Abstract
Purpose
Postoperative adhesion is the most frequent complication of abdominal surgery. Therefore, we investigated the individual effects of synthetic barrier [hyaluronic acid/carboxymethylcellulose (HA/CMC)] and pharmacologic agents [low molecular weight heparin (LMWH) cyclo-oxygenase-2 inhibitor (COX-2 inhibitor)] using animal model of intra-abdominal adhesion.
Materials and Methods
The cecum was rubbed with sterile alcohol wet gauze until subserosal haemorrhage and punctate bleeding developed under the general anesthesia. Five animal groups were prepared using the film HA/CMC, gel HA/CMC, LMWH and COX-2 inhibitor.
Results
The grade of adhesion by modified Leach method for group I (control), II (film type HA/CMC), III (gel type HA/CMC), IV (LMWH) and V (COX-2 inhibitor) were 5.35±1.8, 6.15±1.3, 4.23±2.6, 5.05±0.7 and 5.50±0.9, respectively. Group III showed the least grade of adhesion and it is statistically significant in adhesion formation (p=0.028). The numbers of lymphocytes were significantly low in group III and group V compared to the control group (lymphocyte: p=0.004). The mast cell counts were generally low except for the control group (I: 1.05, II: 0.35, III: 0.38, IV: 0.20, V: 0.37), however, it was not statistically significant (p=0.066).
Conclusion
The gel barriers were shown to be partly efficient in inhibiting the formation of postoperative adhesions and might provide an option for abdominal surgery to reduce postoperative adhesions. The LMWH and COX-2 inhibitor had been known for their inhibitor effect of fibrin formation and anti-angiogenic/anti-fibroblastic activity, respectively. However, their preventive effects of adhesion and fibrosis were found to be obscure.
Keywords: Adhesion prevention, cyclo-oxygenase-2 inhibitor, low molecular weight heparin, hyaluronic acid/carboxymethylcellulose
INTRODUCTION
Adhesions are internal scars and still remain as an almost inevitable consequence of most abdominal procedures, occurring after 63-93% of intra-abdominal procedures, and the rate increases up to 97% following pelvic surgery.1,2 Adhesions become apparent clinically in the form of chronic abdominal pain, female infertility, and small-bowel obstruction.3 The main factor of the intra-abdominal adhesions is surgical trauma (incision, cauterization, suturing, ischemia, desiccation abrasion). However, there exists no clinically relevant and effective method which has shown to be adequate in the prevention of adhesion formation, even after engaging in meticulous operative techniques which require delicate handling of tissue.
Recently, several synthetic biologic products have been developed. Despite the biochemical differences of these products, they act as a barrier between peritoneal surfaces and intra-abdominal organs. In addition, pharmacologic agents that target fibrin, fibroblasts and angiogensis have been applied and assessed. These agents reduce the peritoneal inflammatory response following the surgical trauma, thereby reducing the fibrous reaction and mature stages of adhesion formation.4 The cyclo-oxygenase-2 inhibitor (COX-2) inhibitor suppresses prolonged inflammation of injury and selectively inhibits angiogenesis. Therefore, it may enhance the reduced adhesion formation with anti-fibroblastic and anti-angiogenic properties. The fibrin blood clots can serve as a nexus for adhesions. Consequently, low molecular weight heparin (LMWH) prevents clot formation and reduces the adhesion formation.
Although these synthetic material and pharmacologic agents have their positive results, there is no comparative study using the same model. Therefore, we investigated the individual effects of synthetic products [hyaluronic acid/carboxymethylcellulose (HA/CMC)] and pharmacologic agents (COX-2 inhibitor, LMWH) using animal model of intra-abdominal adhesion.
MATERIALS AND METHODS
Animals
The animals used were specific pathogen free Sprague-Dawley rats (male, NTacSam: SD, Samtako Co, Seoul, Korea), 12 to 13 weeks of age, weighing 200 to 220 gm. The rats were kept in controlled ambient temperature (22-24℃) and lighting (12-h light-dark cycle) conditions. They were fed with standard rabbit pellets and tap water ad libitum. The animal care and procedures were performed in accordance with the recommendations outlined in the ethics committee of the animal experiment of Ewha Womans University College of Medicine.
Anesthesia, animal model and euthanasia
Each rat was anesthetized by intramuscular administration with mixture of Zoletil 50® (Virbac Laboratories, France, Tiletamine 125 mg/5mL, Zolazepam 125 mg/5mL, 50 mg/kg) and Rompun® (xylazine hydrochloride, BAYER Korea Co., 23.32 mg/mL, 2.5 mg/kg). The abdomen was shaved and cleaned with a povidine iodine solution and the abdominal laparotomy was performed by midline incision exposing the wall of the cecum. The cecum was rubbed with sterile alcohol wet gauze until subserosal haemorrhage and punctate bleeding developed (Fig. 1). Then, about 1×1 cm of peritoneum of anterior abdominal wall was removed and the cecum was returned to its anatomic position. Before closing the wound, a thin film plate and gel of HA/CMC were applied between the cecum and the abdominal wall in group II and III, respectively. In group I, normal saline was given and represented the control group (Table 1). The abdominal cavity was then closed in 2 layers with simple, continuous sutures of Vicryl® 3-0. The group IV was treated with Cleaxane® (enoxaparine Na, Sanofi Aventis Korea, 1 mg/kg) subcutaneously for 7 days after the identical surgery in group I. The group V was prepared by the same manner as in group I (control group) and was given Clebrex® (celecoxib, Pharmacia Korea, 50 mg/kg) orally for 2 weeks (Table 1). During surgery, rat was handled always with starch-free gloves, and body temperature was maintained using light bulb and warm mat. Each group was consisted of 20 rats and the above procedures were done by one surgeon for minimizing the bias of surgery of animal model.
