Abstract
Purpose
This study evaluated the feasibility of a laparoscopic approach in children with generalized peritonitis secondary to perforated appendicitis.
Materials and Methods
We retrospectively analyzed the medical records of patients who underwent laparoscopic appendectomy with drainage for generalized peritonitis secondary to perforated appendicitis at our hospital between September 2001 and April 2012. Laparoscopic outcomes were compared with outcomes of an open method for perforated appendicitis.
Results
Ninety-nine patients underwent laparoscopic appendectomy (LA) for generalized peritonitis from perforated appendicitis, and 87 patients underwent open appendectomy (OA) for perforated appendicitis. Wound infection was more common in the OA group (12.6%) than in the LA group (4.0%; p=0.032). The incidence of intestinal obstruction during long-term follow-up was significantly higher in the OA group (4.6% vs. 0.0% in the LA group; p=0.046). LA was possible in most patients for whom LA was attempted, with a conversion rate of 10.8%. Conversion to OA was affected by the preoperative duration of symptoms and the occurrence of intraoperative complications.
Conclusion
LA is feasible for use in children with generalized peritonitis from perforated appendicitis, with reasonable open conversion and perioperative complication rates comparable to those of the OA group.
Keywords: Appendicitis, peritonitis, laparoscopy, children
INTRODUCTION
Acute appendicitis in young children is commonly accompanied by perforation, resulting in a significant increase in morbidity.1 Generalized peritonitis secondary to perforated appendicitis is a challenging disease in children because of its systemic clinical characteristics and substantially increased morbidity. Although laparoscopic appendectomy (LA) is commonly performed in children with appendicitis, laparoscopic approaches for treating generalized peritonitis have some difficulties. These difficulties include a limited view due to severe adhesions from generalized peritonitis and confined space of the small abdominal cavity of children. Moreover, the use of LA for complicated appendicitis is controversial because of the high incidence of intra-abdominal abscess.2,3
In this study, we reviewed our experience, which used a laparoscopic approach for generalized peritonitis secondary to perforated appendicitis in children, to evaluate its feasibility. The results of LA for generalized peritonitis from perforated appendicitis were compared to those of an open approach for perforated appendicitis.
MATERIALS AND METHODS
We retrospectively analyzed the medical records of patients who underwent LA with drainage for generalized peritonitis secondary to acute perforated appendicitis at our hospital between September 2001 and April 2012. We also reviewed the medical records of patients who underwent open appendectomy (OA) with drainage for perforated appendicitis with localized or generalized peritonitis or periappendiceal abscess at our hospital during the same study period. Demographics, preoperative duration of symptoms, operative findings, operative time, conversion from laparoscopy to open surgery, length of hospital stay, and intraoperative and postoperative complications were reviewed.
The diagnosis of appendicitis was confirmed by typical presentation on physical examination, laboratory findings, and/or ultrasonography or CT. Generalized peritonitis was defined as purulent fluid collection in the entire peritoneal cavity, confirmed by laparoscopic findings, in the LA group. In the OA group, patients with appendiceal perforation and localized or generalized peritonitis or periappendiceal abscess were included to compare laparoscopic outcomes for generalized peritonitis secondary to perforated appendicitis. The patients who had other co-morbidity that was not correlated to appendicitis were excluded. Triple antibiotic therapy (ampicillin or cephalosporin, aminoglycoside, and metronidazole) was used postoperatively in both groups.
LA was performed using three ports: one supra- or infraumbilical port for the camera and two working ports in the left lower quadrant of the abdomen and suprapubic area. After ligation of the appendiceal stump using an endo-loop and removal of the appendix, the entire abdominal cavity was cleaned, including both paracolic gutters, pelvic cavity, perihepatic area, splenic fossa, and intermesenteric space, by thorough and meticulous irrigation with warm saline under the direct view of the laparoscope until the irrigation fluid became clear. Two or three draining catheters were inserted into the pelvic cavity and both paracolic gutters via one suprapubic port site.
OA was performed via a right lower transverse or paramedian incision. Cotton tapes were used to protect the abdominal wall from dirty, contaminated intra-abdominal contents. After appendectomy, dirty materials were removed via sponge stick sweeps and thorough irrigation with warm saline was performed until the drainage fluid became clear. Draining catheters were inserted via another incision into the pelvic cavity or paracolic gutter, depending on the operative findings of peritoneal contamination from the appendiceal perforation.
