Abstract
Outcome predictors between two methadone maintenance treatment clinics in Tel-Aviv, Israel, and Las Vegas, Nevada, were determined by comparing patients’ characteristics. All patients admitted to the two clinics (302 from Las Vegas and 492 from Tel-Aviv) were studied with respect to variables at admission and follow-up. Las Vegas patients were older, contained more females, had more hepatitis C positive markers, and more urine analyses that were positive for cocaine, amphetamines, and tetrahydrocannabinol (THC) on admission than the Tel-Aviv patients. After 1 year, Tel-Aviv patients had higher retention (73.6% vs. 61.6%) and similar opiate abstinence (65.8% vs. 64.9%) compared to Las Vegas patients. Predictors for cumulative retention (Cox regression) for both clinics were higher methadone dosages greater than or equal to 100 mg/day (Tel-Aviv OR [odds ratio] = 2.1, 95% confidence interval [CI] = 1.6–2.9; Las Vegas OR= 1.8, 95% CI = 1.3–2.5). Also, in Tel-Aviv, predictors were no opiate use after 1 year (OR = 1.7, 95% CI = 1.4–2.2) and no benzodiazepine after 1 year, and in Las Vegas no cocaine and no amphetamines after 1 year and age less than or equal to 30 years. The two major predictors in the two clinics were successful in both outcomes: 1 year retention and opiate abstinence.
Keywords: Methadone maintenance treatment, countries’ differences, Kaplan-Meier analyses, retention, predictors
INTRODUCTION
Methadone maintenance treatment (MMT), the most effective pharmacotherapy for heroin addiction, is now available worldwide. In the United States, the first research that established the efficacy of methadone as used in chronic pharmacotherapy was done in 19641,2 and treatment was started in the early 1960s. In Israel, methadone was first legally prescribed for chronic treatment of opiate addiction in 1973, and following diverse changes finally was implemented in MMTs accompanied with psychotherapy in 1992 (Ministry of Health). Most successful MMT clinics introduce the same basic treatment principles, but they are still highly diverse from one another both within and between countries.
Criteria for opioid maintenance therapy of the American Society of Addiction Medicine3 describe setting, staff, therapies, assessment, treatment plan review, documentation, and diagnostic admission criteria; the six-dimensional admission criteria are (1) acute intoxication or withdrawal, (2) biomedical conditions and complications, (3) emotional, behavioral, or cognitive conditions and complications, (4) readiness to change, (5) relapse, continued use, or continued potential problems, and (6) recovery environment criteria, which are similar among clinics.
Comparison between different countries can identify unique variables that are more culturally or environmentally related, as well as affirm the common variables that all opiate addicts share and the standard procedures that characterize all effective clinics and standard medical practice programs. Prediction of outcome in different clinics can be attributed to either the unique variables or the shared variables.
Studies from around the world reporting about MMT have been published; however, prospective studies of outcome predictors between countries, and also between clinics, including standard staffing patterns and procedures, are rare. It is difficult to compare MMT clinics, which differ in all parameters, from patients’ characteristics through their environments as well as clinic guidelines and principles.
In the current study, we compared two MMT clinics, both named Dr. Miriam & Sheldon G. Adelson Clinic for Drug Abuse, Treatment & Research, located in different countries. The clinic in Israel, located in a discreet suite of rooms with a private entrance to a large, municipal, university affiliated, medical center in Tel-Aviv. This clinic’s characteristics and outcome were previously reported.4 The other clinic in Las Vegas, Nevada, was located in a community setting. These two clinics, the “Adelson” treatment and research MMT clinics, share one physician who established them both (Tel-Aviv in 1993 and Las Vegas in 2000), and thus have similar guidelines and principles. However, as the locations of these two clinics are in two different countries, it provides an excellent opportunity to compare the two clinics solely with respect to patients’ characteristics and outcomes. The specific aims of this article are to compare the two clinics with respect to patient characteristics, patient outcome (1 year retention in treatment and abstinence from any illicit opiate abuse), factors that predict 1 year retention, and long-term cumulative retention. In addition, the characteristics of the clinic staff and the different rules of the clinics are compared.
METHOD
Study Population
The current study analyzed prospective data that were collected during the treatment of each patient. No special or additional data were generated for the study. In both clinics, each patient consented when admitted to MMT clinic for treatment and for clinical evaluation research. In Israel, the clinic is affiliated with the Tel-Aviv Sourasky Medical Center, and the evaluation analysis for publication was approved by the local Institutional Helsinki Committee.
The Adelson Clinic in Las Vegas was established February 1,2000, and all 302 patients who had been admitted through April 25, 2004, were included in the current study and were followed-up until first discharge or until April 25, 2005. The Adelson Clinic in Tel-Aviv was established on June 25, 1993, and all 492 unique patients who had been admitted for treatment by June 24, 2003, were included in the current study and all patients were followed-up until first discharge or until June 24, 2004. The study of cumulative long-term retention and predictors for retention of the Tel-Aviv clinic only was published in an earlier paper.4 If a patient was discharged and readmitted (which may happen after a predefined period of absence from clinic), data from the first admission only were used (see details about readmissions in the Appendix).
Patients in both clinics were all former heroin-addicted adults (none younger than 18 years); both clinics met criteria similar to those of the U.S. Federal Regulations for entering methadone treatment (i.e.. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR)5 criteria for dependence and multiple daily self-administrations of heroin for 1 year or more.
In Las Vegas, the patients must meet Federal and State guidelines: they must meet criteria for opioid dependence as defined in the DSM-IV-TR criteria for dependence; they must meet Opioid Maintenance Treatment levels of care per the American Society of Addiction Medicine guidelines; and they must have medical clearance by the medical staff. Patients in both clinics may enter the clinic in several different ways, such as walk-ins, referrals (in Tel-Aviv in particular from the affiliated hospital), or word-of-mouth. Before admission in either clinic, each patient reads and signs the policy of the clinic (which is in full accordance with the Israeli Ministry of Health guidelines or in Las Vegas with the American Society of Addiction Medicine Commission on Accreditation of Rehabilitation Facilities). The patient also reviews, signs, and receives a copy of the patient handbook, which has clinic rules and guidelines.
In both clinics, each patient drinks the individual methadone dosage every day in the clinic and is encouraged to earn the privilege to receive “take home” dosages of medication if he or she stops illicit drug use and presents acceptable behavior. In Las Vegas, patients may receive up to 30 “take home” dosages, according to Federal and State guidelines, whereas in Tel-Aviv up to 14 “take-home” dosages of medication are allowed according to the Israeli Ministry of Health.
In both clinics, patients attend regular appointments with personal therapists who are drug and alcohol counselors in Las Vegas and social workers or clinical criminologists in Tel-Aviv. In a limited number of cases with special needs, a physician or a psychiatrist serves as a personal therapist (in both clinics the ratio between personal therapists to patients was 1:50). Further details are presented in Table 1. In Las Vegas, patients can participate in diverse therapy groups focusing on cocaine, women, Methadone Anonymous, or relapse prevention issues. Attendance is not obligatory, but patients are encouraged to participate by giving them food (such as cookies) and beverages for attendance.
