Abstract
Parenthood is associated with decreased physical activity and unhealthy dietary changes. Previously mothers have been the focus of studies examining the influence of children on parents’ BMI, largely ignoring whether parenting affects fathers. This study assessed weight gain in mothers and fathers (by birth or other), using longitudinal repeated-measures models to assess BMI changes, over time; parents were compared to non-parents. Data was from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort study and included 2881 black and white adults, age 18-30, without children at baseline (1985-86), from four urban locations. At each time point (years 2, 5, and 7), changes in BMI from baseline were analyzed, comparing those who had their children in their household at that time point (parents) and those without children (non-parents). The “child effect” is the average difference in BMI-change in parents compared to non-parents. In fathers, overall, the child effect was not significant (black males 0.30 kg/m2, p=0.09; white males 0.03 kg/m2, p=0.77). Among black men, however, interactions between age and parental status were significant (p=0.02). Black men who were aged 18-24 at baseline, and became fathers during the next 7 years, demonstrated a significant child effect, gaining an average of 0.68 kg/m2 more than non-fathers (p=0.003). Mothers of both races demonstrated the child effect; for blacks it equaled 0.65 kg/m2 (p=0.003); for whites it equaled1.12 kg/m2 (p= <0.001). These data reveal that becoming a parent can affect the BMI of some adults and suggests that obesity prevention interventions for children and adult-focused healthy-lifestyle interventions could have additional impact through a family focus targeting both parent and child outcomes.
Keywords: BMI, Parents, Parent-Child relations, longitudinal
Parenthood often triggers dietary changes1-5 and decreased physical activity,6-9 so one might expect parents to gain more weight than nonparents. This assumption is examined in this and the authors’ previously publisher paper, both of which examine data from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort study5 to determine how children can influence the BMI and diet patterns of adults. In the previous paper, dietary changes, over a 7-year period, are compared in parents and non-parents, showing that the predominant difference was that parents tended to eat more saturated fat than non-parents.
This paper examines that same cohort and time period to estimate the average weight gained in early parenthood compared to nonparents. Previous studies, 10-12 including studies of post-partum women in the CARDIA cohort,13,14 showed that mothers tended to gain more weight than nonmothers, especially if they were non-smokers or overweight before becoming parents. It is not surprising, then, that postpartum women who gained weight also consumed more calories and exercised less.15 Nevertheless, fathers share much of the same food and physical activity environments as mothers, so it might be expected that fathers might similarly change their habits after children enter their home.3,6 Few studies, however, examined lifestyle changes of fathers. The three published studies that did examine fathers’ diets found that all parents tend to consume more saturated fat3-5 and a few studies suggested that fathers also decrease their physical activity.6-9 Therefore, fathers might be expected to gain more weight than non-fathers. Since very few studies have examined weight gain in fathers, this paper primarily focuses on them.
Although data on weight gain in fathers is sparse, two cross-sectional studies on men show their risk for obesity correlates with the number of children they have; and having more than five children (including adult children) correlated with an elevated BMI.16,17 Nevertheless, both of those studies examined BMI in older men (average 55 and 70 years), who are unlikely to have had children under 10 years. Moreover, those studies were neither longitudinal (including early parenthood), nor did they compare men with and without children. One longitudinal study used self-reported heights and weights to suggest that fathers do gain more weight than non-fathers, over time, but studies rarely collect the measured height and weight data needed for a longitudinal analysis.
Thus, the CARDIA study is particularly useful because it contains valuable longitudinal data, e.g., age, measured BMI, and parental status. These data were used to examine how parenthood affects BMI changes in black and white adults compared to non-parents, over a 7-year time period, with the hypothesis that parents would increase their BMI more.
