Abstract
Oncolytic herpes simplex virus-1 (oHSV)–based vectors selectively replicate in tumor cells causing direct killing, ie., oncolysis, while sparing normal cells. oHSV’sare promising anticancer agents, but their efficacy, when used as single agents, leaves room for improvement. We hypothesized that combining the direct oncolytic and antiangiogenic activities of the IL-12 secreting NV1042 oHSV with microtubule disrupting agents (MDA’s) would be an effective means to enhance antitumor efficacy. Vinblastine (VB) was identified among several MDA’s screened that displayed consistent and potent cytotoxic killing of both prostate cancer and endothelial cell lines. In matrigel tube forming assays, VB was found to be highly effective at inhibiting tube formation of HUVEC cells. The combination of VB with NV1023 (the parental virus lacking IL-12) or NV1042 showed additive or synergistic activity against prostate cancer cell lines and was not due to increased oHSV replication by VB. In athymic mice bearing CWR22 prostate tumors, VB in combination with NV1042 was superior to the combination of VB plus NV1023 in reducing tumor burden, appeared to be nontoxic and resulted in a statistically significant diminution in the number of CD31+ cells as compared to other treatment groups. In human organotypic cultures using surgical samples from radical prostatectomies, both NV1023 and NV1042 were localized specifically to the epithelial cells of prostatic glands but not to the surrounding stroma. These data highlight the therapeutic advantage of combining the dual-acting anti-tumor and anti-angiogenic activities of oHSV’s and MDA’s.
Keywords: oncolytic HSV-1, prostate cancer, IL-12, angiogenesis, microtubule disrupting agents, combination therapy
Introduction
Selectively replication-competent viral vectors, such as oncolytic herpes simplex viruses type 1 (oHSVs) are genetically engineered from herpes-simplex virus (HSV) type I. These lytic viruses represent an attractive strategy for tumor-based therapies because they can specifically replicate and spread in cancer cells in situ, exhibiting oncolytic activity through direct cytopathic effects while sparing normal cells. Since the first report of a conditionally replicating genetically engineered virus1, a number of oHSV vectors have been developed which are highly effective against a myriad of solid tumors2-5. For example, NV1023 and the IL-12 expressing NV1042, are derived from an HSV1/2 intertypic mutant, which retains one copy of gamma34.5 gene6. NV1042 has been shown to inhibit squamous cell carcinoma growth through both antiangiogenic mechanisms as well as direct cytopathic effects7. We have shown that NV1042 is superior to the NV1023 parent vector in inhibiting prostate cancer growth of both primary and metastatic tumors via both immune and antiangiogenic mechanisms in syngeneic mouse models8-10. The antiangiogenic activity is due, in part, to the induction of IFNγ pro-inflammatory activities11. IFNγ affects the neovasculature through induction of the angiostatic chemokines CXCL9 (MIG) and CXCL10 (IP-10), up-regulation of VCAM-1 and inhibition of MMP9 expression12. Although IL-12 is also known to enhance antitumor response by inducing a Th1 response, it has also been shown that blood vessel formation is markedly decreased by IL-12 treatment in severe-combined immunodeficient (SCID) mice11, suggesting that the antiangiogenic effects of IL-12 is independent of T and B-cells.
Previously, we reported that the combination of oHSV plus a microtubule disrupting agent (MDA), ie.,docetaxel or paclitaxel, acts synergistically to promote prostate cancer cell killing in vitro and in vivo13. Similar synergestic interactions have been reported for another HSV-1 mutant as well as for vaccinia virus and reovirus in various cancers including prostate cancer14-16. In addition, studies involving the use of adenovirus mutants in combination with either paclitaxel or docetaxel have reported synergistic interactions in prostate cancer cells17,18. MDA’s have been shown to be effective inhibitors not only of tumor growth but also angiogenesis in numerous in vivo models19. In order to take additional advantage of a dual killing mechanism (tumor cells plus tumor endothelial cells) and to further improve upon the efficacy of currently available oncolytic vectors, we examined the strategy of using an “armed” oHSV expressing IL-12 combined with an MDA. We have evaluated the preclinical therapeutic effects of NV1042 (expressing IL-12) in combination with vinblastine and show that this combination enhances antitumor efficacy, in part by, inhibiting angiogenesis.
Materials and methods
Cells and viruses
Vero (African green monkey kidney), MS1 (mouse pancreatic endothelial), C166 (mouse yolk sac endothelial), CWR22 (human prostate cancer) and PC3 (human prostate cancer) cells were obtained from American Type Culture Collection (Manassas, VA) and human umbilical endothelial cells (HUVEC) from Lonza (Hopkinton, MA). HBME-1 (human bone marrow endothelial) cells were a generous gift from Dr. K. Pienta (University of Michigan). Vero cells were grown in DMEM supplemented with 10% calf serum and HUVEC in EGM-2. PC3 cells were grown in FK-1 media containing 10% heat-inactivated fetal calf serum (Hyclone, Logan, UT). Primary human prostate epithelial cells and its culture medium PrEGM were maintained as described by the manufacturer (Lonza). Construction of NV1023 and NV1042 has previously been described20. NV1023, derived from NV1020 (R7020), a HSV-1/HSV-2 intertypic recombinant developed as a vaccine strain21, contains an insertion of LacZ into the ICP47 locus, deleting ICP47, US11, and US1020. NV1042 is NV1023 with an insertion of murine IL-12 cDNA (p35 and p40 as a single polypeptide separated by elastin motifs) expressed from a hybrid α4-TK promoter20.
Cell Viability assays
Viability assays were performed over a 3 day period using the MTS assay kit (Promega, Madison, WI) in a 96-well format. The compounds used in this study included, Paclitaxel (Bristol-Myers Squibb, Princeton, NJ), docetaxel (Aventis Pharmaceuticals Inc., Bridgewater, NJ), vinblastine (APP Pharmaceuticals, Schaumburg, IL), epothilone-B (EpoB) (Sigma-Aldrich), vincristine (Hospira Inc, Lake Forest, IL) and 2-methoxyestradiol (2ME2) (Sigma-Aldrich).
Virus titration
Monolayer cultures of Vero cells grown in a six-well plate were infected with serial dilutions of virus. After removal of virus inoculum, the cells were incubated in DMEM supplemented with 1% inactivated FCS and 0.1%pooled human immunoglobulin at 37°C for 3-4 days until plaques were visible and counted.