TABLE 1.
Comparison in Staff Characteristics Between Tel-Aviv and Las Vegas Methadone Maintenance Treatment Clinics
| Tel-Aviv | Las Vegas | |||
|---|---|---|---|---|
|
| ||||
| Director Medical Director | n | Administrator, Psychiatric Part time (%) | n | Nurse Addiction Medicine Part time (%) |
| Addiction medicine (internal medicine) | 3 | 180 | 35 + 20§ | |
| Psychiatric | 2 | 25 + 20‡ | ||
| Nurses | 5 | 310 | 2 | 200 (including Director) |
| Urine taking | 1 | 100 | ||
| Social worker | 5 | 450 | ||
| Clinical criminologists | 2 | 140 | ||
| Drug and alcohol counselors | 3 | 300 | ||
| Reception | 2 | 200 | 1 | 100 |
| Security | 3 | 300 | 1 | 100 |
Medical Director in Tel-Aviv (3 times/week, 8 hours/week).
Medical Director in Las Vegas.
In Tel-Aviv, patients must participate in several therapy groups (i.e., a mandatory seminar if the patient is new in clinic or a “cocaine group” if the patient abuses cocaine) and can participate in others (e.g., women’s issues, violence, and 12 Steps). Only violent aggressive behavior or selling drugs within the clinic may result in immediate discontinuation of treatment in both clinics. For further details, see Table 2. Patients in Tel-Aviv are required to pay for treatment equaling about $70 USD per month. All patients have monthly government support (for being an MMT patient or due to another disability), unless they have permanent work. In Las Vegas, patient payments for treatment ranged from between no fee to $200 USD per month depending on the ability to pay. In both clinics, all patients undergo blood tests (i.e., hepatitis C antibody, human immunodeficiency virus [HIV] antibodies, hepatitis B antigens, or the venereal disease research laboratory test) for infectious diseases and X-rays for tuberculosis on admission (and annually in Tel-Aviv). In Las Vegas, X-rays for tuberculosis are completed annually only for patients who have previously tested positive.
TABLE 2.
Comparison in Regulations Between Tel-Aviv and Las Vegas Methadone Maintenance Treatment Clinics
| Tel-Aviv | Las Vegas | |
|---|---|---|
| Counselors Sessions Frequency | Varied between once a week to once a month | Varied between once a week to once a month |
| Involuntary termination | ||
| Missing dosages | After 1 month | After 1 month |
| Missing counselor sessions | – | – |
| Non-payment of fees | After 1 month | – |
| Illicit drug use | – | – |
| Violence | Immediate | Immediate |
| Selling drugs | Immediate | Immediate |
In Tel-Aviv, all blood tests and X-rays are performed and paid for by the patient’s personal medical care insurance. In Las Vegas, the blood tests are performed in the clinic and provided by health department nurses with no extra charge; however. X-rays must be performed and paid for by patient’s medical care coverage. In both clinics, electrocardiography has been done on site in recent years.
Analyses were done in the Tel-Aviv clinic patients’ names were deleted in data from Las Vegas. Demographic data were collected from the patients’ charts, which routinely include a modified Addiction Severity Index (ASI) questionnaire.6 Currently, in Tel-Aviv there is a waiting list (up to 1.5 years); however, pregnant women and HIV-positive patients are admitted immediately to treatment with no waiting requirement. In Las Vegas, patients can be admitted immediately.
Urine Toxicology and Methadone
At least one randomized observed urine was obtained each week (range: 1 to 11 samples per month; mean = 4 samples per month) throughout the patient’s entire course of treatment (range; 1 day to 10.8 years). All urine samples were analyzed for opiates, methadone, cocaine metabolite (benzoylecgonine), benzodiazepines (BDZ), cannabis (THC), methadone (until 2002) or its metabolite (since 2002), and amphetamines using enzyme immunoassay systems (DRI®, Diagnostix, Ontario, Canada for the first 6 drugs and CEDIA®, Diagnostix, Ontario, Canada for the last 2 drugs).7 A patient was classified as being “positive” on admission if at least one urine sample for the drug was positive during the first month of treatment. For patients who remained in treatment for at least 13 months (Group A), at the completion of 1 year of treatment the patient was defined as being “positive” for a drug if there had been at least one positive urine screen for that drug during month 13 (Group A). For patients who remained in treatment for more than 4 but less than 13 months (Group B), illicit drug use during the last month in treatment was recorded.
Methadone Dose
Methadone dosage was recorded daily, and the dosages administered at the beginning of month 13 were recorded for Group A and at the beginning of the last month in treatment for Group B. Patients (n = 50 in Tel-Aviv; n = 44 in Las Vegas) who left the MMT clinic before 4 months were excluded from the analyses used for compiling cumulative retention to be sure that the methadone dosage during the last month was stabilized and not a temporary midway dosage during the stabilization process.
Data Collection
All data were collected prospectively by a social worker (i.e., demographic data, age, sex, and history of drug abuse), nurse (i.e., urine and methadone dosages), and clinician (i.e., HIV and hepatitis C) and saved both in patients’ charts and electronically [in a special program (Magic, Magic Software Enterprises) in Tel-Aviv, and on a Excel (Microsoft Corporation, WA, USA) spreadsheet in Las Vegas]. In addition, the data manager in Tel-Aviv put specific data variables in a separate SPSS (SPSS Inc., Chicago, IL) file in an ongoing manner (which was cleaned in real time) routinely for evaluation analyses. The file included baseline variables including age, sex, marital status, children, education, duration of opiate abuse, status of hepatitis C, HIV, and hepatitis B tests, and urinalyses positive or negative for each drug of potential abuse at the first month in treatment. For each patient, the methadone dosage after 1 year (or at the last month if a patient left before) was also taken from the patient’s chart and the computer. The outcome variables that were taken and put in the file for analysis were urinalyses results after 1 year (or at the last month if a patient left before), at 6 months retention and 1 year retention in treatment, and the total duration in treatment (dates of admission and date of discharge if a patient left treatment or date of end of follow-up if a patient was still in treatment for computing cumulative retention).
The analyses for both clinics were done in Tel-Aviv after receiving data with names deleted from Las Vegas. The Las Vegas file with the relevant variables was moved to the SPSS program and merged with the Tel-Aviv file. Outline values were identified, rechecked in the original clinic chart, and corrected if needed. Analyses were done using the SPSS file in Tel-Aviv.
