Abstract
Purpose
Although the effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) for panic disorder (PD) has been studied previously, data on the predictors of treatment outcomes in MBCT for PD are scarce.
Materials and Methods
Eighty patients with PD were screened to analyze treatment outcomes such as MBCT completion, treatment response, and remission after undergoing MBCT for PD. Sociodemographic characteristics, comorbid personality disorders, and baseline medication doses were examined. The study administered the Panic Disorder Severity Scale, Hamilton Anxiety Rating Scale, Hamilton Depression Rating Scale and Anxiety Sensitivity Inventory-Revised to patients at baseline and at eight weeks.
Results
Sixty-five participants were enrolled in the present study. Comorbid personality disorder was significantly associated with MBCT non-completion. We found that anxiety sensitivity (AS) improvement after an eight week MBCT program was a statistically significant factor associated with treatment response. Using logistic regression analysis, AS improvement after MBCT showed significant association with PD remission after MBCT.
Conclusion
Comorbid personality disorders of participants could be a potential predictor of MBCT non-completion. Furthermore, AS improvement after MBCT may predict treatment response and remission after MBCT for PD. However, better designed studies with a larger number of patients are needed to confirm our findings.
Keywords: Mindfulness-Based Cognitive Therapy, panic disorder, treatment outcome, anxiety sensitivity, comorbid personality disorder
INTRODUCTION
Mindfulness-based interventions, such as Mindfulness-Based Stress Reduction, has been applied to various clinical populations including chronic pain, cancer, and anxiety disorders.1-3 Mindfulness-Based Cognitive Therapy (MBCT) was developed for relapse prevention in depression;4 furthermore, previous reports on MBCT showed a possibility for its use in treating anxiety symptoms.5,6
Similar to previous studies that reported an effect of MBCT on anxiety symptoms among patients with bipolar disorder6 or generalized anxiety disorder,5 MBCT for panic disorder (PD), considering the particular characteristics of PD, has been introduced.7-9 According to previous studies on MBCT for PD, PD patients treated with MBCT stayed in remission without relapse for 12 months.7,8 Although some MBCT studies were limited by a small sample size, lack of follow-up measures, problems with control groups or lack of randomization,10 recent studies have supported the usefulness of adapted versions of MBCT for a greater variety of anxiety disorders including generalized anxiety disorders and social phobia.5,11-15
Conceptually, mindfulness, i.e. a mindful state of being, involves a quality of consciousness with attention to one's current experience.16 It was proposed that present-moment mindful awareness could be a useful, alternative way of responding to future-directed worry in anxiety disorder.5 Also, MBCT participants may be able to stem negative thought processes from worsening to anxiety with the essential skill of being able to de-center from their thoughts and feelings.11
While MBCT for depression has been designed to address rumination to prevent depressive patients from relapsing,17 it has been reported that MBCT for PD could reduce worries and phobia in PD or generalized anxiety disorder.7-9 Above all, according to a report in 2010,7 MBCT could reduce anxiety sensitivity (AS), as well as symptoms in patients with PD, even though the study was small in size (n=17) and non-controlled. AS is a trait-like cognitive characteristic that predisposes individuals to the development of panic problems and may be regarded a risk factor in the development of anxiety disorders.18 Development of mindfulness in individuals with PD was proposed to be beneficial in dealing with high AS, cognitive misinterpretation, and phobic avoidance via a decentralized perspective and acceptance in mindfulness based intervention.19 However, the characteristics of patients who would experience a better response to MBCT have not been explored appropriately.
With increased demand for more cost-effective and accessible treatments, it has become increasingly important to consider patient factors that could influence treatment outcomes. For these reasons, some previous studies made considerable efforts to explore the "predictors" of treatment outcomes using other psychotherapeutic approaches. A recent study examined the predictors of response to interpersonal psychotherapy (IPT) and cognitive behavior therapy (CBT) in depression, reporting that increasing comorbid personality disorder symptomatology was associated with poorer response to IPT.20 Other studies showed that CBT was not effective enough to treat depression in patients with high initial severity of disease and a few sociodemographic findings.21,22 In addition, improvement of AS after mindfulness training may be associated with treatment outcomes.7,19 These findings might imply that certain characteristics of patients are more responsive to particular psychotherapeutic modalities.
However, as far as we know, only one study has investigated the predictors of MBCT,23 and it was conducted with depression patients. No study has investigated the predictors of MBCT in PD. Therefore, the present study sought to provide further information on the factors associated with treatment outcomes from MBCT in PD. We hypothesized that factors such as comorbid personality disorders, baseline depression or anxiety symptom severity, and improvement of AS after MBCT would affect MBCT completion, treatment response, and remission in patients with PD.