Methods and Procedures
Sample population
The CARDIA Study was a primarily urban, multicenter, longitudinal, prospective cohort study to identify how coronary risk factors develop in young adults. The CARDIA cohort consisted of 5115 unrelated black and white men and women, who were between the age of 18 and 30 in 1985, when the study began. The CARDIA cohort was recruited by community-based sampling in Birmingham, AL; Chicago, IL; and Minneapolis, MN, and by sampling from the Kaiser Permanente Health Plan membership in Oakland, CA.18,19 Data were collected at baseline, and at years 2, 5, 7, 10, 15 and 20. At year 7, the retention rate was 81%.19
The analysis focused on the first seven years of the CARDIA study and included participants who neither had children nor were pregnant at baseline (n = 3470). Subjects were excluded if their BMI values were missing at baseline (n = 12), if they had no BMI values beyond year 2 (n = 403); if their energy intake at baseline or year 7 was > 8000 or < 800 kcal/day for men or > 6000 or <600 kcal/day for women (n=87); or if they lacked baseline data for total physical activity, education, caloric intake or smoking status (n = 20). To focus on the effect of having children enter and remain in the home, participants who had a child enter the household by years 2 or 5 but who had no children in the household at year 7 were also excluded (n = 67). If a participant was pregnant at a follow-up visit, the BMI from that visit was treated as missing but the participant remained in the analysis. The final sample size included 2881 participants.
Data Collection
Trained interviewers collected data,20 which included socio-demographics, cardiovascular risk factors, and information about family composition. At baseline and year 7, participants answered a validated, diet-history questionnaire.21,22 Nutrient intake was calculated using the University of Minnesota Nutrition Coordinating Center’s Nutrient Database, versions 10 (baseline) and 20 (year 7).20,22
Variables
The primary exposure (child) was the presence of a child (biological or otherwise and under 18) in the household of the participant. This variable was measured at years 2, 5, and 7. The participants had identified the children as their own, but these children could have entered the household by birth, adoption, marriage or other.
The primary outcome was change in BMI from baseline, computed at years 2, 5, and 7 (BMI change score); thus, a subject with complete data has three scores. Participants in light clothing were weighed by a calibrated balance beam scale; and their height to the nearest 0.5 cm was measured by a stadiometer.23 BMI was calculated as weight (in kilograms) divided by height (in meters squared).
The longitudinal statistical models were adjusted for the following baseline covariates: age (18-24 or 25-30 years), race (black or white), education, field center, partner status (married or living in a marriage-like relationship vs. other), current smoking status, physical activity score, full-time employment status, daily energy intake, and overweight status (BMI < 25 or ≥ 25). The physical activity score is calculated from the validated CARDIA Physical Activity Questionnaire, which assesses usual activity over the past year24 on 13 different moderate-to-vigorous activities.25 The total activity score is the sum of all activities and combines a metabolic equivalents score, frequency and a weighting factor to represent duration.24,25
Statistical Methods
Baseline characteristics of adults compared those whose home included a child at year 7 vs. those whose home did not using two sample t-tests, nonparametric Wilcoxon tests or chi-square tests.
Longitudinal analyses were performed separately according to race and gender (e.g., white male, black female) and included the variables described above. At each time point, the analysis evaluated the change in BMI from baseline, comparing those with children in the household at that time point (parents) and those without (non-parents). The BMI-change scores were averaged across the three visits, and if they differed from zero, then this difference was defined as the “child effect.” If the child effect is a positive number, then the BMI of parents rose more than non-parents Because parent-status can change over time, subjects can be classified in different groups at different visits; e.g. a participant that is a nonparent at year 2 can be a parent at year 5.
Each model included two- and three-way interactions between the variables for parent status (child) and year of visit with either baseline overweight status or age category as well as the interaction of each baseline covariate with year of visit. Primary tests consisted of four child-effect tests, one for each of the four gender-race subgroups. Using a Bonferroni correction, individual test were deemed significant if p ≤ 0.05/4 = 0.0125. All other tests (e.g., for interactions) were considered exploratory and significant if p ≤ 0.05.