Statistical Analyses
Proportional differences between clinics were analyzed by the Fisher’s exact test for variables with only two categories and by Chi Square for variables with more than two categories. Pearson correlation coefficients were used for linear correlation evaluations. The methadone dosage and other continuous variables were analyzed for significant differences using analysis of variance. Duration (in years) in clinic from first admission until the patient stopped treatment or until the end of the follow-up (5.3 years in both Las Vegas and Tel-Aviv, despite the fact that 11 years of follow-up data are available and have been published for Tel-Aviv alone4) was taken to calculate cumulative retention in treatment using survival analyses (Kaplan-Meier) with log rank. Variables that were significantly associated with retention in the Kaplan-Meier analyses (P < .05) were included in the Cox regression multivariate analyses and presented in OR and 95% CI. A model for each clinic separately and one combined was completed. Logistic regression models for 1 year retention in treatment for Tel-Aviv and for Las Vegas were used and included all the variables that were found to be significantly (P < .05) associated with 1 year retention in the univariate analyses. The adequacy of the models were determined using the Hosmer and Lemeshow goodness-of-fit test8 (Chisquare = 3.2, P = .5 for Las Vegas, and not relevant in Tel Aviv because only one variable was found to be significant in univariate analyses). All analyses were completed using the SPSS version 12 package.9
Power Analyses
We could identify a difference in the 1 year retention rate of 10% (for instance, if one clinic had a 70% retention and the other had a 80% retention) with a 80% power and ά of 5% if each clinic’s sample size were of 300 patients.
RESULTS
Comparison Between Patient Characteristics Between Clinics
During the study, 66 of the 492 (13.4%) patients in Tel-Aviv had more than one admission, and 17 of the 302 (5.6%) patients in Las Vegas had more than one admission. However, this difference was not included in the analyses because only the data of each patient’s first admission were used (Table 3).
TABLE 3.
Tel-Aviv and Las Vegas Clinics Patient Characteristics
| Tel-Aviv n (%) | Las Vegas n (%) | P (Fisher’s Exact Test) | |
|---|---|---|---|
| Total | 492 (100) | 302 (100) | |
| Age on admission (y) | 36.7 ± 8.5 (18–67) | 43.4 ±9.4 (19–63) | * F = 105.7, <.0005 |
| 18–29 | 103 (20.9) | 30 (9.9) | <.0005 |
| ≥30 | 389 (79.1) | 272 (90.1) | |
| Gender | .004 | ||
| Male | 358 (72.8) | 190 (62.9) | |
| Female | 134 (27.2) | 112 (37.1) | |
| Education (y) | 9.7 ±2.9 | 12.1 ±1.8 | * F = 160.4, <.0005 |
| <8 | 61 (12.3) | 4 (1.3) | **<.0005 |
| 8–11 | 270 (59.2) | 73 (24.3) | |
| ≥12 | 130 (28.5) | 224 (74.4) | |
| Marital status | .3 | ||
| Alone | 325 (66.6) | 213 (70.5) | |
| In couple | 163 (33.4) | 89 (29.5) | |
| Children | <.0005 | ||
| Yes | 312 (63.8) | 138 (46.3) | |
| No | 177 (36.2) | 160 (53.7) | |
| Opiate abuse before admission (y) | 13.9 ±8.3 (1–38.5) | 17.5± 11.0 (1–43) | * F = 27.4, <.0005 |
| <5 | 57 (11.9) | 35 (11.7) | |
| ≥5 | 423 (88.1) | 265 (88.3) | |
| Retention in treatment 1 year or more | <.0005 | ||
| Yes | 366 (74.4) | 186 (61.6) | |
| No (all) | 126 (25.6) | 116 (38.4) | |
| Left < 4 mo. | 50 (10.2) | 44 (14.6) | |
| Left ≥ 4 mo. | 76 (15.4) | 72 (23.8) | |
| Hepatitis C Antibody | <;.0005 | ||
| Yes | 261 (56.9) | 208 (82.5) | |
| No | 198 (43.1) | 44 (17.5) | |
| Not tested | 33 | 50 | |
| HIV Antibody*** | .06 | ||
| Yes | 36 (7.3) | 3 (1.0) | |
| No | 390 (79.3) | 101 (33.4) | |
| Not tested | 66 (13.4) | 198 (65.6) | |
| Drug of abuse in urine at admission | |||
| Cocaine | <.0005 | ||
| Yes | 67 (13.7) | 158 (52.3) | |
| No | 422 (86.3) | 144 (47.7) | |
| Benzodiazepines | <.0005 | ||
| Yes | 273 (55.8) | 84 (27.8) | |
| No | 216 (44.2) | 218 (72.2) | |
| Amphetamines | .008 | ||
| Yes | 45 (9.2) | 47 (15.6) | |
| No | 444 (90.8) | 255 (84.4) | |
| Cannabis | .005 | ||
| Yes | 56 (11.5) | 57 (18.9) | |
| No | 433 (88.5) | 245 (81.1) |
Analysis of varience.
Fisher’s exact test, excluding the younger than 8 years group.
Fisher’s Exact test, excluding the not tested group.
Some variables have missing date, notice total numbers.
Compared to the Tel-Aviv MMT clinic, the patients in the Las Vegas were older (43.4 ± 9.4 vs. 36.7 ± 8.5; F= 105.7; P < .0005) with more years of opiate use (17.5 ± 11.0 vs. 13.9 ± 8.3; F = 27.4, P < .0005). Age at admission and years of opiate abuse significantly correlated with each other (R = 0.62; P < .0005). The Las Vegas patients had more years of education (12.1 ± 1.8 vs. 9.7 ±2.9; F= 160.5; P < .0005) but it was not related to their age at admission (R = −0.05; P = .3), whereas Tel-Aviv patients had an inverse correlation between years of education and age on admission (R = −0.24; P<.0005) as well as years of education and years of opiate use (R = −0.24; P < .0005) was found. Las Vegas patients had a higher proportion of females (37.1% vs. 27.2% Fisher’s Exact Test; P = .004) and of patients with no children on admission (53.7% vs. 36.2%, Fisher’s Exact Test; P < .0005). Las Vegas patients had a higher proportion of cocaine (52.3% vs. 13.7%), amphetamines (15.6% vs. 9.2%), and THC (18.9% vs. 11.5%) abuse at admission, but a lower proportion of patients abusing benzodiazepines (27.8% vs. 55.8%). Also, a higher proportion of patients with positive antibody to hepatitis C (HCV+) was observed in Las Vegas (82.5% of 252 tested) compared with those (56.9% of 459 tested) in Tel-Aviv. The HCV results were unknown in 16.6% in Las Vegas and in 6.7% in Tel-Aviv. HIV antibody was observed in 36 (7.3%) Tel-Aviv patients, with 66 (13.4%) not tested, and in 3 (1.0%) Las Vegas patients, with 198 (65.6%) not tested.
Six Months and 1 Year Retention and Factors Related to 1 Year Retention
Fifty (10.2%) patients from the Tel-Aviv clinic and 44 (14.6%) patients from the Las Vegas clinic stayed in treatment for less than 4 months. After 6 months, 83.5% (411 of 492) of patients in Tel-Aviv and 78.5% (237 of 302) in Las Vegas stayed in the MMT clinic. Of those who stayed 6 months, 231 (56.2%) of patients in Tel-Aviv and 127 (53.6%) of patients in Las Vegas had negative urines for opiates.
