Abstract
Objectives
To develop easily disseminated educational materials that enable early detection of skin cancer, and to examine the effectiveness of the materials to promote skin self-examination (SSE) among kidney transplant recipients (KTRs).
Design
Randomized controlled trial of an educational intervention in comparison with a group that received only the assessment, education, and treatment as part of usual care with a nephrologist.
Setting
Academic ambulatory nephrology practice.
Patients
Seventy-five KTRs returning for routine care to their nephrologists 1 to 1.2 years or 3 to 7 years after transplantation.
Intervention
Educational workbook.
Main Outcome Measures
Skin self-examination performance and new appointments with a dermatologist if a concerning skin lesion was found.
Results
Twenty-two percent of those in the control group checked their skin after the visit compared with 89% of the treatment condition; thus, KTRs receiving the intervention were significantly more likely to have checked their skin (χ2; P<.001). Among the 8 control KTRs who checked their skin, none found areas of concern. Of the 34 intervention KTRs who checked their skin, 12 participants (35%) found areas of concern. All 12 of these individuals made appointments with a dermatologist for follow-up.
Conclusions
The KTRs were receptive to performing SSE and acted on the recommendation made in the workbook to make an appointment with a dermatologist when a concerning lesion was discovered. Printed educational materials can be initiated in the tertiary care center 1 year after transplantation and used across a continuum of time during which KTRs may be transferred from the tertiary care center to community nephrologists.
Trial Registration
clinicaltrials.gov Identifier: NCT01127737
In the united states, an estimated 100 000 living kidney transplant recipients (KTRs) are at risk to develop squamous cell carcinoma (SCC).1 The mean (SD) time to presentation of the first SCC after organ transplantation is 7.8 (4.6) years.2 After 20 years of immunosuppression, cumulative SCC incidences in areas of high UV radiation (UVR), such as Australia, can be as high as 70% in KTRs, whereas in areas with more temperate climates, such as the United Kingdom or the Netherlands, the cumulative incidence after 20 years ranges from 20% to 40%.3–5 Most KTRs with a first SCC develop multiple skin cancers within 5 years, and some develop more than 100 skin cancers within a year.6,7
The quality of life of KTRs is impaired, with disfigurement from surgical removal of SCC, the emotional burden of anxiety and fear about the return or spread of the cancer, and concern about the reaction of others.8 Squamous cell carcinoma can metastasize in 5% to 8% of patients; however, the precise rate of death from SCC is not known.6,9 Early detection of SCC among KTRs may reduce the extent of disfigurement and help to alleviate some of the emotional burden. It is not known whether KTRs will perform skin self-examination (SSE) and, if SSE is performed, how effective it may be.
Easily disseminated patient educational materials that assist with early detection are needed. We developed and evaluated the short-term efficacy of an educational intervention consisting of a mnemonic and a workbook used by KTRs to assist with early detection of SCC. Our hypothesis was that KTRs would be more likely to implement SSE if KTRs were told when SCC might develop and if they received an educational intervention close to the time when SCC might appear, which is 7 to 8 years after transplantation. However, our focus groups and cognitive interviews of KTRs stated that 1 year after transplantation was the ideal time for SSE education.10 Therefore, we performed a randomized controlled educational intervention with KTRs without a history of skin cancer who had undergone the transplant 1 to 1.2 years or 3 to 7 years prior to the intervention. In selecting the intervention period to occur about 1 year after the procedure, we sought to verify or disprove the opinion of the KTRs that 1 year after transplantation was the best time to receive SSE education.10 The report by Bordea et al2 of the mean time to presentation of the first SCC after organ transplantation was used to select the period 3 to 7 years after the transplantation. By defining the beginning of our accrual at 3 years, which is the early period of the first appearance of a SCC, and concluding before most KTRs would be expected to develop a SCC at 7.8 years, we maximized accrual of participants who received similar care at the time of transplantation2.