Virus Replication assay
Cells were seeded in 12-well plate 1 day before infection and infected with NV1023 or NV1042 at a multiplicity of infection (MOI) of 1. At the times indicated, cells were harvested from the wells and viral titers were determined on Vero cells. Prostate cancer and endothelial cell lines either remained untreated or were pretreated with vinblastine (0.1nM) for 12h and thereafter, cells were infected with NV1023 or NV1042 at an MOI of 1.5. At 24 or 48h after infection, cells were scraped into the medium and subjected to three freeze-thaw cycles. Virus titers were determined by plaque assays on Vero cells. Each concentration in an experiment was plated in duplicate, and each experiment was performed three times. Supernatants collected from single burst assays were assayed for IL-12 derived from NV1042 at the indicated time points by ELISA(R&D Systems, Minneapolis, MN) and normal goat IgG (2 μg/ml/well) (R&D Systems) was included as a species-specific control.
Cell susceptibility assays and Chou–Talalay analysis
Prostate cancer (PC3 and CWr22) and endothelial (HUVEC, HBM-1, C166 and MS1) cells were seeded into 96-well plates at 1500-3000 cells per well. Viability assays will be performed over a 3 day period using the MTS assay kit (Promega) with a concentration range of MDA’s and varying MOI’s of oHSV. Dose-response curves were generated using GraphPad v5.0 (San Diego, CA). For Chou–Talalay analysis, dose– response curves and 50% effective dose values (ED50) were obtained and compared at day 3. For ED50 determination, cells were incubated for 3 days with varying concentrations or MOIs of drug and virus, respectively, and cell survival was then assessed using MTS assays. Dose–response curves were fit to Chou–Talalay lines, which are derived from the law of mass action and are described by the equation log(fa/fu)=m log D–m log Dm, in which fa is the fraction affected (percent cell death), fu is the fraction unaffected (percent cell survival), D is the dose, Dm is the median-effect dose (the dose causing 50% of cells to be affected, that is, 50% survival), and m is the coefficient signifying the shape of the dose–response curve. The combination index (CI)-isobologram by Chou and Talalay22 was used to analyze virus and drug combinations. Fixed ratios of virus and drug concentrations and mutually exclusive equations were used to determine CIs. All experiments were repeated at least three times.
Tube formation assay
HUVEC cells (~90,000 cells/well) were added to Matrigel™ (BD Biosciences) -coated 24-well plates. Four hours later, docetaxel (10nM), vinblastine (10 nM), vincristine (10nM), EpoB (10 μM) or 2ME2 (10 μM) were added in triplicate. For combination studies, NV1023 or NV1042 (MOI 1) with or without vinblastine (1 nM) were added. Twenty hours later tube formation was quantified by counting the branching points for each wellby light microscopy.
In vivo studies
CWr22 cells (5 × 106 cells) were implanted subcutaneously into the flanks of 6-to 8-week-old balb/c nu/nu mice (n=8 mice per group).When the tumor volume reached 75-150 mm3(~14 days after implantation) mice were stratified by tumor volume and then randomly assigned to treatment groups (n=8 per group).Virus [NV1023 or NV1042; 5×105 plaque-forming units (pfu)] or virus suspension buffer (PBS with 10% glycerol) was injected intratumorally on days 13 and 15 after tumor implantation. Vinblastine monotherapy or its combination with virus was administered intraperitoneally on day 15 at 0.35 mg/kg for nine consecutive days. All procedures were approved by the MGH Subcommittee on Research Animal Care. Tumor volume was calculated using the formula width (mm)2 × length (mm) × 0.52.
CD31 immunohistochemistry and quantification
Mice (n=3/group) were treated as described above and at day 30 post-implantation tumors were harvested, frozen and cut into tissues sections. Tissue sections were stained with a rat anti-mouse CD31 antibody (BD Biosciences, San Jose, CA) followed by secondary anti-rat IgG conjugated to HRP (GE Healthcare, Piscataway, NJ). CD31+ staining was revealed with 3,3′-diaminobenzidine (DAB) histochemistry (Vector Laboratories, Burlingame, CA). Sections were counterstained with hematoxylin (Sigma, St. Louis, MO). Tumor microvessel density was quantified for all treatment groups. At least 6-10 representative 40X fields per view were captured as epifluorescent digital images using a Spot digital camera (Spot Diagnostic instruments, Sterling, MI). To calculate microvessel density, area occupied by CD31-positive microvessels and total tissue area, per section were quantified using Image J software (NIH, Bethesda, MD). Microvessel density was then calculated as a percentage of CD31 stained per tumor section.
Prostate organ cultures
Prostate organ cultures were performed as previously described23. Briefly, tissue fragments were incubated with NV1023 (1 × 106pfu) or NV1042 (1 × 106pfu) for 1 h in direct contact and thereafter, placed on a semi-submersed collagen sponge (Ultrafoam™, Davol Inc., Warwick, RI) for 3 days. Tissue specimens (8 μm) were stained with anti-HSV-1 gC (Virusys Corp., Sykesville, MD, USA) or anti-cytokeratin-8/18 (UCD/PR-10.11, Dakocytomation, Carpinteria, CA, USA) antibodies as previously described. Virus titers were determined by titration of tissue homogenates on Vero cells using plaque assays. Tissues weights were determined to correct for viral titer concentrations. (Average±S.E.M). Each color dot indicates a different prostate surgical specimen that was separately infected with either NV1023 or NV1042 (n=5).
Statistical analysis
All statistical analyses were done using GraphPad prism v5. For comparison of efficacy and mechanism of efficacy, unpaired Student’s t test (two tailed) was used to analyze significance between two treatment groups.
