Abstract
Purpose
High sensitive C-reactive protein (hs CRP) is well known as a strong risk factor of cardiovascular disease (CVD). The aim of this study is to evaluate the impact of elevated hs CRP on coronary artery spasm (CAS) as assessed by intracoronary acetylcholine (ACh) provocation test.
Materials and Methods
A total of 1729 consecutive patients without significant CVD who underwent coronary angiography and intracoronary ACh test between November 2004 and August 2010 were analyzed. The patients were divided into five groups according to quintiles of hs CRP levels.
Results
At baseline, the prevalence of elderly, hypertension, diabetes mellitus, current smoking, and lipid levels were higher in patients with higher hs CRP. During ACh test, the incidences of significant CAS, ischemic electrocardiography (EKG) change, multivessel, and diffuse CAS were higher in patients with higher hs CRP. Multivariate analysis showed that the old age (OR=1.01, CI; 1.0-1.02, p=0.0226), myocardial bridge (OR=3.34, CI; 2.16-5.17, p<0.001), and highest quintile hs CRP (OR=1.54, CI; 1.12-2.18, p=0.008) were independent predictors of ACh induced CAS. However, there was no difference in clinical outcomes up to 12 months.
Conclusion
In conclusion, higher hs CRP was associated with higher incidence of CAS, worse angiographic characteristics and ischemic EKG change, but was not associated with clinical outcomes.
Keywords: C-reactive protein, acetylcholine, coronary artery spasm
INTRODUCTION
The mechanism of coronary artery spasm (CAS) is not yet precisely known. However, endothelial dysfunction is known to be a major cause of CAS, and inflammations worsen the endothelial dysfunction. C-reactive protein (CRP) is a sensitive systemic inflammation marker, and especially high sensitivity CRP (hs CRP), even in the previously considered normal range, is known to be a predictor of cardiovascular events in apparently healthy individuals.1 Furthermore, recent study shows that the patients with CAS had the elevated hs CRP level.2 In the present study, we assessed the clinical and angiographic characteristics with intracoronary acetylcholine (ACh) provocation test among the five patients groups according to quintiles of hs CRP levels, and evaluated the impact of elevated hs CRP level on the major cardiovascular clinical outcomes up to 12 months.
MATERIALS AND METHODS
Study population
This study is a retrospective observational study. A total of 5832 patients underwent coronary angiography from November 2004 to August 2010 in the Cardiovascular Center of the Korea University Guro Hospital. Among them, 2053 patients who had typical or atypical chest pain and had been diagnosed by coronary angiography with insignificant coronary artery disease (CAD), underwent intracoronary ACh provocation test. The exclusion criteria of this study was referenced with previous our studies.3,4 We excluded the patients with one of the following conditions such as prior coronary artery bypass graft, prior percutaneous coronary intervention, prior cerebrovascular disease, advanced heart failure (New York Heart Association class III or IV), or serum creatinine ≥3 mg/dL. Finally, a total of 1727 patients were enrolled for the analysis. Study populations were divided into five groups according to quintiles of the hs CRP level: C1 (hs CRP: 0-0.31 mg/L), C2 (hs CRP: 0.31-0.53 mg/L), C3 (hs CRP: 0.54-0.92 mg/L), C4 (hs CRP: 0.93-2.34 mg/L), and C5 (hs CRP: >2.34 mg/L). hs CRP samples were taken before angiography in every patient if there is no evidence of recent infection or inflammatory conditions. Clinical and angiographic characteristics during the ACh provocation test were compared among the five groups.
