<0.01). Average thickness of all flaps was uniform within 4µm at all measurement points. The flaps in the Ziemer Crystal Line group were more regular than those in the Ziemer Classic group when measured from the center to the periphery. The maximum deviation from the nominal 110µm of 36 measurements was 8µm in the Ziemer Classic group, while in the Ziemer Crystal Line group it was 9µm. Within the 3 600 measurements on the 100 eyes, differences greater than 20µm were observed 0.14% in the Ziemer Classic group, and 0.04% in the Ziemer Crystal Line group.
CONCLUSION
The flaps created with the Ziemer FEMTO LDV Crystal Line femtosecond laser are more uniform and thinner than those created by the Ziemer FEMTO LDV Classic femtosecond laser.
Keywords: laser in situ keratomileusis, flap thickness, femtosecond laser, fourier-domain optical coherence tomography
INTRODUCTION
Laser in situ keratomileusis (LASIK) has become an efficient and commonly performed procedure in refractive surgery. Flap creation is the first critical and probably the most important step during LASIK, and precise corneal flap thickness is vital for accurately correcting refraction in eyes with high myopia or a thin cornea by LASIK[1]-[3]. A too thin flap may be associated with a higher frequency of potential complications such as a free, irregular, incomplete, buttonhole or lacerated flap. In order to maintain postoperative corneal strength, especially to avoid the occurrence of iatrogenic keratoconus and refractive regression, the residual stromal thickness must be more than 250µm [4]-[6]. Complications during flap creation can affect the rest of the procedure and cause permanent visual loss [7]. Therefore, it is important to produce a uniform flap with a narrow standard deviation from the attempted thickness.
Flap preparation is currently performed with either a femtosecond laser or a mechanical microkeratome. Previous studies comparing microkeratome and femtosecond laser flap creation report that the latter may yield better safety, reproducibility and predictability[8]-[10]. The Ziemer FEMTO LDV Crystal Line is the newest generation of fast, low-energy femtosecond laser and it offers additional advantages over its Classic companion. To our knowledge, no published report has compared the new generation Ziemer FEMTO LDV Crystal Line with the FEMTO LDV Classic femtosecond laser for corneal flap creation.
Flap thickness can be measured by Fourier-domain optical coherence tomography (OCT), which is also known as spectral-domain OCT. Recently, some studies found that Fourier-domain OCT (RTVue OCT, Optovue, Inc. Fremont, CA, USA) has better repeatability than time-domain OCT (Visante, Carl Zeiss Meditec, Inc., Dublin, CA, USA) for corneal thickness measurements[11]-[13].
In this study, we used Fourier-domain OCT to compare the flap morphologies created by Ziemer Classic and Ziemer Crystal Line femtosecond lasers (Ziemer Group, Switzerland), assessing the regularity, uniformity and accuracy of flap creation.
SUBJECTS AND METHODS
Subjects
Two hundred eyes of one hundred consecutive patients who were scheduled for bilateral LASIK treatment from August 2010 to September 2010 in the Tongren Ophthalmic Center of Capital Medical University (Beijing, China) were enrolled in this prospective study. Inclusion criteria were as follows: patients at least 18 years old, no contact lens wear for 2 weeks prior to the preoperative examination, stable refractive error for at least 2 years, and corrected distance visual acuity (CDVA) of 20/20 (1.0) or better. Patients with ocular pathologies such as corneal scars, corneal dystrophies, previous ocular surgery, keratoconus, glaucoma, diabetes, and systemic diseases known to affect eyes were excluded. Based on the random and voluntary principle, 100 eyes of 50 patients underwent LASIK with FEMTO LDV Classic femtosecond laser (Ziemer Group, Switzerland) and 100 eyes of 50 patients were treated with the Crystal Line femtosecond laser. The study was approved by the local ethics committee, and informed consent was obtained from all patients
Methods
The same experienced surgeon (Zhou) performed all the LASIK procedures. The corneal flaps were created under topical anesthesia using the Ziemer Classic or Ziemer Crystal Line femtosecond laser. Both femtosecond lasers were programmed to a nominal flap thickness of 110µm and an 8.5mm diameter corneal flap with the hinge placed superiorly. The FEMTO LDV Crystal Line femtosecond laser offers additional advantages over its Classic companion, such as a pulse rate faster than 5MHz, lowest pulse energy (<10nJ), shortest pulse length (200-300 femtoseconds), and smallest 3D spot volume (<2µm in all directions)(Table 1).
