Abstract
Melanocytoma of the optic disc is a benign melanocytic tumour that rarely causes visual impairment. We report a rare case of choroidal neovascularization (CNV) in association with optic disc melanocytoma and its response to intravitreal injection of the anti-vascular endothelial growth factor (VEGF), bevacizumab. The choroidal neovascular membrane regressed following a single intravitreal bevacizumab injection with formation of a scar. CNV associated with optic disc melanocytoma is rare. Intravitreal anti-VEGF treatment may be an effective treatment for CNV associated with optic disc melanocytoma.
Keywords: Anti-VEGF, Bevacizumab, Choroidal neovascular membrane, Melanocytoma, Optic disc
Introduction
Choroidal neovascularization (CNV) consists of growth of the fibrovascular tissue from the choriocapillaris, through defects in Bruch’s membrane into subretinal pigment epithelial space and eventually, into subretinal space. Common causes of CNV include age-related macular degeneration (ARMD), high myopia, angioid streaks, choroidal rupture, posterior uveitis, histoplasmosis, and birdshot chorioretinopathy.1 CNV is an uncommon complication of choroidal nevus, melanoma, or melanocytoma.2,3 Anti-vascular endothelial growth factor (VEGF) compounds have been shown to have a beneficial role in treating CNV. In this case report, we present the treatment of a rare case of CNV associated with optic disc melanocytoma.
Case report
A 45-year-old male patient presented with decreased vision in the right eye for 3 weeks. Best corrected visual acuity (BCVA) was 20/160 in the right eye and 20/20 in the left eye. Slit lamp examination was normal and intraocular pressure (IOP) was 16 mmHg in both eyes. Amsler grid testing indicated a central sparing relative scotoma in the temporal visual field of the right eye. Ophthalmoscopy indicated an optic disc melanocytoma with a yellowish, elevated, well defined membrane overlying the papillomacular bundle surrounded by haemorrhage (Fig. 1). Fundus examination of the left eye was normal with no myopic findings bilaterally.
Figure 1.

Melanocytoma of the optic disc with a yellowish, elevated, well defined membrane overlying the papillomacular bundle surrounded by haemorrhage in the right eye.
Fundus fluorescein angiography (FFA) of the right eye revealed a lacy pattern in the early arterial phase, which increased in intensity and showed leakage in the late arteriovenous phase (Fig. 2). It was surrounded by a haemorrhage that blocked fluorescence (Fig. 3A). Optical coherence tomography (OCT) of the right eye revealed serous detachment of the neurosensory retina and retinal thickness of 515 micron in this area (Fig. 3B).
Figure 2.
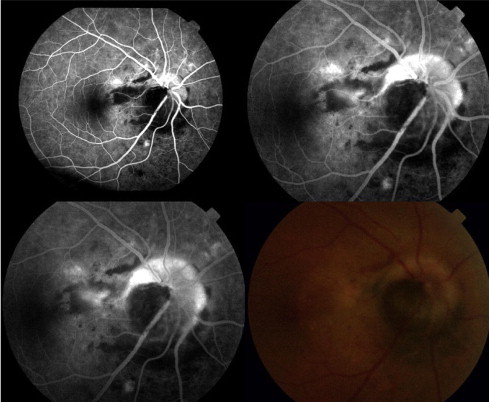
Fluorescein angiogram of the right eye showing a lacy pattern in the early arterial phase, which increased in intensity and showed leakage in the late arteriovenous phase.
Figure 3.
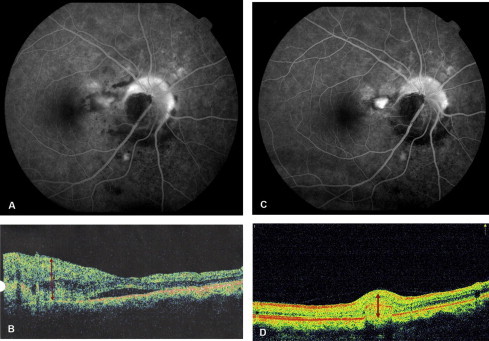
(A) Fluorescein angiogram of the right eye, pre-injection, showing increased intensity and leakage from the CNV in the late arteriovenous phase with an area of blocked fluorescence. (B) Optical coherence tomography of the right eye, pre-injection, showing subretinal fluid with a retinal thickness of 565 microns in the area nasal to the fovea. (C) Fluorescein angiogram of the RE one month postinjection showing only staining of the membrane with surrounding window defects. (D) OCT of right eye one month post-injection showing hyper-reflectivity corresponding to the scar with no residual fluid and a thickness of 290 microns in the corresponding area.