Due to the longitudinal nature of the data, longitudinal repeated measures models were estimated using the SAS procedure, MIXED,26,27 which accounts for within subject correlation. To account for within-subject correlation, the three within-subject outcomes (change in BMI from baseline at year 2, 5, and 7) were assumed to have a multivariate normal distribution across subjects. Because the exposure variable child is time dependent, covariance matrices were allowed to differ according to the four possible child-classification patterns (defined when a child entered the household): never, between baseline and year 2, between years 2 and 5, or between years 5 and 7. Within-subject outcomes were assumed to have the same covariance matrix for subjects with the same child-classification pattern; but the covariance matrices were allowed to differ between child-classification pattern groups. The covariance matrices were allowed to be unstructured; i.e, no constraints were placed on the correlations and variances. (This approach makes less restrictive assumptions than the approach that includes subjects as “random effects” in the model, which implies a specific covariance matrix structure.) All participants providing BMI at baseline and at least year 5 or 7 were included, unless excluded as described above. Missing data was accounted for by the SAS Mixed procedure, which uses a likelihood approach to account for outcomes that are missing at random.26-28
The main analysis included only a variable for physical activity score at baseline. To determine whether the physical activity mediated the relationship between parenthood and BMI, an additional analysis added physical activity scores (measured at each follow up visit) to the main model, to test whether the child effect would change. An additional analysis was also run with a three level BMI classification variable (<25, 25-29 and >29).
Statistical analysis was conducted using Statistical Analysis Software (version 9.2, 2010, SAS Institute Inc, Cary, NC). This study was approved by the University — Institutional Review Board. The CARDIA study was approved by all field center IRBs and participants gave written, informed consent.
Results and Discussion
Throughout this article, parent/father/mother refers to an adult who had his/her child (biological or other) living in his or her home by year 7. Non-parent/non-father/non-mother refers to an adult without any children or without any children living in the home by year 7.
At baseline, future parents had the same average BMI as their counterparts who would remain childless. By year 7, 32% of the participants had become parents, with the average age of parents and non-parents at baseline being 24.8 and 24.2 years, respectively. 40.6% of parents were black compared to 35.9% of non-parents (p<0.05). At baseline, future parents were more likely to be older, female, living with a partner, and employed full-time (Table 1). The final-analysis dataset included 2881 participants (1490 women and 1391 men); 246 had children by year 2, 651 by year 5, and 914 by year 7. The average age of the children at year 7 was 3.9 years with only 11% above age 7.
Table 1.
Baseline (1985-86) sample characteristics of adults with or without children at year 7 (1992-93), CARDIA study
| Children (n = 914)a |
No Children (n = 1967) |
|
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Age at Baseline (yrs) | 24.8 ± 3.5 | 24.2 ± 3.6** |
| Physical activity score (Exercise Units) b | 439 ± 283 | 444 ± 292 |
| Years of Education completed | 14.4 ± 2.4 | 14.4 ± 2.2 |
| BMI | 24.1 ± 4.4 | 24.0 ± 4.6 |
| Calories per day | 2688±1285 | 2738±1264 |
| % | % | |
|
| ||
| Female (%) * | 55.0 | 50.2* |
| Race / Ethnicity (%) * | ||
| Caucasian | 59.4 | 64.1* |
| African American | 40.6 | 35.9 |
| Living with Partner (%) *** c | 36.3 | 15.8** |
| Working Full Time (%) *** | 65.0 | 56.9** |
| Smoking (%) | 23.5 | 23.8** |
p≤ 0.05 for comparison of those with and without children
p ≤ 0.001 for comparison of those with and without children
Children in the home at year 7
Physical Activity score = intensity × frequency = Σbi * (P2i+2*P3i) where bi = the intensity level of the activity in METS, P2i = number of months doing an activity and P3i = the number of months doing the activity above a specified frequency.
