Abstract
Objectives
Low physician density, undercapacitated laboratory infrastructures, and limited resources are major limitations to the development and implementation of widely accessible cervical cancer prevention programs in sub-Saharan Africa.
Materials and Methods
We developed a system operated by nonphysician health providers that used widely available and affordable communication technology to create locally adaptable and sustainable public sector cervical cancer prevention program in Zambia, one of the world’s poorest countries.
Results
Nurses were trained to perform visual inspection with acetic acid aided by digital cervicography using predefined criteria. Electronic digital images (cervigrams) were reviewed with patients, and distance consultation was sought as necessary. Same-visit cryotherapy or referral for further evaluation by a gynecologist was offered. The Zambian system of “electronic cervical cancer control” bypasses many of the historic barriers to the delivery of preventive health care to women in low-resource environments while facilitating monitoring, evaluation, and continued education of primary health care providers, patient education, and medical records documentation.
Conclusions
The electronic cervical cancer control system uses appropriate technology to bridge the gap between screening and diagnosis, thereby facilitating the conduct of “screen-and-treat” programs. The inherent flexibility of the system lends itself to the integration with future infrastructures using rapid molecular human papillomavirus–based screening approaches and wireless telemedicine communications.
Keywords: cervical cancer, visual inspection, telemedicine, developing countries, Zambia
Cervical cancer continues to be the leading cause of cancer-related morbidity and mortality among women worldwide, especially in developing countries [1]. Access to cytology-based screening, referral colposcopy, and any form of treatment services is severely limited in these settings owing to the lack of trained manpower, paucity of financial resources, competing public health priorities, and poor awareness about preventive health [2]. A number of initiatives have heralded alternative approaches to cervical cancer prevention in the past decade. Utilization of single-visit “see-and-treat” services (with visual inspection after application of acetic acid [VIA]) with immediate cryotherapy for eligible lesions has been demonstrated as a practical and efficacious method in settings where access to screening services is extremely limited [3, 4]. However, research on better adaptations for VIA continue, including an attempt to bridge the divide between screening and diagnostic (e.g., colposcopy) methods in the developing world [5].
CERVICOGRAPHY
Cervicography is a method of cervical cancer screening that attempts to reproduce colposcopy, photographically. Since its original description by Adolf Stafl [6, 7], it has undergone significant development as a result of telecommunications innovations, for example, digital and wireless technology. Originally, the analog technology involved capturing cervical photographs on a 35-mm film using a special camera and light source. Rolls of film were then sent, by ground mail, to certified expert colposcopists for interpretation. Although fairly reliable in detecting cervical cancer precursors, the procedure was time-consuming and cumbersome, and up to 15% of patients had to be recalled to have pictures retaken because of technical errors [8–14]. Adapting cervicography to the digital age, a commercial brand digital camera outfitted with macro lens and automatic flash is connected to a television monitor on which magnified real-time images can be easily viewed [15]. This modern form of “digital cervicography” has been evaluated in research settings in low-resource environments and found to have acceptable performance characteristics when compared with cytology, VIA, and colposcopy [16–19]. In fact, VIA plus digital cervicography compared with VIA alone can improve the decision-making process, thus becoming a valid adjunctive screening test for cervical cancer in low-resource settings [20, 21].
ZAMBIAN ADAPTATION OF DIGITAL CERVICOGRAPHY
Since January 2006, we have implemented a see-and-treat cervical cancer prevention program in Zambia [22]. Nurses have been the backbone of providing these services in the 18 clinics currently operating in the program along with a single tertiary hospital–based referral center. An early review of programmatic processes and outcomes uncovered 3 major deficiencies regarding the clinical activities of nurses: (i) the lack of a system to monitor their decisions because they independently functioned in clinics, (ii) the absence of a reliable communication method for them to rapidly access expert advice, as necessary, for confirming their test results and making treatment decisions, and (iii) a framework for their continued education. We used widely available and affordable mobile technology to design and implement a system—dubbed “electronic cervical cancer control” (eC3)—that addressed these problems and also facilitated patient education and medical records documentation. In this article, we discuss the components of the system and its operationalization.