One year retention was higher in Tel-Aviv (74.4% vs. 61.6%; P< .0005), but with no difference in cessation of opiate abuse after 1 year (65.8% vs. 64.9%; P = 0.9). Mean methadone dosage after 1 year (Group A) was 132.6 ±51.5 mg/day for 366 patients in Tel-Aviv, which is similar to the 134.3 ±57.0 mg/day for 186 patients in Las Vegas (F = 0.1; P = .7), and mean methadone dosage for patients who left before 1 year was 108.2 ±46.7 mg/day for 75 patients from Tel-Aviv (Group B) versus 105.9 ±53.0 mg/day for 70 patients in Las Vegas (P = .8). In both clinics, the 1 year retention rate was significantly higher in older patients (those older than 30 years) with no relation to gender, marital status, or abuse of cocaine, benzodiazepine, and cannabis on admission (Table 4). In Las Vegas, but not in Tel-Aviv, the 1 year retention was lower in patients with positive urine for amphetamines (46.8% vs. 64.3%), in those who abused opiates less than 5 years (45.7% vs. 63.8%), in patients with no children (56.3% vs. 68.1%), and in seronegative HCV patients (47.7% vs. 73.1%).
TABLE 4.
Significant Differences in 1 Year Retention in Treatment by Variables That Were Significantly Different in the Tel-Aviv or Las Vegas Clinics
| Variables | Tel-Aviv
|
Las Vegas
|
||||
|---|---|---|---|---|---|---|
| Total N | Stay 1 year or more n (%) | p* | Total N | Stay 1 year or more n (%) | P* | |
| Entire Group | 492 | 366 (74.4) | 302 | 186 (61.6) | ||
| Age on Admission (y) | .02 | .05 | ||||
| 18–29 | 103 | 67 (65.0) | 30 | 13 (43.3) | ||
| ≥30 | 389 | 299 (76.9) | 272 | 173 (63.6) | ||
| Children | .2 | .04 | ||||
| Yes | 312 | 239 (76.6) | 136 | 94 (68.1) | ||
| No | 177 | 127 (71.8) | 160 | 90 (56.3) | ||
| Opiate abuse before admission (y) | .1 | .04 | ||||
| <5 | 57 | 38 (66.7) | 35 | 16 (45.7) | ||
| ≥5 | 423 | 326 (77.1) | 265 | 169 (63.8) | ||
| Hepatitis C Antibody | 1.0 | .001 | ||||
| Yes | 261 | 205 (78.5) | 206 | 152 (73.8) | ||
| No | 198 | 155 (78.3) | 43 | 20 (46.5) | ||
| Drug of abuse in urine at admission Amphetamines | .2 | .03 | ||||
| Yes | 45 | 30 (66.7) | 47 | 22 (46.8) | ||
| No | 444 | 336 (75.7) | 255 | 164 (64.3) | ||
Fisher’s Exact Test.
Some variables have missing date, notice total numbers.
Multivariate Analyses for 1 Year Retention
Logistic regression for 1 year retention in treatment in Las Vegas found that no amphetamines on admission (OR = 2.1; 95% CI = 1.05–4.2), having children (OR=l .9; 95% CI = 1.1–3.3), and sera-positive HCV (OR=2.4; 95% CI =1.1–5.3) characterized patients who stayed at least 1 year in treatment. Logistic regression for 1 year retention in treatment in Tel-Aviv found only older age (OR=1.8; 95% CI= 1.1–2.9) to be a characteristic of patients who stayed at least 1 year in treatment.
Of those who left MMT before 1 year, 20.7% in Las Vegas versus 4% in Tel-Aviv moved elsewhere in or out of the country. Also, 7.8% in Las Vegas moved to private physicians who prescribed methadone for “pain,” but none moved to private practice in Tel-Aviv (where privately prescribed methadone is not available).
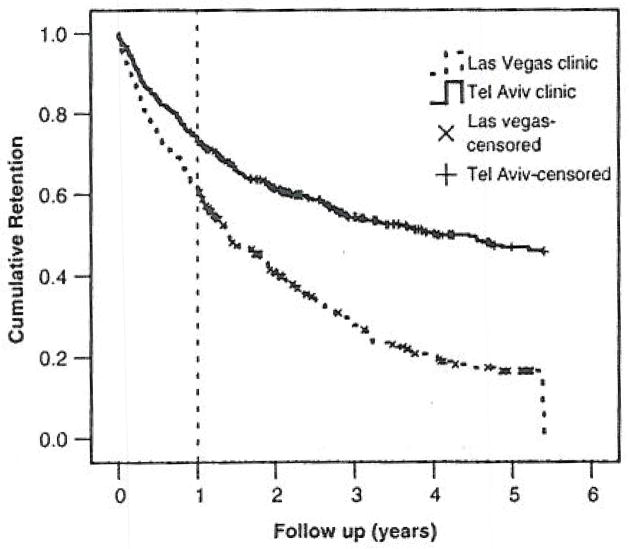
Factors Predicting Cumulative Retention
The cumulative retention was significantly longer in the Tel-Aviv clinic (mean = 3.3 years; 95% CI = 3.1–3.5), compared with the Las Vegas clinic (mean = 2.1 years; 95% CI = 1.9–2.3; log rank = 60.6; P< .0005) (Figure 1). Factors that were similar in both clinics in predicting longer retention in treatment were older age on admission (older than 30 years) and methadone dosage of 100 mg/day or more after 1 year or in the last month in treatment. The two clinics also showed no relation to gender, marital status, having children, and abuse of cocaine and benzodiazepines on admission and THC after 1 year (or last month in treatment).
FIGURE 1.
The cumulative retention in treatment for patients from Tel-Aviv and Las Vegas MMT Adelson clinics. Censored patients from both clinics are marked. Duration (in years) in clinic from first admission until the patient quit treatment or until the end of the follow-up (5.3 years in both Las Vegas and Tel-Aviv, despite the fact that 11 years of follow-up data are available and have been published for Tel-Aviv alone4 was taken for calculating cumulative retention in treatment using survival analyses (Kaplan-Meier) with log rank.
The variables that predicted longer cumulative retention in Las Vegas, but not in Tel-Aviv, were a longer duration of opiate addiction before admission to MMT (5 years or more), more years of education (12 years or more), having positive antibody to hepatitis C, not abusing THC on admission, not abusing amphetamines on admission, and not abusing amphetamines and or cocaine after 1 year or in the last month in treatment. The variable that predicted longer cumulative retention in Tel-Aviv, but not in Las Vegas, was not abusing opiates and benzodiazepines after 1 year in treatment (or in the last month in treatment) (Table 5).
TABLE 5.