Table 1. The different specifications of both femtosecond-lasers.
| Nominal flap | Diameter flap | Plus rate | Plus energy | Spot volume | |
| Ziemer Classic | 110µm | 8.5mm | >1MHz | <100nJ | <2µm spot size |
| Ziemer Crystal Line | 110µm | 8.5mm | >5MHz | <10nJ | <2µm spot size |
After lifting the flap, ablations were performed using the Visx S4 excimer laser (VISX Inc., Santa Clara, USA) with a 6.0mm optical zone and 0.5mm transition zone. The corneal flap and stromal surface were irrigated with balanced normal saline solution, and the flap was repositioned. After the operation, patients were instructed to instill 0.1% fluorometholone four times per day for 3d and then tapered over for two weeks, and levofloxacin and artificial tears four times per day for 2 weeks. All patients were asked to present for regular follow-up visits, and postoperative examinations were performed at 1d, 3d, 7d and 1 month.
Fourier-domain optical coherence tomography
Imaging and measurement of the LASIK flaps were performed by the RTVue OCT system (Optovue, Inc., Fremont, CA, USA), which uses Fourier-domain (FD) optical coherence tomography (OCT) technology, also called spectral-domain OCT, rather than the older time-domain (TD) OCT technology. In the classic TD-OCT system, the scan speed is limited to hundreds of axial scans per second due the need to mechanically move a reference mirror back and forth over a range of several millimeters[14]. The sensitivity of the TD-OCT system is also limited by the sequential collection of signal from various depths in the sample. In the FD-OCT system, the reference mirror does not move during the axial scan, thus eliminating the mechanical restraint on speed. The frequency of axial scans is limited only by the frame rate of the line-scan camera, which can be electronically clocked at tens of thousands or even hundreds of thousands of cycles per second. Furthermore, because the FD-OCT system simultaneously collects signals from the entire depth range of interest, the sensitivity of the system is much higher than that of the TD-OCT[15].In our study, the CAM-L scan pattern of cornea anterior module was used to acquire 8.0mm diameter scans of the cornea for Cross Line analysis (Figure 1). The frame rate is 1024 A-scans. The resolution depth is 5.0µm and the transverse resolution is 15.0µm. The scan was centered on the vertex reflection, and 0°, 45°, 90° and 135° meridian OCT images were acquired and analyzed by the same examiner (Zhang) 1 week after surgery (Figure 2A). Flap thickness was measured at 9 points in each meridian in each of 4 separate OCT images obtained for each eye (the central zone, 1.0mm, 2.0mm, 3.0mm to the vertex and the peripheral zone of flap). The central zone was the range of ±0.5mm from the flap vertex and the peripheral zone was the range within 0.5mm from the flap edge, i.e. approximately 3.75-4.25mm from the center of the flap (Figure 1, 2B).
Figure 1. Example of a 0° meridian cross-sectional OCT image of the cornea.
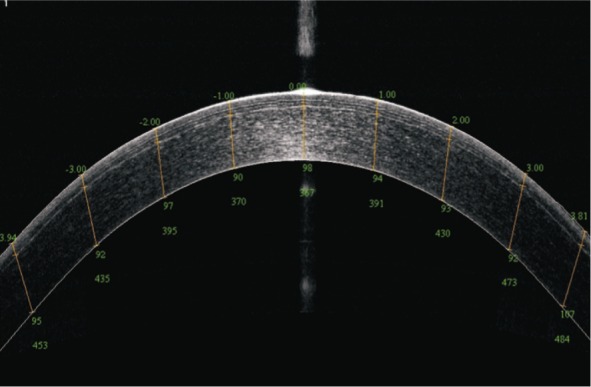
Figure 2. The measurement points in four meridians on each cornea.
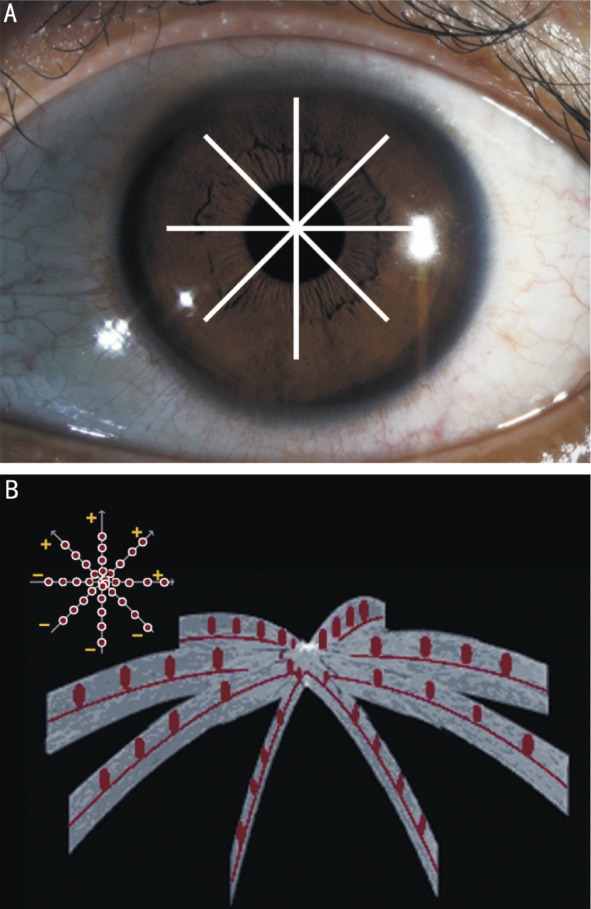
A: The 0°, 45°, 90°, and 135° meridians of the cornea; B: The 9 points in each meridian, totally 36 points.