METHODS
DEVELOPMENT OF MNEMONIC
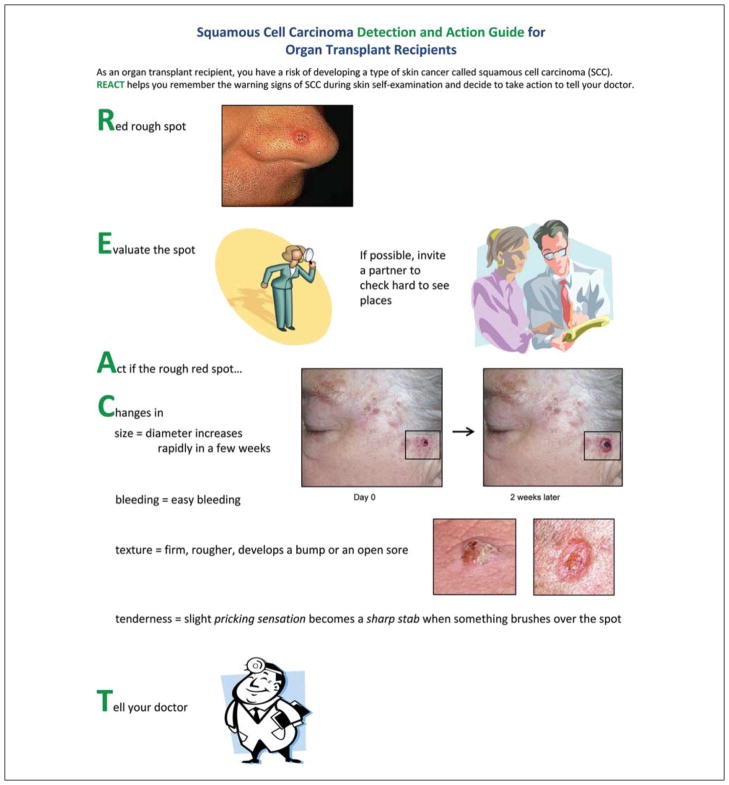
The clinical features of SCC identified in our systematic literature search for review articles or studies in the English literature from 1950 to 2008 were identified independently by 2 reviewers. Similar descriptors were grouped by a dermatologist (J.K.R.), who reduced the number of categories according to the clinical appearance (eg, erythema and inflamed were combined) (Table 1). Clinical features associated with SCC in 8 or more of the reviews or studies were used to create the REACT mnemonic. In this mnemonic, R represents a Red, rough spot to be Evaluated with a partner if possible; and Act if the spot Changes in size by an increase in diameter in a few weeks, ease of bleeding, texture by becoming firm, rougher, or developing a bump or open sore; or tenderness with a slight pricking sensation or a sharp stab when lightly touched by Telling the doctor by making an appointment within 2 weeks (Figure). The REACT mnemonic, which was created by 2 of us (J.K.R. and R.T.), emphasizes the early warning signs of SCC and empowers KTRs to act.
Table 1.
Clinical Features Commonly Associated With Squamous Cell Carcinoma
| Clinical Feature | Review Articles or Studies, No.a |
|---|---|
| Bleeding | 12 |
| Diameter | 20 |
| Elevated, raised | 22 |
| Erythematous, inflamed | 18 |
| Firm | 8 |
| Painful | 2 |
| Rough surface | 14 |
| Scaling | 4 |
| Stings, stabs, pricking | 8 |
| Tender | 9 |
| Ulcer | 10 |
| Other: pigmented, asymptomatic, anatomic location | 4 |
References used to develop the mnemonic are provided in the eReferences (http://www.archdermatol.com).
Figure.
REACT mnemonic provides illustrations of the warning signs of squamous cell carcinoma and advises when to seek health care. See the “Development of Mnemonic” subsection in the “Methods” section.