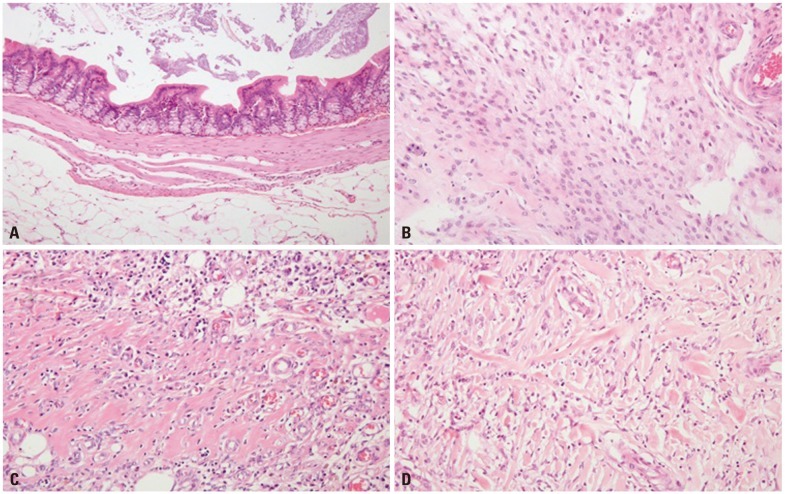
Fig. 1.
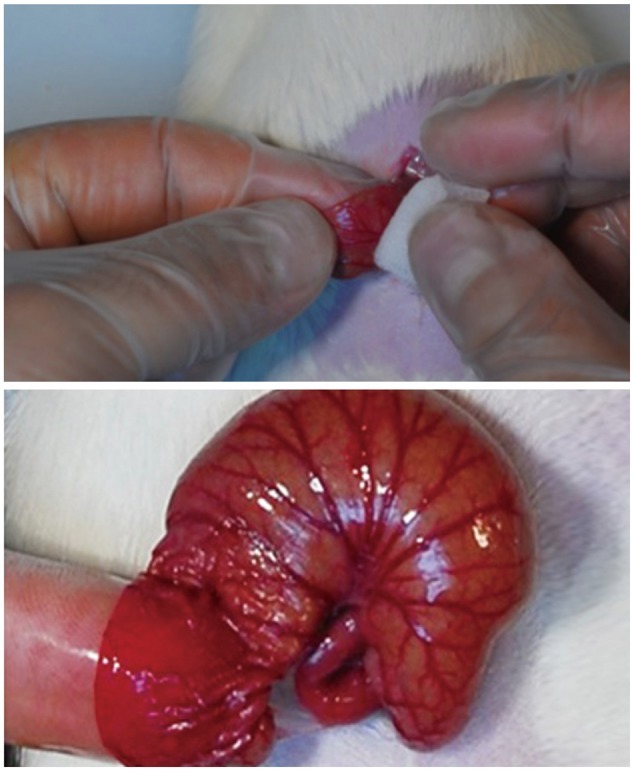
The cecum was rubbed until subserosal haemorrhage and punctate bleeding developed.
Table 1.
The Animal Number and Treated Materials According to the Model Groups
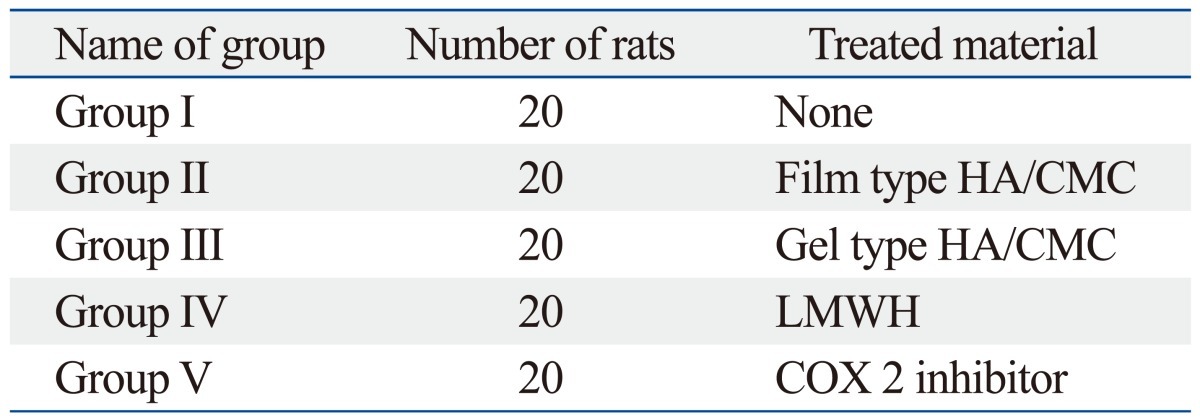
HA/CMC, hyaluronic acid/carboxymethylcellulose; LMWH, low molecular weight heparin; COX-2 inhibitor, cyclo-oxygenase-2 inhibitor.
