Summary
Introduction
fetal rhabdomyoma is the most common fetal cardiac tumor and is often associated with tuberous sclerosis. Usually the tumors are relatively small and show no mediastinal shift. Fetal hydrops and pericardial effusion are rarely seen.
Case
in this case report we present the neonatal clinical course of a case of prenatal diagnosis of giant cardiac rhabdomyomas.
Conclusion
an early prenatal diagnosis may help for an adequate planning of perinatal monitoring and treatment with involvement of a multidisciplinary team.
Keywords: fetal cardiac tumor, rhabdomyoma, tuberous sclerosis
Introduction
Fetal cardiac rhabdomyoma is a rare condition, but it is the most common fetal cardiac tumor and the incidence of association with tuberous sclerosis may be as high as 50–80%.
In this report we present the clinical course of a case of neonatal cardiac rhabdomyoma and discuss the importance of prenatal diagnosis of fetal cardiac tumors.
Case
We report on a 32-year-old gravid 2, para 1, who was referred at 27 weeks of gestation with a mediastinal tumor and suspected pleural effusion. The patient had conceived spontaneously and no genetic disorders were known.
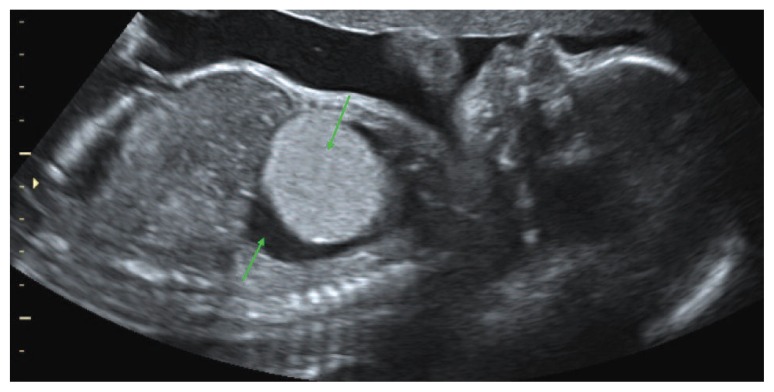
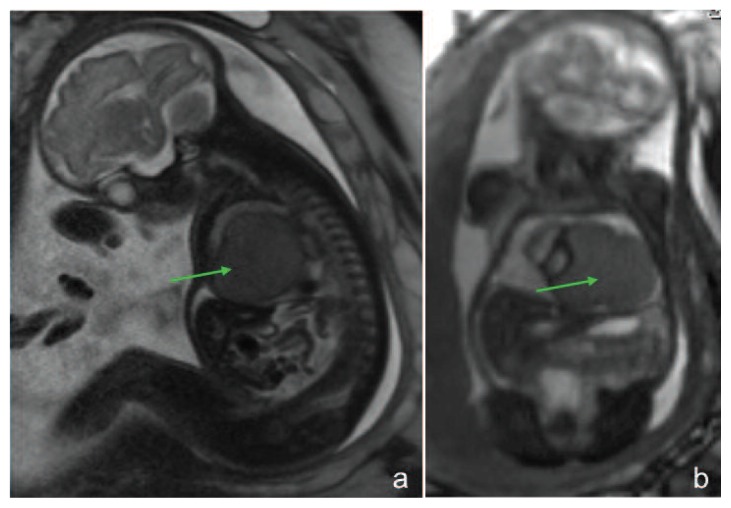
Ultrasonographic examination revealed a large homogeneous, hyperechogenic tumor (39 mm), originating from the left ventricular wall (Figs. 1–3). There was a mediastinal shift with dextroposition of the heart in combination with massive pericardial effusion. The heart was of normal size with no myocardial hypertrophy, the left ventricle hypocontractile but without atrioventricular insufficiency. A cardiac rhabdomyoma was suspected. No other intra- or extracardiac abnormalities were found. An additional MRI was performed confirming the ultrasound findings (Fig. 3), no cerebral lesions were detected. Amniocentesis revealed a normal female karyotype. There was no family history of tuberous sclerosis.
Figure 1.
The fetus at 27 weeks of gestation showing a round homogeneous, hyperechogenic tumor with pericardial effusion.
Figure 3.
MRI presentation of the rhabdomyoma, pericardial effusion and mediastinal shift (b).
The patient received betamethasone for prenatal lung maturation.
Serial ultrasonographic examinations were performed. The size of the tumor increased in the follow-up to 49 mm. There was a passing mild ascites, but a constant massive pericardial effusion and increasing polyhydramnios.
At 36 weeks a second smaller intracardiac tumor (6 mm) was found. Because of newly developed oligohydramnios (PROM negative) and fetal tachycardia a caesarean section was performed in spinal anesthesia. A female neonate was delivered, weighing 2730 g, the 5- and 10 minutes Apgar scores both 9. The neonate was respiratorically instable and was intubated.
Neonatal echocardiography confirmed the prenatal diagnosis of cardiac rhabdomyomas. There was no evidence of outflow tract obstruction or hemodynamic compromise. To prevent cardiac insufficiency the neonate received anticongestive medication.