The REACT mnemonic was depicted in a single color page that was discussed in focus groups and sequentially revised until the final iteration was accepted without suggestions for revision (Figure). The 4 focus groups of 8 KTRs accrued from Northwestern Memorial Hospital’s Organ Transplant Recipient Registry (Chicago, Illinois) each lasted 2 hours, and participants were provided with refreshments and a modest monetary incentive. The study was approved by the institutional review board of Northwestern University. Written informed consent was obtained.
DEVELOPMENT OF WORKBOOK
The 8-page color workbook was created with the 7 sections that provide knowledge and build skills: Knowledge-based sections contained information about antirejection medicine as a risk factor for SCC, how to identify sun spots (actinic keratosis) on the face and forearms, the importance of early detection in affecting the amount of surgery needed to treat SCC and limiting the risk of metastasis, and the REACT mnemonic as a self-care preventive strategy that KTRs can use to help themselves. Skills building was enhanced with a worksheet to evaluate personal sun exposure experiences, exercises to recognize sun spots that demonstrate a personal risk of SCC, and actions to take if an area of concern was noticed. The workbook was continuously refined in cognitive interviews (n = 25) until the last 10 participants did not suggest changes and agreed that the content was clear and easily read. The format of the workbook was derived from an SSE workbook developed by 4 of us (J.K.R., R.T., K.A.M., and J.S.) for patients with melanoma and their partners.11
SAMPLE AND PROCEDURE
The study population consisted of KTRs returning for routine care to their nephrologists 1 to 1.2 years or 3 to 7 years after transplantation. Inclusion criteria were having received a kidney transplant 1 to 1.2 years or 3 to 7 years prior to the visit; being 18 years or older; being able to read English and to clearly see newspaper-size print; being willing to answer a telephone survey 1 month after the visit; having no history of skin cancer; and not being under the care of a dermatologist. In 2009, all KTRs with scheduled appointments were screened for eligibility. Eligible patients were contacted by telephone 2 weeks before the visit and invited to participate with an explanation that it was expected that 1 hour of time would be required on the day of the visit. Patients in each of the 2 groups, those 1 to 1.2 years or those 3 to 7 years after kidney transplantation, were randomized to either receive the educational intervention or to the control group that only completed surveys. The intervention consisted of the patient reading the workbook at the time of the clinic visit. The research assistant administered the self-report survey questionnaire both before and immediately after the patient reviewed the workbook. After completion and collection of the first survey, those receiving the intervention read the brochure and marked questions or concerns on the pages and returned it. Those randomized to the control group received only initial assessment at the time of the physician visit and education as usually provided during the physician visit. Since only the participants receiving the workbook responded to the post-intervention survey, the survey itself became part of the intervention, which may have contributed to differences between groups at 1 month. One month after entry into the study, patients from both the intervention and control groups responded to the final survey questionnaire during a telephone interview lasting about 10 minutes. The participants were offered parking vouchers in appreciation of their participation.
ASSESSMENT
Demographic information obtained included: sex, age, highest level of education, and ethnic/racial group, including non-Hispanic white; Hispanic; black/African American; Asian or Pacific Islander; and Aleut, Eskimo, or Native American.
Personal risk of developing a skin cancer was assessed by Fitzpatrick skin type using the standard ease of sunburning and tanning, and 1 self-report of prior sun exposure. Responses to the question “Approximately how much has your skin been exposed to the sun?” ranged from “not at all,” to a “small amount,” “moderate amount,” or a “huge amount.”
Knowledge
Knowledge measures were true/false responses to 4 items: (1) People with an organ transplant are at risk to develop a type of skin cancer, SCC; (2) change in tenderness of a red rough spot on the skin is a warning that it may be becoming a squamous cell carcinoma; (3) rapid growth with doubling in size in about 2 weeks indicates that the spot is an SCC; and (4) if a red rough spot develops a firm tender bump, it is OK to watch it for another month or 2 before calling the physician.