Our program development and screening approach has been previously described [22, 23]. After application of 5% acetic acid, nurses perform naked-eye evaluation of the cervix (VIA) followed by digital cervicography (photography) using a commercial brand (“off-the-shelf”) digital camera. Once obtained, real-time digital images are displayed and enlarged on a bedside television monitor for detailed examination of abnormal surface morphology and discussion of findings with patients. Digital images (cervigrams) are uploaded to a laptop computer in the clinic where they can be (i) electronically transmitted to off-site experts for rapid distance consultation (telecervicography), when necessary, (ii) batched and later routinely reviewed to form the basis of a rigorous ongoing continuing education and quality control program, and (iii) stored with the patient’s electronic medical record. Patients eligible for cryotherapy are offered same-day treatment, whereas those requiring histologic assessment are referred to the gynecologic cancer prevention unit at the University Teaching Hospital of Zambia for biopsy or loop electrosurgical excision procedure. Digital cervical images of all referrals are transmitted to a web site that can be accessed by consultants at the time of patient visits.
TRAINING AND QUALITY CONTROL
All nurses (already trained in VIA and cryotherapy) participate in a 1-week training course in basic computer operation including Microsoft Outlook, Excel, Internet, and Word (Microsoft Corporation, Redmond, WA) and downsizing and electronically transmitting cervigrams. The course is led by an expert computer analyst and consists of didactic and clinically mentored instruction. In a separate training on digital photography, nurses are also taught the basic theory of how a camera works, principles of camera operations and care, use of appropriate accessories, and the mechanics and subtleties of digital photography of the cervix (Tables 1 and 2). Initially, trainees observe an experienced provider take 5 digital photographs of the cervix, after which they are observed taking pictures under the mentorship of the experienced provider until high-quality images are obtained without guidance. The duration of digital photography training is determined individually but averages 2 weeks. During the actual program implementation, weekly monitoring and evaluation meetings are held and attended by all nurses and consultants. All digital photographs taken by nurses during the previous week, and their clinical decisions, are reviewed and discussed. Nurses unable to attend the meetings instead transmit their images to consultants before the meetings, accompanied by interpretations and treatment decisions. All digital photographs are stored on the hard drives of the computer of each clinic and maintained as part of the permanent patient record. Owing to the size and number of files being stored on laptops, nurses are instructed to select the one best image, compress it using commercially available image manipulation software (e.g., Genius Picture Resize, Lonking Software, LLC, web site: http://www.lonking.com), and tag it with the patient’s identification number. Establishing a standardized file storage system allows a nurse who is covering for another in a different clinic to find any photograph needed for reference as well as to appropriately store new images. Copies of all photographs taken in the clinic are saved on a server at the University Teaching Hospital of Zambia for backup.
Table 1.
Materials Required for Digital Cervicography
| Particular | Average cost per unit |
|---|---|
| Digital camera [e.g. Olympus SP-510UZ™; 7.1 megapixel with 10x Optical Zoom & flash, or Canon Powershot™ S5IS Digital Camera; 8.0 megapixels; 12x optical zoom with automatic flash] |
$350 |
| 58 mm Close-up Macroconverter Lens 500D with Lens Adapter tube | $100 |
| Memory card(s) for cameras | $50 |
| Charger [e.g. Energizer Rechargeable Compact Charger 2500 (NiMH/NiCd)] | $20 |
| Rechargeable AA batteries – 8 or 12 | $2 |
| Television or computer monitor (preferably at least 15 inches) | $150 |
| Cable for connecting camera to television or computer (usually included with camera) | $5 |
| PC Tuner card (if using camera with computer rather than television) | $100 |
| Extension cord/surge protectors | $5 |
| Laptop computers with external mouse | $2000 |
| Software for integrating photographs into patient’s electronic medical records (E.g. DBPix™: redistribution license) | $350 |
| Picture resizing software (e.g. Genius Picture Resize™: unlimited business license) | $40 |
| Internet source to share images and data electronically (optional) | variable costs |
Table 2.
