Abstract
Objective
We introduce The Psychological Adaptation Scale (PAS) for assessing adaptation to a chronic condition or risk and present validity data from six studies of genetic conditions.
Methods
Informed by theory, we identified four domains of adaptation: effective coping, self-esteem, social integration, and spiritual/existential meaning. Items were selected from the PROMIS “positive illness impact” item bank and adapted from the Rosenberg self-esteem scale to create a 20-item scale. Each domain included five items, with four sub-scale scores. Data from studies of six populations: adults affected with or at risk for genetic conditions (N=3) and caregivers of children with genetic conditions (N=3) were analyzed using confirmatory factor analyses (CFA).
Results
CFA suggested that all but five posited items converge on the domains as designed. Invariance of the PAS amongst the studies further suggested it is a valid and reliable tool to facilitate comparisons of adaptation across conditions.
Conclusion
Use of the PAS will standardize assessments of adaptation and foster understanding of the relationships among related health outcomes, such as quality of life and psychological well-being.
Practice Implications
Clinical interventions can be designed based on PAS data to enhance dimensions of psychological adaptation to a chronic health condition or risk.
1. Introduction
The diagnosis of a genetic condition, or the identification of an increased risk for a disease, poses a threat to one’s health that leads to stress. How successfully an individual manages that stress determines how well they adapt to the condition over time. One goal of genetic counseling is to facilitate adaptation to a genetic condition or risk (1). Yet research to identify client needs related to adaptation has been thwarted by a lack of consistency in how the concept is defined and measured (2). This problem has resulted in limited studies into factors associated with adaptation, particularly those that may be amenable to clinical intervention. The lack of standardized measures of adaptation has precluded meta-analysis of the studies that have been done. Similarly, the association between adaptation and related health outcomes, such as quality of life and psychological wellbeing has been relatively unexamined.
Insight into factors that contribute to adaptation can be gained from models of chronic illness. Lazarus and Folkman’s Transactional Model of Stress and Coping outlines the relationship of primary and secondary stress appraisals to coping strategies, and ultimately adaptation (3). Appraisals refer to an assessment of the degree of stress and ways to control or manage it. Examples include perceived risk, illness perceptions, perceived personal control, self–efficacy, and past coping success. Coping that stems from such appraisals may be more or less effective in fostering adaptation (4,5). When successful, adaptation can be viewed as a positive outcome of responding to a health threat. Similarly, Taylor (6) defined three critical components in the Cognitive Theory of Adaptation: meaning making, mastery, and self-esteem. A number of studies of adaptation to common and chronic illness have generated empirical evidence to support these theories (7-9). However, the conceptualization and assessment of adaptation among these studies has varied significantly.
We previously defined adaptation as the dynamic and multi-dimensional process of coming to terms with the implications of a health threat and the outcomes of that process (2). Other names for this construct that appear in the literature include adjustment and acceptance, measured using a variety of scales that assess related but distinct constructs including psychological well-being, physical functioning, anxiety and depression (2). For example, Wakefield and colleagues review of eight studies of caregiver “adjustment” to a pediatric cancer diagnosis yielded scales measuring at least eight distinct outcomes (10). They were: symptoms of post-traumatic stress disorder (Impact of Events Scale and Reaction Index), general health (General Health Questionnaire), family impact (Important Family Events Scale), resilience (SSERQ), anxiety (STAI), psychological distress (GHQ), family life (Family Life Scale) and family needs (Family Needs Survey). The array of scales used precludes a meta-analysis of adaptation/adjustment and exemplifies the lack of consensus in distinguishing and assessing adaptation. We argue the need for a more explicit measure of the construct of adaptation enabling across-study comparisons.