Cancer Concerns
Participants with cancer concerns were asked to report how concerned they were about developing SCC. Response options ranged from not at all concerned (0) to very concerned (3).
Attitude Toward SSE
Two attitude items were used: “How important is it to you to regularly and carefully examine your skin?” and “How important is it to you to have a partner help you check places that you cannot see for yourself, such as your back and ears?” Response options ranged from not at all important (0) to extremely important (4).
Self-efficacy for Recognizing SCC
Participants were asked to indicate how confident they felt that they could recognize a SCC on a 5-point Likert scale ranging from not at all confident (0) to extremely confident (4).
Likelihood of Asking for Partner Assistance
Participants were asked to indicate how likely they were to ask a partner to help look at areas that may be difficult to see on a 5-point Likert scale ranging from very unlikely (0) to very likely (4).
SSE Behavioral Tendencies
Skin self-examination behavior was assessed in the preintervention baseline and 1-month follow-up surveys with yes/no responses to the following questions:
In the past month have you checked the skin on your face?
In the past month have you checked the skin on your body?
If yes, did you find a concerning spot?
Did you call to make an appointment with a physician for a skin check?
For participants randomized to receive the intervention, their intention to check the skin was assessed with 2 items in the immediate postintervention survey. Participants were asked how likely they were to start examining their body or face in the next month. Responses were measured on a 5-point Likert-type scale ranging from very unlikely (0) to very likely (4).4
At the 1-month follow-up survey, both intervention and control participants answered questions about their SSE behavioral tendencies. Participants were asked if they had examined their skin since the previous office visit. If participants responded that they had checked, they were asked if they found a concerning spot. Those who found a concerning spot were asked whether they had called to make an appointment with a physician for a skin examination.
MEASURES
The measures were derived from survey items previously used in our research with partner-assisted SSE with melanoma patients.12 The questions were adapted for use with KTRs, and each item had test-retest reliability performed with KTRs (α knowledge, 0.92; cancer concern, 0.85; attitude toward SSE, 0.87; self-efficacy, 0.81; likely to ask for partner assistance, 0.79; SSE behavior, 0.90). A composite knowledge item was created by summing the 4 knowledge items. Each of the 4 knowledge question answered correctly received a score of 1; thus, the total possible correct was 4.0 for the composite measure.
STATISTICAL ANALYSIS
Postintervention Changes in Cognitive Variables
Intervention participants’ knowledge, cancer concern, attitudes toward SSE, and self-efficacy were measured both prior to receiving the intervention and immediately following the intervention. To assess intervention effects, paired-samples t tests were used to detect participants’ changes in these variables from pre-intervention to postintervention. This analysis compares means on the same variables over time to test for a significant change.
Postintervention Differences in Intervention and Control Participants’ SSE Behaviors
To test for efficacy of the intervention in increasing SSE behavior, participants from the intervention condition were compared with those in the control condition at a 1-month follow-up. Intervention and control participants were compared on performance of SSE and whether those participants who performed SSE found lesions that they considered concerning.
RESULTS
DEMOGRAPHIC CHARACTERISTICS
Among the 80 eligible KTRs, 75 participated. Those declining to participate stated that they did not have time on the day of the visit. Among the 75 participants, 58% were male, and 42% were female. Fifty-nine percent were non-Hispanic white; 20%, black; 19%, Hispanic; and 2%, Asian or Pacific Islander. The median age was 60 years (range, 25–79 years). The median level of education was some college.
PARTICIPANTS FROM THE 2 PERIODS AFTER TRANSPLANTATION
Participants in the 2 periods (1–1.2 years and 3–7 years after transplantation) were compared on the demographic measures of age, sex, education, skin type, and race/ethnicity, and there were no significant differences between the 2 groups for these variables. (P>.05 for all comparisons): The 2 groups were compared at baseline on the cognitive measures of knowledge, concern about SCC, and self-efficacy; the attitudinal measures of beliefs about the importance of SSE and importance of having a partner assist with SSE; and the behavioral measures of examining their skin in the past month. There were no significant differences between the 2 groups for these variables (P>.05 for all comparisons).