Digital Photography Mechanics
| Step Number | Action to be performed |
|---|---|
| 1 | Position the goose-necked halogen floor lamp to maximize illumination of the cervix |
| 2 | Wash the cervix with 5% acetic acid and wait 2–3 minutes before taking a photograph |
| 3 | While waiting to capture the image, make sure camera batteries are fully charged. If they are not fully charged, replace them. Turn on the automatic flash |
| 4 | Press power button to turn on camera. Put setting on “automatic.” By placing the setting on “automatic” camera adjusts the exposure time and performs automatic focusing |
| 5 | Visualize the cervix in the center of the field of the camera’s viewfinder, then pull the zoom lever to the right, zooming in on the cervix until only the cervix is visible, excluding the vulva, lower vagina and handle of the speculum from the field of view |
| 6 | Hold the shutter release button halfway down to bring the cervix into sharp focus while simultaneously viewing the picture on the monitor of the camera LCD or television. Focus optimization may additionally require moving the camera forward (towards the cervix) or backward (away from the cervix), while still holding the shutter release button halfway down |
| 7 | Once the cervix is sharply focused, tilt the camera lens up (towards the ceiling) or down (away from the ceiling) to minimize shadow. When the colored rectangle comes into view on the view finder the picture is in focus and the shutter should be fully depressed to take the photograph |
| 8 | Move the mode dial to view the picture |
CONTINUOUS REFINEMENT FOR ENHANCED DIGITAL IMAGING, PATIENT EDUCATION, AND DISTANCE CONSULTATION
Thanks to the high-magnification factor of the camera’s lens and the high-sensor resolution, our images yield a high-pixel density across the entire examination area (Figure 1). This allows for highly detailed magnified viewing far beyond life size when displayed on a larger monitor such as a laptop or a television screen. This facilitates enhanced inspection of surface morphology of the cervix, which can be of assistance in evaluating various aspects of abnormal lesions, e.g., sharpness of borders, degree of extension into the endocervical canal, and the presence or absence of abnormal vasculature (mosaicism, punctuations, atypical vessels). Accurate determination of these features is important in decisions about offering cryotherapy or referral for punch biopsy or loop electrosurgical excision procedure. Enhanced digital images can also be used to educate patients regarding the anatomy and physiology of the cervix, the natural history of cancer, and the need for further evaluation or treatment. After uploading pictures from the camera to the laptop computer, those needing immediate expert review are compressed for electronic transmission/rapid distance consultation and downsized via commercially available software (e.g., Genius Picture Resize) to prepare for rapid transmission for distance consultation.
Figure 1.
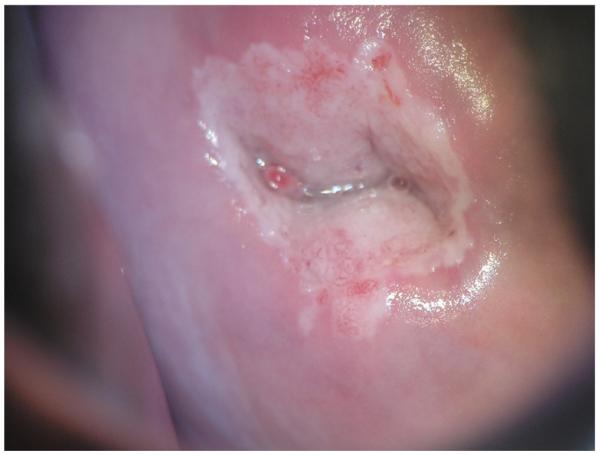
Ideal image. The entire cervix can be visualized without any shadow and only minimal glare.
The primary communication modality that nurses and consultants use is e-mail. An e-mail address has been set to be a distribution list. Once an e-mail is sent to it, copies are sent to all participating consultant physicians, enabling all involved to get a copy of the feedback. Photographs can also be put into an attached word processing document and be annotated. Otherwise, questions can be asked by the clinic nurse, aided by partitioning the cervix into 4 quadrants or treating it as if it is the face on a clock, with 12 o’clock representing the center of the anterior lip and 6 o’clock representing the center of the posterior lip. E-mail communication provides a consistent transcript of all communications while being tolerant of intermittent connectivity. For security reasons, only relevant clinical information related to the photograph is ever discussed or transcribed on e-mail messages. No patient identifiers are transmitted over e-mail.