MATERIALS AND METHODS
Participants
For this study, 80 patients with PD were screened. The subjects were recruited via advertisements from among patients treated on an outpatient basis at the Department of Psychiatry, CHA Bundang Medical Center, CHA University, between September 2006 and June 2010. Subjects were 20-60 years old and fulfilled the DSM-IV criteria for PD with or without agoraphobia, as diagnosed by two psychiatrists through a structured clinical interview to assess DSM-IV (SCID) Axis I disorders (inter-rater reliability κ: 0.82).24,25 After more than 3 months of pharmacotherapy, all subjects had shown a response, but had not achieved remission as defined according to Ballenger's criteria.26 They had stabilized and their remaining symptoms had not changed in clinical global impression27 for at least two months prior to commencement of MBCT as confirmed by psychiatrists. Prior to the commencement of the study, subjects were treated with antidepressants, including paroxetine, escitalopram, or venlafaxine, and benzodiazepines as anxiolytics, including alprazolam, diazepam or clonazepam. Kinds and dosages of medications prescribed were not altered during the study. Exclusion criteria included comorbid Axis I disorders, mental retardation, significant medical problems (e.g. chronic obstructive pulmonary disease, bronchial asthma, tuberculosis, cardiac disease, diabetes mellitus, pheochromocytoma, and thyroid disease), participation in meditation, yoga or regular psychotherapy on their own and involvement in litigation or compensation. Generally, there are a fair amount of PD patients with comorbid Axis I disorders in clinical settings; however, we excluded them because we aimed to determine factors associated with treatment outcomes of MBCT in "pure" PD. All study procedures complied with CHA Bundang Medical Center Institutional Review Board regulations, the Declaration of Helsinki, and the principles of Good Clinical Practice. Written informed consent was obtained after providing subjects with a full description of the study.
MBCT program
Our MBCT program for PD has been described in detail elsewhere8 (Table 1). Briefly, the MBCT program was led by three specialist psychiatrists with three years of MBCT education and training experience. All sessions were monitored and feedback was exchanged by those three psychiatrists. The manual for the MBCT program was written in Korean in order to maintain treatment integrity. The MBCT program used in the present study was devised for PD patients based on Segal, et al.'s17 MBCT for depression and Korean mindfulness meditation,28 which is substantially the same as mindfulness meditation,29 but reframed in the Korean language with regard to culture. The MBCT for PD included mindfulness techniques (e.g., body scan, three-minute breathing space, sitting meditation, mindful walking, etc.), cognitive approaches, education about PD and cognitive distortions specific to PD, and homework to encourage the use of mindfulness in everyday life through regular practice. The program was conducted in 13 separate groups, each of which comprised up to 12 participants. The duration of the weekly MBCT program was about 90 minutes, and a total of eight sessions was conducted. At the end of each session, the participants received homework and an audio CD that the authors recorded in Korean. Program adherence, which was assessed with a homework checklist consisting of everyday practice before beginning each session by psychiatrists leading the program, was good (>80%). While reviewing homework, there were intensive discussions with the participants to ensure that they could understand the important concepts of MBCT and use them in daily life.
Table 1.
Eight Week Program of Mindfulness-Based Cognitive Therapy (MBCT) for Panic Disorder
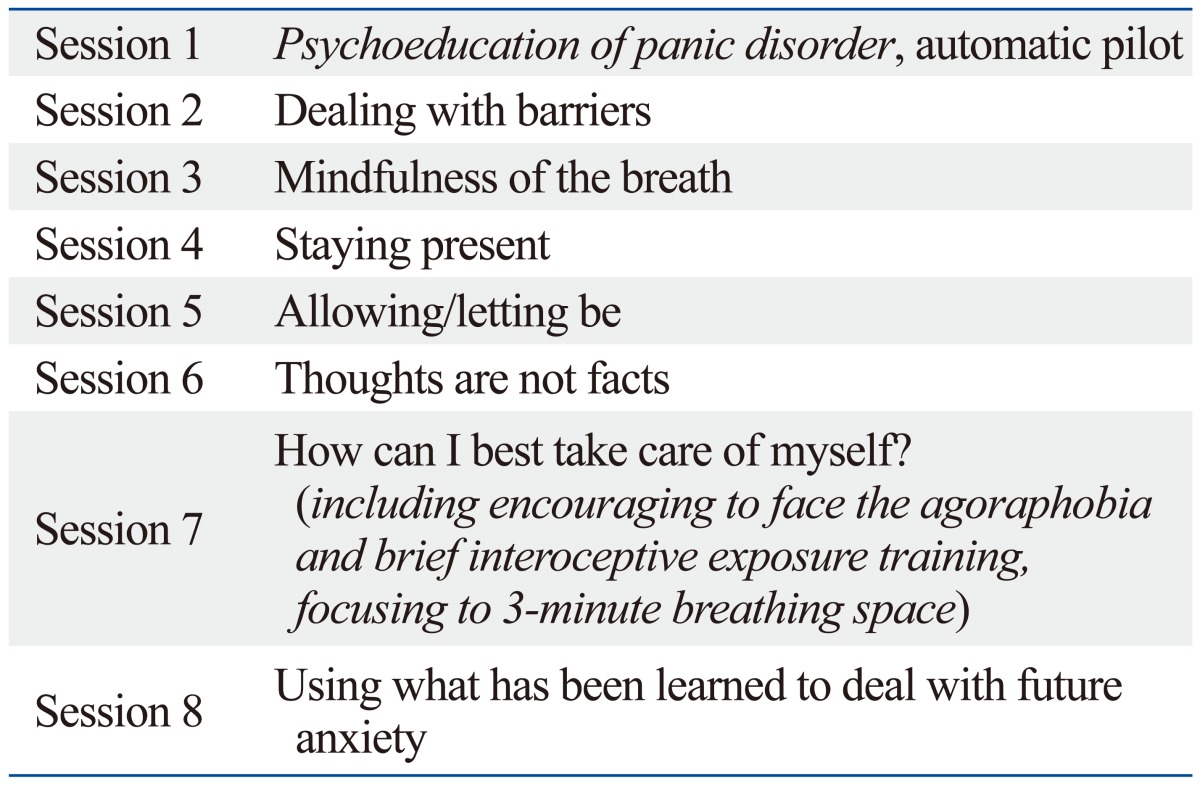
Components different from MBCT for depression are shown in italic letters.