PARTICIPANTS IN THE INTERVENTION AND CONTROL GROUPS
Intervention and control group participants were compared on several demographic measures. There were non-significant differences between the conditions on the following variables (P >.05 for all comparisons): sex, education, skin type, or race/ethnicity. When comparing those in the control group (n=37) with those receiving the intervention (n=38), the intervention group was older, with a median age of 64 years compared with the controls, who had a median age of 57 years ( ; N=75; P <.01).
Intervention and control participants were also compared on the cognitive measures at the preintervention baseline. Nonsignificant differences were found in baseline knowledge, concern about SCC, and self-efficacy (P>.05 for all comparisons) (Table 1). However, significant differences were observed for the attitudinal measures. Participants in the control condition reported significantly more favorable mean levels of beliefs about the importance of SSE (2.03) compared with the intervention participants (1.34) (t73=3.08; P <.001) and mean levels of importance of having a partner assist with SSE (1.38) compared with intervention participants (0.70) (t72=2.65; P<.01). In addition, 6 controls reported examining the skin on their body in the past month compared with no intervention participants ( ; N=75; P <.01). None of the controls reported finding an area of concern.
POSTINTERVENTION CHANGES IN COGNITIVE VARIABLES FOR PARTICIPANTS IN THE INTERVENTION AND CONTROL GROUPS
The change in knowledge from baseline mean (3.11±1.14) to postintervention mean (3.76±.49) was statistically significant (t37= −3.28; P <.01) (Table 2). Statistically significant changes were also observed for concern about developing an SCC (baseline mean, 0.94 ± 0.92; post-intervention mean, 1.92±1.03) (t35=−5.84; P <.01), importance of SSE (baseline mean, 1.34 ± 0.90); postintervention mean, 3.08 ± 0.91) (t37 = −10.95; P < .01), and importance of having a partner help (baseline mean, 0.70 ± 1.08; postintervention mean, 2.97 ± 1.07) (t36=−11.14; P <.01). Confidence in recognizing an SCC significantly improved (baseline mean, 0.16±0.44; post-intervention mean, 2.18 ± 1.25) (t37= −9.15; P <.001).
Table 2.
Comparison of Knowledge, Cancer Concern, Attitude Toward Skin Self-examination, Self-efficacy, and Skin Self-examination (SSE) Prior to Educational Intervention and Immediately After Intervention
| Measure | Baseline, Prior to Intervention
|
Immediately After Intervention
|
|||
|---|---|---|---|---|---|
| Control (n=37) | Intervention (n=38) | P Value, Baseline Mean Difference | Intervention (n=38) | P Value, Baseline to Immediately After Intervention, Mean Difference | |
| Rating, mean (SD) | |||||
| Knowledge (range, 0–4) | 2.83 (1.14) | 3.10 (1.13) | NS | 3.76 (0.49) | .01 |
| Cancer concern (range, 0–3) | 1.00 (0.88) | 0.94 (0.92) | NS | 1.92 (1.03) | .001 |
| Attitude, importance of SSE (range, 0–4) | 2.03 (1.01) | 1.34 (0.91) | .001 | 3.08 (0.91) | .001 |
| Attitude, importance of partner help (range, 0–4) | 1.38 (1.11) | 0.70 (1.08) | .001 | 2.97 (1.07) | .001 |
| Self-efficacy (range, 0–4) | 0.38 (0.68) | 0.16 (0.44) | NS | 2.18 (1.25) | .001 |
| Patients, % | |||||
| Checked face in past month? (% yes) | 32 | 21 | NS | NA | NA |
| Checked body in past month? (% yes) | 16 | 0 | .05 | NA | NA |
| Intend to check face? (% likely or very likely) | NA | NA | NA | 93 | NA |
| Intend to check body? (% likely or very likely) | NA | NA | NA | 94 | NA |
Abbreviations: NA, not applicable; NS, not significant.