Results
Evaluation of a panel of MDA’s on endothelial and prostate cancer cell lines
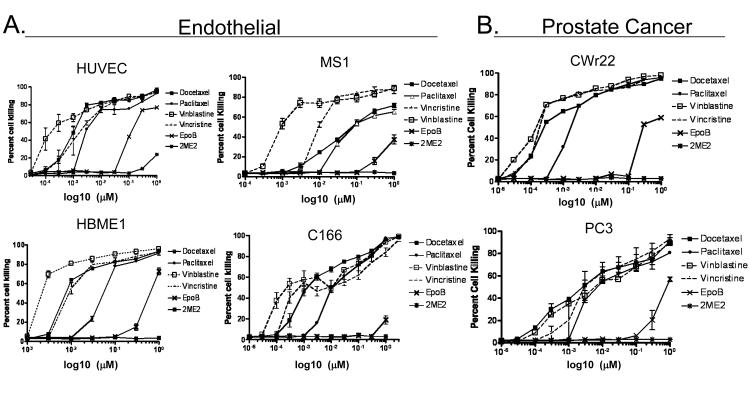
MDA’s have been shown to have broad-based antitumor and antiangiogenic properties19,24. We initially screened a series of MDA’s (docetaxel, paclitaxel, vinblastine, vincristine, epothilone-B and methoxyestradiol) on a panel of human (HUVEC, HBME1) and mouse-(MS1 and C166) derived endothelial and human prostate cancer cell lines. While the majority of MDA’s tested yielded potent cytotoxic effects on all four endothelial cell lines, vinblastine (VB), was consistently superior (EC50= 0.18-1.7 nM), demonstrating potent dose-dependent endothelial cell killing (Figure 1A; Table 1). In vitro matrigel assays, which partially recapitulate the mechanisms of neovascularizaion observed in vivo, confirmed that VB was highly effective at inhibiting tube formation of HUVEC cells (Supplementary Figure 1). Furthermore, in prostate cancer cell lines, VB was more or equally potent as the other MDA’s tested. For example, in the androgen-dependent CWR22 cell line, the cytotoxic effects of VB paralleled vincristine, while VB’s cytotoxic effects on the androgen-independent PC3 cell line was similar to vincristine, docetaxel and paclitaxel (Figure 1B; Table 1). In contrast, EpoB and 2-ME2 had negligible effects on both endothelial and tumor cell lines. Lastly, when endothelial (HUVEC and HBME) or prostate cancer cells (CWR22 and PC3) were treated with MDA’s for only 3 hrs and then washed away, VB was still cytotoxic, suggesting that even transient exposure of VB is effective (Supplemental Figure 2).
Figure 1.
Cytotoxic effects of MDA’s. (A) HUVEC (human umbilical vein endothelial cells) primary cultures and endothelial cell lines MS1 (mouse pancreatic), C166 (mouse yolk sac), HBME-1 (human bone marrow) and (B) Human CWR22 and PC3 prostate cancer cell lines were treated with increasing concentrations of the indicated MDA’s. MTS assays were performed on day 3 to determine the extent of cell killing.
Table 1.
| Doc | Pac | VB | VC | epoB | 2ME2 | ||
|---|---|---|---|---|---|---|---|
| PCa Endothelial | HUVEC | 0.88 ± 0.2 | 2.5 ± 1 | 0.18 + 0.04 | 1.7 ± 0.3 | 540 ± 56 | >1000 |
| HBME1 | 7.8 + 2 | 53 ± 12 | 1.7 + 0.5 | 8.6 ± 2 | 540 ± 45 | >1000 | |
| MS1 | 82 ± 11 | 98 ±14 | 1.6 + 0.4 | 8.2 ± 3 | >1000 | >1000 | |
| C166 | 1.9 ± 0.1 | 12 ± 4 | 0.38 + 0.1 | 0.64 ± 0.1 | >1000 | >1000 | |
| CWR22 | 0.28± 0.3 | 1.7 ± 0.7 | 0.27 ± .02 | 0.26 ± .03 | 290 ± 35 | >1000 | |
| Pc3 | 4.6 + 0.8 | 6.1 ± 1 | 7.8 ±1 | 6.3 ± 0.5 | 890 ± 76 | >1000 |
Values represent EC50’s; mean (nM) ±SEM; 3-day
In vitro assessment of oHSV and MDA combination
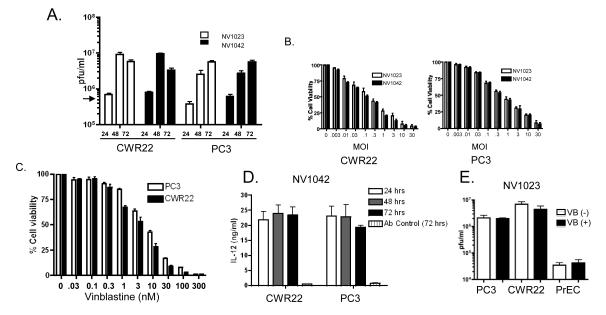
Previously, we reported that NV1023 and IL-12 secreting NV1042 were effective in vitro and in vivo at killing mouse prostate cancer cells8-10. To evaluate the cellular permissiveness of the human CWR22 and PC3 cancer cell lines toward NV1023 and NV1042, we performed viral burst assays. Figure 2A shows that by 48 hrs, virus production in CWR22 cells peaked, resulting in a ~32-fold increase in viral titers over input virus. By 72 hrs, the generation of virus progeny had plateaued. In PC3 cells, NV1023 and NV1042 virus production steadily increased over a 72 hr time period, resulting in a ~22-fold enhancement over input virus. Dose-response curves reflected the above findings, with both NV1023 and NV1042 more cytopathic toward CWR22 [EC50= 0.24; Multiplicity of infection (MOI)] than PC3 (EC50= 0.85 MOI) cells (Figure 2B). In addition, VB treatment of PC3 (EC50 = 7.8 nM) and CWR22 (EC50= 4.2 nM) resulted in a dose dependent response over a 3d period (Figure 2C). IL-12 secretion after NV1042 infection showed relatively high levels in both prostate cancer cell lines over a 72 period, even though differences in viral titers were observed between cell lines (Figure 2D).Lastly, both NV1023 and NV1042 (data notshown) can replicate to various degrees in the four aforementioned endothelial cell lines (Supplemental Figure 3).
Figure 2.
Analysis of NV1023 and NV1042 replication and effects on prostate cancer cell killing (A) Single burst assays were performed using either NV1023 or NV1042 (MOI =1.5) on CWR22 or PC3 cells over a 72 hr period. Virus (cell pellet plus supernatants) on days 1, 2 and 3 post-infection and viral titers (pfu/ml) determined by plaque assay on Vero cells as described previously13. Input virus: ~4×105 plaque forming units (pfu; indicated by arrow). (B) Cell susceptibility assays were performed using NV1023 or NV1042 on either CWR22 (left) or PC3 (right) prostate cancer cells. Cell lines were inoculated with the indicated MOI’s of virus and cell killing was evaluated by MTS assay on day 3 (error bars represent S.E.M.). (C) PC3 (open bar) or CWR22 (solid bar) prostate cancer cells were treated with increasing concentration of VB (0.01-100 nM) and MTS assays were performed to generate dose-response curves. (D) Supernatants collected from single burst assays were assayed for IL-12 derived from NV1042 by ELISA at the indicated time points. NV1023 was used as a control vector to normalize for background andnormal goat IgG control was also included to demonstrate specificity for murine IL-12. (E) Prostate cancer (PC3 and CWR22) and normal prostate epithelial (PrEC) cells were incubated in the presence or absence of non-toxic concentrations of VB (0.1 nM) for 12h and thereafter, cells were infected with NV1023 (MOI of 1.5) for 72 hrs. Virus titers were determined by plaque assay on Vero cells. Note that virus replication is not altered in the presence of VB and is negligible in PrEC.