We introduce the Psychological Adaptation Scale (PAS), which measures adaptation to a chronic condition or disease risk. Our objective in developing the PAS was to create a succinct scale grounded in existing theory to assess the cognitive and emotional outcomes of coping. To that end, we strived to select key components of adaptation, thereby simplifying a complex outcome. Although we recognize adaptation as a dynamic and multi-dimensional construct that occurs over time, the PAS was designed to capture the extent of adaptation at a single time point. We developed the PAS with four sub-scales representing each of the domains and the intention for the four sub-scales to represent an overall score of adaptation. Important related outcomes of living with the stress of a health threat include: quality of life, psychological well-being and depressive symptoms. By differentiating adaptation from these outcome measures and assessing how they are related, we hope to clarify prior theoretical and empirical work on adaptation and to eventually improve clinical outcomes.
The purpose of this study is to confirm the factor structure and reliability of the PAS, including invariance of the factor structure across six diverse populations including individuals with disease or at risk for disease and caregivers of children with a condition.
2. Methods
Both the Transactional Theory of Stress and Coping (3) and the Cognitive Theory of Adaptation (6) were used to guide the selection of four domains of adaptation included in the PAS. The domains are coping efficacy, self-esteem, spiritual/existential well being, and social integration. Coping appears as a key mediator of adaptation in both theories and informed our choice of coping efficacy as the first domain. Taylor’s theory further elucidates a key role for self-esteem, “meaning making” that leads to existential wellbeing, and re-engagement in social encounters. Using the domains as a guide, individual items were adapted from the Patient-Reported Outcomes Measurement Information System® (PROMIS®) item banks measuring psychological illness impact (http://www.nihpromis.org/) for three of the four domains. All items in the PROMIS item banks had been found to be valid and reliable indicators of “psychological illness impact” through extensive qualitative and quantitative evaluation. We selected among a set of about 200 items labeled “coping response,” “spirituality” and “social support” that were ranked highly by the PROMIS psychometricians for content validity and good psychometric performance. Items for the self-esteem subscale were adapted from Rosenberg’s self-esteem scale (11). Both of these item resources are in the public domain. Overall, five items were selected for each subscale after consensus assessment of how well the items represented each of the four domains. In constructing the PAS, the first five items composed coping efficacy, the next five self-esteem, the next social integration and the last five, spiritual/existential well-being for an overall scale of 20 items.