An enhanced web-based solution has also been implemented for remote clinics. Upon uploading a camera’s images to the nurse’s computer, they can be immediately transmitted to the secure consultation web site. This consultation web site has been programmed using the open-source software Python (Python Software Foundation, Hampton, NH) and is currently hosted on one of the servers of the intranet within the gynecologic oncology prevention unit (referral center). Nurses access the web site in the outlying clinics using the Internet protocol address of the server as the uniform resource locator address. When the nurses upload a cervigram as well as pertinent patient details such as HIV status, features of lesions seen, and so on, a text message (short message service) is automatically sent to all consultants on call notifying them to review the image. Any consultant may respond, but the “on-call” consultant for the day is immediately responsible. The consultant sends a short message service back to the nurse after the consultation request has been answered. If necessary, the two of them can discuss the photographs over cell phoneswhile viewing them simultaneously on their individual computer monitors. Each web site user has unique login credentials. One interface exists for physicians, which allows them to view activities for all nurses; another interface exists for nurses restricting them to viewing their own profiles and has limited features that, for instance, cannot allow them to delete the physicians’ comments. By using these mobile technologies, every attempt is made to respond to distance consultation requests while patients are still in the clinic and, in some cases, yet on the examination table.
LIMITATIONS AND CHALLENGES
We have faced several limitations and challenges, some of which include the following: (i) photographs are two-dimensional rather than stereoscopic, possibly affecting the operator’s ability to fully appreciate lesion depth (e.g., ulcers), (ii) the ability of consultants to make appropriate decisions is limited by the quality of the image, (iii) cameras fail and, in low-resource environments, will usually need to be sent outside the country for repair, and (iv) digital cervicography is only a screening test and, to be effective, must be incorporated within a system where its results can be monitored, evaluated, assessed by experts, and linked with appropriate treatment when necessary. In addition, as a screening modality, cervicography is rater-dependent, thus suffers from the traditional shortcomings of a subjective visual screening test. Common problems encountered during the process of learning digital photography include inadequate zooming (Figure 2), obstructed views of the cervix (Figure 3), batteries not being fully charged (Figure 4), and improper lighting (Figure 5). Troubleshooting guidelines were developed (Table 3).
Figure 2.

Inadequate use of magnification. The zoom feature was not used properly, resulting in too much of the speculum and the vaginal walls being included in the cervigram.
Figure 3.

Obstructed view of the cervix. To optimize visualization, the largest available speculum should be used. If the vaginal walls continue to obstruct the view, a vaginal wall retractor should be used. In the absence of a vaginal wall retractor, place a condom with the tip cut off over the speculum before insertion. As the speculum is opened, the condom will help retract the vaginal walls.
Figure 4.

Orange coloring that can occur on digital cervigrams when camera batteries are low and need recharging.
Figure 5.

Inadequate lighting leading to shadows. This is an inadequate digital cervigram. The entire cervix cannot be visualized, and shadow obstructs the view. A flashlight (torch) or spotlight should be used to increase lighting, or the floor lamp should be readjusted.
Table 3.