Statistical Analysis
Data were expressed as mean±standard deviation (SD) and analyzed with the SPSS 13.0 software (SPSS Inc, Chicago, Illinois, USA). An independent samples t-test and one-way analysis of variance (ANOVA) were used to analyze measurement data conforming to normal distribution, and a Wilcoxon signed ranks test was applied for measurement data not conforming to normal distribution. A P value less than 0.05 was considered statistically significant.
RESULTS
Preoperative Characteristics
The preoperative characteristics of the patients are shown in Table 2. No significant differences were observed between Ziemer Classic and Ziemer Crystal Line femtosecond lasers (P>0.05).
Table 2. Preoperative characteristics of two groups.
| Parameters | Ziemer classic | Ziemer crystal line | 1P |
| No. of eyes | 100 | 100 | |
| Age (a) | 26.83±4.8 | 27.16±5.2 | 0.523 |
| Spherical equivalent (D) | -7.05±3.28 | -6.96±2.85 | 0.546 |
| Cylindric equivalent(D) | -1.75±0.63 | -1.68±0.72 | 0.671 |
| Central thickness (µm) | 525.92±28.37 | 527.67±31.21 | 0.784 |
| Corneal curvature (D) | 44.71±1.32 | 44.69±1.41 | 0.608 |
1Analyzed by independent samples t-test.
Central Flap Thickness
The means of the central flap thickness made by Ziemer Classic and Ziemer Crystal Line at one week post-surgery were 105.88±6.65µm and 100.86±3.54µm (P<0.01, t-test for independent-samples). In the Ziemer Classic group, the minimum mean central flap thickness was 92.75µm and the maximum was 125.75µm, resulting in a range of 33µm. In the Ziemer Crystal Line group, the corresponding values were 91µm, 113.25µm and 22.25µm, respectively. The distribution of mean central flap thicknesses for all eyes is depicted in Figure 3.
Figure 3. Central flap thicknesses.
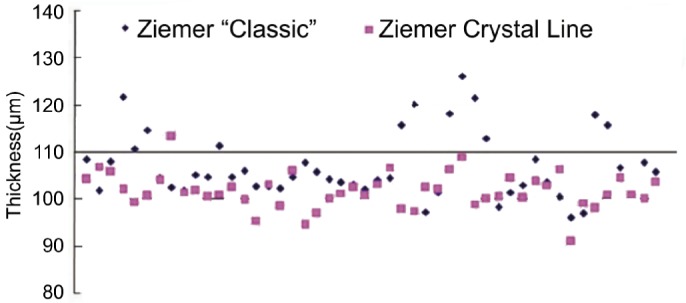
Distribution of mean central flap thicknesses at one week post-surgery for all eyes treated with Ziemer Classic and Ziemer Crystal Line.
Mean Flap Thickness
The mean thickness of corneal flap for each eye was calculated by averaging the 36 thickness measurements in four meridians in two groups. The mean flap thickness in the Ziemer Classic group was 107.65±5.09µm, while the mean flap thickness in the Ziemer Crystal Line group was 102.49±2.68µm. Figures 4A and 4B show the mean and range of the 36 flap thicknesses measured in each eye of the two groups. In the Ziemer Classic group, the mean range was 19.53±4.10µm, with a minimum and maximum range of 9.00µm and 29.00µm, respectively. In the Ziemer Crystal Line group, the mean range, minimum and maximum ranges were 15.48±3.05µm, 8.00µm and 23.00µm, respectively. The mean flap thickness in the Ziemer Crystal Line group was thinner than that in the Ziemer Classic group (P<0.01, t-test for independent-samples), and the variation range of the 36 flap thicknesses measured in each eye in the Ziemer Crystal Line group was significantly smaller than that in the Ziemer Classic group (P<0.01, t-test for independent samples).
Figure 4. Average thicknesses and ranges of 36 measurements.