Prior to the intervention, KTRs in the intervention condition were not likely to examine the skin of the face (79% did not) or body (100% did not). After the intervention, 73% reported being very likely to start to examine the face in the next month, and 74% were very likely to start examining the body. Approximately 20% reported being likely to examine both their face and body (Table 3).
Table 3.
Comparison of Control and Intervention Participants on Skin Self-examination Performance at Follow-up 1 Month After Intervention
| Outcome | No (%)
|
P Value, Test for Mean Difference | |
|---|---|---|---|
| Control (n=37) | Intervention (n=38) | ||
| Checked skin after visit | 8 of 37 (22) | 34 of 38 (89) | .001 |
| If checked, found an area of concern | 0 of 8 (0) | 12 of 34 (35) | NA |
| If concerned, called dermatologist | 0 of 0 (NA) | 12 of 12 (100) | NA |
Abbreviation: NA, not applicable.
POSTINTERVENTION DIFFERENCES IN INTERVENTION AND CONTROL PARTICIPANTS’ SSE BEHAVIORS
One month after the intervention, all KTRs in both the control and intervention groups remembered completing the survey during the office visit. Twenty-two percent of those in the control condition checked their skin after the visit compared with 89% of the treatment condition (Table 2). Thus, KTRs receiving the intervention were significantly more likely to have checked their skin ( ; N = 75; P <.001).
Among the 8 control KTRs who checked their skin, none found areas of concern. Of the 34 intervention KTRs who checked their skin, 12 participants (35%) found areas of concern. All 12 of these individuals made appointments with a dermatologist.
BEHAVIOR OF KTRS 1 TO 1.2 YEARS AND 3 TO 7 YEARS AFTER TRANSPLANTATION
When comparing the 2 subcategories of number of years after transplant (1–2 years or 3–7 years), there was a non-significant difference in skin checking ( ; N = 38; P= .91), and calling to make an appointment with a dermatologist if an area of concern was noticed ( ; N = 38; P= .95). The KTRs who had their transplant 3 to 7 years previously had a significant difference in finding an area of concern in comparison with KTRs 1 to 2 years after transplant ( ; N = 38; P <.01).
COMMENT
This randomized controlled trial of an SSE and SCC detection educational intervention with KTRs demonstrated changes in knowledge, attitude, self-efficacy, and performance of SSE. The educational intervention effectively increased awareness of the KTRs’ risk of developing SCC and provided sufficient training to enhance self-efficacy in their ability to detect an area of concern. The KTRs were receptive to performing skin checks and acted on the recommendation to make an appointment with a dermatologist when a concerning lesion was discovered.
In this study, KTRs receiving education about 1 year after transplantation performed SSE as much as those receiving education 3 to 7 years after transplantation. The participants in the latter group, 3 to 7 years after transplantation, were more likely to find an area of concern. While the short duration of this study made it impossible to examine the potential reinforcement of SSE by finding a suspicious lesion, the belief of the KTRs who participated in our focus groups and cognitive interviews that 1 year after transplantation was an appropriate time for education was supported.10 The SSE education provided a framework for KTRs to understand the nephrologists’ recommendation to see a dermatologist, which was baffling to KTRs participating in our focus groups and cognitive interviews. The KTRs reported thinking that there was nothing wrong with their skin and discounted the need to seek dermatologic care.
The frequency of patient visits in the first year after transplantation gave nephrologists and nurse practitioners the best opportunity to provide counseling. The KTRs, who are faced with many stressors that can affect their adherence to the medical regimen and physician instructions in the first 6 months after transplantation, may not find early detection of skin cancer relevant.13 By failing to provide education that facilitates KTRs’ assessment of their personal risk of developing skin cancer and directing patients to see a dermatologist without providing a relevant context, clinicians created a “disconnect” for KTRs. Our program informed KTRs that SCC often appears 3 to 7 years after transplantation, provided quizzes for the KTRs to assess their personal risk of developing SCC, and linked a motivational message about the importance of SSE to the information about the warning signs of SSE.