Acetylcholine provocation test
The method of acetylcholine provocation test in this study was referenced with previous our studies.3,4 Nitrates, calcium channel blockers (CCB), beta blockers (BB), angiotension-converting enzyme inhibitors (ACEI) and other vasodilators or vasoconstrictors was discontinued at least 72 hours before the coronary angiography. The provocation test of CAS was performed with intracoronary injection of ACh immediately after diagnostic angiography by either transradial or transfemoral approach. ACh was injected with incremental doses of 20 (A1), 50 (A2) and 100 (A3) µg/min into the left coronary artery over a 1 minute period with 5 minutes intervals to the maximum tolerated dose. Angiography was performed after each ACh dose until significant focal or diffuse narrowing more than 70% was visually achieved. If focal or diffuse significant vasoconstriction (>70%) of coronary arteries was induced with any dose of ACh, the ACh infusion was stopped. Coronary artery diameters were measured using the proper quantitative coronary angiographic (QCA) system of the catheterization laboratory (FD-20, Phillips, Amsterdam, the Netherlands) before and after administration of ACh. Reference vessel diameters were analyzed at the proximal and distal portions of each artery. The mean reference vessel diameter was used to assess the diameter narrowing by QCA. During the coronary angiography and ACh provocation test, significant CAS was defined as an abnormal significant constriction of an epicardial coronary artery resulting in transient myocardial ishemia. Myocardial bridge (MB) was defined with characteristic phasic systolic compression of the coronary artery on the angiogram. Multivessel spasm (MVS) was defined with significant CAS of ≥2 major epicardial coronary arteries. The presences of baseline spasm was defined with focal or diffuse narrowing more than 30% in diameter on the angiogram before the ACh provocation test. Diffuse CAS was defined with significant CAS site length ≥20 mm.
Study definition
The study definition of this study was referenced with previous our studies.3,4 Hypertension was defined with elevation of blood pressure ≥140/90 mm Hg or current treatment of antihypertensive drugs. Dyslipidemia was defined with a total cholesterol level ≥200 mg/dL or current treatment with lipid-lowering drugs. Current smoking was defined with active smoking within the past 12 months. Diabetes mellitus was defined with the fasting blood glucose level ≥126 mg/dL, or current treatment with hypoglycemic drugs or insulin. Insignificant coronary artery disease (CAD) was defined with the ≤20% diameter stenosis in coronary arteries documented by image studies including computed tomographic angiography, magnetic resonance angiography or invasive angiography.
Statistical analysis
All the statistical analyses were performed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA). For continuous variables, differences among the five groups were evaluated by ANOVA. For discrete variables, differences were expressed as counts and percentages, and analyzed with χ2 test among the five groups as appropriate. Multivariate logistic regression analysis, which included baseline confounding factors, was used for assessing the independent impact factors. A two-tailed p-value of <0.05 was considered to be statistically significant. Data were expressed as mean±standard deviations.
RESULTS
Among a total of 2053 patients, the proportion of acute coronary syndrome was 7.7% (158/2053), and the percentage of positive stress test was 6.0% (123/2053). The first investigations for CAS were stress test such as treadmill and stress echocardiography or direct invasive coronary angiography.
To assess the association between hs CRP and ACh induced CAS, the pts were divided into five groups according to quintiles of hs CRP levels: C1 (hs CRP: 0-0.31 mg/L), C2 (hs CRP: 0.31-0.53 mg/L), C3 (hs CRP: 0.54-0.92 mg/L), C4 (hs CRP: 0.93-2.34 mg/L), and C5 (hs CRP: >2.34 mg/L). The baseline clinical characteristics of patients are shown in Table 1. The prevalence of elderly, diabetes mellitus, hypertension, current smoking, and body mass index (BMI) were higher in patients with higher hs CRP. Platelet count, white blood cell count, creatinine, fasting glucose, and glycated hemoglobin (HbA1c) level were higher in patients with higher hs CRP. Lipid levels including total cholesterol, triglyceride, and low density lipoprotein-cholesterol, and erythrocyte sedimentation rate, and N-terminal pro brain type natriuretic peptide were higher in patients with higher hs CRP. Before the ACh test, the prescription of BB, CCB, ACEI, nitrate, and lipid-lowering drugs were similar among the five quintiles of pts. However, aspirin was more frequently prescribed in patients with higher hs CRP.
Table 1.