Categorical parameters were analyzed using the Pearson's chi-squared test or Fisher's exact test. Continuous parameters were analyzed with an independent t-test or Mann-Whitney's U test. Multivariate analyses were performed to define the factors related to open conversion from laparoscopy. Statistical analyses were carried out with SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 indicated statistical significance. The Institutional Review Board of our hospital approved this study (4-2012-0448).
RESULTS
During the study period, 519 patients (73.3%) underwent LA and 189 patients (26.7%) underwent OA at our hospital. Of these, 186 patients (26.3%) were included in this study because they had perforated appendicitis with generalized peritonitis confirmed by laparoscopy or underwent OA with drainage for perforated appendicitis. LA for generalized peritonitis from perforated appendicitis was performed without open conversion in 99 patients. OA for perforated appendicitis was performed in 87 patients, including 12 patients who were converted to the open method.
The clinical characteristics of the two groups are presented in Table 1. The mean age at appendectomy was 8.4±3.6 years (8.3±3.3 years in the LA group vs. 8.4±3.9 years in the OA group; p=0.947). The mean duration of symptoms was 3.8±3.4 days (3.4±2.5 days in the LA group vs. 4.3±4.1 days in the OA group; p=0.074).
Table 1.
Clinical Characteristics of the LA and OA Groups
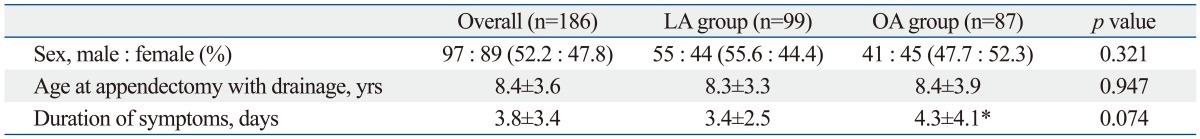
LA, laparoscopic appendectomy; OA, open appendectomy.
*Three patients in whom the duration of symptoms was unavailable were excluded.
In most of the LA group, CT [77.8% (77/99)] and ultrasonography [7.1% (7/99)] were used for diagnosis. Only 15 patients (15.2%) in the LA group underwent surgery after diagnosis by clinical assessment without radiologic evaluation. In the OA group, 48.3% (42/87) of the patients were diagnosed by clinical assessment including physical examination and laboratory findings. CT and ultrasonography were performed in 42.5% (37/87) and 9.2% (8/87) of patients in the OA group, respectively.
Perioperative clinical data are presented in Table 2. During surgery, nine patients (4.8%) had complications. Intraoperative complications were more frequent in the OA group than in the LA group [9.2% (8/87) in the OA group vs. 1.0% (1/99) in the LA group; p=0.013]. However, among the eight patients in the OA group with intraoperative complications, laparoscopic attempts were converted to open procedures in three patients due to these complications (i.e., mesenteric bleeding, serosal tearing with bleeding of the small bowel and cecum, and rupture of the appendiceal stump during laparoscopic ligation). Considering these complications in the patients who underwent open conversion from laparoscopy, there were no significant differences in the rate of intraoperative complications between the two groups [3.9% (4/102) in the LA group vs. 6.0% (5/84) in the OA group; p=0.734]. Other intraoperative complications included serosal tearing of the small bowel in both groups. A larger amount of irrigation fluid was used in the LA group (4.0±2.6 L in the LA group vs. 1.8±1.0 L in the OA group; p=0.019). The operative time was longer in the LA group (114.2±34.0 min) than in the OA group (87.0±63.0 min; p<0.001).
Table 2.