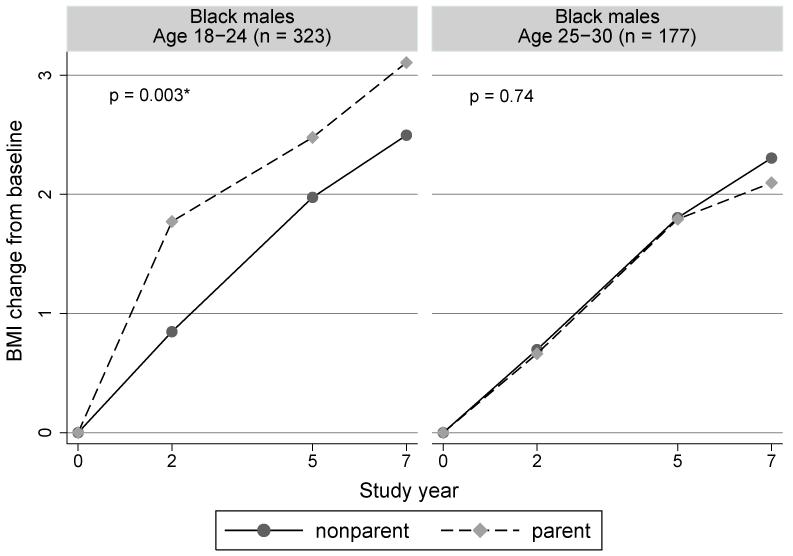
Living with partner = married or living as married at baseline
The CARDIA data were used to calculate the child effect: the average difference in BMI change (from baseline to years 2, 5, and 7) between parents and non-parents. In contrast to the child effect observed in women, these data show no significant child effect for men (Figure 1): the child effect for black men was 0.30 kg/m2 (CI: −0.05 to 0.64, p = 0.09) and for white men was 0.03 kg/m2 (CI: −0.17 to 0.23, p = 0.77). In other words, fathers did not increase their BMI more than non-fathers. Neither group showed a significant interaction between baseline overweight status and parent status. Substituting a three-level weight-status variable did not change the findings.
Figure 1.
Adjusted average change in BMI from baseline at each time point for parents and nonparents.
n is the number of subjects.
* p < 0.0125.
Data points are the estimated BMI changes from baseline, adjusted for baseline covariates.
These were computed using the LSMEANS statement in SAS. The points of value zero at year 0 are added only for illustrating the change from baseline for the other visits.
The p-value is for testing if the adjusted BMI change from baseline, averaged across the 2-, 5-, and 7-year time points, differs between the parent and nonparent groups
Note participants change groups as they have children.
Few studies are comparable to this study because studies of the effects of parenthood on adult weight largely ignore men. One study found that more than one child in the home increased a man’s risk for obesity by 4% per child.16 Another found that men (age 50-89) with five or more children were significantly more obese than childless men.17 Both studies were cross-sectional and compared weight after the men’s children were grown. Another 5-year longitudinal study looked solely at young men with children and found fatherhood had not affected their BMI.9 In contrast, a 15-year study showed that, over time, the average father gained 6 kilograms more than a non-father. That study, however, relied on self-reported heights and weights.10 In the current study, only 54% of the men with children had more than one child, and few had more than two. This might explain why the current analysis did not detect the BMI increase detected by others. Taken together, these studies suggest fathers who gain more weight do so only after the early years of parenthood or if they have many children.