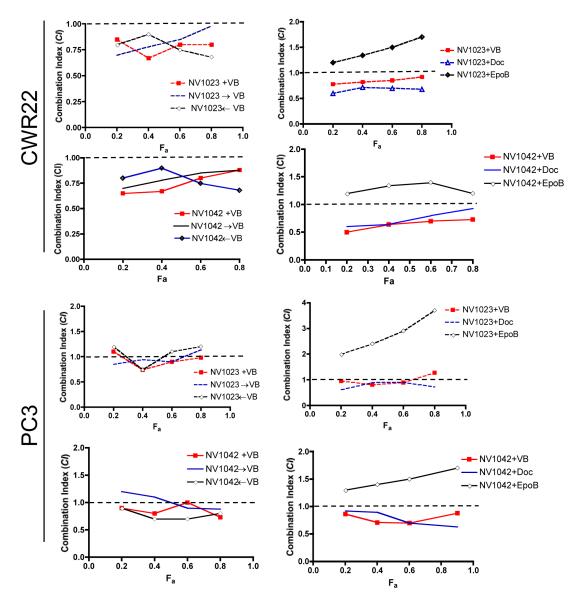
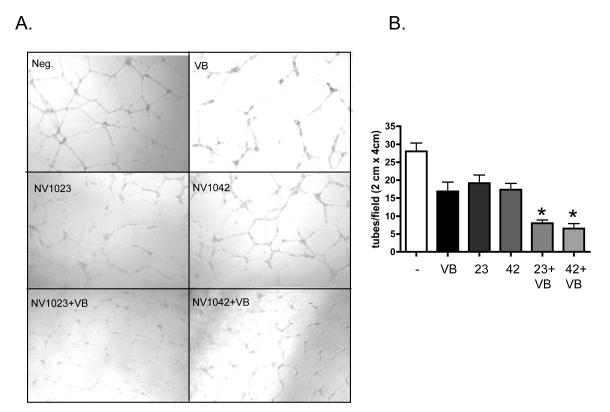
We used the combination index (CI) method of Chou-Talalay22 to assess whether the parental virus NV1023 in conjunction with VB could promote CWR22 or PC3 cell killing in a synergistic manner. A CI value of less than1 indicates synergism and CI>1 indicates antagonism. Mild synergism (CI~0.8) was observed when NV1023 or NV1042 (EC50= 0.24 MOI) and VB (EC50 = 4.2 nM) were added together in CWR22 cells (Figure 3). We further explored whether the observed synergistic effect was dependent on the timing of drug administration. A similar synergistic effect (CI~0.8) was observed regardless of whether VB was added 12hr before or after treatment of NV1023 or NV1042 (Figure 3C). Lastly, docetaxel but not EpoB could be substituted for VB in combination with NV1023 or NV1042 resulting in mild synergy (Figure 3C). In PC3 cells, the combination of NV1023 or NV1042 (EC50 = 0.85 MOI) with VB (EC50 =7.8 nM) resulted in an additive effect regardless of the order of administration. We also addressed whether the observed synergistic effects were due to increased oHSV replication by VB. The addition of a nontoxic concentration of VB (0.1 nM) to NV1023 neither increased nor decreased viral titers as compared to NV1023 alone at 48 hr after infection in single-step growth curve assays (Figure 2E). Lastly, in matrigel tube formation assays, we observed that the combination of either NV1023 or NV1042 (MOI 0.2) with VB (1 nM) was significantly more effective at disrupting tube formation than any single agent alone (Figure 4).
Figure 3.
Combination-Index analysis. Fraction affected (Fa) versus combination index plots were generated using the method of Chou and Talalay22 to determine the extent of synergy if any for either vinblastine (VB), docetaxel (Doc) or epothilone-B (EpoB) in combination with NV1023 or NV1042 in CWR22 (upper panels) and PC3 (lower panels) cell lines. (+) indicates simultaneous oHSV and drug addition; (→) indicates oHSV inoculation 24 hrs before drug treatment; (←) indicates drug treatment 24 hrs prior to oHSV infection. Synergistic effects are defined as combination index (CI) < 1 additive effects are CI=1, and antagonistic effects are CI>1. Note that the dotted line in each plot indicates a reference point of a CI value of 1.
Figure 4.
Increased antiangiogenic effects ofNV1042/vinblastine combination in an in vitro tube formation assay. HUVEC cells were plated on matrigel-coated plates and either remained untreated (Neg.) or treated with NV1023 or NV1042 (MOI 1), vinblastine (1nM) or their combination. Twentyhrs later, tube formation was scored. Representative fields are shown for each condition (A) and the number of tubes/field was quantified (B). Each treatment was performed in triplicate. Student’s t test was used to determine statistical significance between the indicated control and treatment groups. Bars represent average ± S.E.M..*, P< 0.01 for NV1023+VB and NV1042+VB verses NV1023 alone, NV1042 alone, VB alone or untreated.