Perioperative Clinical Data in the LA and OA Groups
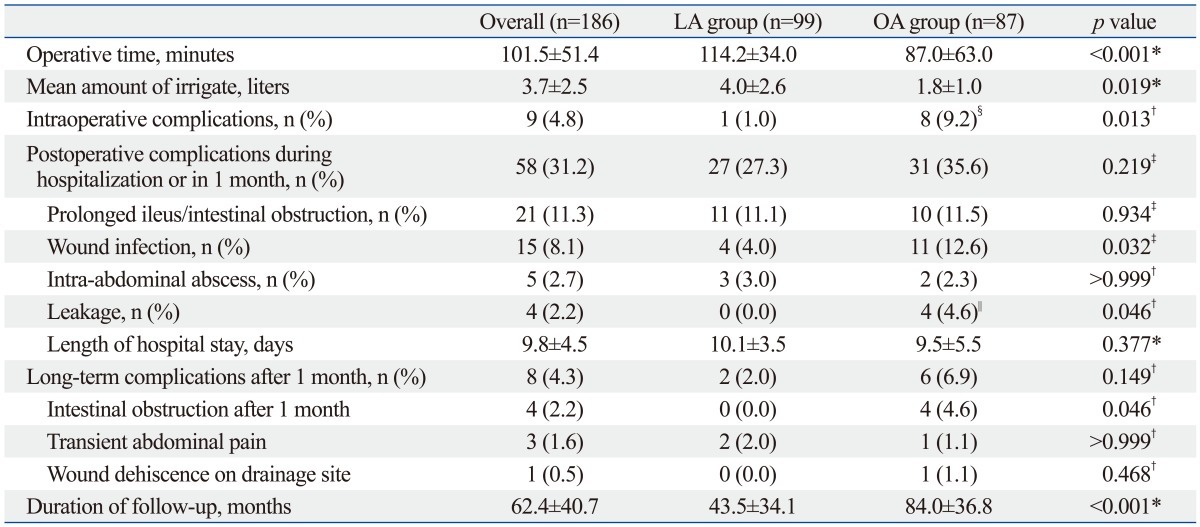
LA, laparoscopic appendectomy; OA, open appendectomy.
*Independent t-test.
†Fisher's exact test.
‡Pearson chi-square test.
§Three patients underwent open conversion from laparoscopy due to intraoperative complications during laparoscopy.
∥Three patients underwent open conversion.
Fifty-eight postoperative complications (31.2%) occurred during hospitalization or within the first month after appendectomy. Those complications included prolonged ileus or intestinal obstruction, wound infection, intra-abdominal abscess, leakage, pleural effusion, voiding difficulty, and drug eruption. Although there were no differences between the two groups in the overall rate of postoperative complications, the rates of wound infection and bowel leakage were higher in the OA group. The incidence of wound infection was higher in OA group even after the exclusion of the converted group in the OA group [4.0% (4/99) in the LA group vs. 14.7% (11/75) in the OA group; p=0.013]. However, initial laparoscopic attempts were converted to an open approach in three of four patients with postoperative leakage. Among the four patients exhibiting postoperative leakage, three patients were treated by conservative management with drainage, total parenteral nutrition, and intravenous antibiotic treatment. Surgery was repeated in only one patient in whom ligation of the appendiceal stump was impossible due to severe inflammation during the initial open-converted surgery.
The incidence of long-term complications after the first month of follow-up did not differ between the two groups. However, the long-term incidence of intestinal obstruction significantly differed between the two groups [0.0% (0/99) in the LA group vs. 4.6% (4/87) in the OA group; p=0.046]. Surgical management was indicated in two of these cases. The mean duration of follow-up was longer in the OA group (84.0±36.8 months) than in the LA group (43.5±34.1 months; p<0.001) because the majority of the OA group underwent surgery in the earlier study period.
Laparoscopic attempts were converted to OAs in 12 patients [10.8% (12/111)] with peritonitis. Severe adhesion, the most common cause of open conversion, was noted in four patients [33.3% (4/12)]. Intraoperative complications, including disruption of the appendiceal stump during laparoscopic ligation, mesenteric bleeding, or serosal tearing of the small bowel, were other causes of open conversion. Among the 12 open conversions in this study, three patients underwent open conversion due to intraoperative complications. In one patient, a pneumoperitoneum could not be made because of a rigid and distended abdominal wall. In another patient with open conversion, laparoscopic instruments could not approach the retrocecal position of the appendiceal base. The cause of open conversion was not specific for three patients, nevertheless, the difficulties of laparoscopic procedures were noted.
Factors associated with the conversion of laparoscopy to an open method are shown in Table 3. Multivariate analyses revealed that the preoperative duration of symptoms and the occurrence of intraoperative complications were associated with open conversion (p=0.033 for the duration of symptoms and p=0.003 for intraoperative complications). The incidence of postoperative complications did not differ between the laparoscopy and conversion groups, excluding a difference in the incidence of leakage [0.0% (0/99) in the laparoscopy group vs. 25.0% (3/12) in the conversion group; p=0.001].