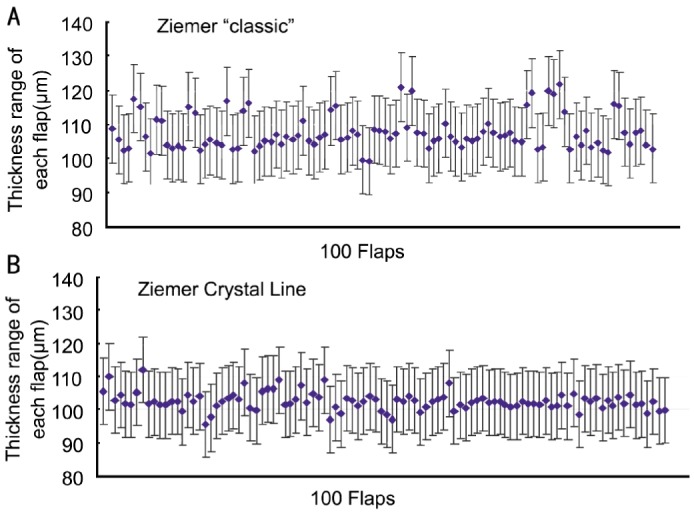
A: Ziemer Classic group; B: Ziemer Crystal Line group.
Flap Regularity
The mean and standard deviation of flap thickness obtained at 36 points in four meridians of each eye are shown in Table 3.
Table 3. Mean flap thicknesses and standard deviation of 36 points measured in the Ziemer Classic group and the Ziemer Crystal Line group.
| Measurement points | Flap thickness (µm) |
||||||||
| -Peripheral | -3mm | -2mm | -1mm | Central | 1mm | 2mm | 3mm | Peripheral | |
| Classic | |||||||||
| 0° | 109±6 | 107±7 | 108±7 | 106±7 | 105±8 | 106±7 | 109±7 | 107±7 | 110±7 |
| 45° | 106±6 | 106±6 | 107±7 | 107±7 | 105±8 | 106±7 | 108±7 | 108±6 | 110±6 |
| 90° | 108±6 | 107±6 | 109±7 | 107±8 | 107±7 | 107±7 | 109±7 | 109±6 | 111±6 |
| 135° | 108±6 | 108±5 | 109±7 | 107±7 | 107±7 | 107±7 | 108±6 | 107±6 | 110±6 |
| Crystal line | |||||||||
| 0° | 104±4 | 102±4 | 103±4 | 101±4 | 101±4 | 101±5 | 102±5 | 103±5 | 105±4 |
| 45° | 104±5 | 102±5 | 102±5 | 102±4 | 101±5 | 101±4 | 102±4 | 103±4 | 105±3 |
| 90° | 104±4 | 102±5 | 102±4 | 102±4 | 101±5 | 102±4 | 103±5 | 103±4 | 106±4 |
| 135° | 103±5 | 101±5 | 102±5 | 101±5 | 101±4 | 102±4 | 102±5 | 103±4 | 105±4 |
Corneal flaps both in the Ziemer Classic group and Ziemer Crystal Line group were uniform and regular, showing an almost-planar configuration. The maximum deviation among the 36 different points measured in each eye was 8µm in Ziemer Classic group and 5µm in Ziemer Crystal Line group (Figure 5).
Figure 5. Mean flap thickness at the relevant 36 points.
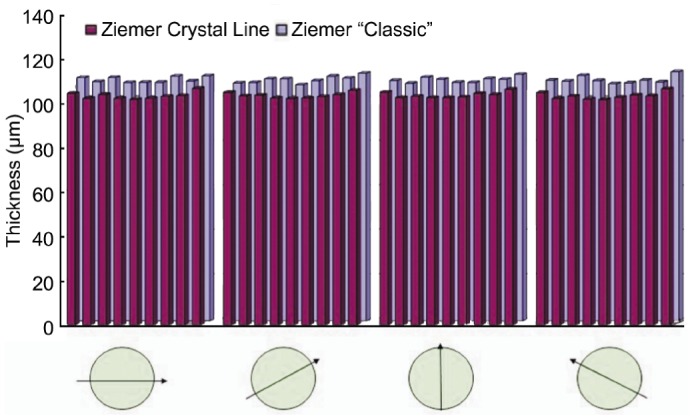
Both the Ziemer Classic group and the Ziemer Crystal Line group flaps showed an almost-planar configuration.