The PAS was used in studies of six populations: adults affected with neurofibromatosis type I, boys and men affected with Klinefelter (XXY) syndrome, adults at risk for Huntington disease (HD), parents of children with autism spectrum disorder (ASD), parents of children with Down syndrome, and parents of children with Rett syndrome (12-17). Only respondents who had completed the PAS were included in the factor analyses (see Table 1). The studies were conducted primarily via electronic surveys, recruiting from relevant on-line support groups, blogs and websites. All were cross-sectional studies with related but distinct research questions assessing factors associated with the primary outcome, adaptation. In all cases adaptation was assessed using the PAS and secondary outcomes, such as depressive symptoms (CES-D) (18), hope (Trait Hope Scale) [19], quality of life (QLI) [20], and family functioning (FAM III) [21], were assessed in one or more of the studies.
Table 1.
Sample Characteristics from Six Studies included in the CFA
| Boys and Men with XXY | Caregivers of children with Down Synd | Adults with NF1 | Caregivers of children with Rett Synd | Adults at risk for HD | Caregivers of children with ASD | |
|---|---|---|---|---|---|---|
| Used in CFA analysis/Total N | 231/310 | 512/546 | 509/509 | 388/426 | 189/191 | 324/324 |
|
| ||||||
| Age (years) | ||||||
| Mean (SD) | 40.7 (14) | 41.7 (8.8) | 38.9 (11.4) | 43.3 (9.7) | 37.2 (11.1) | 40.7 (7.2) |
| Range | 14-75 | 21-84 | 18-69 | 22-74 | 18-75 | |
|
| ||||||
| Child Age | ||||||
| Mean (SD) | --- | 7.8y (7.8) | --- | 12.6 (9.4) | --- | 9.5 (5.6) |
| Range | --- | 0-48 | --- | 1.6-50 | --- | 1.9-37 |
|
| ||||||
| Race (%) | ||||||
| Caucasian | 92.2 | 94.0 | 88.4 | 93.1 | 89.6 | 92.0 |
| Black/African American | 0.8 | 1.7 | 5.7 | 3.6 | 2.6 | 3.1 |
| Asian | 2.1 | 2.2 | 5.1 | 2.8 | 6.3 | 1.2 |
| American Indian/Alaska Native | 0.8 | 1.6 | 2.7 | 1.5 | 1.0 | 2.8 |
| Native Hawaiian/Pacific | 0 | 0.4 | 1.1 | 0 | Assessed with | 0.9 |
| Islander | Asian | |||||
| >1 race indicated | 4.1 | --- | --- | --- | --- | --- |
|
| ||||||
| Ethnicity (%) | ||||||
| Not Hispanic or Latino | 97.1 | 93.9 | 93.5 | 93.8 | 92.2 | 95.4 |
| Hispanic or Latino | 2.9 | 6.1 | 6.5 | 6.2 | 7.8 | 4.6 |
|
| ||||||
| Education Level (%) | ||||||
| Elementary/Junior High | 4.1 | 0 | 3.7 | 1.3 | --- | .06 |
| High school/GED | 22.2 | 7.0 | 20.6 | 12.3 | 8.9 | 6.8 |
| Technical school | 13.6 | 3.4 | --- | 4.3 | 28.3 (plus some college) | 3.4 |
| Some college | 22.6 | 18.8 | 28.9 | 24.7 | See above | 18.8 |
| Completed college | 23.9 | 36.3 | 30.8 | 33.8 | 36.6 | 40.1 |
| Post-graduate | 13.6 | 34.5 | 16.0 | 23.7 | 25.1 | 30.2 |
|
| ||||||
| Marital Status (%) | ||||||
| Single | 39.8 | 2.9 | 36.1 | 2.0 | 35.1 | 4.6 |
| In a partnered relationship | 11.5 | --- | 10.6 | 1.8 | --- | --- |
| Married | 38.1 | 89.0 | 41.9 | 85.2 | 56.6 | 80.2 |
| Divorced or separated | 9.8 | 6.3 | 9.3 | 9.8 | 7.3 | 13.9 |
| Widowed | 0.8 | 1.8 | 2.1 | 1.3 | 1.0 | 1.2 |
|
| ||||||
| Annual Income | ||||||
| Greater than $70,000 | 61.8 | 13.3 | 55.6 | --- | 51.2 | |
| $50,001 - 70,000 | 20.0 | 12.8 | 18.2 | --- | 17.0 | |
| $30,000 - 50,000 | 11.5 | 24.7 | 15.4 | --- | 17.6 | |
| Less than $30,000 | 6.7 | 49.2 | 10.8 | --- | 14.2 | |
Statistical Analysis
The goal of the analysis was to assess the validity and reliability of the 20-item PAS measure in Figure 2 for establishing a scale for adaptation for each condition. In addition, the level of invariance of the scale across the conditions was assessed to identify whether a common scale could be designed that would be applicable across all the conditions.
Figure 2.