Patient Characteristics Significantly Associated with Cumulative Retention (up to 5.3 years) in Tel-Aviv or in Las Vegas Clinicsa
| Variables | Cumulative Survival (Kaplan-Meier)
|
|||||
|---|---|---|---|---|---|---|
| Tel-Aviv
|
Las Vegas
|
|||||
| N | Mean (y) (95% CI) | Log Rank (P value) | N | Mean (y) (95% CI) | Log Rank (P value) | |
| Total | 492 | 3.3 (3.1–3.5) | 302 | 2.1 (1.9–2.3) | ||
| Admission age (y) | 5.6 (.02) | 12.6 (<.0005) | ||||
| 18–29 | 103 | 2.8 (2.4–3.3) | 30 | 1.0(0.7–1.4) | ||
| ≥30 | 389 | 3.4 (3.2–3.7) | 272 | 2.2 (2–2.4) | ||
| Gender | 0.5 (.5) | 0.5 (.5) | ||||
| Male | 358 | 3.3 (3.1–3.6) | 190 | 2.0 (1.7–2.3) | ||
| Female | 134 | 3.2 (2.8–3.6) | 112 | 2.2 (1.8–2.6) | ||
| Education (y) | 4.9 (.09) | 4.1 (.04)** | ||||
| <8 | 61 | 3.1 (2.5–3.7) | 4 | 2.1 (0.8–3.4) | ||
| 8–11 | 270 | 3.6 (3.4–3.9) | 73 | 1.7 (1.3–2.1) | ||
| ≥12 | 130 | 3.3 (2.9–3.7) | 224 | 2.2 (1.9–2.5) | ||
| Marital status | 2.4 (.1) | 0.5 (.5) | ||||
| Alone | 325 | 3.2 (3.0–3.5) | 213 | 2.0(1.8–2.3) | ||
| In couple | 163 | 3.5 (3.2–3.9) | 89 | 2.2(1.8–2.7) | ||
| Children | 3.4 (.07) | 1.8 (.2) | ||||
| Yes | 312 | 3.5 (3.2–3.7) | 138 | 2.2 (1.9–2.6) | ||
| No | 177 | 3.1 (2.7–3.4) | 160 | 2.0 (1.7–2.3) | ||
| Opiate abuse before admission (y) | 3.3 (.07) | 4 (.05) | ||||
| <5 | 57 | 2.8 (2.3–3.4) | 35 | 1.5 (0.9–2.0) | ||
| ≥5 | 423 | 3.5 (3.2–3.7) | 265 | 2.2(1.9–2.4) | ||
| Hepatitis C antibody | 1–4 (.2) | 15.6 (<.0005) | ||||
| Yes | 261 | 3.4 (3.2–3.7) | 208 | 2.6 (2.3–2.9) | ||
| No | 198 | 3.6 (3.3–3.9) | 44 | 1.4 (0.9–1.9) | ||
| Drug of abuse in urine at admission | ||||||
| BDZ | 1 (3) | 1 (.8) | ||||
| Yes | 273 | 3.3 (3.0–3.5) | 84 | 2.1 (1.7–2.5) | ||
| No | 216 | 3.4 (3.1–3.7) | 218 | 2.1 (1.8–2.3) | ||
| Cocaine | 0.9 (.4) | 0.8 (.4) | ||||
| Yes | 67 | 3.6 (3.0–4.1) | 158 | 2.0 (1.7–2.3) | ||
| No | 422 | 3.3 (3.1–3.5) | 144 | 2.2 (1.9–2.5) | ||
| Amphetamines | 1.8 (.2) | 6 (.01) | ||||
| Yes | 45 | 2.8 (2.2–3.5) | 47 | 1.5 (1.0–2.0) | ||
| No | 444 | 3.4 (3.2–3.6) | 255 | 2.2 (2.0–2.4) | ||
| THC | 0.2 (.8) | 4.2 (.04) | ||||
| Yes | 56 | 3.4 (2.8–3.9) | 57 | 1.6 (1.2–2.0) | ||
| No | 433 | 3.3 (3.1–3.5) | 245 | 2.2 (1.9–2.4) | ||
| Drug of abuse in urine after 1 year** | ||||||
| Opiates | 36.3 (<.0005) | 3.1 (.08) | ||||
| Yes | 177 | 2.9 (2.6–3.3) | 101 | 2.2 (1.8–2.6) | ||
| No | 263 | 4.2 (3.9–4.4) | 155 | 2.6 (2.3–2.9) | ||
| BDZ | 6.1 (.01) | <0.01 (1.0) | ||||
| Yes | 222 | 3.4 (3.1–3.7) | 110 | 2.4 (2.1–2.8) | ||
| No | 218 | 3.9 (3.6–4.2) | 146 | 2.4 (2.0–2.7) | ||
| Cocaine | 3.4 (.06) | 4.0 (.05) | ||||
| Yes | 61 | 3.2 (2.6–3.7) | 109 | 2.1 (1.8–2.5) | ||
| No | 379 | 3.8 (3.5–4.0) | 147 | 2.6 (2.3–2.9) | ||
| Amphetamines | 0.04 (.8) | 14.9 (<.0005) | ||||
| Yes | 39 | 3.5 (2.8–4.2) | 44 | 1.5 (1.1–1.8) | ||
| No | 401 | 3.7 (3.5–3.9) | 212 | 2.6 (2.3–2.9) | ||
| THC | 1.8 (.2) | 0.8 (.4) | ||||
| Yes | 83 | 3.4 (3.0–3.9) | 39 | 2.1 (1.7–2.6) | ||
| No | 357 | 3.7 (3.5–3.9) | 217 | 2.5 (2.2–2.8) | ||
| Methadone | 14.2 (<.0005) | 7.0 (.008) | ||||
| <l00 mg/day | 124 | 3.1 (2.7–3.5) | 76 | 2.0 (1.6–2,3) | ||
| ≥100mg/day | 316 | 3.9 (3.7–4.1) | 180 | 2.6 (2.3–2.9) | ||
CI = confidence interval; BDZ = benzodiazepines; THC = tetrahydrocannabinol:
Significant differences marked in bold.
For each variable category, the mean and 95% CI cumulative retention in treatment (Kaplan Meier) is presented in years, and the comparison between categories is presented by log-rank and significance (P value).
If patients lelt before 1 year, the last month in treatment was used. Excluding patients who stay less than 4 months.
Some variables have missing date, notice total numbers.
Multivariate Analyses for Cumulative Retention
In Tel-Aviv, no use of opiates after 1 year, no use of benzodiazepines after 1 year, and high methadone dosage of 100 mg/day or more after 1 year predicted longer cumulative retention (Table 6). In Las Vegas older age (30 years or older) on admission, no abuse of cocaine or amphetamines after 1 year, and high methadone dosage 100 mg/day after 1 year predicted longer cumulative retention (Table 6).
TABLE 6.
Cox Multivariate Models for Cumulative Retention in Treatment*
| OR (95% CI) | P value | |
|---|---|---|
| Tel-Aviv Clinic | ||
| Methadone dosage ≥ 100 mg/day after 1 year | 2.1 (1.6–2.9) | <.0005 |
| No urine illicit opiates after 1 year | 2.3 (1.7–3.1) | <.0005 |
| No urine illicit benzodiazepines after 1 year | 1.4 (1.0–2.0) | .03 |
| Age included in model, but was not significant | ||
| Las Vegas Clinic | ||
| Methadone dosage ≥ 100 mg/day after 1 year | 1.8(1.3–2.5) | .0006 |
| No urine cocaine after 1 year | 1.4 (1.0–1.9) | .04 |
| No urine amphetamines after 1 year | 1.7 (1.1–2.7) | .02 |
| Age 30 years or more on admission | 2.2 (1.4–3.6) | .001 |
| Amphetamines and cannabis use on admission included in model, but were not significant. | ||
Cox regression model included variables that were significantly associated with cumulative retention in the Kaplan-Meier analyses (P < .05), Odds Ratio (OR), 95% Confidence Interval (CI), and P values are presented.