Preclinical evaluation NV1023 or NV1042 with vinblastine in CWR22 xenografts
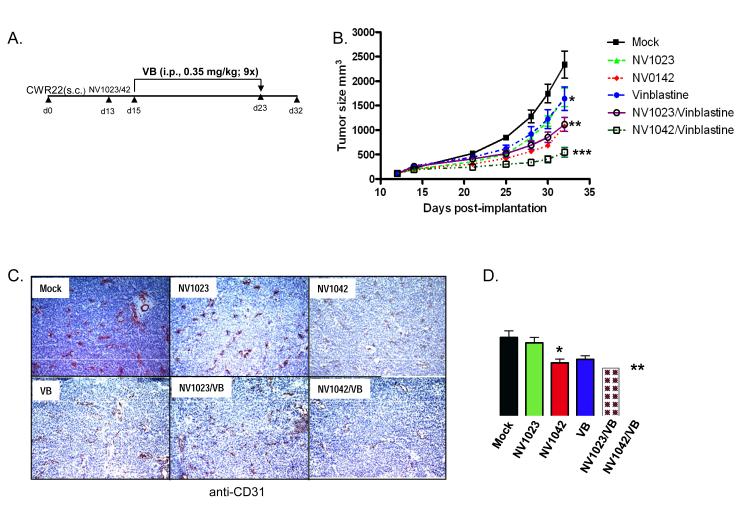
Next, we evaluated the in vivo antitumor efficacy of NV1023 or NV1042 in combination with VB in subcutaneous CWR22 tumors in athymic mice. Initially, doses of individual therapies were established to determine conditions resulting in tumor size reductions of 20-50% (data not shown). Mice were treated with either mock control, NV1023 or NV1042 (5×105pfu) on days 13 and 15, and/or VB (0.35 mg/kg; for 9 consecutive days) starting on day 15 (Figure 5A). By 32 days after tumor implantation, a statistically significant decrease in tumor volume was observed between control (2356±746) and all of the treatment groups (P < 0.05, *; P < 0.01, **) (Figure 5B). As compared with mock, treatment with NV1023 (1575±552), NV1042 (1087±254) and VB (1623±611) resulted in a notable reduction in tumor size; whereas the combination of NV1023/VB (1143±321) was superior to either therapy alone. Importantly, NV1042 plus VB (487+175, P < 0.01, ***), was significantly more effective than NV1023 plus VB or NV1042 alone. These combination therapies appeared to be nontoxic to mice as their body weight were not statistically different (Supplemenary figure 4). As the combination of NV1042/VB appeared to be more efficacious than any of the other treatment groups in reducing tumor volume, we hypothesized that this might be due, in part, to the combined antiangiogenic contributions of IL-12 and VB. This was tested using anti-CD31 antibody staining, which marks endothelial cells, on CWR22 tumor tissue sections. This revealed a reduction in CD31+ cells in the NV1042 plus VB treatment group as compared to the other treatment groups (Figure 5C). A statistically significant reduction in the number of CD31+ cells was observed in tumors treated with NV1042 plus VB as compared to all of the other treatment groups(P<0.05, **) (Figure 5D). In addition, statistically significant differences were also observed between NV1023and NV1042 treatment groups (P< 0.05, *), which is consistent with a previous report demonstrating a reduction of CD31-positive cells in murine prostate tumors treated with NV10428.
Figure 5.
In vivo efficacy studies. (A) Schematic illustrating the dosing and scheduling of single and combination treatment regimes in mice bearing s.c. CWR22 tumors. (B) Assessment of CWR22 tumor growth. Virus [NV1023 or NV1042; 5×105 plaque-forming units (pfu)] or virus suspension buffer (PBS with 10% glycerol) was injected intratumorally on days 13 and 15 after tumor implantation. Vinblastine was administered intraperitoneally at 0.35 mg/kg on day 15 for nine consecutive days. *, P< 0.05 for mock (n = 8) versus NV1023 only (n = 8) and VB only (n = 7); **, P< 0.01 for mock verses NV1042 only (n = 6) and NV1023 + VB (n = 6); ***, P< 0.01 for NV1042+VB (n = 7) verses NV1042 only and NV1023 + VB at day 32. (C) Evaluation of CD31+ staining (brown) as a function of treatment condition. Mice (n=3/group) were treated as described above and at day 30 post-implantation tumors were harvested, frozen and cut into tissues sections. Tissue sections were stained with a rat anti-mouse CD31 antibody and were counterstained with hematoxylin. (D) Quantification of CD31-positive staining. Tumor microvessel density was quantified for all treatment groups. Tumor microvessel density was compared between all treatment groups and untreated control group. (Mean ± S.E.M); * P< 0.04 for NV1023 verses NV1042; **, P<0.03 for NV1042 verses NV1042/VB.
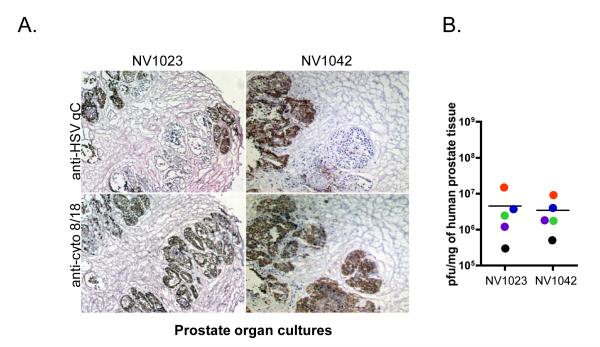
Lastly, we wished to confirm specificity in an additional model system representative of human prostate cancer. Recently, we reported the use of human prostate organ cultures using surgical specimens derived from radical prostatectomies to assess oHSV target specificity and replication competence23. We exploited this system to address the target specificity and replication competence of NV1023 and NV1042. At 3 days after infection, anti-HSV gC staining revealed that both NV1023 and NV1042 appeared to preferentially localize to the prostatic glandular regions in primary human prostate cancer tissues (Figure 6A). The staining of serial sections with anti-cytokeratin 8/18 antibody, which specifically stains luminal epithelial cells, confirmed that both vectors were restricted to epithelial cells and is in agreement with the restricted specificity of oHSV’s previously seen in prostate cancer tissues23. NV1023 and NV1042 replicated to similar degrees in five different prostate cancer tissue specimens examined (Figure 6B). Interestingly, the amount of replication for both viruses was similar in cultures from the same patient (same color dots, Fig 6B), as opposed to different patients.
Figure 6.
Analysis of NV1023 and NV1042 infection of prostate cancer surgical samples. Tissues were incubated with NV1023 (1 × 106pfu) or NV1042 (1 × 106pfu) for 1 h in direct contact and thereafter, placed on a semi-submersed collagen sponge for 3 days. (A) Tissue specimens were stained with anti-HSV-1 gC (upper panels) or anti-cytokeratin-8/18 (lower panels) antibodies. Sections were counterstained with hematoxylin. Note the partial overlap between anti-HSV gC and cytokeratin-8/18+ staining. (B) Evaluation of NV1023 or NV1042 replication in prostate organ cultures. Each color dot indicates a different prostate surgical specimen. Horizonal line denotes the average viral titer for the two groups, which are statistically not significant. Note that infection with NV1023 or NV1042 resulted in similar viral titers. The five specimens examined represent Gleason Scores of either 3+3=6 or 3+4=7.