Sonography of the head revealed a small calcified intracranial lesion. The result of the genetic analysis confirmed the suspicion of tuberous sclerosis. The neurological examination was without pathological findings.
As the cardiac function was normal no surgical treatment was performed, the infant was discharged and has been managed at the outpatient pediatric clinic. No abnormality was detected in the sonography of the head and the kidneys after 6 months. The echocardiographic monitoring showed a spontaneous regression of the cardiac masses in number and dimension (the follow up mri after 12 months showed only one intracardiac tumor of 33 mm).
Discussion
Cardiac rhabdomyomas are the most common fetal cardiac tumors but are still a rare condition (1). They are hamartomas and can be located anywhere within the atrial and ventricular myocardium (1). In ultrasound they appear as round homogenous, hyperechogenic, mostly multiple masses in the ventricles (2). Differential diagnosis are teratoma, fibroma and hemangioma but the presence of multiple tumors involving the ventricular myocardium is indicative of rhabdomyomas (3). Most of these tumors belong to the group of late-onset congenital heart diseases (4). This emphasizes the importance of ultrasound examination around the beginning of the third trimester and serial monitoring.
Complications can include arrhythmias, progressive compression of cardiac, vascular and pulmonary structures by a rapidly growing mass or effusion (5).
The incidence of associated tuberous sclerosis may be as high as 50–80% (6).
Although tuberous sclerosis is generally reported to follow an autosomal dominant hereditary pattern with variable expressivity, this case seems to be sporadic as there was no family history (7). In the absence of a family history a cardiac rhabdomyoma may be the earliest sign of tuberous sclerosis in utero and precede the detection of brain or kidney lesions (7).
After birth rhabdomyomas usually regress in size, as we could confirm in our case, and smaller ones may even completely resolve (1, 5). Therefore an expectant management is advocated if the cardial function is compensated (1, 3). Surgical treatment is advisable only in selected cases. They can be difficult to remove completely, because they are often located deeply in the myocardium and have major vessel supplies from the coronary arteries (8).
With the performed serial ultrasound examinations we were able to monitor the size of the tumor, the amount of pericardial effusion and the cardiac function and therefore could await maturity before delivery.
Conclusion
An early prenatal diagnosis may help for an adequate planning of perinatal monitoring and treatment with involvement of a multidisciplinary team.
Figure 2 a–c.
a) Cross section of the thorax showing the rhabdomyoma, causing a mediastinal shift with dextroposition of the heart in combination with pericardial effusion (asterix). b) Sagittal view of the fetal thorax and abdomen at 33 weeks. c) The frontal view shows mild ascites (asterix) in the lower abdomen as well as the rhabdomyoma and pericardial effusion (asterix) in the thorax.
References
- 1.Holley D, Martin G, Brenner J, Fyfe D, Huhta J, Kleinman C, Ritter S, Silverman N. Diagnosis and management of fetal cardiac tumors: A multicenter experience and review of published reports. J Am Coll Cardiol. 1995;26:516–520. doi: 10.1016/0735-1097(95)80031-b. [DOI] [PubMed] [Google Scholar]
- 2.Allan L. Fetal cardiac tumors. In: Allan L, Hornberger L, Sharland G, editors. Textbook of fetal cardiology. Greenwich Medical Media Limited; London: 2000. pp. 358–365. [Google Scholar]
- 3.Geipel A, Krapp M, Germer U, Becker R, Gembruch U. Perinatal diagnosis of cardiac tumors. Ultrasound Obstet Gynecol. 2001;17:17–21. doi: 10.1046/j.1469-0705.2001.00314.x. [DOI] [PubMed] [Google Scholar]
- 4.Yagel S, Weissmann A, Rotstein Z, Manor M, Hegesh J, Anteby E, Lipitz S, Achiron R. Congenital heart defects. Natural course and in utero development. Circulation. 1997;96:550–555. doi: 10.1161/01.cir.96.2.550. [DOI] [PubMed] [Google Scholar]
- 5.Yinon Y, Chitayat D, Blaser S, Seed M, Amsalem H, Yoo S, Jaeggi E. Fetal cardiac tumors: a single-center experience of 40 cases. Prenatal Diagnosis. 2010;30:941–949. doi: 10.1002/pd.2590. [DOI] [PubMed] [Google Scholar]
- 6.Isaacs H., Jr Fetal and neonatal cardiac tumors. Pediatr Cardiol. 2004;25(3):252–273. doi: 10.1007/s00246-003-0590-4. [DOI] [PubMed] [Google Scholar]
- 7.Chao AS, Chao A, Chang YC, Chang YL, Hsieh CC, Lien R, Sun WJ. Outcome of antenatally diagnosed cardiac rhabdomyoma: case series and a meta-analysis. Ultrasound Obstet Gynecol. 2008;31:289–295. doi: 10.1002/uog.5264. [DOI] [PubMed] [Google Scholar]
- 8.Benyounes N, Fohlen M, Devys J, Delalande O, Moures J, Cohen A. Cardiac rhabdomyomas in tuberous sclerosis patients: A case report and review of the literature. Archives of Cardiovascular Disease. 2012;105:442–445. doi: 10.1016/j.acvd.2012.01.009. [DOI] [PubMed] [Google Scholar]