Assessments
Subjects participated in weekly MBCT sessions for PD for eight weeks. Written questionnaires administered at baseline collected data on sociodemographic data of all subjects. Also, two psychiatrists assessed comorbid Axis I disorders using SCID-I modules A (mood episodes), C (psychotic disorders), D (mood disorders), E (substance use disorders), F (anxiety disorders), G (somatoform disorders), H (eating disorders) and I (adjustment disorders). Comorbid Axis II disorders, such as personality disorders, were examined according to the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) covering eleven DSM-IV Personality Disorders (including personality disorder not otherwise specified), as well as the appendix categories for depressive personality disorder and passive-aggressive personality disorder (inter-rater reliability κ=0.71).30,31
Participants were assessed at baseline (0 week) and eight weeks using self-reporting measures and clinician-rated scales, including Panic Disorder Severity Scale (PDSS),32,33 Anxiety Sensitivity Inventory-Revised (ASI-R),34,35 Hamilton Depression Rating Scale (HAM-D),36 and Hamilton Anxiety Rating Scale (HAM-A).37 Especially, AS and panic symptom severity improvement were analyzed as the proportion of reduction in ASI-R (or PDSS) score after eight weeks in the MBCT program compared to baseline ASI-R (or PDSS) score as a primary outcome measure: AS improvement=[(baseline ASI-R score-ASI-R score at eight weeks)/baseline ASI-R score×100 (%)]; PDSS improvement=[(baseline PDSS score-PDSS score at eight weeks)/baseline PDSS score×100 (%)].
Treatment outcomes were determined based on the three components of MBCT completion, treatment response, and remission. MBCT completion was considered as participating more than six out of eight MBCT sessions. Treatment response was defined as at least a 40% reduction in PDSS score from the baseline level.38,39 We defined remission of PD at 1-year follow-up as HAM-D≤7, HAM-A≤7, freedom from panic attacks, no or mild agoraphobic avoidance, and no functional impairment according to Ballenger's remission criteria for PD.26 One-year follow-up was conducted with patients visiting an outpatient clinic or through telephone interview for all participants.
Statistical analysis
Independent t-test, χ2 test, Mann-Whitney U test, or Fisher's exact test was used to compare sociodemographic and clinical characteristics between groups according to treatment outcome (completers vs. non-completers, responders vs. non-responders, and remission vs. non-remission). In addition, with variables significantly correlated to treatment outcome, such as MBCT completion, response, or remission after MBCT, multivariate logistic regression analysis was conducted to examine the factors associated with treatment outcome. IBM SPSS Statistics Ver. 20 (IBM SPSS Statistics, Somers, New York, NY, USA) was used to conduct all statistical analyses.
RESULTS
Sociodemographic characteristics of the participants
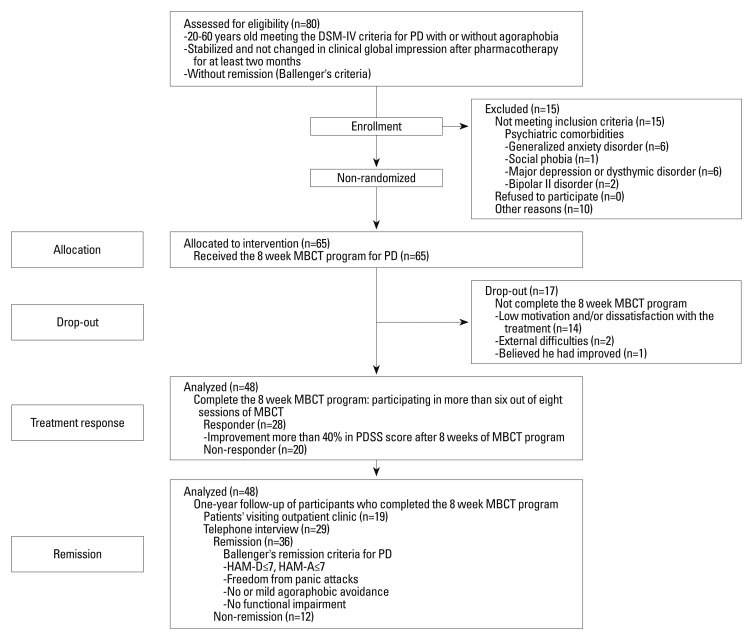
Eighty participants were screened in this study. Fifteen participants were excluded from the analysis as they met the criteria of Axis I comorbidities including generalized anxiety disorder (n=6), major depressive disorder or dysthymic disorder (n=6), bipolar II disorder (n=2), and social phobia (n=1). A detailed flow diagram of the data is shown in Fig. 1. Also, sociodemographic characteristics and clinical features, such as comorbid personality disorders, baseline anxiety, and depressive symptom severities of sixty-five subjects participating MBCT, are described in Table 2. Comorbid personality disorders (n=16) included obsessive-compulsive (n=6), histrionic (n=3), avoidant (n=3), narcissistic (n=2), or dependent personality traits (n=2). Assessed by the SCID-II, no participants met criteria for the remaining personality disorders such as paranoid, schizoid, schizotypal, antisocial, borderline, depressive, passive-aggressive or personality disorder not otherwise specified. The mean number of MBCT sessions attended for all participants was 6.88±1.65.
Fig. 1.