Discussion
The discovery that tumors induce angiogenesis to generate new blood vessels for their growth and progression25,26 has recently led to numerous anti-angiogenic therapeutic strategies as well as demonstrated promise in improving the outcomes in cancer patients27. Our study focused on implementing a treatment regimen for prostate cancer by combining the antitumor and antiangiogenic activities of an “armed” oncolytic oHSV (NV1042) with a cytotoxic microtubule disrupting agent, vinblastine, in order to improve antitumor efficacy. Of the six microtubule disrupting agents (MDA) tested, we found vinblastine to be the most potent at killing not only prostate cancer cells but also all endothelial cells. This is in agreement with published observations that show that continuous treatment of VB at a low dose, can result in antiangiogenesis and sustained tumor regression28.
Strategies of “arming” oHSV’s with anti-angiogenic transgenes have also shown promise in various preclinical models. For instance, IL-12 expressing NV1042 has shown enhanced therapeutic efficacy over NV1023 in subcutaneous or metastatic lung murine prostate cancer TRAMP-C2 tumors9,10 and C3(1)/T-Ag breast cancers29. In addition, “armed” oHSV’s expressing other antiangiogenic agents such as dominant-negative fibroblast growth factor receptor, platelet factor-4 or angiostatin have been shown to substantially decrease blood vessel formation and increase survival30-32.
In vivo, we demonstrate that the combination of IL-12 expressing NV1042 with low dose VB can enhance CWR22 tumor killing by partially impairing endothelial cell growth and/or neovascularization. VB alone administered at a low dose (0.35mg/kg) over a 9-day period, or NV1042 monotherapies were effective at promoting tumor regression. However, in combination a superior antitumor effect was observed, accompanied by minimal adverse side effects, such as stable body weight. The decreased tumor growth elicited by combining NV1042 with VB was most likely due to the cooperative effect on blood vessels as shown by the significant decrease in CD31+ blood vessels as well as the cytotoxic effects on tumor cells by either agent. Angiogenesis is a complex process that involves multiple regulatory proteins and endothelial cell activation. Endothelial cells that make up existing blood vessels are activated to multiply and migrate as surrounding basement membrane and extracellular matrix is degraded to make way for new capillaries. IL-12 primarily modulates tumor growth by the recruitment of immune cells such as natural killer cells and T cells33. Our previous work addressed the antitumor and anti-angiogenic properties of the NV1042 expressing IL-12 virus in both syngeneic and transgenic mouse models of prostate cancer8-10. In this paper, our study focused on the anti-angiogenic effects of NV1042 in combination with vinblastine in human prostate cancers. Therefore, we utilized athymic xenograft models of prostate cancer, which lack T-cells and therefore, eliminates the tumor regression effects contributed by T-cells34. However, nude and SCID mice have relatively normal levels of NK-cells, which have been shown to contribute, in part, to the inhibition of angiogenesis by IL-1211,35. Our data show that NV1042 was superior to NV1023 either alone or in combination with vinblastine in slowing tumor growth in nude mice and that these results correlated with the percentage CD31+ blood vessels in tumor xenografts as a function of treatment condition.
Previous studies have shown that chemotherapy can enhance oncolytic viral replication36. In vitro, we did not observe any significant change in NV1042/NV1023 viral yield in the presence of vinblastine. This is in accordance with our previous findings, where pretreatment with nontoxic concentrations of taxanes had negligible effects on G47Δ replication13. A similar dose-range of either docetaxel or paclitaxel in combination with G47Δ significantly increased prostate cancer cell killing13. In the present study, irrespective of treatment sequence with the combination of NV1023/NV1042 and VB, a weak synergy-to-additive effect was observed. Because α-herpesviruses are dependent on intact microtubules for efficient transport and egress37, MDA treatment would be expected to compromise NV1023/N1042 replication, particularly under conditions where vinblastine was added prior to virus infection. Disruption of microtubules by MDA’s such as nocodazole or taxol (ie., paclitaxel), have shown varying effects on HSV-1 transport and replication. Avitabile and colleagues reported that neither MDA significantly affected the release of free virus into the media at micromolar concentrations38. In contrast, Kotaskis etal, reported that treatment of synchronized cells with nocadozale or taxol at similar concentrations prevented optimal HSV-1 replication39. These discrepancies may be attributed to whether cells were synchronized or alternatively, due to differences in the sensitivities of cells to nocodazole or taxol. A likely explanation for the observed weak synergy-to-additive effects is that at low VB concentrations, microtubules are minimally disrupted, which would allow for sufficient NV1023/NV1042 replication. In agreement these observations, the addition of G207 to nanomolar concentrations of paclitaxel resulted in weak synergy in promoting thyroid cancer cell killing with minimal effects G207 replication40.
Combination therapy regimens with anti-angiogenic agents will be critical to treat prostate cancer, as microvessel density has been shown to correlate strongly with Gleason grade and predict disease progression41,42. Although a recently concluded phase III trial of prostate cancer using bevacizumab (anti-VEGF antibody) in addition to the current standard of docetaxel and prednisone was negative43 other antiangiogenic strategies are worth exploring and the use of dual angiogenesis inhibition with direct oncolytic oHSV therapy is an attractive strategy for prostate cancer, and can hopefully be used to overcome resistance that is observed with anti-angiogenic monotherapies44.
Supplementary Material
Acknowledgments
We thank Melissa Marinelli for laboratory assistance. We also thank Dr. K. Pienta (University of Michigan) for the bone marrow-derived HBME-1 endothelial cells. The authors have no potential conflicts of interest.
Grant support: Support for this study was in part from a grant to RLM (R01CA102139).