Radial Flap Uniformity
The flaps in the Ziemer Crystal Line group were more regular than in the Ziemer Classic group when measured from the center to the periphery. The average flap thickness values in the central and 1.0mm, 2.0mm, 3.0mm to the vertex were not significantly different in the Ziemer Crystal Line group (100.86±3.54µm, 101.42±3.05µm, 102.41±3.17µm, 102.28±2.82µm, respectively: P=0.138 by ANOVA), while the peripheral flaps were slightly thicker (104.67±2.64µm, P=0.027 by ANOVA). In the Ziemer Classic group, the central and 1.0mm to the vertex flap thickness were significantly thinner than the other three points, with a mean flap thickness of 105.88±6.65µm, 106.76±6.27µm, 108.36±5.73µm, 107.28±4.63µm and 109.10±4.34µm, respectively (P=0.029 by ANOVA).
Meridian Flap Uniformity
In the four meridians (0°, 45°, 90° and 135°), the flap mean thicknesses both in the Ziemer Classic group (107.55±4.33µm, 106.99±4.37µm, 108.25±4.44µm, 107.83±4.16µm, P=0.418 by ANOVA) and in the Ziemer Crystal Line group (102.46±3.69µm, 102.45±3.64µm, 102.70±3.51µm, 102.35±3.58µm, P=0.956 by ANOVA) did not differ significantly. But, the Ziemer Crystal Line group has significant difference compared with the Ziemer Classic group in four meridians (P<0.001, respectively).
Flap Thickness Accuracy
The maximum deviation from the nominal 110µm of 36 measurements was 8µm in the Ziemer Classic group, while the Ziemer Crystal Line group was 9µm. The average deviation of flap thickness was 6.03±2.16µm in the Ziemer Classic group and 7.75±2.83µm in the Ziemer Crystal Line group (P<0.001, t-test for independent samples) (Table 4).
Table 4. Mean deviations from nominal flap thickness of 36 measurements in the Ziemer Classic group and the Ziemer Crystal Line group.
| Measurement points | Flap thickness (µm) |
||||||||
| -Peripheral | -3mm | -2mm | -1mm | Central | 1mm | 2mm | 3mm | Peripheral | |
| Classic | |||||||||
| 0° | 5±4 | 6±4 | 6±4 | 7±4 | 8±5 | 7±5 | 6±4 | 6±4 | 5±4 |
| 45° | 5±3 | 6±4 | 6±4 | 7±4 | 6±5 | 6±4 | 6±4 | 5±4 | 5±3 |
| 90° | 5±4 | 6±4 | 7±4 | 7±4 | 8±4 | 7±4 | 6±5 | 5±3 | 5±4 |
| 135° | 5±4 | 5±3 | 6±4 | 7±4 | 7±4 | 7±3 | 5±4 | 5±4 | 5±4 |
| Crystal line | |||||||||
| 0° | 6±4 | 8±4 | 7±4 | 9±4 | 9±4 | 9±5 | 8±4 | 7±4 | 5±4 |
| 45° | 6±4 | 9±4 | 8±3 | 8±4 | 9±4 | 9±4 | 7±4 | 7±3 | 5±3 |
| 90° | 6±4 | 8±4 | 8±4 | 8±4 | 9±5 | 9±4 | 8±4 | 7±4 | 5±3 |
| 135° | 7±4 | 9±4 | 8±4 | 9±4 | 9±4 | 8±4 | 8±4 | 7±4 | 5±3 |
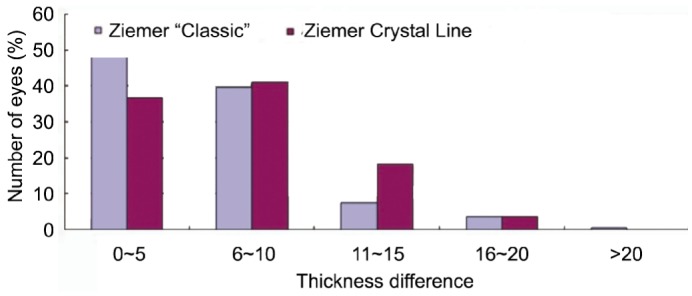
Figure 6 shows the distributions of the differences between the nominal corneal flap thicknesses and the measured flap thicknesses in the Ziemer Classic group and Ziemer Crystal Line group. There are 1 709 measurements (47.47%) on which the difference was less than 5µm in the Ziemer Classic group and 1 091 measurements (30.31%) in Ziemer Crystal Line group. But differences greater than 20µm were observed in 5 measurements (0.14%) in the Ziemer Classic group, but only one (0.03%) in the Ziemer Crystal Line group one week after surgery.
Figure 6. Distribution of the differences between nominal and measured flap thickness in the Ziemer Classic and Ziemer Crystal Line groups.