In a model that included both clinics and all the variables that were significant in either one of the clinics in multivariate analyses, coming from the Tel-Aviv clinic (OR=2.3; 95% CI = 1.9–3.0) with a high methadone dosage of 100 mg/day or more (OR=l .8; 95% CI = 1.4–2.3), being older on admission OR = 1.5 (95% CI = 1.1–2.0), and with no opiate use after 1 year (OR = 1.7; 95% CI = 1.4–2.2) were all predictors of longer cumulative retention.
DISCUSSION
We found modest but significant differences in the distribution of patients’ characteristics between clinics. Despite these differences, both clinics presented a similar rate of opiate abuse cessation after 1 year, which is one of the two objective measurable main outcomes of MMT. Retention in treatment, however, which is the other major outcome, differed between clinics. Specifically, the 1 year retention rate was higher in Tel-Aviv than in Las Vegas (74.4% vs. 61.6%), but both clinics presented high retention rates compared to other clinics throughout the world whose retention rates have been reported: 1 year retention rate was 48% in 674 patients from Massachusetts and Connecticut MMT clinics;10 52% in 338 MMT patients from New York;11 60% in 1,487 MMT patients from Spain;12 38.4% in 477 from Australia;13 61% in 136 MMT and 65% in 121 buprenorphine patients from Italy;14 and 43.8% in 206 other buprenorphine patients from Italy.15
Comparing the two clinics with respect to patients’ characteristics on admission, the Las Vegas patients were admitted when they were older (mean = 43.4 years) than the Tel-Aviv patients (mean = 36.7 years). Older age on admission is already known and was also found by us in the current study, and elsewhere, as a predictor of longer retention.4,16–17 In the Las Vegas MMT clinic, but not in the Tel-Aviv, a history of opiate abuse of less than 5 years (compared with 5 years or more) predicted shorter retention. This could be explained because opiate abuse and age on admission linearly correlated in both clinics. However, although the mean age of patients abusing opiates for 5 years or more was 37.5 years in Tel-Aviv, the mean age of this group was 44.3 years in Las Vegas. Therefore, the older age that is known to be a predictor for longer retention explains the longer retention in the 5 years or more of opiate abuse patients in Las Vegas, Indeed, evaluating the two variables, only age was a significant predictor for longer retention.
In both Las Vegas and Tel-Aviv, 10 years of education is mandatory; the Las Vegas patients had completed more years of school than the patients in Tel-Aviv. However, interestingly, more years of education (more than 12 years) was found as a predictor for longer retention only in Las Vegas, whereas the most educated group in Tel-Aviv (more than 12 years) predicted shorter retention (but only as a trend). Although the most educated group (more than 12 years) in Las Vegas comprised the majority of patients (74.4%), the same level of education in Tel-Aviv comprised only in a minority (28.5%) of the patients. Differences in levels of education between clinics were even more pronounced in the non-educated group; in Tel-Aviv, 12.3% of patients had less than 8 years of education, whereas in Las Vegas less than 8 years of education was rare (only 1.3%). Mean age of starting opiate use was also modestly but significantly younger in Tel-Aviv compared with Las Vegas patients (22.9 ±7.3 vs. 25.9 ±9.4; P < .0005). This was not related to the differences in education levels between the two clinics. When stratified into age of starting opiate use (younger than 16 years, 16 to 26 years, and older than 26 years) and years of education, there was no difference in years of education among the three groups (9.2 ±2.3, 10±2.9, and 9.6 ±3.2, respectively) in Tel-Aviv, whereas years of education increased in concordance with an older age of starting opiate use (11.5 ± 1.7, 12 ± 1.6, 12.3 ± 2.0, respectively) in Las Vegas (P = .05).
There were a higher percentage of women in the Las Vegas clinic (37.1 %) compared with the Tel-Aviv clinic (27.2%). This is despite the fact that the affiliated hospital referred all pregnant women to the Tel-Aviv clinic. The proportion of women from other MMT clinics diverged; 30% of patients were females in a study in Barcelona,18 but 46% of patients were females in a different study in the United States.19 The proportion of women was not related to retention because both genders had similar 1 year and cumulative retentions.
We would expect that a clinic with more women would comprise more parents, but the opposite was observed; the proportion of patients who are parents was higher in Tel-Aviv (63.8%) than in Las Vegas (46.3%). “Being a parent” in the Las Vegas clinic was significantly related to the 1 year retention rate, but it was not related to cumulative retention. In the current study analyzing only 5.3 years of follow-up, the variable “being a parent” was not significantly related to cumulative retention in Tel-Aviv; however, it had already been found significant when analyzed in 11 years of follow-up,20 where it was also found as an independent predictor (in multivariate analyses). Such a predictor was identified only in the Tel-Aviv clinic and by no other investigators except in one report where it was a component in univariate analyses.17
Being hepatitis C positive was much more prevalent in Las Vegas (82.5%) than in Tel-Aviv (56.9%). However, although there were no differences in retention with only a slight trend of longer retention in the sera-negative HCV patients in Tel-Aviv, a significantly shorter retention was found in the sera-negative HCV patients in Las Vegas compared to the sera-positive group. This finding was unexpected. After exploring if there were any characteristics that substantially differed between the HCV positive and HCV negative patients in Las Vegas, we found that the HCV negative patients in Las Vegas were significantly younger (36.7 ± 11.6 years) than the HCV positive patients (45.6 ± 8.1 years). Young age is associated with lower retention. In Tel-Aviv, on the other hand, HCV groups were similar with respect to age (mean of 36 years for both groups). Therefore, it appeared that the age and not the HCV status predicted retention. The HCV negative patients in Las Vegas, less than one-fifth of the clinic, differed from HCV positive patients in other variables: they had a much shorter duration of opiate addiction (10 ± 9 vs. 19.8 ± 10.7 years, respectively), more years of education (12.6 ±2.1 vs. 11.9 ±1.7, respectively), fewer of them had cocaine positive urine on admission (34.1% vs. 56.3%), more had amphetamines on admission (25% vs. 13%), and less reported benzodiazepines abuse on admission (22.7% vs. 30.3%). All of these variables were not different between the HCV groups in Tel-Aviv except for duration of opiate abuse, which, as in Las Vegas, was longer in HCV positive versus HCV negative (14.6 ±8.2 vs. 12.7 ±8.0) patients. Clinics differed in prevalence of HIV (7.3% in Tel-Aviv and 1% in Las Vegas), but also in rates of not tested (13.4% vs. 65.6%, respectively). In Tel-Aviv, HIV testing is mandatory (although no action is taken if patient refuses testing), and most unknowns were patients who left treatment after a short time. In Las Vegas, on the other hand, testing was not mandatory and was suggested, but a high rate of patients refused.