The Baseline Clinical Characteristics of Study Groups
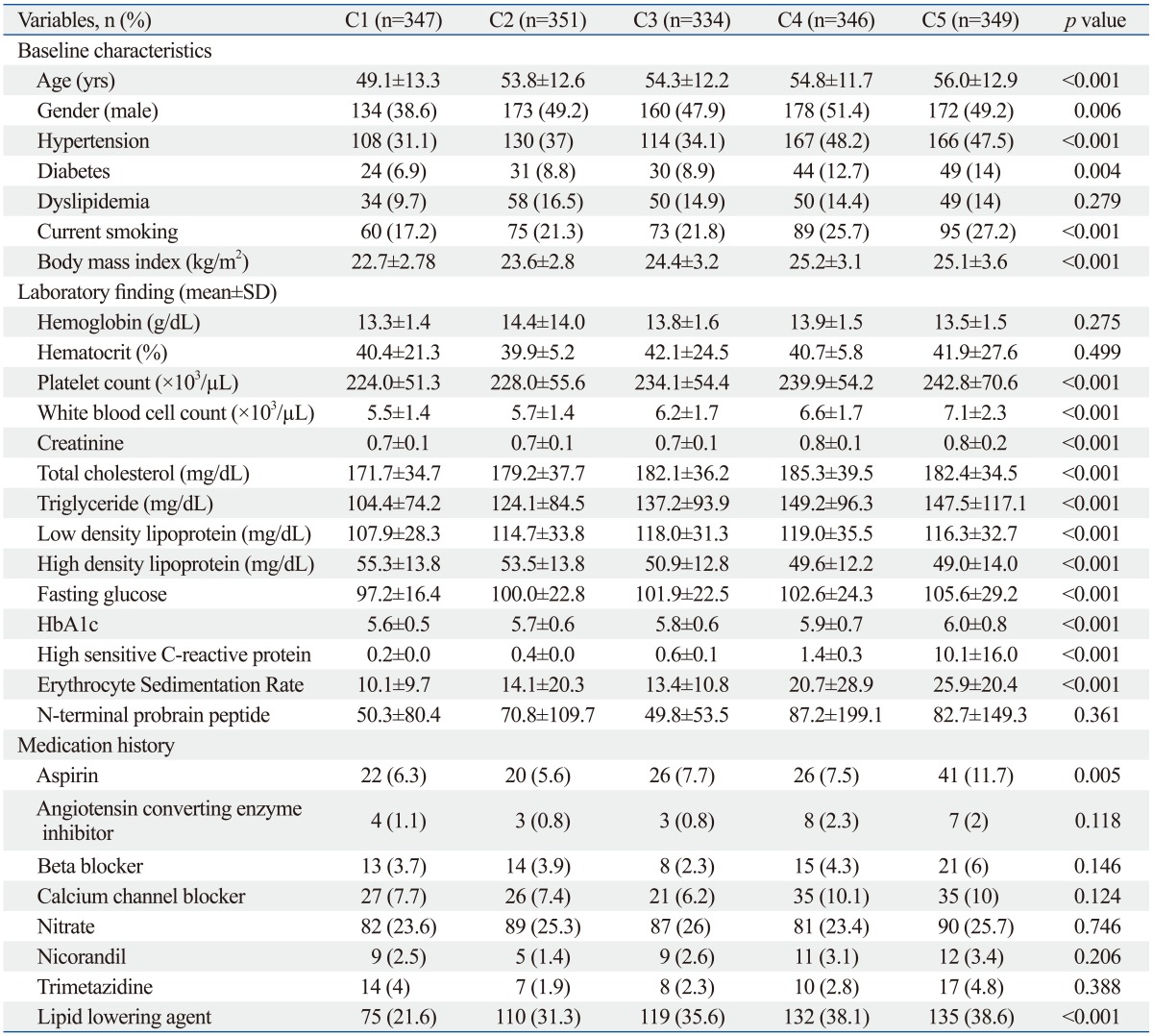
SD, standard deviation.
C1 (hs CRP: 0-0.31 mg/L), C2 (hs CRP: 0.31-0.53 mg/L), C3 (hs CRP: 0.54-0.92 mg/L), C4 (hs CRP: 0.93-2.34 mg/L), and C5 (hs CRP: >2.34 mg/L).
The clinical and angiographic parameters of the ACh provocation test are shown in Table 2.
Table 2.