DISCUSSION
The creation of a corneal flap by laser in situ keratomileusis (LASIK) may affect postoperative corneal biomechanics and visual performance[7],[8]. Flap preparation is performed with a femtosecond laser or a mechanical microkeratome now. Regularity and accuracy of flap morphology play a role in two aspects of LASIK surgery. First, they guarantee the safety of the procedure. Second, they influence the visual outcome, a more recently controversial topic. Previous studies comparing keratome and femtosecond flap creation reported similar visual acuity outcomes, with more predictable flap parameters achieved with the femtosecond laser[8],[9],[16]. Pietilä et al[17] demonstrated that the Ziemer FEMTO LDV laser created thinner LASIK flaps than nominal but with a low standard deviation and minimal intraoperative complications. Although there are several studies of corneal flap creation with femtosecond lasers, to our knowledge this is one of the first to evaluate and compare the Ziemer FEMTO LDV Classic and Crystal Line femtosecond lasers[8]-[10],[16],[17].
In the past, the accuracy and precision of flap creation were assessed by measuring central flap thickness only[18]. Although the central thickness is most important because the cornea is thinnest in this area, the impact of peripheral corneal thickness should not be ignored. Decreased post-operative visual performance such as glare and halo under dim conditions, poor night vision and decreased contrast sensitivity (CS) values have been reported and may be related to more peripheral corneal distortions[19]-[20]. Fortunately, research on flap morphology and its effects on postoperative visual performance have gained more attention in recent years.
Accurate non-contact analysis of corneal structure has been difficult. In recent studies, we found that Fourier-domain OCT corneal pachymetry measurements were highly consistent and, in contrast to time-domain OCT, did not seem to underestimate normal corneal thickness[13],[21]. In this study, flap thickness was measured at 36 points in the 0°, 45°, 90° and 135° meridians in each of 4 separate optical coherence tomography (RTVue OCT) images obtained for each eye (the central zone, 1.0mm, 2.0mm, 3.0mm to the vertex and the peripheral zone of flap). Corneal morphology assessment can be inaccurate in the presence of motion artifacts. Fourier-domain OCT overcomes this problem to a large extent because of its high acquisition speed[12],[15]. With a speed of 26 000 axial scans per second, the RTVue is 13 times faster than the Visante (Carl Zeiss Meditec, Inc., Dublin, CA, USA), which acquires 2 000 axial scans per second. The RTVue has a depth resolution of 5µm (full-width-half-maximum), which is more than 3 times better than the Visante at 17µm. One reason for the higher resolution is the shorter center wavelength and bandwidth, 830nm, compared to Visante at 1 310nm. Recently, Prakash et al[13] reported that Fourier-domain OCT has better repeatability than time-domain OCT for corneal thickness measurements.
In this study, the mean flap thickness of the Ziemer Crystal Line group (102.49±2.68)µm was thinner than that of the Ziemer Classic group (107.65±5.09)µm (P<0.01, t-test for independent-samples). It should be noted that the flap thickness settings in the two lasers were as set at the factory. Based on the precision measurements of this study, the focus depth of the two lasers could be adjusted to achieve values closer to the nominal 110µm. Similar to what we found, Stahl et al[10] reported that the average flap thickness standard deviation in 25 flaps created with the 60KHz Intralase femtosecond laser was 5µm one month after the surgery. Previous studies[22], [23] assumed that increasing ablation depth and flap thickness are risk factors for postoperative dry eye and keratitis filiformis. This risk might therefore be reduced in eyes treated with the Ziemer Crystal Line femtosecond laser. Further studies are needed to confirm this assumption.
Our data revealed that the flaps in the Ziemer Crystal Line group were more regular than that in the Ziemer Classic group when measured from the center to the periphery. The average flap thickness values in the central and 1.0mm, 2.0mm, 3.0mm to the vertex were not significantly different in the Ziemer Crystal Line group (100.86±3.54µm, 101.42±3.05µm, 102.41±3.17µm, 102.28±2.82µm, respectively: P=0.138 by ANOVA), while the peripheral flaps were thicker than other four points (104.67±2.64µm, P=0.027 by ANOVA). In the Ziemer Classic group, the flaps were slightly but significantly thinner centrally than the points at 2 and 3mm from the vertex and peripherally, with a mean flap thickness of 105.88±4.82µm, 106.36±5.13µm, 108.36±5.76µm, 107.28±5.44µm and 109.10±5.87µm, respectively (P=0.029 by ANOVA).
The pulse rate of the Ziemer Crystal Line femtosecond laser is faster than 5MHz, and the pulse energy is very small (a few nanoJoules); lower than the pulse energy of other current femtosecond lasers. Higher femtosecond pulse energy causes thermal damage to surrounding tissue and will result in trauma and inflammatory reaction. So the stromal bed is smoother and less traumatic tissue dissection would happen in the Ziemer Crystal Line group.