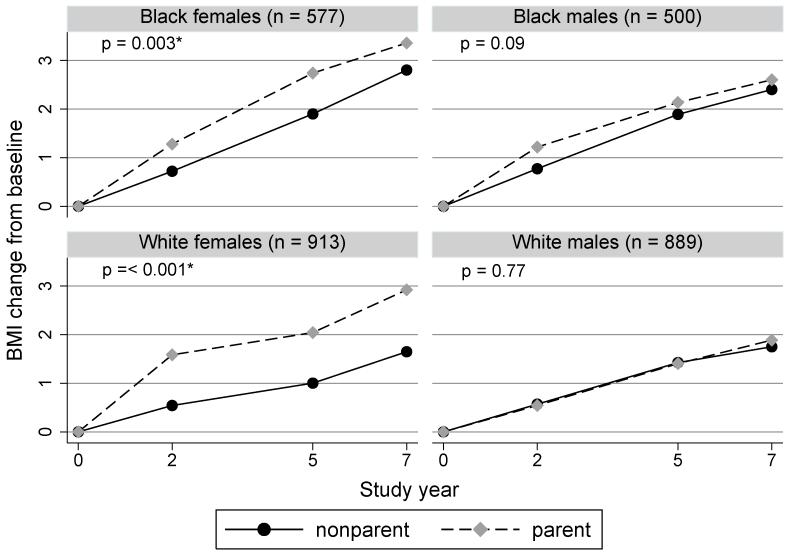
The exception to this trend may be young black men, who showed a significant interaction between age and parental status (p = 0.02). For black men who were age 18-24 at baseline, fatherhood triggered an increase in their BMI by an average of 0.68 kg/m2 (CI: 0.24 to 1.12, p = 0.003). The corresponding “child effect” for black men age 25-30 was −0.08 kg/m2 (CI: −0.58 to 0.41, p = 0.74) (Figure 2). This finding is considered exploratory due to multiple comparisons (p = 0.02) and warrants a further examination of BMI changes in young black fathers.
Figure 2.
Adjusted average change in BMI from baseline at each time point in Black males age 18-24 and 25-30 at baseline comparing parents and nonparents.
n is the number of subjects.
* p < 0.05
Points at 2, 5 and 7 years are the estimated BMI changes from baseline, adjusted for baseline covariates. These were computed using the LSMEANS statement in SAS. The points of value zero at year 0 are added only for illustrating the change from baseline for the other visits.
The p-value is for testing if the adjusted BMI change from baseline, averaged across the 2-, 5-, and 7-year time points, differs between parents and nonparents.
It is unclear why children would influence the BMI of young black men in particular. Young black fathers in our study did not differ from younger black non-fathers with regard to education or full-time employment. On average, all younger black men had less education and were less likely to work full-time than older black men and white men at baseline. Also, age group and race had no effect on the number of children in their home. Thus young black men were either more affected by the presence of children, or having children in their home is a marker for something else related to BMI. Moreover, the data do not support changes in physical activity as the sole cause of increased weight gain because adjusting for physical activity level at each follow up visit did not change the conclusions or p values. Thus, dietary changes related to parenthood may be driving weight gain.
For many people, acquiring a partner and having children often occur within a similar timeframe; thus it is difficult to distinguish how each independently influences weight gain and their effects may be synergistic. The authors could not pursue this line of research because very few men with children lacked a partner. It may be notable that a separate analysis showed that, for all groups, gaining a partner was related to weight gain; and younger black men tended to gain the most (not shown). That analysis, however, did not take parental status into account. Studies by other groups show mixed results, but many suggest married men may gain more weight than their single counterparts.29-32 Thus, addition of a partner could also have contributed to some of parents’ weight gain. Indeed, white men with partners also gained weight but showed no “child effect.” Further analysis is needed.
BMI results for women were consistent with previous studies of weight changes and retention post-partum.13,14 The current study, however, did not require that the child entering the home be the biological offspring. This type of analysis shows that pregnancy aside, compared to non-mothers, women who became mothers increased their BMI significantly; this child effect was seen in both blacks (child effect = 0.65 kg/m2, CI 0.22 to 1.08, p = 0.003) and whites (child effect = 1.12 kg/m2, CI 0.80 to 1.44, p < 0.001)(Figure 1). Although age did not interact with the child effect for black or white women, the child effect did vary by overweight status for white women only (p=0.02). For white females already overweight at baseline, the “child effect” was associated with an average increase in their BMI of 1.50 kg/m2 (CI: 0.93 to 2.06, p < 0.001). In contrast, normal-weight, white mothers averaged a BMI increase of 0.74 kg/m2 (CI: 0.44 to 1.04, p < 0.001). Even when women’s physical activity was accounted for the “child effect” remained, suggesting that diet changes related to parenthood may have a role in excess weight gain. Since the majority of mothers experienced pregnancy, their weight gain is likely a combination of weight changes related to pregnancy and lifestyle changes related to parenthood.