References
- 1.Martuza RL, Malick A, Markert JM, Ruffner KL, Coen DM. Science. 1991;252:854–856. doi: 10.1126/science.1851332. [DOI] [PubMed] [Google Scholar]
- 2.Mineta T, Rabkin SD, Yazaki T, Hunter WD, Martuza RL. Attenuated multi-mutated herpes simplex virus-1 for the treatment of malignant gliomas. Nat Med. 1995;1:939–943. doi: 10.1038/nm0995-938. [DOI] [PubMed] [Google Scholar]
- 3.Varghese S, Rabkin SD. Oncolytic herpes simplex virus vectors for cancer virotherapy. Cancer Gene Ther. 2002;9:967–978. doi: 10.1038/sj.cgt.7700537. [DOI] [PubMed] [Google Scholar]
- 4.Kuruppu D, Tanabe KK. Viral oncolysis by herpes simplex virus and other viruses. Cancer BiolTher. 2005;4:524–531. doi: 10.4161/cbt.4.5.1820. [DOI] [PubMed] [Google Scholar]
- 5.Kaur B, Chiocca EA, Cripe TP. Oncolytic HSV-1 Virotherapy: Clinical Experience and Opportunities for Progress. Curr Pharm Biotechnol. 2011 doi: 10.2174/138920112800958814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong RJ, Patel SG, Kim S, DeMatteo RP, Malhotra S, Bennett JJ, et al. Cytokine gene transfer enhances herpes oncolytic therapy in murine squamous cell carcinoma. Hum Gene Ther. 2001;12:253–265. doi: 10.1089/10430340150218396. [DOI] [PubMed] [Google Scholar]
- 7.Wong RJ, Chan MK, Yu Z, Ghossein RA, Ngai I, Adusumilli PS, Stiles BM, Shah JP, Singh B, Fong Y. Angiogenesis inhibition by an oncolytic herpes virus expressing interleukin 12. Clin Cancer Res. 2004;10:4509–4516. doi: 10.1158/1078-0432.CCR-04-0081. [DOI] [PubMed] [Google Scholar]
- 8.Varghese S, Rabkin SD, Liu R, Nielsen PG, Ipe T, Martuza Enhanced therapeutic efficacy of IL-12, but not GM-CSF expressing oncolytic herpes simplex virus for transgenic mouse derived prostate cancers. Cancer Gene Ther. 2005;13:253–265. doi: 10.1038/sj.cgt.7700900. [DOI] [PubMed] [Google Scholar]
- 9.Varghese S, Rabkin SD, Nielsen PG, Wang W, Martuza RL. Systemic oncolytic herpes virus therapy of poorly immunogenic prostate cancer metastatic to lung. Clin Cancer Res. 2006;12:2919–2927. doi: 10.1158/1078-0432.CCR-05-1187. [DOI] [PubMed] [Google Scholar]
- 10.Varghese S, Rabkin SD, Nielsen GP, MacGarvey U, Liu R, Martuza RL. Systemic therapy of spontaneous prostate cancer in transgenic mice with oncolytic herpes simplex viruses. Cancer Res. 2007;67:9371–9379. doi: 10.1158/0008-5472.CAN-07-0674. [DOI] [PubMed] [Google Scholar]
- 11.Duda DG, Sunamura M, Lozonschi L, Kodama T, Egawa S, Matsumoto G, Shimamura H, Shibuya K, Takeda K, Matsuno S. Direct in vitro evidence and in vivo analysis of the antiangiogenesis effects of interleukin 12. Cancer Res. 2000;60:1111–1116. [PubMed] [Google Scholar]
- 12.Mitola S, Strasly M, Prato M, Ghia P, Bussolino F. IL-12 regulates an endothelial cell-lymphocyte network: effect on metalloproteinase-9 production. J Immunol. 2003;171:3725–3733. doi: 10.4049/jimmunol.171.7.3725. [DOI] [PubMed] [Google Scholar]
- 13.Passer BJ, Castelo-Branco P, Buhrman JS, Varghese S, Rabkin SD, Martuza RL. Oncolytic herpes simplex virus vectors and taxanes synergize to promote killing of prostate cancer cells. Cancer Gene Ther. 2009;7:551–560. doi: 10.1038/cgt.2009.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin SF, Gao SP, Price DL, Li S, Chou TC, Singh P, Huang YY, Fong Y, Wong RJ. Synergy of a herpesoncolytic virus and paclitaxel for anaplastic thyroid cancer. Clin Cancer Res. 2008;14:1519–1528. doi: 10.1158/1078-0432.CCR-07-4628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang B, Sikorski R, Kirn DH, Thorne SH. Synergistic anti-tumor effects between oncolyticvaccinia virus and paclitaxel are mediated by the IFN response and HMGB1. Gene Ther. 2011;18:164–172. doi: 10.1038/gt.2010.121. [DOI] [PubMed] [Google Scholar]
- 16.Heinemann L, Simpson GR, Boxall A, Kottke T, Relph KL, Vile R, Melcher A, Prestwich R, Harrington KJ, Morgan R, Pandha HS. Synergistic effects of oncolyticreovirus and docetaxel chemotherapy in prostate cancer. BMC Cancer. 2011;11:221. doi: 10.1186/1471-2407-11-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radhakrishnan S, Miranda E, Ekblad M, Holford A, Pizarro MT, Lemoine NR, Hallden G. Efficacy of oncolytic mutants targeting pRb and p53 pathways is synergistically enhanced when combined with cytotoxic drugs in prostate cancer cells and tumor xenografts. Hum Gene Ther. 2010;10:1311–1325. doi: 10.1089/hum.2010.019. [DOI] [PubMed] [Google Scholar]
- 18.Oberg D, Yanover E, Adam V, Sweeney K, Costas C, Lemoine NR, Halldén G. Improved potency and selectivity of an oncolytic E1ACR2 and E1B19K deleted adenoviral mutant in prostate and pancreatic cancers. Clin Cancer Res. 2010;16:541–553. doi: 10.1158/1078-0432.CCR-09-1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz EL. Antivascular actions of microtubule-binding drugs. Clin Cancer Res. 2009;15:2594–601. doi: 10.1158/1078-0432.CCR-08-2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong RJ, Patel SG, Kim S, DeMatteo RP, Malhotra S, Bennett JJ, St-Louis M, Shah JP, Johnson PA, Fong Y. Cytokine gene transfer enhances herpes oncolytic therapy in murine squamous cell carcinoma. Hum Gene Ther. 2001;12:253–265. doi: 10.1089/10430340150218396. [DOI] [PubMed] [Google Scholar]
- 21.Meignier B, Longnecker R, Roizman B. In vivo behavior of genetically engineered herpes simplex viruses R7017 and R7020: construction and evaluation in rodents. J Infect Dis. 1988;158:602–14. doi: 10.1093/infdis/158.3.602. [DOI] [PubMed] [Google Scholar]