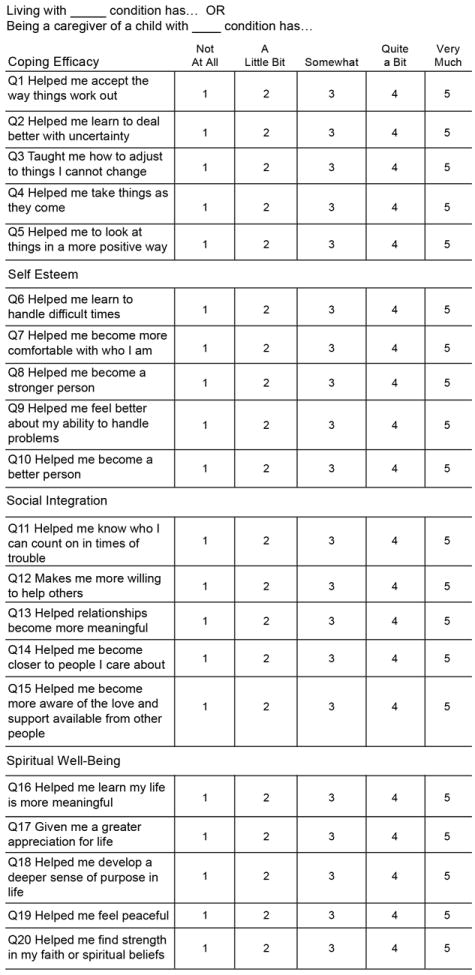
PAS
The measurement model in Figure 3*, which hypothesizes that the 20 scale items are indicators of the four constructs related to someone’s degree of adaptation to a genetic condition or risk for a disease, was fit to each data set using confirmatory factor analysis (CFA) with AMOS 16. The resulting models were evaluated using a typical set of CFA model fit measures including a chi-square goodness-of-fit statistic (χ2), the goodness-of-fit index (GFI), the adjusted goodness-of-fit *index (AGFI), the root mean square error of approximation (RMSEA) and the comparative fit index (CFI). Since the χ2 often yields significant values for large data sets, the resulting models were deemed to be supported by the data if the normed χ2 (χ2 /degrees of freedom) < 3 and the other measures satisfied GFI >0 .9, AGFI > 0.8, RMSEA < 0.1 and CFI > 0.9. In addition to measures of model fit, construct validity for each construct was established by assessing convergent validity (standardized loadings >0 .5, construct reliability > 0.7 and average variance extracted >0 .5) and discriminant validity (average variance extracted greater than the squared correlation).[22] Maximum likelihood estimation (MLE) was used to fit the models. Since all the data sets violated multivariate normality and exhibited outliers, bootstrapping was used to demonstrate that any resulting bias present in the MLE parameter estimates was negligible. Consequently, the MLE parameter estimates are utilized for the purposes of this analysis.
Figure 3.
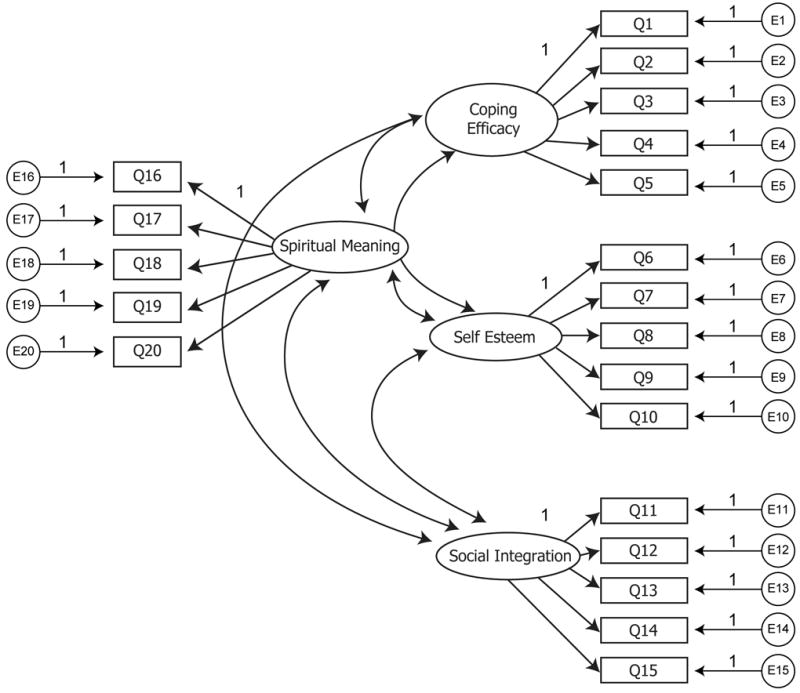
Measurement Model
In addition to fitting a CFA model to each data set, a multi-group analysis [22] was used to assess the level of model invariance and the extent to which the same CFA model was supported across all the data sets. Configural invariance requires that the same factor structure is supported by all the data sets. We tested this by fitting the common model to all the data sets simultaneously and evaluating the fit using the same criteria mentioned above for the individual CFA models. Metric invariance assumes configural invariance and also requires that the factor loadings for the indicator variables are equal across all groups. If configural invariance can be established, then metric invariance can be tested by constraining the factor loadings for the common factor structure to be equal across groups and comparing the results with the unconstrained model using a χ2 difference test. We also tested for partial invariance when full invariance was not supported. For example, partial metric invariance requires that the same factor structure is appropriate across groups and that at least two factor loadings are equal across groups for each factor.