Our study’s strengths include a large biracial cohort from four geographic locations, followed prospectively over seven years; in addition all measurements were taken by study personnel rather than by self-reporting subjects.33,34 Still, our interpretations are not without limitations. Our data were collected between 1985 and 1993; and it is possible that findings could differ in current families. Furthermore, the child effect might depend on the age of the children. In our cohort, most children were under age 7 years. Also, our data controlled for educational level and full-time employment but not directly for income. Nevertheless, education and employment are good indicators of SES; and education correlates better with weight gain than income.35 Finally, diet data was only available at baseline and year 7, precluding an analysis of how diet mediates changes in BMI. For more information on dietary changes in parents,36 see the authors’ previous paper.
In conclusion, all adults (parents and non-parents) in this cohort gained weight over time and thus would benefit from intervention, but young black fathers and black and white mothers gained more weight than their childless counterparts and may deserve specific attention. Because becoming a parent can affect an adult’s BMI, obesity prevention interventions for children and adult-focused healthy-lifestyle interventions could have additional impact through a family focus targeting both parent and child outcomes. While this analysis made use of some of the best data available, future studies should confirm the findings in a more recent generation. In addition, further studies should explore the factors that affect parents’ lifestyle changes and how to tailor interventions for families with children.
Acknowledgements
We would like to acknowledge the contributions of our data analyst Kelly Richardson PhD.
Funding Disclosure
This work was supported by a K23 from NHLBI (---------). Work on this manuscript was also supported (or partially supported) by contracts: University of Alabama at Birmingham, Coordinating Center, N01-HC-95095; University of Alabama at Birmingham, Field Center, N01-HC-48047; University of Minnesota, Field Center and Diet Reading Center (Year 20 Exam), N01-HC-48048; Northwestern University, Field Center, N01-HC-48049; Kaiser Foundation Research Institute, N01-HC-48050; University of California, Irvine, Echocardiography Reading Center (Year 5 & 10), N01-HC-45134; Harbor-UCLA Research Education Institute, Computed Tomography Reading Center (Year 15 Exam), N01-HC-05187; Wake Forest University (Year 20 Exam), N01-HC-45205; New England Medical Center (Year 20 Exam), N01-HC-45204 from the National Heart, Lung and Blood Institute. This material is the result of work supported with resources and the use of facilities at the--------Veterans Affairs Medical Center. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors have nothing to disclose.
Contributor Information
Helena H Laroche, Department of Internal Medicine and Pediatrics, University of Iowa, Iowa City, Iowa; Comprehensive Access & Delivery Research and Evaluation (CADRE), Iowa City VA Medical Center, Iowa City, Iowa.
Robert B Wallace, Department of Epidemiology, University of Iowa, Iowa City, Iowa.
Linda Snetselaar, Department of Epidemiology, University of Iowa, Iowa City, Iowa.
Stephen L Hillis, Department of Biostatistics, University of Iowa, Iowa City, Iowa; Comprehensive Access & Delivery Research and Evaluation (CADRE), Iowa City VA Medical Center, Iowa City, Iowa.
Xueya Cai, Previous: Department of Internal Medicine, University of Iowa, Iowa City, Iowa; Current: Department of Biostatistics and Computational Biology, University of Rochester School of Medicine and Dentistry, Rochester, New York.
Lyn M Steffen, Division of Epidemiology and Community Health, University of Minnesota School of Public Health, Minneapolis, Minnesota.