After the peritoneal trauma, the cellularity of adhesion was replaced almost entirely by collagen fibrils associated with macrophages between 2 weeks and 2 months. Therefore, three weeks after the surgery, the rats were euthanized by intraperitoneal injection of Zoletil 50® (200 mg/kg) and the inverted U-shape window was made for the assessment of adhesion grading. For histopathologic evaluation of adhesion sites, the cecum and adhered organ were resected en-bloc together with any adhesive tissue and preserved in 4% buffered formaldehyde solution.
Grading of adhesion
Macroscopic grading
Macroscopic grading was assessed by two general surgeons using the modification tool of Leach grade and Nair grade (Table 2 and 3).5 The adhesion to the uterine horn is usually scored using Leach grade. We modified original grade of Leach, which included uterine horn as well as the whole intra-peritoneal organs for scoring of adhesion. Other detected intra-peritoneal pathologies were also recorded.
Table 2.
Modified Leach Grading of Adhesion*
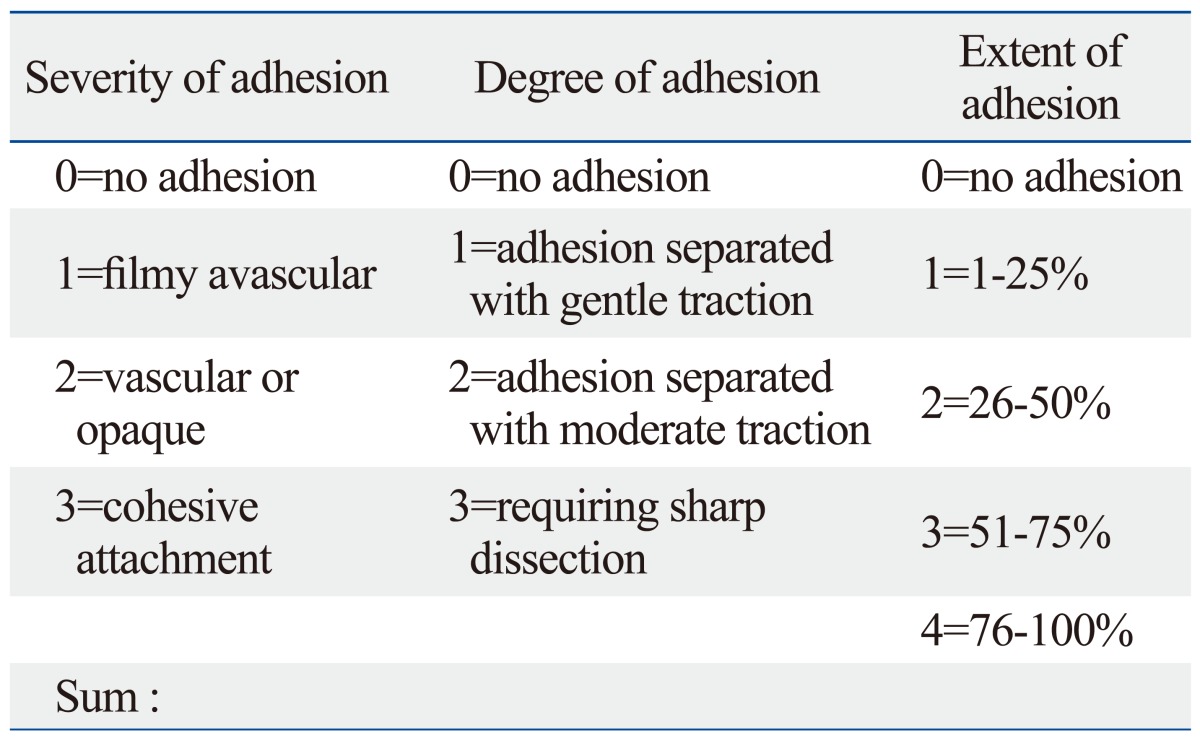
*Modification was done by author.
Table 3.
Nair's Grading of Adhesion
Microscopic grading
Serial sections were stained with haematoxylin and eosin, and evaluated the grade of adhesion and fibrosis under light microscopy. All evaluations were performed by single pathologist who was blinded to the methods and groups.
The degree of fibrosis was assessed by the percentage of extent adhesion area, the grade of fibrosis and the fibrosis depth. The extent adhesion area was defined as the percentage of fibrotic area on the most severe adhesion field. The grade of fibrosis was divided into four grades according to the density of collagen fibers (0: none, 1: thin, 2: moderate, 3: thick). The depth of fibrosis was evaluated by penetration depth of fibrosis from serosa to mucosa (0: none, 1: serosa, 2: muscle, 3: submucosa, 4: mucosa). The inflammation degree was evaluated by the number of inflammatory cells (neutrophils, macrophages, lymphocytes, giant cells and mast cell) under the 10 high power fields (HPFs) (Fig. 2).
Fig. 2.
The Grade of fibrosis. (A) Grade 0: no collagenous fibrosis in the bowel wall. (B) Grade 1: the mild degree of collagenous fibrosis in the perihepatic soft tissue. (C) Grade 2: the moderate degree of collagenous fibrosis involving colonic mucosa, muscle layer, and pericoloic fat tissue. (D) Grade 3: the extensive collagenous fibrosis in the whole layer of colonic wall with mucosal ulceration (Under the 10 high power fields).
Statistical analysis
Kruskall-Wallis test was used to detect significance of intergroup differences. If the Kruskall-Wallis test was significant, we used Post hoc Mann-Whitney U test with Bonferroni adjustment. The statistical analyses were performed using the SPSS software package (version 16.0, IBM, USA). The numerical data were expressed as mean and standard deviation. The results were evaluated with a confidence interval of 95%, and p-values below 0.05 were considered to be statistically significant.