Flow diagram of the study of MBCT for panic disorder. MBCT, Mindfulness-Based Cognitive Therapy; PD, panic disorder; PDSS, Panic Disorder Severity Scale; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale.
Table 2.
Sociodemographic and Clinical Characteristics of All Participants Who Underwent the MBCT Program (n=65)
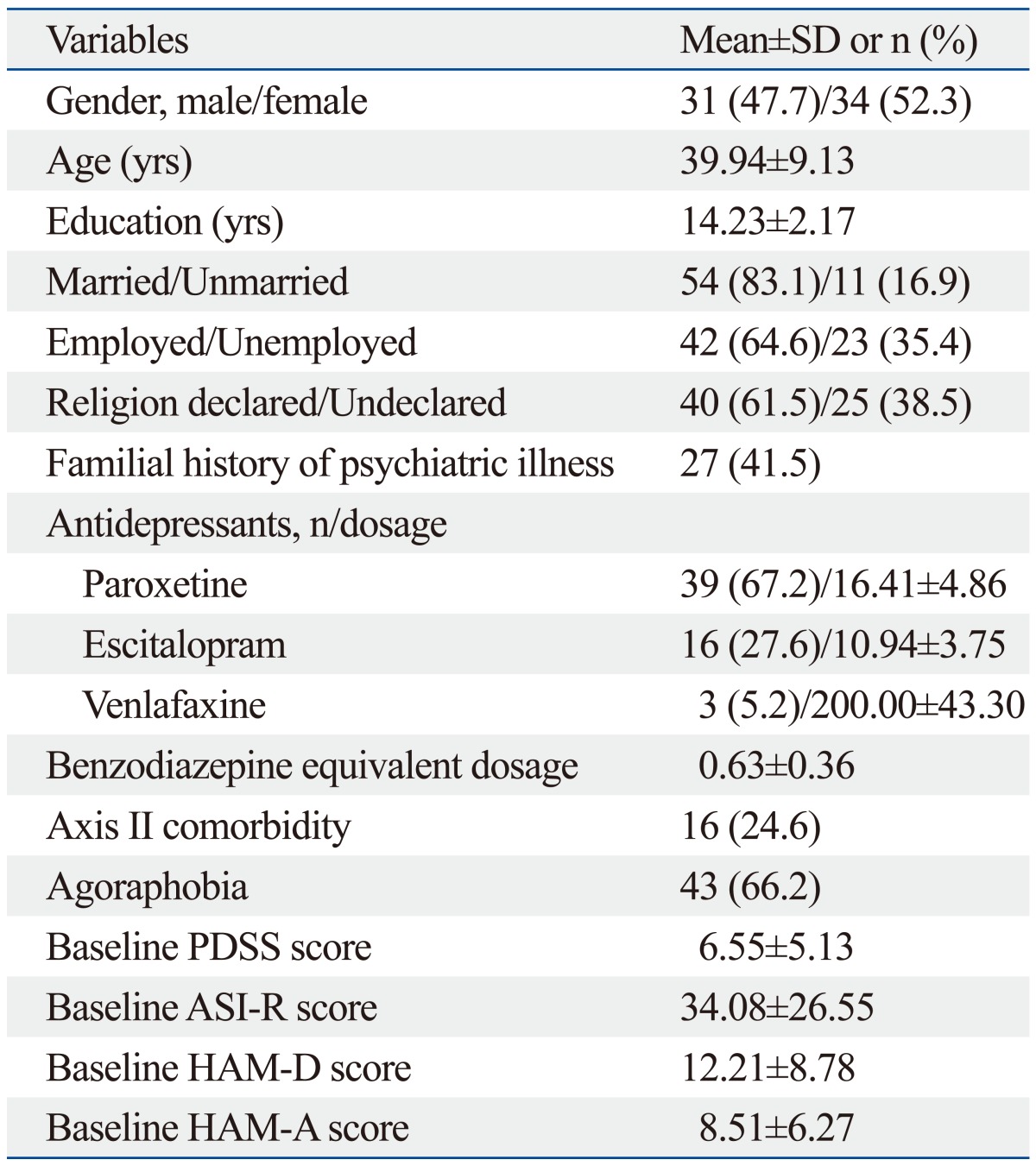
MBCT, Mindfulness-Based Cognitive Therapy; SD, standard deviation; PDSS, Panic Disorder Severity Scale; ASI-R, Anxiety Sensitivity Inventory-Revised; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale.
Factors associated with treatment outcomes of MBCT
MBCT completion
Of 65 subjects enrolled in the present study, 48 completed the MBCT program (defined as participating in more than six out of eight sessions of MBCT; participating 7.79±0.62 sessions), but 17 participants did not complete the program (4.29±0.47 sessions). Among sociodemographic and clinical characteristics, comorbid personality disorders (p<0.001) and a family history of psychiatric illness (p=0.049) were significantly associated with completion of MBCT for PD according to Fisher's exact test. Considering multiple comparison correction (Bonferroni correction, level of significance alpha=0.05/15≒0.003), comorbid personality disorders (p<0.001) were the only factor associated with MBCT completion. Also, evaluating factors associated with completion of MBCT program according to logistic regression analysis, only comorbid personality disorders were shown to have a significant association (Table 3).
Table 3.