Results
The original hypothesized model for adaptation as represented in Figure 3 was not supported by the data for any of the groups. In particular, low communalities and other model diagnostics suggested that Q5, Q11, Q12, Q19 and Q20 should be reviewed for exclusion from the model. Review of these questions in light of the CFA diagnostics, suggested that Q19 and Q20 were qualitatively slightly different in content than the other items in the Spiritual Well-Being subscale (Q16, Q17 and Q18). Similarly, Q11 and Q12 were slightly different than the other items in the Social Integration sub-scale (Q13, Q14 and Q15). Q5 appeared to be quite generic compared to the other questions on the coping efficacy construct. These observations caused us to refine the model by eliminating these items. The reduced model represented in Figure 4 provided an acceptable fit to the data for each group (i.e. each model satisfied the overall model fit statistics indicated earlier, had standardized loadings >.5, construct reliabilities >.8, variance extracted > .5 and exhibited discriminant validity). In two of the models, the standardized loadings for Q15 were 0.4 but all the other measures indicated an acceptable fit, so Q15 was retained.
Figure 4.
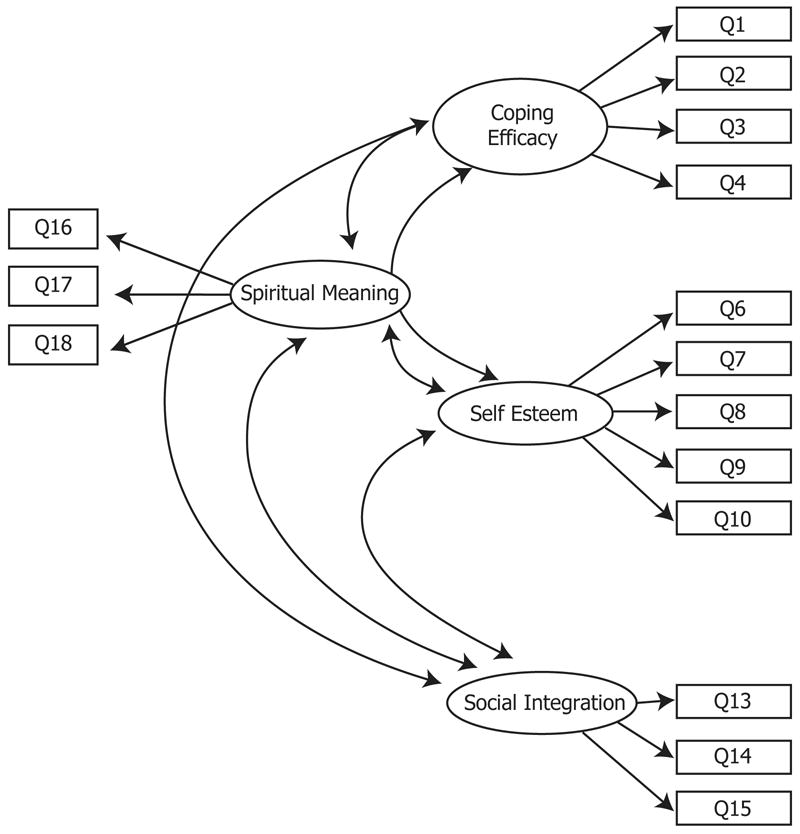
Reduced Model
To assess configural invariance across all data sets, the model in Figure 4 was fit simultaneously to all the groups. The resulting model fit statistics (χ2 = 1465.8 and 504 degrees of freedom (p< .01), normed χ2 = 2.9, GFI = 0.92, AGFI = 0.88, CFI = 0.96 and RMSEA = 0.03) indicated that full configural invariance was supported for the factor structure represented. Full metric invariance was evaluated by fitting the model simultaneously to all the groups under the restriction that all the factor loadings were equal across the six groups. The difference in the chi-square values for the constrained and unconstrained model was 223.5 with 55 degrees of freedom (p = 0) indicating that full metric invariance was not supported. Partial metric invariance was investigated assuming equality of the loadings for Q1, Q2, Q6, Q9, Q10, Q13, Q14, Q16 and Q18 (i.e. at least two factor loadings are the same across groups) which resulted in a chi-square difference test (Δχ2=30.4, df=25, p=.21). This result confirmed that the data supported partial metric invariance for the model in Figure 4. In addition, the fit statistics (GFI=.92, AGFI=.89, CFI=.96 and RMSEA=.029) also supported partial metric invariance. Partial metric invariance appears to be the strongest conclusion that can be drawn for the PAS measure based on the samples included in the analysis. The resulting loadings for the various diseases are given in Table 2 where the invariant loadings are bolded to highlight the partial invariance.