RESULTS
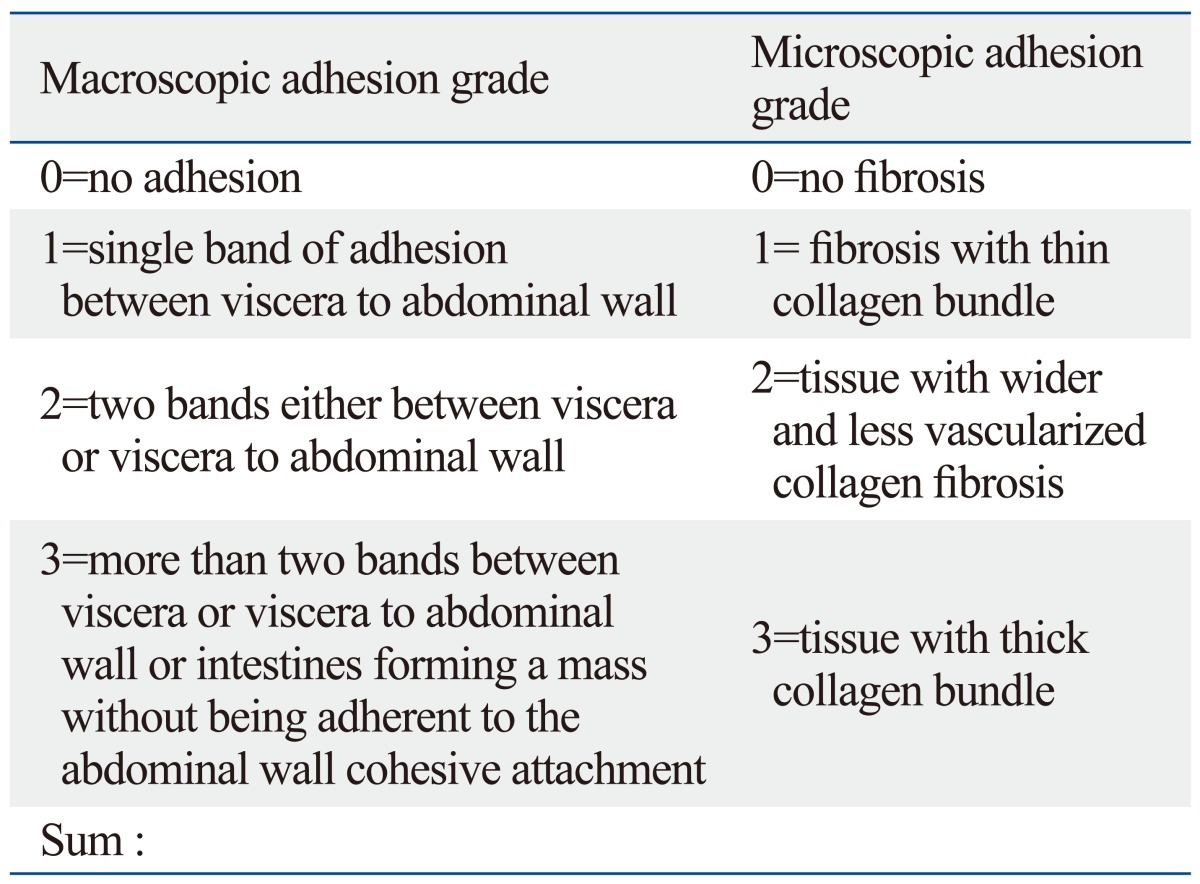
The organs adhered to rubbed cecum were small bowel, colon and abdominal wall, respectively. The grade of adhesion by modified Leach method (mean±standard deviation) for groups I, II, III, IV and V were 5.35±1.8, 6.15±1.3, 4.23±2.6, 5.05±0.7 and 5.50±0.9, respectively. Group III showed the least grade of adhesion and it is statistically significant in adhesion formation (p=0.028). Subsequent analysis revealed that group I and III were statistically significant in the severity of adhesion of the modified Leach (p=0.024). In Nair's classification, the grade of adhesion was as follows; group I: 2.24±1.0, group II: 2.10±0.7, group III: 2.23±1.4, group IV: 2.65±0.4, group V: 2.88±0.8. The Nair's macroscopic grade did not show any statistical significance even though the animal groups were same (Table 4).
Table 4.
Grade of Adhesion According to the Groups
*Mann-Whitney U test with Bonferroni adjustment.