Table 3.
Factors Associated with Conversion of Laparoscopy to an Open Method
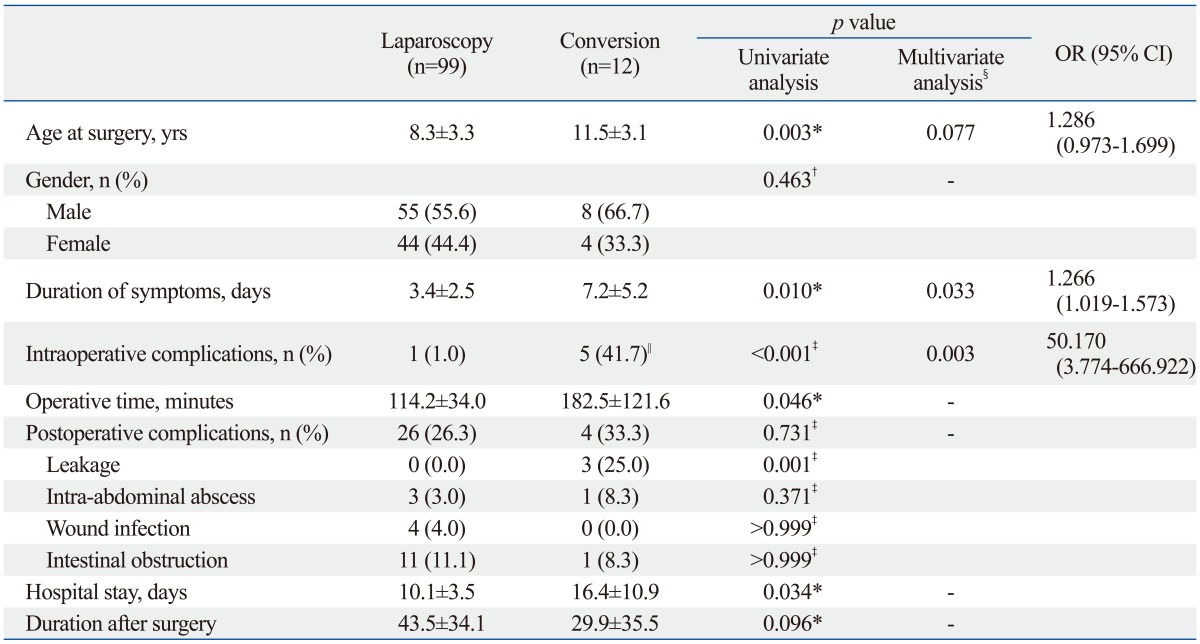
OR, odds ratio; CI, confidence interval.
*Mann-Whitney U test.
†Pearson's chi-square test.
‡Fisher's exact test.
§Binary logistic regression.
∥Two patients had intraoperative complications after open conversion.
DISCUSSION
As a surgical treatment modality for appendicitis, LA permits easy and rapid localization of the appendix (regardless of its location), excellent control of hemostasis, exploration of the entire abdominal cavity, and complete lavage of the contaminated peritoneal cavity. Considering these advantages of laparoscopy, it was believed that the postoperative incidence of intra-abdominal abscess could be reduced using a laparoscopic approach for appendicitis.4 However, the incidence of intra-abdominal abscess in cases of complicated appendicitis was reported to be increased during laparoscopy compared to that for an open approach.2,3 There is a debate regarding the use of LA to treat perforated or complicated appendicitis in children.5-7 In recent reports of complicated appendicitis in children, LA was considered the treatment of choice.8-13 To treat children with complicated appendicitis accompanied by generalized peritonitis, the severely advanced form of complicated appendicitis, the only one prospective study comparing laparoscopy with an open method reported the superiority of laparoscopic treatment; however, only a small number (n=12) of patients were treated with laparoscopy in this study.14 Therefore, to our best knowledge, the present study is the largest to examine treatments for generalized peritonitis in children with appendicitis.