The Clinical and Angiographic Parameters during ACh Provocation Test
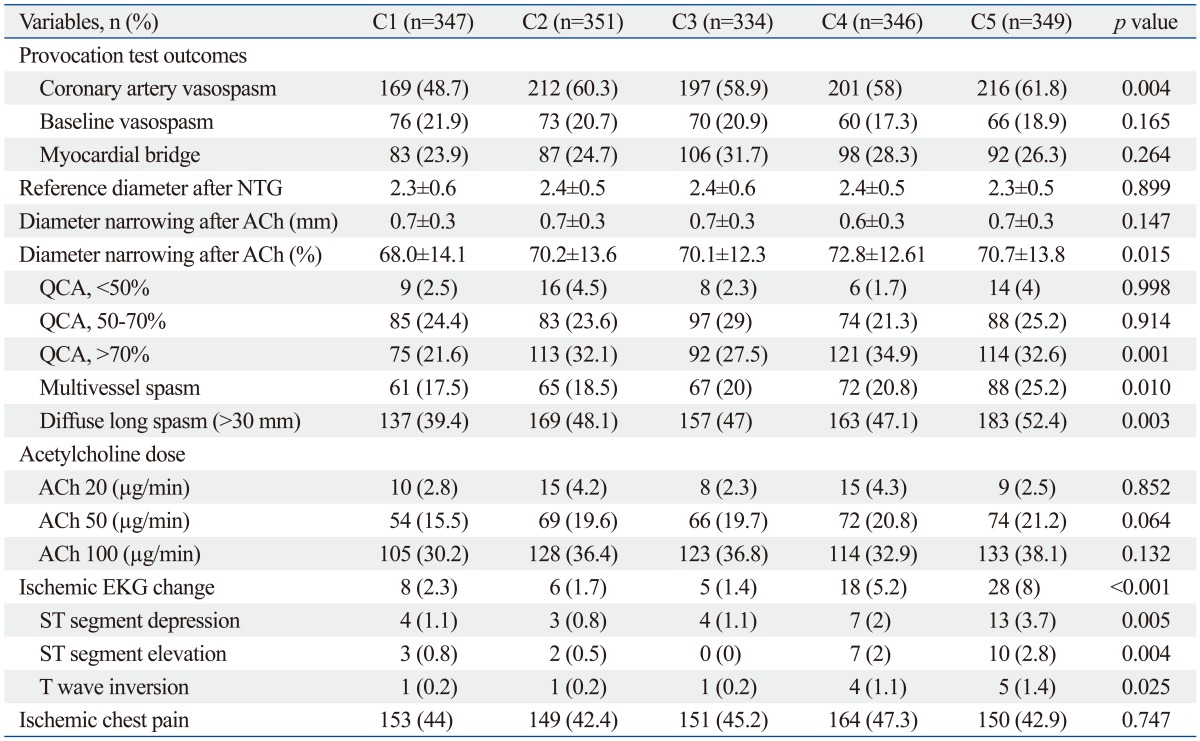
ACh, acetylcholine; QCA, quantitative coronary angiographic; EKG, electrocardiography; NTG, nitroglycerin.
At baseline coronary angiogram before the ACh provocation test, the incidences of baseline spasm were higher in patients with higher hs CRP. QCA was performed in five quintiles of patients, and the QCA results are shown in Table 2. NTG was infused after completion of the ACh provocation not before ACh-test. The reference diameters were similar among the five quintiles of patients. However, after ACh infusion, diameter narrowing (%) by QCA significantly increased in the pts with higher hs CRP. During the ACh test, the incidences of ischemic EKG changes were most frequently developed in patients with higher hs CRP.
The overall rate of positive ACh provocation test which shows significant CAS was significantly higher in the patients with higher hs CRP. The results for response to the ACh doses and spasm extent are shown in Table 2, and the incidence of diffuse and multivessel spasm (MVS) was frequently observed more in patients with higher hs CRP. Clinical outcomes during twelve months are shown in Table 3. Total mortality was 0.17% (3/1729), and cardiac death out of them was 0.11% (2/1729) and non-cardiac death was 0.05% (1/1729). The incidence of percutaneous revascularization was 0.4% (7/1729) and cerebrovascular accident was 0.05% (1/1729).