Table 2.
Loadings
| Boys/Men with XXY | Caregivers Down syn | Adults with NF | Caregivers Rett syn | Adults at risk HD | Caregivers ASDs | |
|---|---|---|---|---|---|---|
| Coping Efficacy | ||||||
| Q1 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Q2 | 1.10 | 1.10 | 1.10 | 1.10 | 1.10 | 1.10 |
| Q3 | 1.06 | 1.04 | 1.21 | 0.99 | 1.11 | 1.05 |
| Q4 | 0.99 | 1.00 | 1.22 | 0.95 | 0.98 | 1.05 |
|
| ||||||
| Self Esteem | ||||||
| Q6 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Q7 | 1.12 | 1.24 | 0.95 | 1.30 | 1.15 | 1.15 |
| Q8 | 1.18 | 0.96 | 1.14 | 1.03 | 1.14 | 0.95 |
| Q9 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 |
| Q10 | 1.07 | 1.07 | 1.07 | 1.07 | 1.07 | 1.07 |
|
| ||||||
| Social Integration | ||||||
| Q13 | 0.96 | 0.96 | 0.96 | 0.96 | 0.96 | 0.96 |
| Q14 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Q15 | 0.90 | 0.67 | 0.93 | 0.65 | 1.0 | 0.80 |
|
| ||||||
| Spiritual Well - Being | ||||||
| Q16 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Q17 | 1.07 | 0.91 | 1.05 | 0.89 | 1.02 | 0.97 |
| Q18 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
4. Discussion and Conclusion
4.1 Discussion
The use of confirmatory factor analysis meets a high standard for validation of a new measure. Our analysis was strengthened by the use of six unique studies of sizable cohorts. The items were correlated to the domains that they were intended to, with the exception of five items that did not contribute to the overall measure. Upon close inspection, these items did vary slightly in content from the others. The PAS can be used with the five items removed without jeopardizing its validity. Our plans are to identify news items for each domain that are consistent with the content of the residual items, use the scale in future studies and re-assess its factor structure. We are planning higher order analysis of the validity of the four domains in representing a single construct of adaptation. Data obtained in these six and additional studies on related health outcomes (ie, quality of life, psychological well-being and depressive symptoms) will provide valuable concurrent and discriminant validity data on the efficacy of the PAS in measuring a distinct but related variable. Additional use of the scale with related health outcomes will provide further understanding of its relationship among a number of psychological outcomes and personality traits such as dispositional optimism and resilience.
Our intentions are to use the PAS to evaluate how the scale performs in prospective studies of adaptation. Longitudinal studies are planned to explore change over time. Adaptation is a dynamic process and understanding the impact of interventions on adaptation, such as those aimed at enhancing coping efficacy (23, 24), will help to assess ways providers may effectively intervene.
We also hope to use the PAS among members of the same family to compare relative adaptation. Such studies will facilitate understanding of the degree of similarity in adaptation among relatives. These efforts are expected to expand understanding of a dynamic process and to identify families who may be in greatest need of intervention studies to enhance adaptation.