The patient was diagnosed as a case of melanocytoma of optic disc with classic juxtafoveal CNV in the right eye. The patient underwent one injection of intravitreal bevacizumab 1.25 mg in 0.05 ml.
FFA one month after treatment, showed staining and no leakage consistent with scarring (Fig. 3C). OCT showed resolution of the serous detachment with retinal thickness of 290 micron in the corresponding area (Fig. 3D). One year after treatment, there has been no recurrence of the CNV and vision in the right eye is 20/30.
Discussion
Melanocytomas appear as grey to jet-black elevated lesions and usually do not exceed one disc diameter in size on ophthalmoscopy. However, one report presented a lesion that was six disc diameters in size.4 Melanocytomas are usually asymptomatic. CNV is rarely associated with melanocytoma and can lead to severe visual loss. This lesion can be differentiated from malignant transformation by the constant size of the tumour.5 Inflammation or necrosis2 is known to occur in melanocytoma and can induce rupture of Bruch’s membrane and choroidal neovascularization.
Anti-VEGF compounds are promising treatment modalities for a number of retinal lesions. Bevacizumab is an antibody that binds to the VEGF with a direct angiostatic effect. Good visual outcomes have been reported with intravitreal bevacizumab for CNV related to ARMD,6 pathological myopia,7 inflammatory and idiopathic membranes.8 Beneficial outcomes with intravitreal bevacizumab for a case of melanocytoma-associated CNV have been previously reported by Kamisasanuk and colleagues.9 Kamisasanuk and colleagues’9 report concurs with the outcome in our case. Our patient had regression of CNV with a single injection, and there was a functional improvement. Intravitreal bevacizumab seems to be an effective treatment modality for CNV associated with melanocytoma.
Footnotes

References
- 1.Bressler N.M., Bressler S.B., Fine S.L. Neovascular (exudative) age-related macular degeneration. In: Ryan S.J., editor. Retina. 4th ed. Elsevier Mosby; St. Louis: 2005. pp. 1075–1111. [Google Scholar]
- 2.Rubin M.L. Disciform lesion overlying melanocytoma simulating progression of choroidal melanoma. Trans Am Ophthalmol Soc. 1976;74:282–294. [PMC free article] [PubMed] [Google Scholar]
- 3.Chalam K.V., Shah V.A., Rappaport K.D. Choroidal neovascular membrane associated with melanocytoma of the optic nerve. Retina. 2006;26:703. doi: 10.1097/01.iae.0000236487.26594.de. [DOI] [PubMed] [Google Scholar]
- 4.Joffe L., Shields J.A., Osher R.H., Gass J.D. Clinical and follow-up studies of melanocytomas of the optic disc. Ophthalmology. 1979;86:1067–1078. doi: 10.1016/s0161-6420(79)35421-5. [DOI] [PubMed] [Google Scholar]
- 5.Tran H.V., Bovey E.H., Uffer S., Zografos L. Peripapillary choroidal neovascularization associated with melanocytoma of the optic disc: a clinicopathologic case report. Graefes Arch Clin Exp Ophthalmol. 2006;244(10):1367–1369. doi: 10.1007/s00417-006-0270-1. [DOI] [PubMed] [Google Scholar]
- 6.Avery R.L., Pieramici D.J., Rabena M.D., Castellarin A.A., Nasir M.A., Giust M.J. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113:363–372. doi: 10.1016/j.ophtha.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Chan W.M., Lai T.Y., Liu D.T., Lam D.S. Intravitreal bevacizumab (avastin) for myopic choroidal neovascularization: six-month results of a prospective pilot study. Ophthalmology. 2007;114:2190–2196. doi: 10.1016/j.ophtha.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 8.Chan W.M., Lai T.Y., Liu D.T., Lam D.S. Intravitreal bevacizumab (avastin) for choroidal neovascularization secondary to central serous chorioretinopathy, secondary to punctate inner choriodopathy, or of idiopathic origin. Am J Ophthalmol. 2007;143:977–983. doi: 10.1016/j.ajo.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 9.Kamisasanuk T., Uchino E., Sakamoto T. Choroidal neovascularization of optic disk melanocytoma treated with bevacizumab. Eur J Ophthalmol. 2012;22(3):503–505. doi: 10.5301/ejo.5000060. [DOI] [PubMed] [Google Scholar]