In the present study, the outcomes of the LA group were similar to or better than those of the OA group. Intraoperative and postoperative complications of the LA group occurred at an acceptable frequency. Among them, wound infection and long-term intestinal obstruction occurred less frequently in the LA group. We believe that these complications could be reduced by the innate characteristics of laparoscopy, that is, a minimal incision, compared to extended laparotomy for the treatment of complicated appendicitis. Another factor reducing the incidence of long-term intestinal obstruction in our study was thorough irrigation under direct vision of the entire abdominal cavity in the LA group, in contrast to sponge stick sweeps and irrigation with a limited view in the OA group. We attempted meticulous irrigation using a magnified, laparoscopic view by cleaning the entire abdominal cavity, including both paracolic gutters, pelvic cavity, perihepatic space, splenic fossa, and most of the intermesenteric spaces in most patients of the LA group. Those careful and meticulous irrigations may have partly contributed to the longer operative time in the LA group.
Our study also found a low rate of conversion from laparoscopy to an open approach. Technical limitations can be expected from the small working space and diffuse adhesions during laparoscopy in children with peritonitis secondary to perforated appendicitis, which could limit the use of the laparoscopic approach and lead to an initial consideration of open surgery. However, the limited working space was not a problem for appendectomy in most of the children with generalized peritonitis from perforated appendicitis in this study. The open conversion rate of our study (10.8%) is comparable to those of previous studies reporting 4.1-39.1%.15-18 Considering that our study included severe forms of perforated appendicitis, our results indicate the favorableness of a laparoscopic approach.
Although the conversion rate was low in this cohort with generalized peritonitis, bowel leakage was common among patients who required open conversion. Among the patients with generalized peritonitis from perforated appendicitis, severe adhesions and more advanced inflammatory changes around the operative field could be expected in patients in whom laparoscopic attempts failed and who required conversion to open surgery. If patients undergo conversion from laparoscopy to open appendectomy, they then should be managed carefully to prevent postoperative complications such as leakage from bowel anastomoses.
This study had a few limitations. First, it was impossible to compare the use of antibiotics, duration of drainage, or start of oral feeding between the two groups because of the innate limitation of the retrospective design. In addition, the duration of follow-up differed between the LA and OA groups. The shorter mean duration of follow-up of the LA group may have resulted in underestimation of the incidence of long-term complications. Thus, a longer follow-up period could be required for the LA group to compare the long-term outcomes between the two groups. However, we believe that the mean follow-up period of 43.5 months in the LA group was sufficient for estimating the incidence of postoperative complications.
The other limitation was the difference in disease severity between the LA and OA groups. To evaluate the outcomes of LA for children with generalized peritonitis from perforated appendicitis, we included patients who underwent OA for perforated appendicitis with localized or generalized peritonitis in the control group. In contrast to the easy confirmation of generalized peritonitis by laparoscopic findings in the LA group, OA may be inappropriate for evaluating the entire abdomen. Therefore, there were inevitable differences in disease severity between the two groups. However, the severity of morbidity in the LA group was equal to or more advanced than that in the OA group. Moreover, the outcomes of laparoscopy for generalized peritonitis were comparable to those of an open approach for perforated appendicitis.