Table 3.
12 Months Clinical Outcomes
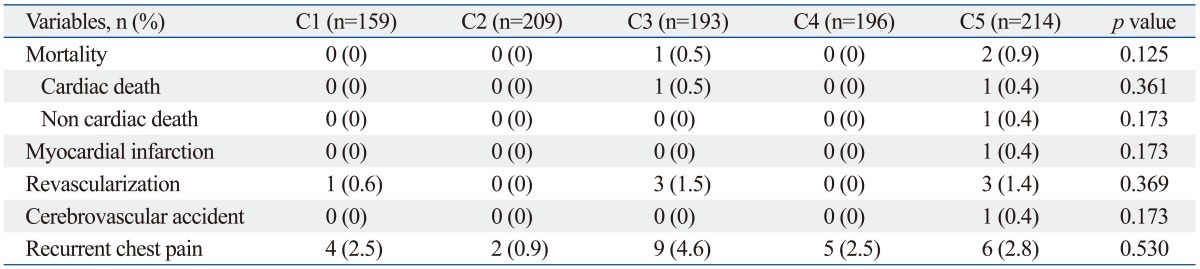
The incidence of recurrent chest pain was 1.5% (26/1729). However, there was no difference among the five quintiles of patients. We evaluated independent predictors for ACh-induced CAS by adjusting possible baseline confounding factors such as age, gender, body mass index (BMI), hypertension, diabetes mellitus, hyperlipidemia, current smoking, peripheral artery disease (PAD), and medication history including aspirin, BB, CCB, cilostazol, ACEI, nitrate, lipid lowering agents, and presence of angiographic baseline spasm, and myocardial bridge. Multivariate analysis showed that C5 versus C1 (OR=1.5, p=0.0079, 95% CI=1.1-2.1) and MB (OR=3.3, p<0.001, 95% CI=2.1-5.1) were independent predictors of ACh induced CAS. Other classical coronary risk factors including hypertension, current smoking, diabetes mellitus, and hyperlipidemia were not independent predictors of CAS (Table 4).
Table 4.
Multivariable Logistic Analysis of the Predictors of ACh Induced CAS
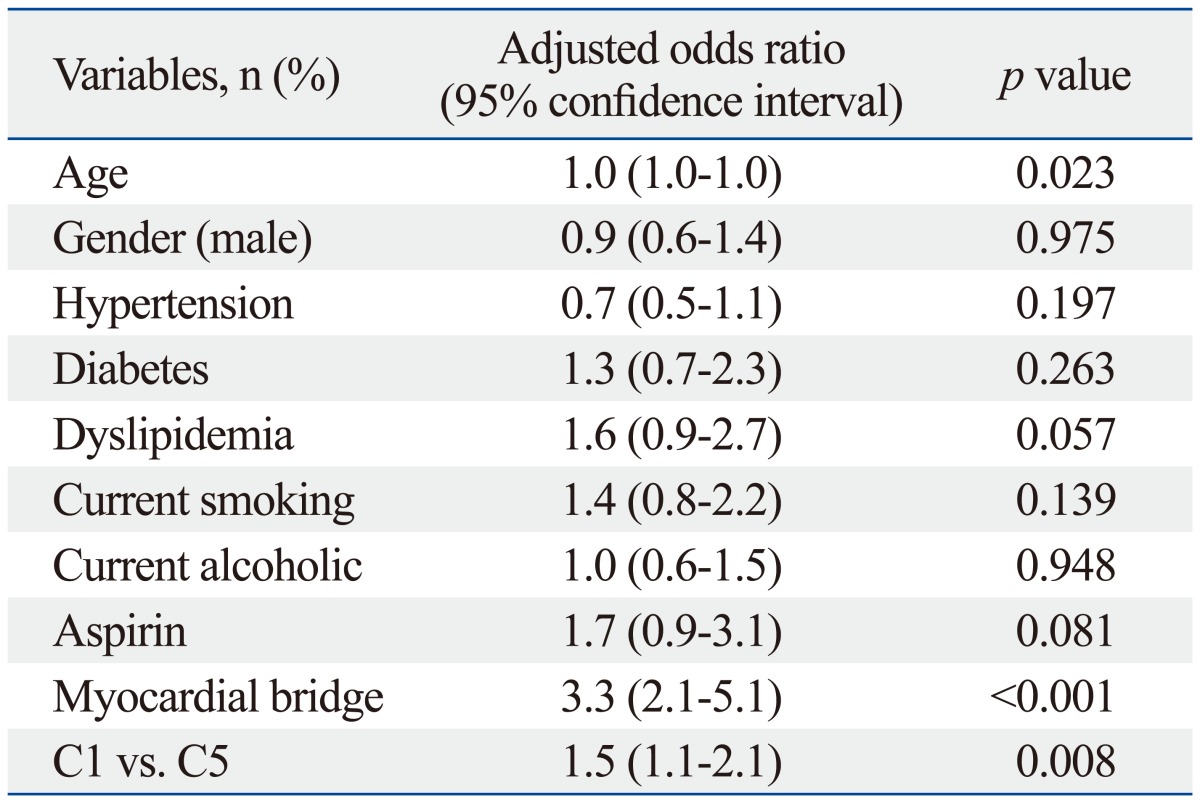
ACh, acetylcholine; CAS, coronary artery spasm.
DISCUSSION
The main findings of the present study are that the elevated hs CRP was associated with higher incidence of ischemic EKG change during the ACh provocation test, significant CAS, diffuse and multivessel CAS, suggesting that inflammation may trigger significant CAS. Therefore the patients with CAS documented by ACh test and concomitant elevated hs CRP would require more aggressive and intensive medical therapies including CCB, long acting nitrate and nicorandil in real world clinical practice. In the present study, MB was an independent predictor of ACh-induced CAS. We have reported that the patients with MB had a higher incidence of ACh-induced CAS than those of control group (p<0.001), and these results led us to consider that longstanding compression-relaxation stress of MB may cause endothelial dysfunction of coronary arteries, which may increase the risk of CAS.5 CAS is primarily due to vascular smooth muscle hyper-reactivity with endothelial dysfunction playing a major role, although inflammation is also believed to be important.