Logistic Regression Analysis Evaluating Factors Associated with Completion of the MBCT Program in Patients with Panic Disorder (n=65)
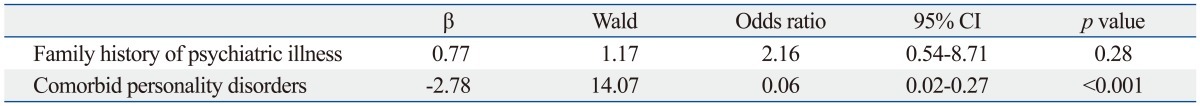
MBCT, Mindfulness-Based Cognitive Therapy; CI, confidence interval.
The main reasons for not completing MBCT were grouped into three categories in line with previous studies.40 Of all the subjects who did not complete MBCT (n=17), 14 patients (82.4%) missed sessions due to low motivation and/or dissatisfaction with the treatment, two patients (11.8%) because of external difficulties, and one patient (5.9%) who believed he had improved.
Treatment response
Treatment response was assessed as improvement of more than 40% in PDSS score after eight weeks in the MBCT program among those who completed the MBCT program (n=48). Comparing responders (n=28) and non-responders (n=20) in regards to sociodemographic and clinical variables, treatment responders showed a significantly greater reduction in ASI-R score after eight weeks in the MBCT program [(baseline ASI-R score-ASI-R score at eight weeks)/baseline ASI-R score×100 (%)] [Responder (median, %), 87.74; non-responder, 50.00; Z=-2.94, p=0.003] (Mann-Whitney U test for variables without normal distribution; Bonferroni correction, level of significance alpha=0.05/16≒0.003).
Remission
Overall, 36 out of 48 subjects (75%) satisfied the Ballenger's remission criteria26 at one-year follow-up after the MBCT program. Remission was attained in participants who had shown greater improvement in AS after undergoing MBCT according to ASI-R score [(baseline ASI-R score-ASI-R score at eight weeks)/baseline ASI-R score×100 (%)], greater improvement in PDSS score after MBCT [(baseline PDSS score-PDSS score at eight weeks)/baseline PDSS score×100 (%)], and lower baseline HAM-D score, compared to the non-remission group (Table 4). After multiple comparison correction (Bonferroni correction, level of significance alpha=0.05/17≒0.003), improvements in AS (p<0.001) and PDSS (p=0.001) were significantly different between the remission and non-remission groups. Furthermore, when we analyzed factors according to logistic regression analysis, only improvement in AS after MBCT was associated with remission in PD (Table 5).
Table 4.
Comparison of Sociodemographic and Clinical Characteristics between Remission and Non-Remission Groups of Panic Disorder Patients after Completion of the MBCT Program (n=48)
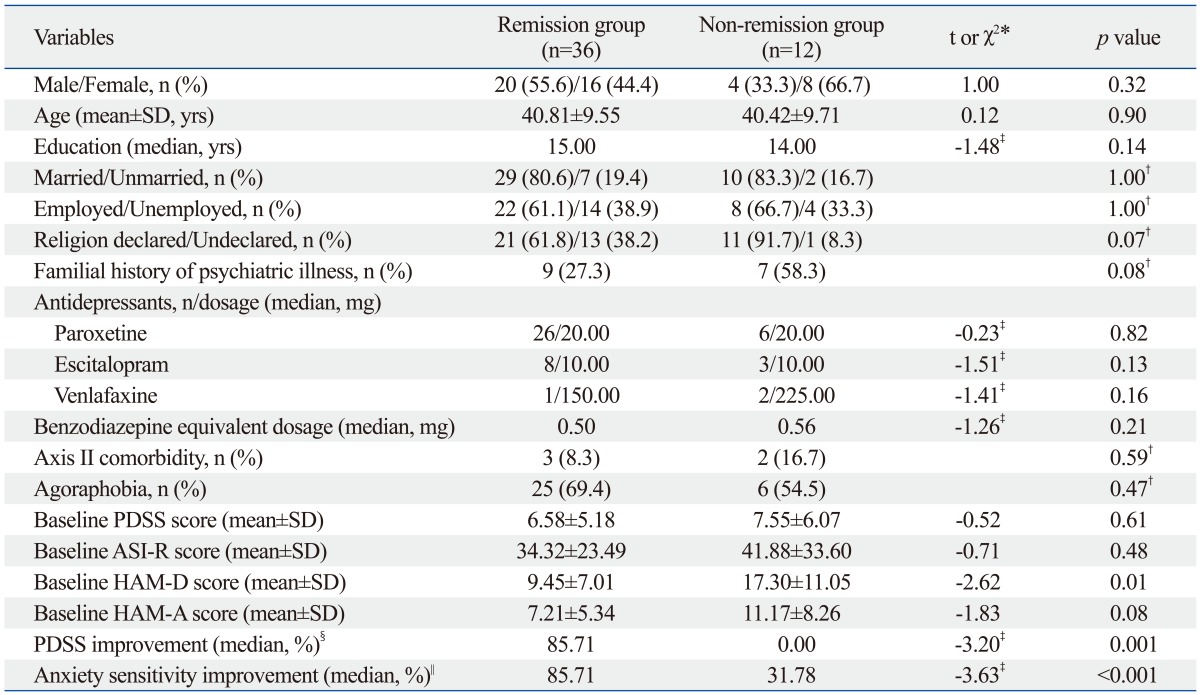
MBCT, Mindfulness-Based Cognitive Therapy; SD, standard deviation; PDSS, Panic Disorder Severity Scale; ASI-R, Anxiety Sensitivity Inventory-Revised; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale.