After the first year, most transplant centers refer KTRs to nephrologists in the community for routine long-term care. Because uniform guidelines as to when this transfer of care to the community physicians occurs are lacking, uniform delivery of an educational intervention can be achieved in the tertiary care center at the end of the first year. As care is transferred, patient education directed toward improving the self-management of skin cancer and the importance of early detection may be overlooked; thus, there is an advantage in KTRs having the workbook, which may be a reference for KTRs and their partners.
Limitations of this proof of concept study include a small sample at a single center for a limited period of follow-up; thus, the results may not be generalizable. In addition, the dermatologists’ assessment of the participants’ concerning lesions was not performed, and the absence of external verification of participants’ attendance at dermatologists’ offices following the intervention limited external validity. An additional concern is the demographic difference between the control and intervention groups. While the control group (median age, 57 years) was younger than the intervention group (median age, 62 years), both groups comprised adults with similar social influences. The control KTRs initially placed greater importance on SSE and having a partner assist with SSE and reported doing more body checks initially than those randomized to the educational intervention. We examined the time of accrual of the control KTRs, who reported doing body checks at baseline, to determine if there was diffusion of the SSE educational message to the nephrologists and nurse practitioners which may have changed their customary care over the course of this research. The 6 control participants were accrued across the duration of the study, which thus failed to support the concern of increased SSE awareness by clinicians in the early phase of the study or diffusion of content in the later phases of the study. Since participants with more favorable attitudes about the importance of SSE and performance of SSE happened to have been randomized to the control group, any introduced bias would weaken the intervention effects because those in the control condition hold more theoretically favorable cognitive and behavioral variables related to SSE prior to the intervention.
The educational intervention needs to be studied in a larger, more ethnically diverse sample for a longer duration with additional measurable end points such as the number of visits made with a dermatologist, the dermatologic evaluation of the concerning lesions, and the number of biopsies performed. Further research may demonstrate the validity of SSE by KTRs and their partners and evaluate whether continuation of the behavior is dependent on detection of concerning lesions.
Systematic educational efforts are needed to bridge the gap between tertiary care provided in transplant centers and delivery of care in the community for KTRs. Printed educational materials can be initiated at the end of the first year and can be a reference for KTRs across a continuum of time during which KTRs may be transferred from the tertiary care center to the community nephrologists.
Footnotes
Financial Disclosure: None reported.
Disclaimer: Dr Robinson is the Editor of the Archives of Dermatology. She was not involved in the editorial evaluation or editorial decision to accept this work for publication.
Online-Only Material: The eReferences are available at http://www.archdermatol.com.
Additional Information: The trademark of REACT is registered to Northwestern University and June K. Robinson, MD.
Author Contributions: All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Robinson, Kim, and Riyat. Acquisition of data: Robinson, Kim, and Riyat. Analysis and interpretation of data: Robinson, Turrisi, Stapleton, Mallett, Boone, and Gordon. Drafting of the manuscript: Robinson. Critical revision of the manuscript for important intellectual content: Turrisi, Stapleton, Mallett, Boone, Kim, Riyat, and Gordon. Statistical analysis: Turrisi and Stapleton. Obtained funding: Robinson. Administrative, technical, and material support: Robinson, Kim, and Riyat. Study supervision: Robinson and Mallett. Coordination and acquisition of data and creation of patient education materials: Riyat.
Additional Contributions: The support of the members of the Solid Organ Transplantation Team of Northwestern Memorial Hospital is appreciated, especially the following physician members: Michael Abecassis, MD, MBA; John Friedewald, MD; Josh Levitsky, MD; Xunrong Luo, MD, PhD; and Daniel R. Ganger, MD.