During the ACh test, the elevated hs CRP group had higher incidence of ischemic EKG changes, compared with normal hs CRP group. However, the frequencies of antianginal agents such as CCB and nitrate were similar between the two groups. Therefore, the patients with elevated hs CRP group would require more aggressive medical treatment with antianginal agents.
In the present study, the incidence of positive ACh provocation test after ACh infusion was frequent more in the elevated hs CRP group. Furthermore, mean % narrowing and minimal luminal diameter (mm) by QCA were more severe in the elevated hs CRP group, suggesting that these angiographic characteristics may induce worse clinical symptoms and signs not only during the ACh test, but also their future clinical course.
In the present study, the elevated hs CRP group required more low to intermediate dose (20-50 µg/min) of ACh to induce significant CAS. These results suggest that the elevated hs CRP group showed response more vulnerable to a lower dose of ACh stimuli and have a higher chance of having significant CAS than normal hs CRP group in real world clinical practice even with less strong stimuli.
In the present study, elevated hs CRP itself was an independent predictor of ACh induced CAS, regardless of other coexisting factors. The mechanism of CAS is not yet clearly known.6,7 However, endothelial dysfunction and inflammation are known to be a major cause of CAS. Several previous studies have demonstrated the relationship between inflammation and CAS. In 1978, Lewis, et al.8 first reported a case of CAS associated with inflammation. Since Shimokawa, et al. developed a swine model, and reported that CAS induced by chronically applying IL-β was related to elevated adhesion-molecule such as P-selectin.9 Hung, et al.2 prospectively investigated the effect of hs CRP, a sensitive marker of inflammation, on CAS with 428 patients who had no significant coronary artery disease, and reported that hs CRP level was an independent factor of CAS. Itoh, et al.10 reported that minor elevation of serum hs CRP values, even within the range previously considered normal, is also significantly associated with CAS. These results suggest that patients with elevated hs CRP have higher chance of having CAS than those of control group, suggesting systemic involvement of endothelial dysfunction and subsequent early atherosclerosis.