Digital Cervicography Trouble-Shooting
| Description | Problem | Trouble shooting |
|---|---|---|
| Picture appears dark or has a shadow |
Inadequate lighting | Redirect floor lamp onto cervix, reposition speculum and make sure camera flash is turned on. If shadow is on anterior tilt lens of camera towards the ceiling; if shadow is on posterior cervix tilt lens towards the floor |
| Image is hazy or blurred | Inadequate focus | Check that autofocus is selected. Depress the button halfway to allow automatic focus. Once focus is optimized, hold the camera steady while fully depressing shutter release button |
| Image appears orange | Batteries are not fully charged |
Recharge or replace |
| Vaginal walls obstructing view of cervix |
Speculum is too small or not fully open. |
Use a larger speculum and open as wide as possible. If speculum is large and fully open and view is still obstructed, use a vaginal wall retractor. If no vaginal wall retractor is available, cut off the tip of a condom and place residual condom over speculum then reinsert in vagina |
| Too much speculum in image |
Inadequate zoom | Move camera closer to the cervix before capturing the image |
CONCLUSIONS
We operationalized a public-sector cervical cancer prevention program in Zambia using trained nurses and widely available and affordable technology (digital camera, laptop computer, television, cell phone, and Internet) as core infrastructural components. The design of our telecommunications matrix facilitated monitoring and evaluation of nurses’ performance measures, rapid access to off-site experts, continued education of nurses, as well as patient education and medical records documentation. Our system—electronic cervical cancer control (eC3)—provides the flexibility to compensate for the manpower shortages and medical infrastructure underdevelopment frequently found in low-resource nations, such as Zambia. Our experiences in the establishment and maintenance of this system are presently being used to train providers and public health program managers from other low-resource settings, modified to fit their particular environments. Efforts are underway to develop rapid human papillomavirus–based screening methods that will significantly improve the accuracy of cervical cancer screening [24, 25]. However, just as with cytology-based screening, women testing human papillomavirus–positive will require visual assessment to determine whether there is an underlying neoplastic lesion and the type of treatment required. The Zambian cervical cancer prevention system (eC3) provides a low-cost and locally appropriate platform for the integration of future HPV-based cervical cancer screening protocols.
Acknowledgments
This study was supported by the President’s Emergency Plan for AIDS Relief grant through the Elizabeth Glaser Pediatric AIDS Foundation from the Centers for Disease Control and Prevention Global AIDS Program with additional support from the Fogarty International Clinical Research Scholars Program and Vanderbilt–CIDRZ AIDS International Training and Research Program (National Institutes of Health grants R24TW007988 and D43TW001035).
REFERENCES
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Sankaranarayanan R, Gaffikin L, Jacob M, Sellors J, Robles S. A critical assessment of screening methods for cervical neoplasia. Int J Gynaecol Obstet. 2005;89:S4–12. doi: 10.1016/j.ijgo.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Sankaranarayanan R, Esmy PO, Rajkumar R, Muwonge R, Swaminathan R, Shanthakumari S, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster-randomised trial. Lancet. 2007;370:398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- 4.Denny L, Kuhn L, De Souza M, Pollack AE, Dupree W, Wright TC., Jr Screen-and-treat approaches for cervical cancer prevention in low-resource settings: a randomized controlled trial. JAMA. 2005;294:2173–81. doi: 10.1001/jama.294.17.2173. [DOI] [PubMed] [Google Scholar]
- 5.Denny L, Kuhn L, Pollack A, Wainwright H, Wright TC., Jr Evaluation of alternative methods of cervical cancer screening for resource-poor settings. Cancer. 2000;89:826–33. doi: 10.1002/1097-0142(20000815)89:4<826::aid-cncr15>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 6.Stafl A. Cervicography: a new method for cervical cancer detection. Am J Obstet Gynecol. 1981;139:815–25. doi: 10.1016/0002-9378(81)90549-4. [DOI] [PubMed] [Google Scholar]