Drugs in urine on admission differed between clinics, reflecting the differences in the environment between Israel and the United States. There was evidence of cocaine use in half of the Las Vegas MMT clinic patients. This is in accordance with other clinics elsewhere in the United States (i.e., 59% in the Bronx in New York City, New York).21 In Tel-Aviv, the rate of cocaine abusers on admission was only 13.7%, which reflects the low rate of cocaine abuse in Israel.22 Importantly, the abuse of cocaine on admission was not related to 1 year retention, nor to the cumulative retention, either in Tel-Aviv or in Las Vegas, where cocaine was highly prevalent. However, unlike positive cocaine on admission, cocaine abuse after 1 year (or in the last month in treatment), which is an “in treatment” variable, predicted shorter cumulative retention in Las Vegas and only as a trend for significance in Tel-Aviv. These findings suggest that patients who still abuse cocaine while in treatment (start or did not stop) have the odds of a worse outcome: shorter retention. The fact that the patient abused on admission does not predict the outcome because cocaine abuse can be stopped while in treatment (and that is what mostly happened),4,20 and thus does not reflect outcome.
Amphetamines abuse on admission was higher in Las Vegas than in Tel-Aviv (15.6% vs. 9.2%). Drug abuse on admission and after 1 year (an “in treatment” variable) predicted shorter retention in Las Vegas but not in Tel-Aviv. No significant differences shown between positive versus negative urinalysis results for amphetamines patients in Tel-Aviv could be due to low statistical power because of the small number of amphetamine abusers.
Cannabis abuse, like amphetamines, was also more prevalent in Las Vegas than in Tel-Aviv and also predicted shorter retention in the MMT clinic in Las Vegas, whereas it was not related to the retention rate in Tel-Aviv. However, unlike amphetamines that predicted lower retention both on admission and after 1 year (an “in treatment” variable), cannabis abuse on admission (but not after 1 year) predicted lower retention. With respect to the effect of cannabis on retention and other outcomes in MMT, a previous study from our clinic in Tel-Aviv23 as well as in others (see review24) found no effect, but other investigators did.25
The only drug that was more prevalent in Tel-Aviv compared with Las Vegas was benzodiazepine (55.8% vs. 27.8%). The retention was not related to the benzodiazepine abuse on admission in both clinics, but abuse after 1 year or in the last month in treatment was a predictor for a worse outcome (shorter retention) in Tel-Aviv only. A high benzodiazepine use rate is common in some MMT clinics, often exceeding 45% in both the United States and Israel.26–27 The Las Vegas clinic has relatively low benzodiazepine abuse.
Any illicit opiate abuse after 1 year or in the last month in treatment was not different between the two clinics (65.8% in Tel-Aviv vs. 64.9% in Las Vegas). In Tel-Aviv, no opiate use after 1 year or in the last month in treatment was a strong predictor for longer retention; in Las Vegas it was only as a trend. Although the finding observed in Tel-Aviv was expected, the one in Las Vegas was surprising.
In Las Vegas, but not in Tel-Aviv, a larger number of patients (20.7%) left treatment as they moved elsewhere in or out of the United States. Israel is a small country and people do not move as frequently (only 4% in the current study). In the United States, many people often move from state to state. This fact is not unique to addicted people; it is well known, and has interfered with other studies as well (such as diverse clinical trials and epidemiological study follow-ups). For example, in a study of African-American women from Brooklyn, patients were highly mobile28 and a study on traumatic brain injury was biased because 40% of study participants were “loss to follow-up.”29 Another important fact is that methadone can be given, and now is frequently given, for pain management by private medical doctors in the United States. In some MMT clinics, a high prevalence of patients has been reported as suffering from chronic pain,19,30 but it is hard to estimate who pretends to have pain and who really suffers. In the United States, patients suffering from chronic pain may move to private medical doctors, who sometimes do not know about their addiction, and the addicted patients then have the benefit of obtaining methadone to take home with no requirement of urine monitoring for drug abuse or other obligations. In our study, we know that at least 7.8% of the patients in Las Vegas who left moved to such private medical doctors for treatment of pain; however, most of these patients had no documented recording in their MMT chart of signs or complaints about pain. There are still a significant group of patients (21 %) who “did not show up,” but the reason for leaving cannot be verified. It would be of importance to compare all reasons for leaving treatment; however, the follow-up data among those who left without reason are limited, particularly in Las Vegas. Thus, in the current study, comparison for specific reasons for leaving treatment between the two clinics would be unbalanced and might be biased.
CONCLUSIONS
We conclude that, although using the same methods, comparing two MMT clinics with the same regulations, the differences in population characteristics and other non-medical reasons showed differences in retention that are not medically related. However, the retention rates in both clinics were much higher with respect to other methadone and buprenorphine maintenance clinics over the past 10 years.
In both clinics we found, as is already known, that high methadone dosage is associated with longer retention. Importantly, retention in both clinics was not related to abuse of cocaine or benzodiazepines on admission. Both clinic staffs’ training, compassionate attitudes, and acceptance that addiction is a medical disease, accompanied by treatment with adequate dosages of methadone (adjusted by patients and confirmed by objective serum levels) all added to the good outcomes.
Acknowledgments
Supported by KO5-DA00049 (MJK), NIH-NIDA P60-05130 (MJK), and internal funds (MA).
APPENDIX
Patients’ admissions by year and by admission number in Tel-Aviv and Las Vegas. If patient had more than one admission, first admission data was included in the current study.