We began use of the PAS in studies of genetic conditions or living at risk as relevant to our expertise and the recognized need for improved outcome measures in genetic counseling (25). However, the PAS can be used to study common chronic illnesses generally. Use of the PAS in a population of parents of children with autism spectrum disorders provides evidence to support this claim.
Limitations
The PAS is likely limited in its representation of the complex process of adapting to a significant health threat. Yet it contains four key domains central to the construct and excludes sub-scales on related but distinct constructs. As such, the PAS improves upon existing measures of adaptation/acceptance and offers a single measure that may facilitate measurement consistency across studies.
It is possible that removing the five items from the PAS may have an impact on the domain that each subscale is measuring. Yet in the remaining items closely resemble one another in content and in representing the intended construct.
There was a lack of racial/ethnic diversity in the population samples among the six studies potentially limiting its generalizability.
4.2 Conclusion
We suggest that the PAS may be a robust measure of four key domains of the state of adapting to the stress generated by a chronic disease, or a chronic disease in one’s child. Future use of the PAS will add clarity to variables associated with adaptation, particularly those that may be useful targets for intervention studies.
4.3 Practice implications
Use of the PAS in additional populations will provide data for the future development of interventions designed to enhance the psychological adaptation of individuals in response to a chronic health condition or risk, particularly with regard to the central domains of effective coping, self-esteem, social integration, and spiritual/existential meaning-making. The PAS can also fill a conceptual gap by providing a relatively brief standardized measure for the evaluation of existing programs and services, such as those we have previously described [2]. Future work should also examine the utility of using the PAS in a clinical setting to screen for clients who may need particular assistance at a given point in time and to prioritize domains for intervention.
Figure 1.
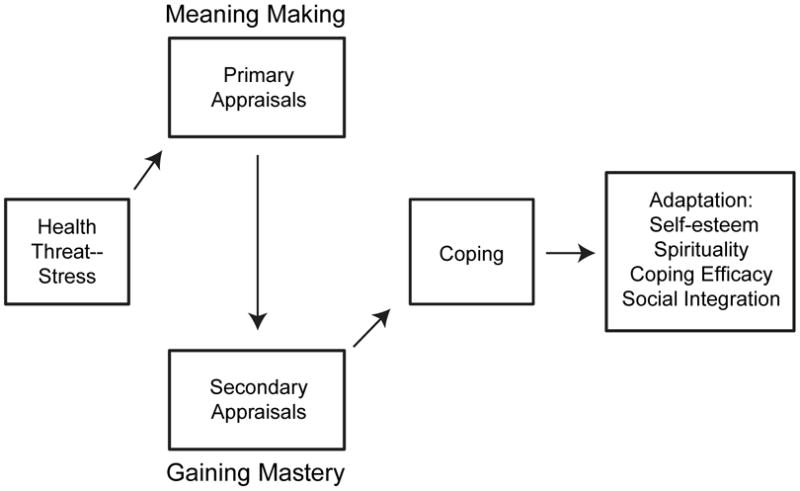
Integrated Theoretical Model of Adaptation
Acknowledgments
This research was funded by the National Human Genome Research Institute Intramural Research Program, National Institutes of Health. We would like to thank Sara Rosenbloom and Sophia Garcia from the PROMIS consortium for their help in assessing psychometric performance of the items.