References
- 1.O’Dougherty M, Story M, Stang J. Observations of parent-child co-shoppers in supermarkets: children’s involvement in food selections, parental yielding, and refusal strategies. J Nutr Educ Behav. 2006;38(3):183–188. doi: 10.1016/j.jneb.2005.11.034. 5/2006. [DOI] [PubMed] [Google Scholar]
- 2.Jabs J, Devine CM, Bisogni CA, Farrell TJ, Jastran M, Wethington E. Trying to find the quickest way: Employed mothers’ constructions of time for food. J Nutr Educ Behav. 2007;39:18–25. doi: 10.1016/j.jneb.2006.08.011. 2007. [DOI] [PubMed] [Google Scholar]
- 3.Laroche HH, Hofer TP, Davis MM. Adult fat intake associated with the presence of children in households: findings from NHANES III. Journal of the American Board of Family Medicine. 2007;20(1):9–15. doi: 10.3122/jabfm.2007.01.060085. 1/2007. [DOI] [PubMed] [Google Scholar]
- 4.Emmons L, Hayes M. Accuracy of 24-hr. recalls of young children. J Am Diet Assoc. 1973;62(4):409–415. 4/1973. [PubMed] [Google Scholar]
- 5.Laroche HH, Wallace RB, Snetselaar L, Hillis SL, Steffen LM. Changes in diet behavior when adults become parents. J Acad.Nutr Diet. 2012;112(6):832–839. doi: 10.1016/j.jand.2012.02.024. 6/2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nomaguchi KM, Bianchi SM. Exercise Time: Gender Differences in the Effects of Marriage, Parenthood, and Employment. J Marriage Fam. 2004;66:413–430. 2004 May. [Google Scholar]
- 7.Bellows-Riecken KH, Rhodes RE. A birth of inactivity? A review of physical activity and parenthood. Prev Med. 2008;46(2):99–110. doi: 10.1016/j.ypmed.2007.08.003. 2008. [DOI] [PubMed] [Google Scholar]
- 8.Burton NW, Turrell G. Occupation, hours worked, and leisure-time physical activity. Prev Med. 2000;31(6):673–681. doi: 10.1006/pmed.2000.0763. 12/2000. [DOI] [PubMed] [Google Scholar]
- 9.Berge JM, Larson N, Bauer KW, Neumark-Sztainer D. Are parents of young children practicing healthy nutrition and physical activity behaviors? Pediatrics. 2011;127(5):881–887. doi: 10.1542/peds.2010-3218. 5/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Umberson D, Liu H, Mirowsky J, Reczek C. Parenthood and trajectories of change in body weight over the life course. Soc.Sci.Med. 2011;73(9):1323–1331. doi: 10.1016/j.socscimed.2011.08.014. 11/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Ann.Behav Med. 2003;26(2):149–159. doi: 10.1207/S15324796ABM2602_07. 10/2003. [DOI] [PubMed] [Google Scholar]
- 12.Harris HE, Ellison GT, Clement S. Relative importance of heritable characteristics and lifestyle in the development of maternal obesity. J Epidemiol.Community Health. 1999;53(2):66–74. doi: 10.1136/jech.53.2.66. 2/1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gunderson EP, Murtaugh MA, Lewis CE, Quesenberry CP, West DS, Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J Obes Relat Metab Disord. 2004;28(4):525–535. doi: 10.1038/sj.ijo.0802551. 4/2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gunderson EP, Quesenberry CP, Jr., Lewis CE, et al. Development of overweight associated with childbearing depends on smoking habit: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Obes Res. 2004;12(12):2041–2053. doi: 10.1038/oby.2004.255. 12/2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boardley DJ, Sargent RG, Coker AL, Hussey JR, Sharpe PA. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86(5):834–838. doi: 10.1016/0029-7844(95)00283-W. 11/1995. [DOI] [PubMed] [Google Scholar]
- 16.Weng HH, Bastian LA, Taylor DH, Jr., Moser BK, Ostbye T. Number of children associated with obesity in middle-aged women and men: results from the health and retirement study. J Womens Health (Larchmt.) 2004;13(1):85–91. doi: 10.1089/154099904322836492. 1/2004. [DOI] [PubMed] [Google Scholar]
- 17.Kritz S, Barrett-Connor E, Friedlander NJ. Parenthood and lipid and lipoprotein levels in older men. Ann Epidemiol. 1997;7(4):275–279. doi: 10.1016/s1047-2797(97)00016-1. 5/1997. [DOI] [PubMed] [Google Scholar]