- 7.Stafl A. Cervicography. Clin Obstet Gynecol. 1983;26:1007–16. doi: 10.1097/00003081-198312000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Gundersen JH, Schauberger CW, Rowe NR. The Papanicolaou smear and the cervigram. A preliminary report. J Reprod Med. 1988;33:46–8. [PubMed] [Google Scholar]
- 9.Spitzer M, Krumholz BA, Chernys AE, Seltzer V, Lightman AR. Comparative utility of repeat Papanicolaou smears, cervicography, and colposcopy in the evaluation of atypical Papanicolaou smears. Obstet Gynecol. 1987;69:731–5. [PubMed] [Google Scholar]
- 10.McKinnon KJ, Ford RM, Hunter JC. Comparison of cytology and cervicography in screening a high risk Australian population for cervical human papillomavirus and cervical intraepithelial neoplasia. Aust N Z J Obstet Gynaecol. 1993;33:176–9. doi: 10.1111/j.1479-828x.1993.tb02387.x. [DOI] [PubMed] [Google Scholar]
- 11.Solomon D, Wied GL. Cervicography: an assessment. J Reprod Med. 1989;34:321–3. [PubMed] [Google Scholar]
- 12.Sellors JW, Nieminen P, Vesterinen E, Paavonen J. Observer variability in the scoring of colpophotographs. Obstet Gynecol. 1990;76:1006–8. [PubMed] [Google Scholar]
- 13.Coibion M, Autier P, Vandam P, Delobelle A, Huet F, Hertens D, et al. Is there a role for cervicography in the detection of premalignant lesions of the cervix uteri? Br J Cancer. 1994;70:125–8. doi: 10.1038/bjc.1994.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cronjé HS, Cooreman BF, Beyer E, Bam RH, Middlecote BD, Divall PD. Screening for cervical neoplasia in a developing country utilizing cytology, cervicography and the acetic acid test. Int J Gynaecol Obstet. 2001;72:151–7. doi: 10.1016/s0020-7292(00)00382-9. [DOI] [PubMed] [Google Scholar]
- 15.Schneider DL, Burke L, Wright TC, Spitzer M, Chatterjee N, Wacholder S, et al. Can cervicography be improved? An evaluation with arbitrated cervicography interpretations. Am J Obstet Gynecol. 2002;187:15–23. doi: 10.1067/mob.2002.122848. [DOI] [PubMed] [Google Scholar]
- 16.Bomfim-Hyppólito S, Franco ES, Franco RG, de Albuquerque CM, Nunes GC. Cervicography as an adjunctive test to visual inspection with acetic acid in cervical cancer detection screening. Int J Gynaecol Obstet. 2006;92:58–63. doi: 10.1016/j.ijgo.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Cremer M, Jamshidi RM, Muderspach L, Tsao-Wei D, Felix JC, Blumenthal PD. Digital camera assessment for detection of cervical intraepithelial neoplasia in rural El Salvador. Int J Gynaecol Obstet. 2005;91:42–6. doi: 10.1016/j.ijgo.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 18.Chen ZP, Chen HM, Lee TT. Use of compact digital cervicography: an adjuvant screening tool for precancerous cervical lesions. Taiwan J Obstet Gynecol. 2008;47:187–91. doi: 10.1016/S1028-4559(08)60078-9. [DOI] [PubMed] [Google Scholar]
- 19.Moscicki AB, Durako SJ, Ma Y, Darragh T, Vermund SH. Utility of cervicography in HIV-infected and uninfected adolescents. J Adolesc Health. 2003;32:204–13. doi: 10.1016/s1054-139x(02)00461-5. [DOI] [PubMed] [Google Scholar]
- 20.Cronjé HS, Parham GP, Cooreman BF, de Beer A, Divall P, Bam RH. A comparison of four screening methods for cervical neoplasia in a developing country. Am J Obstet Gynecol. 2003;188:395–400. doi: 10.1067/mob.2003.153. [DOI] [PubMed] [Google Scholar]
- 21.Howard M, Sellors JW, Lytwyn A, Roth P, Mahony JB. Combining human papillomavirus testing or cervicography with cytology to detect cervical neoplasia. Arch Pathol Lab Med. 2004;128:1257–62. doi: 10.5858/2004-128-1257-CHPTOC. [DOI] [PubMed] [Google Scholar]
- 22.Mwanahamuntu MH, Sahasrabuddhe VV, Pfaendler KS, Mudenda V, Hicks ML, Vermund SH, et al. Implementation of ‘see-and-treat’ cervical cancer prevention services linked to HIV care in Zambia. AIDS. 2009;23:N1–5. doi: 10.1097/QAD.0b013e3283236e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfaendler KS, Mwanahamuntu MH, Sahasrabuddhe VV, Mudenda V, Stringer JS, Parham GP. Management of cryotherapy-ineligible women in a “screen-and-treat” cervical cancer prevention program targeting HIV-infected women in Zambia: lessons from the field. Gynecol Oncol. 2008;110:402–7. doi: 10.1016/j.ygyno.2008.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiao YL, Sellors JW, Eder PS, Bao YP, Lim JM, Zhao FH, et al. A new HPV-DNA test for cervical-cancer screening in developing regions: a cross-sectional study of clinical accuracy in rural China. Lancet Oncol. 2008;9:929–36. doi: 10.1016/S1470-2045(08)70210-9. [DOI] [PubMed] [Google Scholar]
- 25.Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385–94. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]