Footnotes
Spirituality was placed on the left in Figure 3 for convenience; it does not designate a unique distinction.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Resta R, Biesecker BB, Bennett RL, Blum S, Hahn SE, Strecker MN, Williams JL. A new definition of Genetic Counseling: National Society of Genetic Counselors’ Task Force report. J Genet Couns. 2006;15:77–83. doi: 10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- 2.Biesecker BB, Erby L. Adaptation to living with a genetic condition or risk: a mini-review. Clin Genet. 2008;74:401–7. doi: 10.1111/j.1399-0004.2008.01088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lazarus RS, Folkman S. Stress. Appraisal and Coping. New York City: Springer; 1984. [Google Scholar]
- 4.Walker LS, Smith CA, Garber J, Claar RL. Appraisal and coping with daily stressors by pediatric patients with chronic abdominal pain. J Pediatr Psychol. 2007;32:206–16. doi: 10.1093/jpepsy/jsj124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutterford NA, Wood RL. Evaluating a theory of stress and adjustment when predicting long-term psychosocial outcome after brain injury. J Int Neuropsychol Soc. 2006;12:359–67. doi: 10.1017/s1355617706060450. [DOI] [PubMed] [Google Scholar]
- 6.Taylor SE. Adjustment to Threatening Life Events: A Theory of Cognitive Adaptation. Amer Psychol. 1983;38:1161–1173. [Google Scholar]
- 7.Zakowski SG, Hall MH, Klein LC, Baum A. Appraised control, coping, and stress in a community sample: a test of the goodness-of-fit hypothesis. Ann Behav Med. 2001;23:158–65. doi: 10.1207/S15324796ABM2303_3. [DOI] [PubMed] [Google Scholar]
- 8.Kendall E, Terry D. Predicting emotional well-being following traumatic brain injury: a test of mediated and moderated models. Soc Sci Med. 2009;69:947–54. doi: 10.1016/j.socscimed.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Walker JG, Jackson HJ, Littlejohn GO. Models of adjustment to chronic illness: Using the example of rheumatoid arthritis. Clin Psychol Rev. 2004;24:461–488. doi: 10.1016/j.cpr.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Wakefield CE, McLoone JK, Butow P, Lenthen K, Cohn RJ. Parental adjustment to the completion of their child’s cancer treatment. Pediatr Blood Cancer. 2011;56:524–31. doi: 10.1002/pbc.22725. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 12.Turriff A, Levy HP, Biesecker B. Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genet Med. 2011;13:966–972. doi: 10.1097/GIM.0b013e3182227576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: The experience of caregivers of children with Down syndrome. Patient Educ Couns. 2012;87:233–238. doi: 10.1016/j.pec.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Voss K. Master’s thesis. The Johns Hopkins Bloomberg School of Public Health; Baltimore, MD: 2008. Caregiver adaptation to Autism Spectrum Disorders. [Google Scholar]
- 15.Cohen JS. Master’s thesis. The Johns Hopkins Bloomberg School of Public Health; 2009. Adaptation and Quality of Life Among Adults with Neurofibromatosis Type 1. [Google Scholar]
- 16.Lamb AE. Master’s thesis. The Johns Hopkins Bloomberg School of Public Health; Baltimore, MD: 2010. The Role of Family Functioning in Adaptation to Being a Caregiver of an Individual with Rett Syndrome. [Google Scholar]
- 17.Adcock JY. Master’s thesis. The Johns Hopkins Bloomberg School of Public Health; Baltimore, MD: 2008. The Extent and Patterns of Disclosure Within the Huntington Disease Community and the Association with Adaptation to Living at Risk. [Google Scholar]
- 18.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychol Measure. 1977;1:385–401. [Google Scholar]
- 19.Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C, Harney P. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. 1991;60:570–85. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- 20.Ferrans C, Powers M. Psychometric assessment of the Quality of Life Index. Res Nurs Health. 1992;15:29–38. doi: 10.1002/nur.4770150106. [DOI] [PubMed] [Google Scholar]
- 21.Jacob T, Tennenbaum DL. Family Assessment: Rationale, Methods, and Future Directions. New York City: Plenum Press; 1988. [Google Scholar]
- 22.Hair JF, Jr, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis. 7. New Jersey: Pearson Prentice Hall; 2010. [Google Scholar]
- 23.Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: Results from a randomized trial testing a group-based intervention. Psychosomatic Med. 2003;65:1038–46. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy P, Duff J, Evans M, Beedie A. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. British J Clin Psychol. 2003;42:41–52. doi: 10.1348/014466503762842002. [DOI] [PubMed] [Google Scholar]
- 25.Payne K, Nicholls S, McAllister M, Macleod R, Donnai D, Davies LM. Outcome measurement in clinical genetics services: a systematic review of validated measures. Value Health. 2008;11:497–508. doi: 10.1111/j.1524-4733.2007.00259.x. [DOI] [PubMed] [Google Scholar]