In clinical practice, the safety and accuracy of flap creation remain the most important issues. One of the most dreaded complications of LASIK is iatrogenic keratectasia. Accurate flap thickness is important to maintain a postoperative corneal strength to minimize the risk of ectasia. This study found that the maximum deviation from the nominal 110µm of 36 measurements was 8µm in the Ziemer Classic group, while the Ziemer Crystal Line group was 9µm. The average deviation of flap thickness was 6.03±2.16µm in the Ziemer Classic group and 7.75±2.83µm in the Ziemer Crystal Line group (P<0.001, t-test for independent samples). There are 1 709 measurements (47.47%) on which the difference was less than 5µm in the Ziemer Classic group and 1 091 measurements (30.31%) in Ziemer Crystal Line group. But differences greater than 20µm were observed in 5 measurements (0.14%) in the Ziemer Classic group, but only one (0.03%) in the Ziemer Crystal Line group one week after surgery. It should be noted that the deviations found are mostly within the nominal resolution of the RTVue device and hence close to the achievable measurement accuracy of the used equipment.
It has been reported that the corneal flap creation could increase lower-order, as well as higher-order aberrations which could negatively affect postoperative vision performance[24]-[25]. Previous study reported that creation of the flap alone resulted in a 30% increase in higher-order aberrations. Durrie et al[24] published a study on 51 consecutive patients that had one eye randomized to Intralase and one eye to a conventional microkeratome. The authors showed there was significantly less astigmatism and trefoil in the Intralase group after surgery. Tran et al[25] performed a similar study comparing the Hansatome to the Intralase and found a statistically significant increase in the higher-order aberration in the Hansatome group but not in the Intralase group. Therefore, the thinner and more uniform, predictable and reproducible corneal flaps created by the Ziemer Crystal Line femtosecond laser may be effective to improve visual performance. A long term follow-up and further studies are needed to confirm this finding.
In conclusion, the flaps made by Ziemer Crystal Line femtosecond laser are more uniform and thinner than those created by Ziemer Classic femtosecond laser. Further studies are needed to determine whether the thinner and more regular morphology of the femtosecond laser flap contributes to a reduction in the postoperative biomechanical reaction and higher-order aberrations.
Footnotes
Foundation item: WuJieping Medical Foundation (No.320675010003)
REFERENCES
- 1.Flanagan GW, Binder PS. Role of flap thickness in laser in situ keratomileusis enhancement for refractive undercorrection. J Cataract Refract Surg. 2006;32(7):1129–1141. doi: 10.1016/j.jcrs.2006.01.095. [DOI] [PubMed] [Google Scholar]
- 2.Solomon KD, Donnenfeld E, Sandoval HP, Al Sarraf O, Kasper TJ, Holzer MP, Slate EH, Vroman DT, Flap Thickness Study Group Flap thickness accuracy: comparison of 6 microkeratome models. J Cataract Refract Surg. 2004;30(5):964–977. doi: 10.1016/j.jcrs.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 3.Flanagan GW, Binder PS. Precision of flap measurements for laser in situ keratomileusis in 4 428 eyes. J Refract Surg. 2003;19(2):113–123. doi: 10.3928/1081-597X-20030301-05. [DOI] [PubMed] [Google Scholar]
- 4.Wang Z, Chen J, Yang B. Posterior corneal surface topographic changes after laser in situ keratomileusis are related to residual corneal bed thickness. Ophthalmology. 1999;106(2):406–409. doi: 10.1016/S0161-6420(99)90083-0. [DOI] [PubMed] [Google Scholar]
- 5.Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110(2):267–275. doi: 10.1016/S0161-6420(02)01727-X. [DOI] [PubMed] [Google Scholar]
- 6.Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14(3):312–317. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs JM, Taravella MJ. Incidence of intraoperative flap complications in laser in situ keratomileusis. J Cataract Refract Surg. 2002;28(1):23–28. doi: 10.1016/s0886-3350(01)01097-5. [DOI] [PubMed] [Google Scholar]