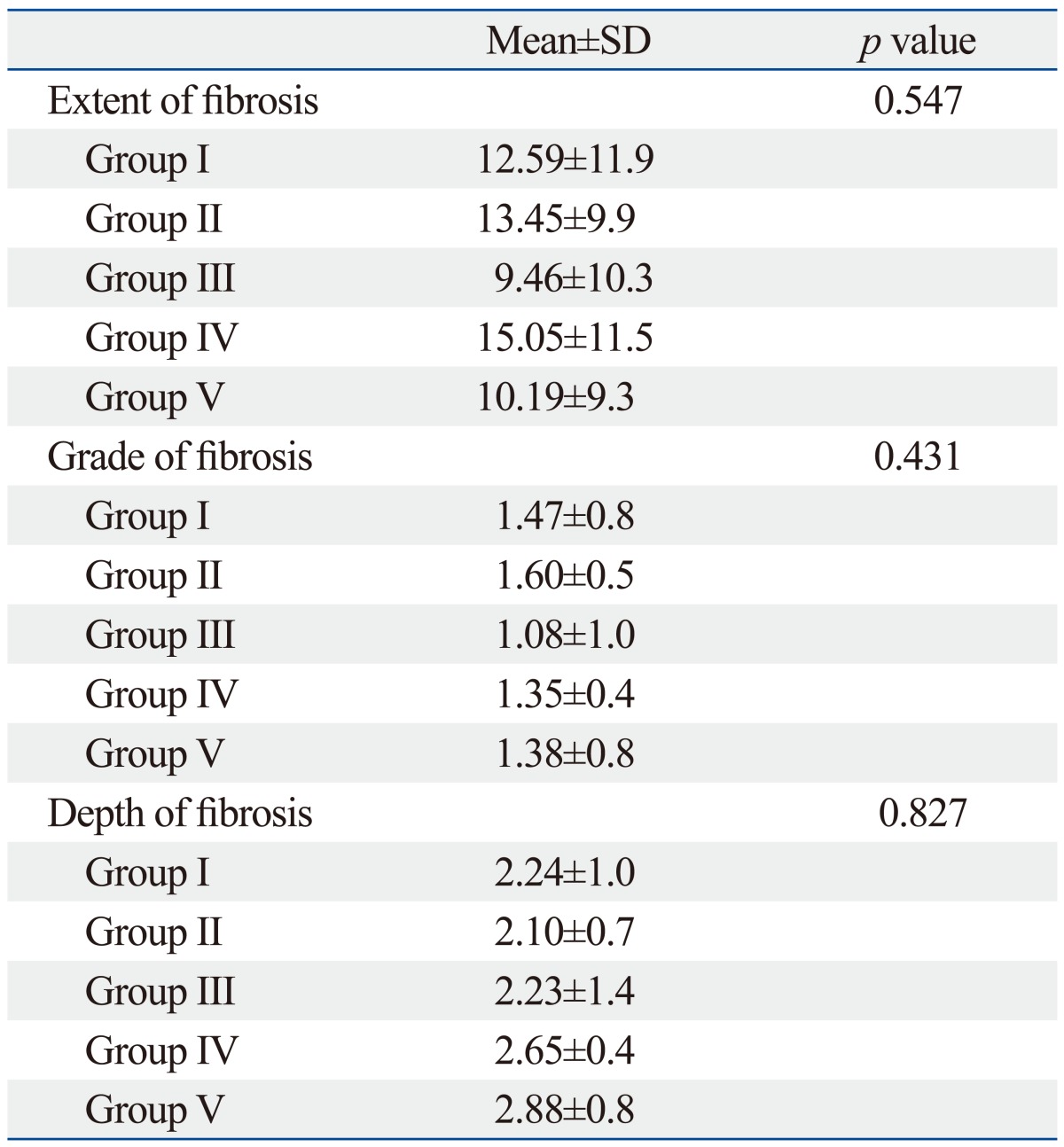
The degree of fibrosis (extent, grade and depth) was analyzed and the group III showed the least fibrosis in the extent, grade and depth. Although the group III showed the intergroup difference with the group I (control group), the observed data could not reveal any statistical significance in the whole group analysis (Table 5).
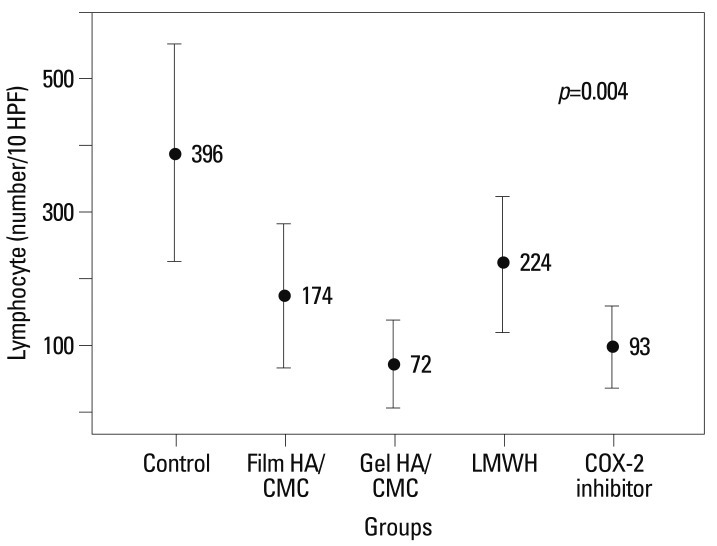
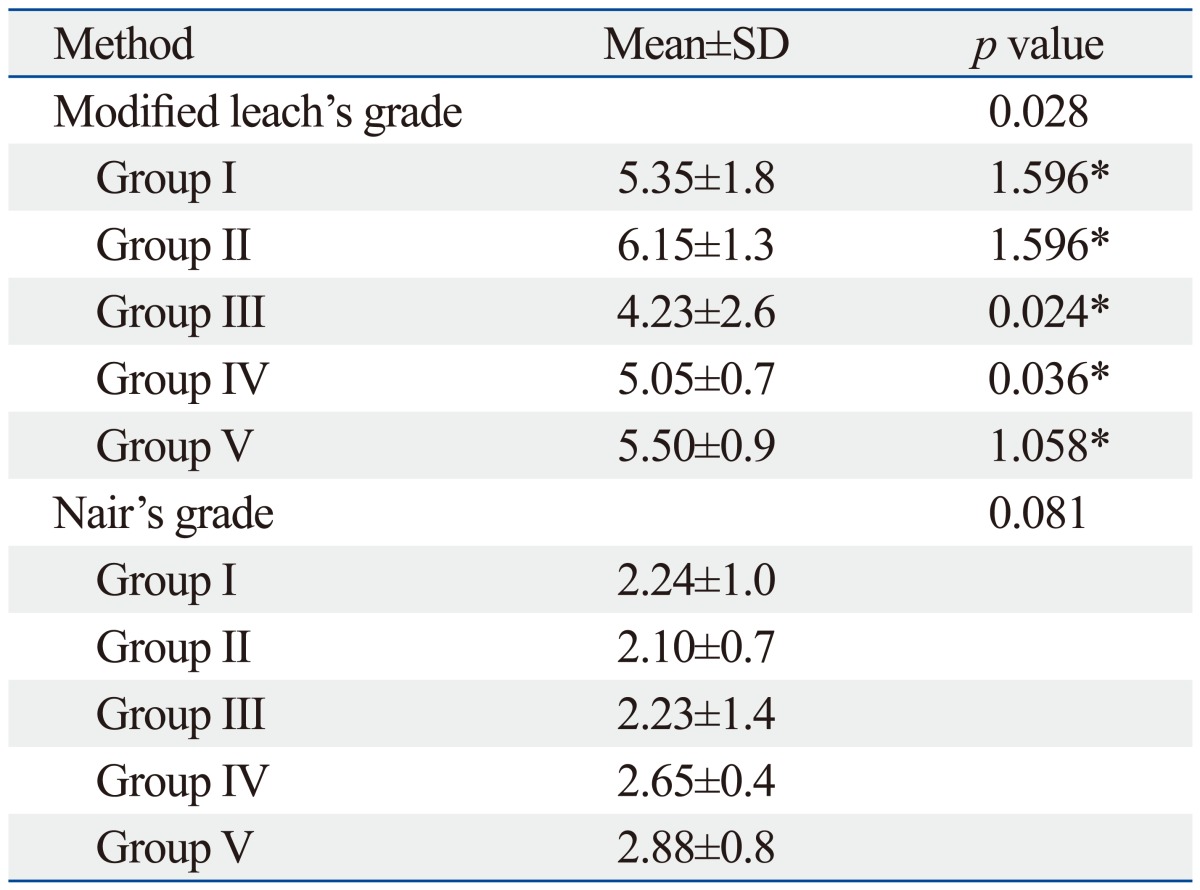
Table 5.
Histologic Degree of Fibrosis
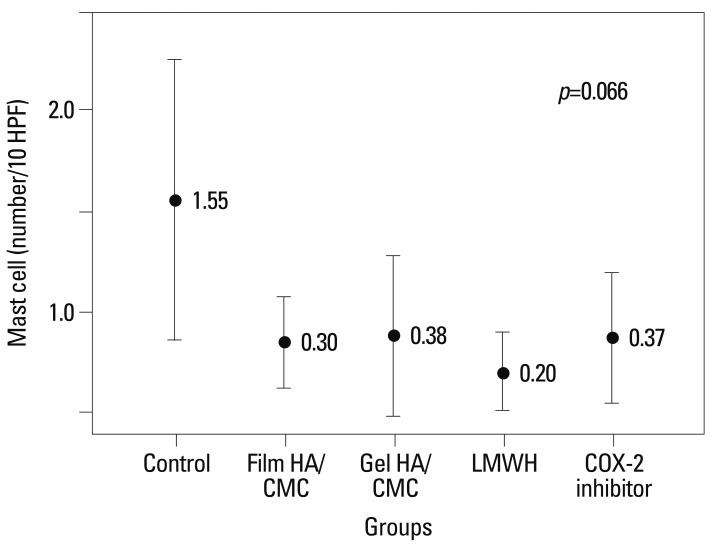
The inflammation degree was evaluated according to the number of inflammatory cells (neutrophils, macrophages, lymphocytes, giant cells, and mast cell) under the 10 HPFs. The cell count of macrophages showed intergroup differences, and the least numbers were detected in the group III and V (group I: 56.6, group II: 33.50, group III: 16.9, group IV: 24.7, group V: 15.4, p=0.383). The number of lymphocyte was significantly low in group III (74) and group V (93) compared to other groups (group I: 390, group II: 174, group IV: 224, p=0.004) (Fig. 3). The mast cell count was generally low except the control group (group I: 1.05, group II: 0.35, group III: 0.38, group IV: 0.20, group V: 0.37) and it was not statistically significant (p=0.066) (Fig. 4).
Fig. 3.
Lymphocyte counts according to the groups. HA/CMC, hyaluronic acid/carboxymethylcellulose; LMWH, low molecular weight heparin; COX-2 inhibitor, cyclo-oxygenase-2 inhibitor; HPF, high power fields.
Fig. 4.
Mast cell counts according to the groups. HA/CMC, hyaluronic acid/carboxymethylcellulose; LMWH, low molecular weight heparin; COX-2 inhibitor, cyclo-oxygenase-2 inhibitor; HPF, high power fields.