In this study, the outcomes of the LA group for generalized peritonitis were comparable or superior to those of the OA group for perforated appendicitis with localized or generalized peritonitis. LA was a safe and useful technique for treating children with generalized peritonitis secondary to perforated appendicitis that decreased the incidence of postoperative wound infections and long-term intestinal obstruction. To reduce the incidence of wound infection and long-term intestinal obstruction, LA should be attempted in all children suspected of having generalized peritonitis from perforated appendicitis.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Morrow SE, Newman KD. Current management of appendicitis. Semin Pediatr Surg. 2007;16:34–40. doi: 10.1053/j.sempedsurg.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Horwitz JR, Custer MD, May BH, Mehall JR, Lally KP. Should laparoscopic appendectomy be avoided for complicated appendicitis in children? J Pediatr Surg. 1997;32:1601–1603. doi: 10.1016/s0022-3468(97)90462-0. [DOI] [PubMed] [Google Scholar]
- 3.Krisher SL, Browne A, Dibbins A, Tkacz N, Curci M. Intra-abdominal abscess after laparoscopic appendectomy for perforated appendicitis. Arch Surg. 2001;136:438–441. doi: 10.1001/archsurg.136.4.438. [DOI] [PubMed] [Google Scholar]
- 4.el Ghoneimi A, Valla JS, Limonne B, Valla V, Montupet P, Chavrier Y, et al. Laparoscopic appendectomy in children: report of 1,379 cases. J Pediatr Surg. 1994;29:786–789. doi: 10.1016/0022-3468(94)90371-9. [DOI] [PubMed] [Google Scholar]
- 5.Meguerditchian AN, Prasil P, Cloutier R, Leclerc S, Péloquin J, Roy G. Laparoscopic appendectomy in children: a favorable alternative in simple and complicated appendicitis. J Pediatr Surg. 2002;37:695–698. doi: 10.1053/jpsu.2002.32255. [DOI] [PubMed] [Google Scholar]
- 6.Ikeda H, Ishimaru Y, Takayasu H, Okamura K, Kisaki Y, Fujino J. Laparoscopic versus open appendectomy in children with uncomplicated and complicated appendicitis. J Pediatr Surg. 2004;39:1680–1685. doi: 10.1016/j.jpedsurg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Partrick DA. Prospective evaluation of a primary laparoscopic approach for children presenting with simple or complicated appendicitis. Am J Surg. 2006;192:750–755. doi: 10.1016/j.amjsurg.2006.08.039. [DOI] [PubMed] [Google Scholar]
- 8.Menezes M, Das L, Alagtal M, Haroun J, Puri P. Laparoscopic appendectomy is recommended for the treatment of complicated appendicitis in children. Pediatr Surg Int. 2008;24:303–305. doi: 10.1007/s00383-007-2102-8. [DOI] [PubMed] [Google Scholar]
- 9.Taqi E, Al Hadher S, Ryckman J, Su W, Aspirot A, Puligandla P, et al. Outcome of laparoscopic appendectomy for perforated appendicitis in children. J Pediatr Surg. 2008;43:893–895. doi: 10.1016/j.jpedsurg.2007.12.033. [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Zhang W, Yang X, Shao J, Zhou X, Yuan J. Complicated appendicitis in children: is laparoscopic appendectomy appropriate? A comparative study with the open appendectomy--our experience. J Pediatr Surg. 2009;44:1924–1927. doi: 10.1016/j.jpedsurg.2009.03.037. [DOI] [PubMed] [Google Scholar]
- 11.Lee SL, Yaghoubian A, Kaji A. Laparoscopic vs open appendectomy in children: outcomes comparison based on age, sex, and perforation status. Arch Surg. 2011;146:1118–1121. doi: 10.1001/archsurg.2011.144. [DOI] [PubMed] [Google Scholar]
- 12.Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, et al. Comparison of outcomes of laparoscopic versus open appendectomy in children: data from the Nationwide Inpatient Sample (NIS), 2006-2008. World J Surg. 2012;36:573–578. doi: 10.1007/s00268-011-1417-8. [DOI] [PubMed] [Google Scholar]
- 13.Nataraja RM, Teague WJ, Galea J, Moore L, Haddad MJ, Tsang T, et al. Comparison of intraabdominal abscess formation after laparoscopic and open appendicectomies in children. J Pediatr Surg. 2012;47:317–321. doi: 10.1016/j.jpedsurg.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Miyano G, Okazaki T, Kato Y, Marusasa T, Takahashi T, Lane GJ, et al. Open versus laparoscopic treatment for pan-peritonitis secondary to perforated appendicitis in children: a prospective analysis. J Laparoendosc Adv Surg Tech A. 2010;20:655–657. doi: 10.1089/lap.2010.0079. [DOI] [PubMed] [Google Scholar]
- 15.Liu SI, Siewert B, Raptopoulos V, Hodin RA. Factors associated with conversion to laparotomy in patients undergoing laparoscopic appendectomy. J Am Coll Surg. 2002;194:298–305. doi: 10.1016/s1072-7515(01)01164-4. [DOI] [PubMed] [Google Scholar]
- 16.Mancini GJ, Mancini ML, Nelson HS., Jr Efficacy of laparoscopic appendectomy in appendicitis with peritonitis. Am Surg. 2005;71:1–4. [PubMed] [Google Scholar]
- 17.Pokala N, Sadhasivam S, Kiran RP, Parithivel V. Complicated appendicitis--is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg. 2007;73:737–741. [PubMed] [Google Scholar]
- 18.Garg CP, Vaidya BB, Chengalath MM. Efficacy of laparoscopy in complicated appendicitis. Int J Surg. 2009;7:250–252. doi: 10.1016/j.ijsu.2009.04.007. [DOI] [PubMed] [Google Scholar]