*χ2 statistics with continuity correction were used to analyze frequencies and t tests were used to test mean differences.
†Fisher's exact test.
‡Mann-Whitney U test, z-score value for variables without normal distribution.
§Reduction in PDSS score after eight weeks of MBCT=[(baseline PDSS score-PDSS score at eight weeks)/baseline PDSS score]×100 (%).
∥Reduction in ASI-R score after eight weeks of MBCT=[(baseline ASI-R score-ASI-R score at eight weeks)/baseline ASI-R score]×100 (%).
Table 5.
Logistic Regression Analysis Evaluating Factors Associated with Remission in Panic Disorder Patients Who Participated in the MBCT Program (n=48)
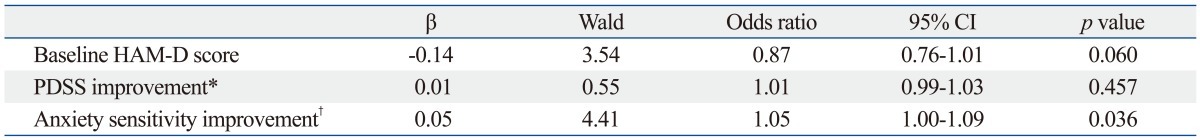
CI, confidence interval; MBCT, Mindfulness-Based Cognitive Therapy; HAM-D, Hamilton Depression Rating Scale; PDSS, Panic Disorder Severity Scale.
*Reduction in PDSS score after eight weeks of MBCT=[(baseline PDSS score-PDSS score at eight weeks)/baseline PDSS score]×100 (%).
†Reduction in ASI-R score after eight weeks of MBCT=[(baseline ASI-R score-ASI-R score at eight weeks)/baseline ASI-R score]×100 (%).
DISCUSSION
The aim of this study was to explore the potential predictors of treatment outcomes after MBCT for PD. Our group has previously reported on the results of MBCT applied to anxiety disorders, focusing on the effectiveness of MBCT in terms of reducing worry, insomnia, AS, phobia, and PD severity.7-9 In this study, we evaluated various characteristics of participants in relation to MBCT completion, treatment response, and remission to examine factors involved in treatment outcome. To our knowledge, this is the first study to investigate the potential predictors of treatment outcomes in MBCT for PD.
In our study, completers and non-completers differed significantly in terms of family history of psychiatric illness and comorbid personality disorders. Among them, comorbid personality disorder was a predictor of MBCT completion. In terms of treatment response, participants demonstrating treatment response after MBCT showed greater improvement in AS according to ASI-R score. In addition, the remission group showed a significantly greater treatment response after eight weeks of MBCT according to PDSS score, greater improvement in AS after MBCT according to ASI-R score, and lower baseline HAM-D score compared to the non-remission group. Of these factors, improvement in AS after MBCT showed significant association with remission of PD after undergoing MBCT.
Previous studies have indicated comorbidity as a factor associated with poorer treatment outcome when utilizing CBT or IPT to treat psychiatric disease.21,22,41 Dow, et al.42,43 suggested comorbidity as a prognostic index with brief and standard CBT for PD. Especially, according to Martinsen, et al.,44 the presence of severe personality disorders was associated with high dropout rate among those participating in CBT for PD.
However, according to another study that explored major depression patients comorbid with one of DSM-III axis II personality disorders, except schizotypal and antisocial personality disorder, personality pathology did not significantly worsen the outcome of treatment including CBT, IPT or antidepressants.45 Also, a study that only included cluster C personality disorders, showed that cluster C personality did not worsen outcomes in those receiving cognitive therapy.46 Another review article mentioned that some personality disorders might have had an adverse effect on outcomes to CBT in anxiety disorder, but did not identify direct predictors.47
We also intended to analyze the effect of comorbid personality disorders on treatment outcomes in MBCT for PD in this study. According to our present findings, comorbid personality disorders predicted non-completion of MBCT for PD. While other mindfulness-based therapies such as DBT have been reported as effective treatments with low drop-outs in borderline personality disorders,48,49 PD subjects with comorbid personality disorders who underwent MBCT were less likely to complete the eight week MBCT program in this study. This difference could be related to the fact that DBT includes specific behavioral, cognitive, emotional, and interpersonal skills training tailored to borderline personality disorder,50 whereas MBCT used in this study was focused on treatment of PD.
On the other hand, even though comorbid personality disorder was a significant predictor of MBCT non-completion, we found comorbid personality disorders did not have a significant effect on treatment response and remission among MBCT completers. This could imply that, so long as we can prevent them from dropping out, the treatment outcomes of MBCT for PD would not be significantly different despite the presence of comorbid personality problems.
Treatment response and remission after participating MBCT were associated with greater improvement in AS according to ASI-R score. AS has been suggested as a predictor of panic-related pathology with direct influence on the clinical course of panic disorder.51 As we reported in 2010,7 MBCT could reduce AS in patients with PD. Furthermore, according to the present results of this study, AS improvement after MBCT program might be a predictor of remission of PD at 1-year follow-up, as well as symptom reduction after 8 weeks of MBCT.
Through an adoption of a decentralized perspective on experiences in mindfulness training,52 decreased levels of AS might be achieved by virtue of an increased level of tolerance for anxiety, especially given that it is possible to become very aware of thoughts, feelings, and body sensations just as they are.7 It may be that remission can be achieved in MBCT participants who are able to effectively reduce AS and increase tolerance for anxiety through mindfulness training.