There are some limitations in this study. Routine ACh provocation test to the right coronary artery was not done due to safety issues by higher prevalence of advanced atrioventricular (AV) block which needs temporary pacemaker for maintaining adequate ACh infusion rate and subsequent cost effectiveness for diagnosis and management of significant CAS. Angiography was repeated after each ACh dose until significant focal or diffuse narrowing more than 70% was visually achieved. This means that calling a reaction "epicardial spasm" was quite subjective. On the other hand the offline QCA was performed correcting for the inevitable subjectivity. The first investigations for CAS were angiogram or stress test such as treadmill and stress echocardiography. However, the definition of CAS in this study was based purely on coronary angiography, which is more relevant for significant endothelial dysfunction and this may occur at the site of a muscle bridge without any clinical symptoms.
In conclusion, the present study showed that elevated hs CRP itself was an independent predictor of ACh induced CAS, regardless of other coexisting factors. Old age and the presence of myocardial bridge were also independent risk factors of ACh induced CAS. Elevated hs CRP was associated with more severe and vulnerable to lower dose of ACh provocation test than those of control group. The patients with elevated hs CRP had more frequent ischemic EKG changes than those of control group during ACh provocation test. Therefore, patients with elevated hs CRP who were diagnosed as CAS by ACh provocation test also would need more intensive medical treatment as compared to control group. However, there were no difference in 12 months clinical outcomes among five groups.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 2.Hung MJ, Cherng WJ, Yang NI, Cheng CW, Li LF. Relation of high-sensitivity C-reactive protein level with coronary vasospastic angina pectoris in patients without hemodynamically significant coronary artery disease. Am J Cardiol. 2005;96:1484–1490. doi: 10.1016/j.amjcard.2005.07.055. [DOI] [PubMed] [Google Scholar]
- 3.Park JY, Rha SW, Poddar KL, Ramasamy S, Chen KY, Li YJ, et al. Impact of low-dose aspirin on coronary artery spasm as assessed by intracoronary acetylcholine provocation test in Korean patients. J Cardiol. 2012;60:187–191. doi: 10.1016/j.jjcc.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Park JY, Rha SW, Jin Z, Poddar KL, Ramasamy S, Chen KY, et al. Multivessel versus single vessel spasm, as assessed by the intracoronary acetylcholine provocation test, in Korean patients. Clin Exp Pharmacol Physiol. 2011;38:819–823. doi: 10.1111/j.1440-1681.2011.05611.x. [DOI] [PubMed] [Google Scholar]
- 5.Kim JW, Park CG, Suh SY, Choi CU, Kim EJ, Rha SW, et al. Comparison of frequency of coronary spasm in Korean patients with versus without myocardial bridging. Am J Cardiol. 2007;100:1083–1086. doi: 10.1016/j.amjcard.2007.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Sugiishi M, Takatsu F. Cigarette smoking is a major risk factor for coronary spasm. Circulation. 1993;87:76–79. doi: 10.1161/01.cir.87.1.76. [DOI] [PubMed] [Google Scholar]
- 7.Xiang D, Kleber FX. Smoking and hyperlipidemia are important risk factors for coronary artery spasm. Chin Med J (Engl) 2003;116:510–513. [PubMed] [Google Scholar]
- 8.Lewis JR, Kisilevsky R, Armstrong PW. Prinzmetal's angina, normal coronary arteries and pericarditis. Can Med Assoc J. 1978;119:36–39. [PMC free article] [PubMed] [Google Scholar]
- 9.Kaikita K, Ogawa H, Yasue H, Sakamoto T, Suefuji H, Sumida H, et al. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation. 1995;92:1726–1730. doi: 10.1161/01.cir.92.7.1726. [DOI] [PubMed] [Google Scholar]
- 10.Itoh T, Mizuno Y, Harada E, Yoshimura M, Ogawa H, Yasue H. Coronary spasm is associated with chronic low-grade inflammation. Circ J. 2007;71:1074–1078. doi: 10.1253/circj.71.1074. [DOI] [PubMed] [Google Scholar]