The numbers of neutrophils (group I: 799.6, group II: 351.1, group III: 106, group IV: 115.5, group V: 126, p=0.115) and giant cells (group I: 8.59, group II: 5.8, group III: 2.4, group IV: 5.7, group V: 2.3, p=0.118) were low in treated groups (group II-V), but there were no statistical differences within the treated groups.
DISCUSSION
Surgical trauma is considered to be the major clinical factor related to the pathogenesis of intra-abdominal adhesions.1 This surgical procedures (incision, cauterization, suturing, ischemia, desiccation abrasion) easily make the injury to peritoneal surfaces, leading to inflammatory processes and fibrosis between tissues and organs.1 In the absence of resolution of fibrinous mass by fibrinolysis, fibroblasts migrate into the fibrinous mass from the injured tissue surfaces. Then, collagen and other forms of extracellular matrix could be deposited with the subsequent development of a permanent adhesion.6 Therefore, the adhesion can lead to significant morbidity and mortality including strangulation, obstruction, necrosis of bowel loops and/or infertility and organ injury during repeated abdominal surgery. One cohort study reported that 34.7% of patients in the open abdominal surgery experienced at least one outcome readmission over 10 years.7
The generally accepted concept for preventing adhesion formation during surgery is to minimize surgical trauma. Besides minimizing surgical trauma, other factors may influence adhesion formation, such as using materials which form foreign body reaction, including starch from surgical gloves, suture materials, mesh and the duration of surgery. Therefore, the adjuvant materials are needed to reduce adhesion development if surgical techniques are inevitable.
Despite the extensive efforts undertaken to prevent peritoneal adhesion formation, no single method has thus far been successful. As a result, several studies have been performed using different substances and various drugs that may, by acting locally or systemically via different mechanisms of action, safely and efficaciously reduce the incidence, severity and extent of postoperative adhesions in different experimental settings.8-10 Mast cells have been shown to play a significant role in the early inflammatory stage of wound healing and also influence proliferation of tissue. Macrophages are essential contributors towards the resolution of inflammation and can produce profibrotic mediators. Other inflammatory cells are related with the several mediators (e.g. IL-6, 8, TNF-α, IL-1β, IL-6, TGF-β) which lead to an activation of the extrinsic cascade initially resulting in fibrin matrix. This matrix will be organized further, thereby forming peritoneal adhesion.
The film types of HA/CMC and gel type HA/CMC were generated as a synthetic barrier. They remain in the peritoneum for approximately 7-10 days after applying and gradually degrade because of the presence of cross-linked carboxymethylcellulose.5,11-13 As such, they are going to work by separating the injured tissue from other tissue surfaces during the initial postoperative time period while remesotheliazation is occurring, a process that is usually expected to take 3 to 5 days. Retrospective analysis and a randomized controlled trial revealed the safety and efficacy in reducing postoperative adhesion development after intra-abdominal surgery.14-16 Another study showed that the patients group using the HA/CMC had less disability and a lower incidence of pectoralis tightness than the control group, but the difference was not significant.17 In our study, both film types of HA/CMC and gel type of HA/CMC showed the reduction of inflammatory cells (macrophage, lymphocyte and mast cell), but only the gel type of HA/CMC had a benefit in the grade of adhesion, whereas other experiments did not show the same pattern of difference of adhesion grade between film type of HA/CMC and gel type of HA/CMC. Although we were unable to clarify the precise reason behind the difference between the film type and gel type, one possible reason could be the difference in the completeness of the covering. Namely, the film type HA/CMC is fragile and thus difficult to wrap the wound on a curved surface. On the other hand, the gel type of HA/CMC can cover the entire surface of the injured site, hence the adhesion would be less cohesive in comparison to the film type.
Several systemic agents have been proposed to prevent postoperative abdominal adhesions.5,11,18,19 However, it is hard to evaluate the relative effect of adhesion preventions among the anti-adhesive agents. The agents used for this purpose may be divided mainly into two groups as having local and systemic effects. COX-2 inhibitor is one of the familiar NSAID known for its anti-angiogenic effect and anti-fibroblastic activity.6,11 These anti-angiogenic effect and anti-fibroblastic activity could attenuate the adhesion formation. However, our data based on the number of the anti-inflammatory cells (lymphocyte), showed only an anti-inflammatory effect without any preventive effect of the adhesion and fibrosis. Unfortunately, some COX-2 inhibitors exhibited a considerable amount of cardiovascular toxicities, thus no further study was available to investigate the preventive effect of adhesion.
Heparin is used as an anticoagulant agent, having an inhibitor effect of fibrin formation. Therefore, it was used for the prevention of adhesions.8 However, it is not easy to use in immediate postoperative period due to bleeding tendency. The LMWH also prevents clot formation and reduces the adhesion formation. Accordingly, we used the LMWH which has minimal bleeding tendency for immediate administration after surgery. However, our data did not reveal any benefit in the reduction of adhesion and fibrosis, and showed only anti-inflammatory effect, evidenced by low number of inflammatory cells. Other animal study using heparin suggested the possibility of high dose to prevent adhesion.8,17 The study using the combination of heparin and film type of HA/CMC did not show any additive heparin effect.8 Therefore, further studies are needed to determine the preventive effect of adhesion and suitable dose.
In conclusion, our data showed that the gel type of HA/CMC is partly efficient in inhibiting the formation of postoperative adhesions and may provide an option for abdominal surgery to reduce postoperative adhesions among the anti-adhesive materials. While the LMWH and NSAID did exhibit anti-inflammatory effects, their preventive effects in adhesion and fibrosis still remain obscure. Thus, there is a need for more randomized studies and clinical investigation of combination of anti-adhesive agents.