The present study has some limitations. First, it was a small-sized study and the statistical power was limited. Also, the present study was an uncontrolled design, which limits its significance and the possibility to generalize the results. In addition, we could not completely rule out the delayed effect of medication. Though participants were stable without any changes in medication dosages during the study period, it would be hard to determine the impact of medications on the findings, as medications varied across participants. Lastly, cognitive measures as well as Mindful Attention and Awareness Scale (MAAS)16 were not reported in this study. Since MAAS has not been well-validated in Koreans yet, it was not included in the present analysis.
In conclusion, the present study suggested that comorbid personality disorders of participants could be associated with non-completion of MBCT. Furthermore, it could be considered that AS improvement might predict treatment response and remission after MBCT for PD. However, better designed studies with larger numbers of patients are needed to confirm our findings.
ACKNOWLEDGEMENTS
This research was supported in part by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2011-0023359) to S.H. Lee.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 2.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Dell Publishing; 1990. [Google Scholar]
- 3.Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 4.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 5.Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J Anxiety Disord. 2008;22:716–721. doi: 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, et al. Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. J Affect Disord. 2008;107:275–279. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim B, Lee SH, Kim YW, Choi TK, Yook K, Suh SY, et al. Effectiveness of a mindfulness-based cognitive therapy program as an adjunct to pharmacotherapy in patients with panic disorder. J Anxiety Disord. 2010;24:590–595. doi: 10.1016/j.janxdis.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 8.Kim YW, Lee SH, Choi TK, Suh SY, Kim B, Kim CM, et al. Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress Anxiety. 2009;26:601–606. doi: 10.1002/da.20552. [DOI] [PubMed] [Google Scholar]
- 9.Yook K, Lee SH, Ryu M, Kim KH, Choi TK, Suh SY, et al. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: a pilot study. J Nerv Ment Dis. 2008;196:501–503. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]
- 10.Coelho HF, Canter PH, Ernst E. Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. J Consult Clin Psychol. 2007;75:1000–1005. doi: 10.1037/0022-006X.75.6.1000. [DOI] [PubMed] [Google Scholar]
- 11.Lovas DA, Barsky AJ. Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: a pilot study. J Anxiety Disord. 2010;24:931–935. doi: 10.1016/j.janxdis.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. 2011;187:441–453. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Finucane A, Mercer SW. An exploratory mixed methods study of the acceptability and effectiveness of Mindfulness-Based Cognitive Therapy for patients with active depression and anxiety in primary care. BMC Psychiatry. 2006;6:14. doi: 10.1186/1471-244X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharplin GR, Jones SB, Hancock B, Knott VE, Bowden JA, Whitford HS. Mindfulness-based cognitive therapy: an efficacious community-based group intervention for depression and anxiety in a sample of cancer patients. Med J Aust. 2010;193(5 Suppl):S79–S82. doi: 10.5694/j.1326-5377.2010.tb03934.x. [DOI] [PubMed] [Google Scholar]
- 15.Williams MJ, McManus F, Muse K, Williams JM. Mindfulness-based cognitive therapy for severe health anxiety (hypochondriasis): an interpretative phenomenological analysis of patients' experiences. Br J Clin Psychol. 2011;50:379–397. doi: 10.1111/j.2044-8260.2010.02000.x. [DOI] [PubMed] [Google Scholar]
- 16.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 17.Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- 18.Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: prospective prediction of panic attacks and Axis I pathology. J Psychiatr Res. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11:230–241. [Google Scholar]
- 20.Carter JD, Luty SE, McKenzie JM, Mulder RT, Frampton CM, Joyce PR. Patient predictors of response to cognitive behaviour therapy and interpersonal psychotherapy in a randomised clinical trial for depression. J Affect Disord. 2011;128:252–261. doi: 10.1016/j.jad.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Jarrett RB, Eaves GG, Grannemann BD, Rush AJ. Clinical, cognitive, and demographic predictors of response to cognitive therapy for depression: a preliminary report. Psychiatry Res. 1991;37:245–260. doi: 10.1016/0165-1781(91)90061-s. [DOI] [PubMed] [Google Scholar]
- 22.Thase ME, Reynolds CF, 3rd, Frank E, Simons AD, McGeary J, Fasiczka AL, et al. Do depressed men and women respond similarly to cognitive behavior therapy? Am J Psychiatry. 1994;151:500–505. doi: 10.1176/ajp.151.4.500. [DOI] [PubMed] [Google Scholar]
- 23.Michalak J, Hölz A, Teismann T. Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychol Psychother. 2011;84:230–236. doi: 10.1348/147608310X520166. [DOI] [PubMed] [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) Washington, D.C.: American Psychiatric Press, Inc.; 1996. [Google Scholar]