- 8.Lim T, Yang S, Kim MJ, Tchah H. Comparison of the IntraLase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Am J Ophthalmol. 2006;141(5):833–839. doi: 10.1016/j.ajo.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis; prospective contralateral eye study. J Cataract Refract Surg. 2005;31(1):120–126. doi: 10.1016/j.jcrs.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 10.Stahl JE, Durrie DS, Schwendeman FJ, Boghossian AJ. Anterior segment OCT analysis of thin IntraLase femtosecond flaps. J Refract Surg. 2007;23(6):555–558. doi: 10.3928/1081-597X-20070601-03. [DOI] [PubMed] [Google Scholar]
- 11.Chen TC, Cense B, Pierce MC, Nassif N, Park BH, Yun SH, White BR, Bouma BE, Tearney GJ, de Boer JF. Spectral domain optical coherence tomography; ultra-high speed, ultra-high resolution ophthalmic imaging. Arch Ophthalmol. 2005;123(12):1715–1720. doi: 10.1001/archopht.123.12.1715. [DOI] [PubMed] [Google Scholar]
- 12.Yi K, Mujat M, Park BH, Sun W, Miller JW, Seddon JM, Young LH, de Boer JF, Chen TC. Spectral domain optical coherence tomography for quantitative evaluation of drusen and associated structural changes in non-neovascular age-related macular degeneration. Br J Ophthalmol. 2009;93(2):176–181. doi: 10.1136/bjo.2008.137356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prakash G, Agarwal A, Jacob S, Kumar DA, Agarwal A, Banerjee R. Comparison of Fourier-domain and time- domain optical coherence tomography for assessment of corneal thickness and intersession repeatability. Am J Ophthalmol. 2009;148(2):282–290. doi: 10.1016/j.ajo.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, Hee MR, Flotte T, Gregory K, Puliafito CA. Optical coherence tomography. Science. 1991;254(5035):1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Boer JF, Cense B, Park BH, Pierce MC, Tearney GJ, Bouma BE. Improved signal-to-noise ratio in spectral-domain compared with time-domain optical coherence tomography. Opt Lett. 2003;28(21):2067–2069. doi: 10.1364/ol.28.002067. [DOI] [PubMed] [Google Scholar]
- 16.Jagow BV, Kohnen T. Corneal architecture of femtosecond laser and microkeratome flaps imaged by anterior segment optical coherence tomography. J Cataract Refract Surg. 2009;35(1):35–41. doi: 10.1016/j.jcrs.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Pietilä J, Huhtala A, Jääskeläinen M, Jylli J, Mäkinen P, Uusitalo H. LASIK flap creation with the Ziemer femtosecond laser in 787 consecutive eyes. J Refract Surg. 2010;26(1):7–16. doi: 10.3928/1081597X-20101215-02. [DOI] [PubMed] [Google Scholar]
- 18.Reinstein DZ, Srivannaboon S, Archer TJ, Silverman RH, Sutton H, Coleman DJ. Probality model of the inaccuracy of residual stromal thickness prediction to reduce the risk of ectasia after LASIK. Part II: quantifying population risk. J Refract Surg. 2006;22(9):861–870. doi: 10.3928/1081-597X-20061101-05. [DOI] [PubMed] [Google Scholar]
- 19.Marcos S. Aberrations and visual performance following standard laser vision correction. J Refract Surg. 2001;17(5):S596–S601. doi: 10.3928/1081-597X-20010901-19. [DOI] [PubMed] [Google Scholar]
- 20.Applegate RA, Hilmantel G, Howland HC, Tu EY, Starck T, Zayac EJ. Corneal first surface optical aberrations and visual performance. J Refract Surg. 2000;16(5):507–514. doi: 10.3928/1081-597X-20000901-04. [DOI] [PubMed] [Google Scholar]
- 21.Prakash G, Ashok Kumar D, Agarwal A, Sarvanan Y, Jacob S, Agarwal A. Evaluation of bilateral minimum thickness of normal corneas based on Fourier-domain optical coherence tomography. J Cataract Refract Surg. 2010;36(8):1365–1372. doi: 10.1016/j.jcrs.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 22.Patel SV, Maguire LJ, McLaren JW, Hodge DO, Bourne WM. Femtosecond laser versus mechanical microkeratome for LASIK; a randomized controlled study. Ophthalmology. 2007;114(8):1482–1490. doi: 10.1016/j.ophtha.2006.10.057. [DOI] [PubMed] [Google Scholar]
- 23.De Paiva CS, Chen Z, Koch DD, Hamill MB, Manuel FK, Hassan SS, Wilhelmus KR, Pflugfelder SC. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006;141(3):438–445. doi: 10.1016/j.ajo.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis; prospective contralateral eye study. J Cataract Refract Surg. 2005;31(1):120–126. doi: 10.1016/j.jcrs.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 25.Tran DB, Sarayba MA, Bor Z, Garufis C, Duh YJ, Soltes CR, Juhasz T, Kurtz RM. Randomized prospective clinical study comparing induced aberrations with IntraLase and Hansatome flap creation in felloweyes; potential impact onwavefront-guided laser in situ keratomileusis. J Cataract Refract Surg. 2005;31(1):97–105. doi: 10.1016/j.jcrs.2004.10.037. [DOI] [PubMed] [Google Scholar]