ACKNOWLEDGEMENTS
This work was supported by the Ewha Womans University Research Grant.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 2.Menzies D. Peritoneal adhesions. Incidence, cause, and prevention. Surg Annu. 1992;24(Pt 1):27–45. [PubMed] [Google Scholar]
- 3.Vrijland WW, Jeekel J, van Geldorp HJ, Swank DJ, Bonjer HJ. Abdominal adhesions: intestinal obstruction, pain, and infertility. Surg Endosc. 2003;17:1017–1022. doi: 10.1007/s00464-002-9208-9. [DOI] [PubMed] [Google Scholar]
- 4.Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18:260–273. doi: 10.1159/000050149. [DOI] [PubMed] [Google Scholar]
- 5.Diamond MP, Wexner SD, diZereg GS, Korell M, Zmora O, Van Goor H, et al. Adhesion prevention and reduction: current status and future recommendations of a multinational interdisciplinary consensus conference. Surg Innov. 2010;17:183–188. doi: 10.1177/1553350610379869. [DOI] [PubMed] [Google Scholar]
- 6.Saed GM, Zhang W, Chegini N, Holmdahl L, Diamond MP. Transforming growth factor beta isoforms production by human peritoneal mesothelial cells after exposure to hypoxia. Am J Reprod Immunol. 2000;43:285–291. doi: 10.1111/j.8755-8920.2000.430507.x. [DOI] [PubMed] [Google Scholar]
- 7.Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–1480. doi: 10.1016/S0140-6736(98)09337-4. [DOI] [PubMed] [Google Scholar]
- 8.Avsar FM, Sahin M, Aksoy F, Avsar AF, Aköz M, Hengirmen S, et al. Effects of diphenhydramine HCl and methylprednisolone in the prevention of abdominal adhesions. Am J Surg. 2001;181:512–515. doi: 10.1016/s0002-9610(01)00617-1. [DOI] [PubMed] [Google Scholar]
- 9.Karaca T, Gözalan AU, Yoldaş Ö, Bilgin BÇ, Tezer A. Effects of tamoxifen citrate on postoperative intra-abdominal adhesion in a rat model. Int J Surg. 2013;11:68–72. doi: 10.1016/j.ijsu.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Kement M, Censur Z, Oncel M, Buyukokuroglu ME, Gezen FC. Heparin for adhesion prevention: comparison of three different dosages with Seprafilm in a murine model. Int J Surg. 2011;9:225–228. doi: 10.1016/j.ijsu.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 11.Schreinemacher MH, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND. Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg. 2009;96:305–313. doi: 10.1002/bjs.6446. [DOI] [PubMed] [Google Scholar]
- 12.Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG, et al. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003;46:1310–1319. doi: 10.1007/s10350-004-6739-2. [DOI] [PubMed] [Google Scholar]
- 13.Lalountas MA, Ballas KD, Skouras C, Asteriou C, Kontoulis T, Pissas D, et al. Preventing intraperitoneal adhesions with atorvastatin and sodium hyaluronate/carboxymethylcellulose: a comparative study in rats. Am J Surg. 2010;200:118–123. doi: 10.1016/j.amjsurg.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Diamond MP, Burns EL, Accomando B, Mian S, Holmdahl L. Seprafilm® adhesion barrier: (1) a review of preclinical, animal, and human investigational studies. Gynecol Surg. 2012;9:237–245. doi: 10.1007/s10397-012-0741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dietrich A, Bouzidi M, Hartwig T, Schütz A, Jonas S. Rapamycin and a hyaluronic acid-carboxymethylcellulose membrane did not lead to reduced adhesion formations in a rat abdominal adhesion model. Arch Gynecol Obstet. 2012;285:1603–1609. doi: 10.1007/s00404-011-2184-3. [DOI] [PubMed] [Google Scholar]
- 16.Hashimoto D, Hirota M, Yagi Y, Baba H. Hyaluronate carboxymethylcellulose-based bioresorbable membrane (Seprafilm) reduces adhesion under the incision to make unplanned re-laparotomy safer. Surg Today. 2012;42:863–867. doi: 10.1007/s00595-012-0191-z. [DOI] [PubMed] [Google Scholar]
- 17.Yang EJ, Kang E, Jang JY, Kim D, Yom CK, Lim JY, et al. Effect of a mixed solution of sodium hyaluronate and carboxymethyl cellulose on upper limb dysfunction after total mastectomy: a double-blind, randomized clinical trial. Breast Cancer Res Treat. 2012;136:187–194. doi: 10.1007/s10549-012-2272-5. [DOI] [PubMed] [Google Scholar]
- 18.Imai A, Takagi H, Matsunami K, Suzuki N. Non-barrier agents for postoperative adhesion prevention: clinical and preclinical aspects. Arch Gynecol Obstet. 2010;282:269–275. doi: 10.1007/s00404-010-1423-3. [DOI] [PubMed] [Google Scholar]
- 19.Aksakal O, Yilmaz B, Gungor T, Sirvan L, Sut N, Inan I, et al. A randomised controlled trial on melatonin and rosiglitazone for prevention of adhesion formation in a rat uterine horn model. Arch Gynecol Obstet. 2010;282:55–61. doi: 10.1007/s00404-009-1240-8. [DOI] [PubMed] [Google Scholar]