- 25.Han OS, Hong JP. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) Korean version. Seoul: Hana Medical; 2000. [Google Scholar]
- 26.Ballenger JC. Treatment of anxiety disorders to remission. J Clin Psychiatry. 2001;62(Suppl 12):5–9. [PubMed] [Google Scholar]
- 27.Guy W. Clinical Global Impressions (CGI). ECDEU Assessment Manual for Psychopharmacology revised. Rockville: National Institute of Mental Health; 1976. [Google Scholar]
- 28.Lee SH, Ahn SC, Lee YJ, Choi TK, Yook KH, Suh SY. Effectiveness of a meditation-based stress management program as an adjunct to pharmacotherapy in patients with anxiety disorder. J Psychosom Res. 2007;62:189–195. doi: 10.1016/j.jpsychores.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 29.Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 30.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, D.C.: American Psychiatric Press, Inc.; 1997. [Google Scholar]
- 31.Kim CG. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Korean version. Seoul: Hana Medical; 2005. [Google Scholar]
- 32.Lim YJ, Yu BH, Kim JH. Korean panic disorder severity scale: construct validity by confirmatory factor analysis. Depress Anxiety. 2007;24:95–102. doi: 10.1002/da.20206. [DOI] [PubMed] [Google Scholar]
- 33.Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, et al. Reliability and validity of the Panic Disorder Severity Scale: replication and extension. J Psychiatr Res. 2001;35:293–296. doi: 10.1016/s0022-3956(01)00028-0. [DOI] [PubMed] [Google Scholar]
- 34.Taylor S, Cox BJ. An expanded anxiety sensitivity index: evidence for a hierarchic structure in a clinical sample. J Anxiety Disord. 1998;12:463–483. doi: 10.1016/s0887-6185(98)00028-0. [DOI] [PubMed] [Google Scholar]
- 35.Lim YJ, Yu BH, Kim JH. Korean Anxiety Sensitivity Index-Revised: its factor structure, reliability, and validity in clinical and nonclinical samples. Depress Anxiety. 2007;24:331–341. doi: 10.1002/da.20210. [DOI] [PubMed] [Google Scholar]
- 36.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 38.Aaronson CJ, Shear MK, Goetz RR, Allen LB, Barlow DH, White KS, et al. Predictors and time course of response among panic disorder patients treated with cognitive-behavioral therapy. J Clin Psychiatry. 2008;69:418–424. doi: 10.4088/jcp.v69n0312. [DOI] [PubMed] [Google Scholar]
- 39.Furukawa TA, Katherine Shear M, Barlow DH, Gorman JM, Woods SW, Money R, et al. Evidence-based guidelines for interpretation of the Panic Disorder Severity Scale. Depress Anxiety. 2009;26:922–929. doi: 10.1002/da.20532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bados A, Balaguer G, Saldaña C. The efficacy of cognitive-behavioral therapy and the problem of drop-out. J Clin Psychol. 2007;63:585–592. doi: 10.1002/jclp.20368. [DOI] [PubMed] [Google Scholar]
- 41.Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: a comprehensive review of controlled outcome research. Psychol Bull. 1990;108:30–49. doi: 10.1037/0033-2909.108.1.30. [DOI] [PubMed] [Google Scholar]
- 42.Dow MG, Kenardy JA, Johnston DW, Newman MG, Taylor CB, Thomson A. Prognostic indices with brief and standard CBT for panic disorder: II. Moderators of outcome. Psychol Med. 2007;37:1503–1509. doi: 10.1017/S0033291707000682. [DOI] [PubMed] [Google Scholar]
- 43.Dow MG, Kenardy JA, Johnston DW, Newman MG, Taylor CB, Thomson A. Prognostic indices with brief and standard CBT for panic disorder: I. Predictors of outcome. Psychol Med. 2007;37:1493–1502. doi: 10.1017/S0033291707000670. [DOI] [PubMed] [Google Scholar]
- 44.Martinsen EW, Olsen T, Tønset E, Nyland KE, Aarre TF. Cognitive-behavioral group therapy for panic disorder in the general clinical setting: a naturalistic study with 1-year follow-up. J Clin Psychiatry. 1998;59:437–442. doi: 10.4088/jcp.v59n0808. [DOI] [PubMed] [Google Scholar]
- 45.Shea MT, Pilkonis PA, Beckham E, Collins JF, Elkin I, Sotsky SM, et al. Personality disorders and treatment outcome in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry. 1990;147:711–718. doi: 10.1176/ajp.147.6.711. [DOI] [PubMed] [Google Scholar]
- 46.Hardy GE, Barkham M, Shapiro DA, Stiles WB, Rees A, Reynolds S. Impact of Cluster C personality disorders on outcomes of contrasting brief psychotherapies for depression. J Consult Clin Psychol. 1995;63:997–1004. doi: 10.1037//0022-006x.63.6.997. [DOI] [PubMed] [Google Scholar]
- 47.Dreessen L, Arntz A. The impact of personality disorders on treatment outcome of anxiety disorders: best-evidence synthesis. Behav Res Ther. 1998;36:483–504. doi: 10.1016/s0005-7967(98)00026-6. [DOI] [PubMed] [Google Scholar]
- 48.Kliem S, Kröger C, Kosfelder J. Dialectical behavior therapy for borderline personality disorder: a meta-analysis using mixed-effects modeling. J Consult Clin Psychol. 2010;78:936–951. doi: 10.1037/a0021015. [DOI] [PubMed] [Google Scholar]
- 49.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- 50.Rosenthal MZ, Lynch TR. Dialectical Behavior Therapy. In: Sadock BJ, Sadock VA, Ruiz P, editors. Kaplan & Sadock's Comprehensive Textbook of Psychiatry. 9th ed. Baltimore: Lippincott Williams & Wilkins; 2009. pp. 2884–2893. [Google Scholar]
- 51.Stewart SH, Taylor S, Jang KL, Cox BJ, Watt MC, Fedoroff IC, et al. Causal modeling of relations among learning history, anxiety sensitivity, and panic attacks. Behav Res Ther. 2001;39:443–456. doi: 10.1016/s0005-7967(00)00023-1. [DOI] [PubMed] [Google Scholar]
- 52.Safran JD, Segal ZV. Interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]