- 18.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. 1988. [DOI] [PubMed] [Google Scholar]
- 19.University of Alabama at Birmingham DoPM Coronary Artery Risk Development in Young Adults (CARDIA) 2007 http://www.cardia.dopm.uab.edu/
- 20.Hilner JE, McDonald A, L VH, et al. Quality control of dietary data collection in the CARDIA study. Control Clin Trials. 1992;13(2):156–169. doi: 10.1016/0197-2456(92)90021-q. 4/1992. [DOI] [PubMed] [Google Scholar]
- 21.McDonald A, Van HL, Slattery M, et al. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc. 1991;91(9):1104–1112. 9/1991. [PubMed] [Google Scholar]
- 22.Liu K, Slattery M, Jacobs D, Jr., et al. A study of the reliability and comparative validity of the cardia dietary history. Ethn.Dis. 1994;4(1):15–27. 1994. [PubMed] [Google Scholar]
- 23.Lewis CE, Smith DE, Wallace DD, Williams OD, Bild DE, Jacobs DR., Jr. Seven-year trends in body weight and associations with lifestyle and behavioral characteristics in black and white young adults: the CARDIA study. Am J Public Health. 1997;87(4):635–642. doi: 10.2105/ajph.87.4.635. 4/1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs D, Jr., Hahn L, Haskell W, Price P, Sidney S. Validity and Reliability of Short Physical Activity History: Cardia and the Minnesota Heart Health Program. Journal of Cardiopulmonary Rehabilitation. 1989;9:448–459. doi: 10.1097/00008483-198911000-00003. 1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hankinson AL, Daviglus ML, Bouchard C, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304(23):2603–2610. doi: 10.1001/jama.2010.1843. 12/15/2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. 1976. [Google Scholar]
- 27.Little RJA. Modeling the drop-out mechanism in repeated-measures studies. Journal of the American Statistical Association. 1995;90:1112–1121. 1995. [Google Scholar]
- 28.Verbeke W, De B. I. Dietary behaviour of pregnant versus non-pregnant women. Appetite. 2007;48(1):78–86. doi: 10.1016/j.appet.2006.07.078. 1/2007. [DOI] [PubMed] [Google Scholar]
- 29.The NS, Gordon-Larsen P. Entry into romantic partnership is associated with obesity. Obesity (Silver.Spring.) 2009;17(7):1441–1447. doi: 10.1038/oby.2009.97. 7/2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Averett SL, Sikora A, Argys LM. For better or worse: relationship status and body mass index. Econ.Hum.Biol. 2008;6(3):330–349. doi: 10.1016/j.ehb.2008.07.003. 12/2008. [DOI] [PubMed] [Google Scholar]
- 31.Sobal J, Hanson KL, Frongillo EA. Gender, ethnicity, marital status, and body weight in the United States. Obesity (Silver.Spring.) 2009;17(12):2223–2231. doi: 10.1038/oby.2009.64. 12/2009. [DOI] [PubMed] [Google Scholar]
- 32.Eng PM, Kawachi I, Fitzmaurice G, Rimm EB. Effects of marital transitions on changes in dietary and other health behaviours in US male health professionals. J Epidemiol Community Health. 2005;59:56–62. doi: 10.1136/jech.2004.020073. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lois K, Kumar S, Williams N, Birrell L. Can self-reported height and weight be relied upon? Occupational medicine (Oxford, England) 2011 Dec;61(8):590–592. doi: 10.1093/occmed/kqr140. [DOI] [PubMed] [Google Scholar]
- 34.Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007 Jul;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 35.Ball K, Crawford D. Socioeconomic status and weight change in adults: a review. Soc Sci Med. 2005;60(9):1987–2010. doi: 10.1016/j.socscimed.2004.08.056. 5/2005. [DOI] [PubMed] [Google Scholar]
- 36.Laroche HH, Wallace RB, Snetselaar L, Hillis SL, Steffen LM. Changes in diet behavior when adults become parents. Journal of the Academy of Nutrition and Dietetics. 2012 Jun;112(6):832–839. doi: 10.1016/j.jand.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]