| 1st Admission (Unique Individual) | 2nd Admission (Repeat Admission, Not Included in Analyses) | 3rd Admission (Repeat Admission, Not Included in Analyses) | Total Admissions/Year | |
|---|---|---|---|---|
| Admission year | ||||
| Tel-Aviv (N = 492) | ||||
| 1993 | 35 | 35 | ||
| 1994 | 51 | 2 | 53 | |
| 1995 | 73 | 4 | 77 | |
| 1996 | 38 | 5 | 43 | |
| 1997 | 27 | 5 | 32 | |
| 1998 | 34 | 6 | 40 | |
| 1999 | 16 | 6 | 22 | |
| 2000 | 67 | 9 | 6 | 82 |
| 2001 | 52 | 14 | 2 | 68 |
| 2002 | 77 | 11 | 2 | 90 |
| 2003 | 22 | 4 | 2 | 28 |
| Las Vegas (N = 302) | ||||
| 2000 | 116 | 4 | 120 | |
| 2001 | 45 | 3 | 48 | |
| 2002 | 17 | 5 | 22 | |
| 2003 | 77 | 2 | 1 | 80 |
| 2004 | 47 | 1 | 1 | 49 |
References
- 1.Dole VP, Nyswander ME, Kreek MJ. Narcotic blockade. Arch Intern Med. 1966;118:304–9. [PubMed] [Google Scholar]
- 2.NIH Consensus Statement. Effective Medical Treatment of Opiate Addiction. 1997;15(6):1–6. [Google Scholar]
- 3.Graham AW, Schultz TK, Mayo-Smith ME, Ries RK, Wilford BB, editors. Principles of Addiction Medicine. 3. American Society of Addiction Medicine, Inc; Chevy Chase, MD: 2003. Crosswalk of the ASAM Adult Patient Placement Criteria; pp. 1594–1596. [Google Scholar]
- 4.Peles E, Schreiber S, Adelson M. Factors predicting retention in treatment: 10-year experience of a methadone maintenance treatment (MMT) clinic in Israel. Drug Alcohol Depend. 2006;82:211–7. doi: 10.1016/j.drugalcdep.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 4. Washington, DC: American Psychiatric Press; text revision. [Google Scholar]
- 6.McLellan AT, Luborsky L, O’Brien CP, Barr HL, Evans F. The Addiction Severity Index in three different populations. NIDA Res Monogr. 1984;55:217–23. [PubMed] [Google Scholar]
- 7.Hawks RL. Analytical methodology. NIDA Res Monogr. 1986;73:30–42. [PubMed] [Google Scholar]
- 8.Hosmer DW, Lemeshow S. A goodness-of-fit test for the multiple logistic regression model. Comm Stat. 1980;A10:1043–69. [Google Scholar]
- 9.SPSS Inc; Chicago, IL: 2008. p. 60606. [Google Scholar]
- 10.MacGowan RJ, Swanson NM, Brackbill RM, Rugg DL, Barker T, Molde S. Retention in methadone maintenance treatment programs, Connecticut and Massachusetts, 1990–1993. J Psychoactive Drugs. 1996;28:259–65. doi: 10.1080/02791072.1996.10472487. [DOI] [PubMed] [Google Scholar]
- 11.Kayman DJ, Goldstein MF, Deren S, Rosenblum A. Predicting treatment retention with a brief “Opinions About Methadone” scale. J Psychoactive Drugs. 2006;38:93–100. doi: 10.1080/02791072.2006.10399832. [DOI] [PubMed] [Google Scholar]
- 12.Esteban J, Gimcno C, Barril J, Aragones A, Climent JM, de la Cruz Pellin M. Survival study of opioid addicts in relation to its adherence to methadone maintenance treatment. Drug Alcohol Depend. 2003;70:193–200. doi: 10.1016/s0376-8716(03)00002-4. [DOI] [PubMed] [Google Scholar]
- 13.Bell J, Burrell T, Indig D, Gilmour S. Cycling in and out of treatment; participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend. 2006;81:55–61. doi: 10.1016/j.drugalcdep.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Vigezzi P, Guglielmino L, Marzorati P, et al. Multimodal drug addiction treatment: A field comparison of methadone and buprenorphinc among heroin- and cocaine-dependent patients. J Subsl Abuse Treat. 2006;31:3–7. doi: 10.1016/j.jsat.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Gerra G, Leonardi C, D’Amore A, et al. Buprenorphine treatment outcome in dually diagnosed heroin dependent patients: A retrospective study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:265–72. doi: 10.1016/j.pnpbp.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Strike CJ, Gnam W, Urbanoski K, Fischer B, Marsh DC, Millson M. Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addict Behav. 2005;30:1025–8. doi: 10.1016/j.addbeh.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93:51–60. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- 18.Puigdollers E, Domingo-Salvany A, Brugal MT, et al. Characteristics of heroin addicts entering methadone maintenance treatment: quality of life and gender. Subst Use Misuse. 2004;39:1353–68. doi: 10.1081/ja-120039392. [DOI] [PubMed] [Google Scholar]
- 19.Stein MD, Herman DS, Bishop S, et al. Sleep disturbances among methadone maintained patients. J Subst Abuse Treat. 2004;26:175–80. doi: 10.1016/S0740-5472(03)00191-0. [DOI] [PubMed] [Google Scholar]
- 20.Peles E, Kreek MJ, Kellogg S, Adelson M. High methadone dose significantly reduces cocaine use in methadone maintenance treatment (MMT) patients. J Addict Dis. 2006;25:43–50. doi: 10.1300/J069v25n01_07. [DOI] [PubMed] [Google Scholar]
- 21.Hartel DM, Schoenbaum EE, Selwyn PA, Friedland GH, Klein RS, Drucker E. Patterns of heroin, cocaine and speedball injection among Bronx (USA) methadone maintenance patients: 1978–1988. Addiction Research. 1996;3:323–40. [Google Scholar]
- 22.Bar-Hamburger R, Ezrachi Y, Rosiner I, Steinberg D. Final report: illegal use of drugs and alcohol in Israel, sixth national epidemiological survey. [Survey was done on 2005) Available from: http://www.antidrugs.org.il/ last updated October. 2007.
- 23.Weizman T, Gelkopf M, Melamed Y, Adelson M, Bleich A. Cannabis abuse is not a risk factor for treatment outcome in methadone maintenance treatment: a 1-year prospective study in an Israeli clinic. Aust N Z J Psychiatry. 2004;38:42–6. doi: 10.1046/j.1440-1614.2003.01296.x. [DOI] [PubMed] [Google Scholar]
- 24.Epstein DH, Preston KL. Does cannabis use predict poor outcome for heroin-dependent patients on maintenance treatment? Past findings and more evidence against. Addiction. 2003;98:269–79. doi: 10.1046/j.1360-0443.2003.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wasserman DA, Weinstein MG, Havassy BE, Hall SM. Factors associated with lapses to heroin use during methadone maintenance. Drug Alcohol Depend. 1998;52:183–92. doi: 10.1016/s0376-8716(98)00092-1. [DOI] [PubMed] [Google Scholar]
- 26.Iguchi MY, Handelsman L, Bickel WK, Griffiths RR. Benzodiazepine and sedative use/abuse by methadone maintenance clients. Drug Alcohol Depend. 1993;32:257–66. doi: 10.1016/0376-8716(93)90090-d. [DOI] [PubMed] [Google Scholar]
- 27.Bleich A, Gelkopf M, Weizman T, Adelson M. Benzodiazepine abuse in a methadone maintenance treatment clinic in Israel: characteristics and a pharmacotherapeutic approach. Isr J Psychiatry Relat Sci. 2002;39:104–12. [PubMed] [Google Scholar]
- 28.Russell C, Palmer JR, Adams-Campbell LL, Rosenberg L. Follow-up of a large cohort of Black women. Am J Epidemiol. 2001;154:845–53. doi: 10.1093/aje/154.9.845. [DOI] [PubMed] [Google Scholar]
- 29.Corrigan JD, Bogner JA, Mysiw WJ, Clinchot D, Fugate L. Systematic bias in outcome studies of persons with traumatic brain injury. Arch Phys Med Rehabil. 1997;78:132–7. doi: 10.1016/s0003-9993(97)90253-7. [DOI] [PubMed] [Google Scholar]
- 30.Peles E, Schreiber S, Gordon J, Adelson M. Significantly higher methadone dose for methadone maintenance treatment (MMT) patients with chronic pain. Pain. 2005;113:340–6. doi: 10.1016/j.pain.2004.11.011. [DOI] [PubMed] [Google Scholar]