- 22.Chou TC, Talalay P. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul. 1984;22:27–55. doi: 10.1016/0065-2571(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 23.Passer BJ, Wu C-l, S Wu C-l, Rabkin SD, Martuza RL. Analysis of genetically engineered oncolytic herpes simplex viruses in human prostate cancer organotypic cultures. Gene Ther. 2009;16:1477–1482. doi: 10.1038/gt.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanthou C, Tozer GM. Tumour targeting by microtubule-depolymerizing vascular disrupting agents. Expert Opin Ther Targets. 2007;11:1443–1457. doi: 10.1517/14728222.11.11.1443. [DOI] [PubMed] [Google Scholar]
- 25.Folkman J. Anti-angiogenesis: new concept for therapy of solid tumors. Ann Surg. 1972;175:409–416. doi: 10.1097/00000658-197203000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 27.Folkman J. Angiogenesis: an organizing principle for drug discovery? Nat Rev Drug Discov. 2007;6:273–286. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 28.Klement G, Baruchel S, Rak J, Man S, Clark K, Hicklin DJ, Bohlen P, Kerbel RS. Continuous low-dose therapy with vinblastine and VEGF receptor-2 antibody induces sustained tumor regression without overt toxicity. J Clin Invest. 2000;105:R15–24. doi: 10.1172/JCI8829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu R, Varghese S, Rabkin SD. Oncolytic herpes simplex virus vector therapy of breast cancer in C3(1)/SV40 T-antigen transgenic mice. Cancer Res. 2005;65:1532–1540. doi: 10.1158/0008-5472.CAN-04-3353. [DOI] [PubMed] [Google Scholar]
- 30.Liu TC, Zhang T, Fukuhara H, Kuroda T, Todo T, Canron X, Bikfalvi A, Martuza RL, Kurtz A, Rabkin SD. Dominant-negative fibroblast growth factor receptor expression enhances antitumoral potency of oncolytic herpes simplex virus in neural tumors. Clin Cancer Res. 2006;12:6791–6799. doi: 10.1158/1078-0432.CCR-06-0263. [DOI] [PubMed] [Google Scholar]
- 31.Liu TC, Zhang T, Fukuhara H, Kuroda T, Todo T, Martuza RL, Kurtz A, Rabkin SD. Oncolytic HSV armed with platelet factor 4, an antiangiogenic agent, shows enhanced efficacy. MolTher. 2006;14:789–797. doi: 10.1016/j.ymthe.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Zhang W, Fulci G, Buhrman JS, Stemmer-Rachamimov AO, Chen JW, Wojtkiewicz GR, Weissleder R, Rabkin SD, Martuza RL. Bevacizumab With Angiostatin-armed oHSV Increases Antiangiogenesis and Decreases Bevacizumab-induced Invasion in U87 Glioma. MolTher. 2012;1:37–45. doi: 10.1038/mt.2011.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colombo MP, Trinchieri G. Interleukin-12 in anti-tumor immunity and immunotherapy. Cytokine Growth Factor Rev. 2002;13:155–168. doi: 10.1016/s1359-6101(01)00032-6. [DOI] [PubMed] [Google Scholar]
- 34.Voest EE, Kenyon BM, O’Reilly MS, Truitt G, D’amato RJ, Folkman J. Inhibition of Angiogenesis In Vivo by Interleukin 12. JNCI. 1995;87:581–586. doi: 10.1093/jnci/87.8.581. [DOI] [PubMed] [Google Scholar]
- 35.Yao L, Sgadari C, Furuke K, Bloom ET, Teruya-Feldstein J, Tosato G. Contribution of natural killer cells to inhibition of angiogenesis by interleukin-12. Blood. 1999;5:1612–1621. [PubMed] [Google Scholar]
- 36.Yu DC, Chen Y, Dilley J, Li Y, Embry M, Zhang H, Nguyen N, Amin P, Oh J, Henderson DR. Antitumor synergy of CV787, a prostate cancer-specific adenovirus, and paclitaxel and docetaxel. Cancer Res. 2001;61:517–525. [PubMed] [Google Scholar]
- 37.Penfold MET, Armati P, Cunningham AL. Axonal transport of herpes simplex virions to epidermal cells: Evidence for a specialized mode of virus transport and assembly. Proc Natl Acad Sci USA. 91:6529–6533. doi: 10.1073/pnas.91.14.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Avitabile E, Di Gaeta S, Torrisi MA, Ward PL, Roizman B, Campadelli-Fiume G. Redistribution of microtubles and golgi apparatus in herpes simplex virus-infected cells and their role in viral exocytosis. J Virol. 1995;69:7472–782. doi: 10.1128/jvi.69.12.7472-7482.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kotaskis A, Pomeranz LE, Blouin A, Blaho JA. Microtubule reorganization during herpes simplex virus type I infection facilitates nuclear localization of VP22, a major virion tegment protein. J Virol. 2001;75:8697–8711. doi: 10.1128/JVI.75.18.8697-8711.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin S-F, Gao SP, Price DL, Li S, Chou T-C, Singh P, Huang Y-Y, Fong Y, Wong RJ. Synergy of a Herpes Oncolytic Virus and Paclitaxel for Anaplastic Thyroid Cancer. Clin Cancer Res. 2008;14:1519–1528. doi: 10.1158/1078-0432.CCR-07-4628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weidner N, Carroll PR, Flax J, Blumenfeld W, Folkman J. Tumor angiogenesis correlates with metastasis in invasive prostate carcinoma. Am J Pathol. 1993;143:401–409. [PMC free article] [PubMed] [Google Scholar]
- 42.Gettman MT, Pacelli A, Slezak J, Bergstralh EJ, Blute M, Zincke H, Bostwick DG. Role of microvessel density in predicting recurrence in pathologic Stage T3 prostatic adenocarcinoma. Urology. 1999;54:479–485. doi: 10.1016/s0090-4295(99)00202-2. [DOI] [PubMed] [Google Scholar]
- 43.Kelly WK, Halabi S, Carducci M, George D, Mahoney JF, Stadler WM, Morris M, Kantoff P, Monk JP, Kaplan E, Vogelzang NJ, Small EJ. Randomized, Double-Blind, Placebo-Controlled PhaseIII Trial Comparing Docetaxel and Prednisone With or Without Bevacizumab in Men With Metastatic Castration-Resistant Prostate Cancer: CALGB 90401. J Clin Oncol. 2012;30:1534–1540. doi: 10.1200/JCO.2011.39.4767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kerbel RS, Yu J, Tran J, Man S, Viloria-Petit A, Klement G, Coomber BL, Rak J. Possible mechanisms of acquired resistance to anti-angiogenic drugs: implications for the use of combination therapy approaches. Cancer Metastasis Rev. 2001;20:79–86. doi: 10.1023/a:1013172910858. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.