References
- 1.Health Resources and Services Administration; [Accessed July 27, 2009]. Welcome to the 2009 OPTN/SRTR annual report: transplant data 1999–2008: the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients. Web site http://www.ustransplant.org/annual_reports/current/ [Google Scholar]
- 2.Bordea C, Wojnarowska F, Millard PR, Doll H, Welsh K, Morris PJ. Skin cancers in renal-transplant recipients occur more frequently than previously recognized in a temperate climate. Transplantation. 2004;77(4):574–579. doi: 10.1097/01.tp.0000108491.62935.df. [DOI] [PubMed] [Google Scholar]
- 3.Tessari G, Naldi L, Boschiero L, et al. Incidence and clinical predictors of a subsequent nonmelanoma skin cancer in solid organ transplant recipients with a first nonmelanoma skin cancer: a multicenter cohort study. Arch Dermatol. 2010;146(3):294–299. doi: 10.1001/archdermatol.2009.377. [DOI] [PubMed] [Google Scholar]
- 4.Hartevelt MM, Bavinck JN, Kootte AMM, Vermeer BJ, Vandenbroucke JP. Incidence of skin cancer after renal transplantation in the Netherlands. Transplantation. 1990;49(3):506–509. doi: 10.1097/00007890-199003000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Bouwes Bavinck JN, Hardie DR, Green A, et al. The risk of skin cancer in renal transplant recipients in Queensland, Australia: a follow-up study. Transplantation. 1996;61(5):715–721. doi: 10.1097/00007890-199603150-00008. [DOI] [PubMed] [Google Scholar]
- 6.Ulrich C, Kanitakis J, Stockfleth E, Euvrard S. Skin cancer in organ transplant recipients: where do we stand today? Am J Transplant. 2008;8(11):2192–2198. doi: 10.1111/j.1600-6143.2008.02386.x. [DOI] [PubMed] [Google Scholar]
- 7.Berg D, Otley CC. Skin cancer in organ transplant recipients: epidemiology, pathogenesis, and management. J Am Acad Dermatol. 2002;47(1):1–17. doi: 10.1067/mjd.2002.125579. [DOI] [PubMed] [Google Scholar]
- 8.Burdon-Jones D, Thomas P, Baker R. Quality of life issues in nonmetastatic skin cancer. Br J Dermatol. 2010;162(1):147–151. doi: 10.1111/j.1365-2133.2009.09469.x. [DOI] [PubMed] [Google Scholar]
- 9.Stockfleth E, Ulrich C, Meyer T, Christophers E. Epithelial malignancies in organ transplant patients: clinical presentation and new methods of treatment. Recent Results Cancer Res. 2002;160:251–258. doi: 10.1007/978-3-642-59410-6_30. [DOI] [PubMed] [Google Scholar]
- 10.Kim NN, Boone SL, Ortiz S, et al. Squamous cell carcinoma in solid organ transplant recipients: influences on perception of risk and optimal time to provide education. Arch Dermatol. 2009;145(10):1196–1197. doi: 10.1001/archdermatol.2009.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson JK, Turrisi R, Mallett K, Stapleton J, Pion M. Comparing the efficacy of an in-person intervention with a skin self-examination workbook. Arch Dermatol. 2010;146(1):91–94. doi: 10.1001/archdermatol.2009.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson JK, Turrisi R, Stapleton J. Efficacy of a partner assistance intervention designed to increase skin self-examination performance. Arch Dermatol. 2007;143(1):37–41. doi: 10.1001/archderm.143.1.37. [DOI] [PubMed] [Google Scholar]
- 13.Muehrer RJ, Becker BN. Life after transplantation: new transitions in quality of life and psychological distress. Semin Dial. 2005;18(2):124–131. doi: 10.1111/j.1525-139X.2005.18214.x. [DOI] [PubMed] [Google Scholar]