Abstract
Background
There is controversy regarding the association between age and being female and survival to hospital discharge after out-of-hospital cardiac arrest (OHCA). We hypothesized that younger females (aged 12–49 years) would be independently associated with increased survival after OHCA when compared to other age and sex groups.
Methods
We conducted a secondary analysis of prospectively collected data from 29 United States cities that participate in the Cardiac Arrest Registry to Enhance Survival (CARES). Patients were included if they were ≥12 years of age and had a documented resuscitation attempt from October 1, 2005 through December 31, 2009. Hierarchical multivariable logistic regression analyses were used to estimate the associations between age and sex groups and survival to hospital discharge.
Results
Females were less likely to have a cardiac arrest in public, was witnessed, or was treatable with defibrillation. Females in the 12–49 year old age group had a similar proportion of survival to hospital discharge when compared to age-matched males (females 11.6% vs. males 11.2%), while males ≥50 years old were more likely to survive when compared to age matched females (females 6.9% vs. males 9.6%). Age stratified regression models demonstrated that 12–49 year old females had the largest association with survival to hospital discharge (OR 1.55, 95% CI 1.20–2.00), while females in the ≥50 year old age group had a smaller increased odds of survival to hospital discharge (OR 1.18, 95% CI 1.03–1.35), which only lasted until the age of 55 years (OR 1.12, 95% CI 0.97–1.29).
Conclusions
Younger aged females were associated with increased odds of survival despite being found with poorer prognostic arrest characteristics.
Keywords: Cardiac arrest, Estrogen, Survival, Sex
1. Introduction
Out-of-hospital cardiac arrest (OHCA) accounts for approximately 300,000 deaths annually in the United States.1 There are known sex disparities in OHCA characteristics, specifically females are more likely to arrest at older ages, arrest at home, have an unwitnessed arrest, and be found in non-shockable rhythms (i.e., pulseless electrical activity or asystole).2–5 Although each of these characteristics is associated with poorer outcomes, currently there is no consensus on whether females with cardiac arrest are less likely to survive to hospital discharge.
Three recent studies, two Japanese studies of OHCA patients6,7 and another United States study of in-hospital cardiac arrest (IHCA) patients8 suggest there may also be an interaction between age and sex on survival from cardiac arrest. These studies have found that females of childbearing age are more likely to survive to hospital discharge when compared to other age and sex groups. It is postulated that this may be due to a protective effect provided by sex hormones in women of childbearing age, as this survival benefit is not seen among females who are >50 years of age or age-matched male counterparts. These findings are further supported by basic science research demonstrating that female sex hormones may have a role in decreasing the reperfusion injury thought to mediate poor outcomes in patients who experience cardiac arrest.7–14
Although the two clinical studies on OHCA from Japan and the IHCA study from the United States report associations between sex and age and survival after cardiac arrest, no studies have been conducted on a racially heterogeneous population from different communities. As such, we utilized the Cardiac Arrest Registry to Enhance Survival (CARES) to further determine if females from a heterogeneous patient population within the United States had increased odds of survival after OHCA. We hypothesized that within this population, females of child-bearing age would have increased odds of surviving OHCA.
2. Methods
2.1. Study design, setting, and population
Data were obtained from the CARES dataset, which is funded by the Centers for Disease Control and Prevention and supported by Emory University.15 The communities that contribute to CARES include a catchment area of approximately 22 million people from 29 cities across the United States (Appendix Table 1). CARES is an EMS-based registry for OHCA, composed of a limited standard set of data elements from three sources: 911 call centers, EMS providers, and receiving hospitals. Data from submitted reports are linked and reviewed by an independent data analyst from Emory University. Detailed information on the design and development of this registry as well as the data elements included in the registry is published elsewhere.15
This was a secondary data analysis of prospectively collected data submitted to CARES from October 1, 2005 through December 31, 2009. All 911-activated cardiac arrest patients for whom resuscitation was attempted and the etiology was presumed to be cardiac were included in the study sample. Exclusion criteria included: not being of presumed cardiac etiology, age <12 years, missing data for sex, or if survival to hospital discharge could not be determined.
Because the CARES registry contains only de-identified data, our study was considered exempt by the Colorado Multiple Institutional Review Board.
2.2. Data collection and processing
All data were entered into a web-based platform (Sansio Corporation, Minneapolis, MN) and an Excel file (Microsoft Corporation, Redmond, WA) was generated. All data analyses were conducted using Stata 11 (Stata Corporation, College Station, TX). Patientlevel characteristics collected in the registry included: age, sex, race/ethnicity (as coded by the EMS provider), location of the arrest (public vs. private residence), whether the arrest was witnessed (by someone other than the first responder/EMS provider), whether CPR was initiated by the bystander, use of an automated external defibrillator, initial cardiac rhythm, return of spontaneous circulation (ROSC), and survival to hospital admission and discharge. Bystander CPR was defined as any time CPR was performed by a person who was not part of the medical or EMS teams.
Age cutoffs were initially defined as the average age of menarche in the United States (12 years)16 and the average age of menopause in the United States (49 years).17 Two principal age groups were created consisting of ages from 12 to 49 years and patients aged greater than 49 years.
2.3. Statistical analysis
In order to confirm that our age categories were associated with survival, we used bivariate fractional polynomial regression to evaluate the non-linear relationship between patient age and survival to hospital discharge among females. The best fit resulted in a two-order transformation (b0 + b1(age)2 + b2(age)3). We then plotted the probability of survival to hospital discharge for females using these transformations in a separate logistic regression model (Appendix figure 1). This demonstrated an inflection point at approximately 50 years of age, confirming our initial age categorization.
Baseline characteristics between age and sex groups were compared using the chi-square test for categorical variables. To estimate associations between individual-and site-specific characteristics, including specifically the relationships between age, sex, and survival, we used hierarchical logistic regression analyses. This statistical approach allowed us to account for 20,018 individual cardiac arrest patients nested within 29 distinct cities. To determine the extent to which city-specific factors have effects independent of individual characteristics, we used a random intercept model to partition the variance between catchment areas and the individuallevel characteristics. Individual level effects were then added as fixed effects to the model to examine their independent contributions. Individual and site-specific characteristics included in the model were: age, sex, race/ethnicity, witnessed by bystander, witnessed by EMS, location of arrest, bystander CPR, use of a public AED, and initial rhythm. In order to test whether there was effect modification between age and sex we included an interaction term between age and sex.
To minimize bias and preserve study power, we used multiple imputation to handle missing values. We and others have previously demonstrated the validity of multiple imputation for imputing missing out-of-hospital values under a variety of conditions.18–20 Individual-level race/ethnicity was coded as unknown in approximately 25% of our sample, whereas arrest witnessed by a bystander, initial presenting rhythm, and location of the arrest had missing values in less than 3% of the dataset. The multiple imputation model included the following variables: age, sex, race/ethnicity, witnessed arrest, initial rhythm, AED use, arrest location, regional site, prehospital disposition, and survival to hospital discharge. Ten imputed datasets were created using imputation by flexible chain equations based on bootstrapped samples from the complete dataset.
2.4. Sensitivity analysis
We performed a sensitivity analysis (Appendix Table 2) to examine the independent association between sex and survival to hospital discharge across different age ranges. Age ranges of 5–49 years, 12–65 years, >55 years, and >65 years were used in our fully adjusted model and imputed datasets. An additional analysis using only complete cases was performed on the 12–49 year old age group.
3. Results
3.1. Population
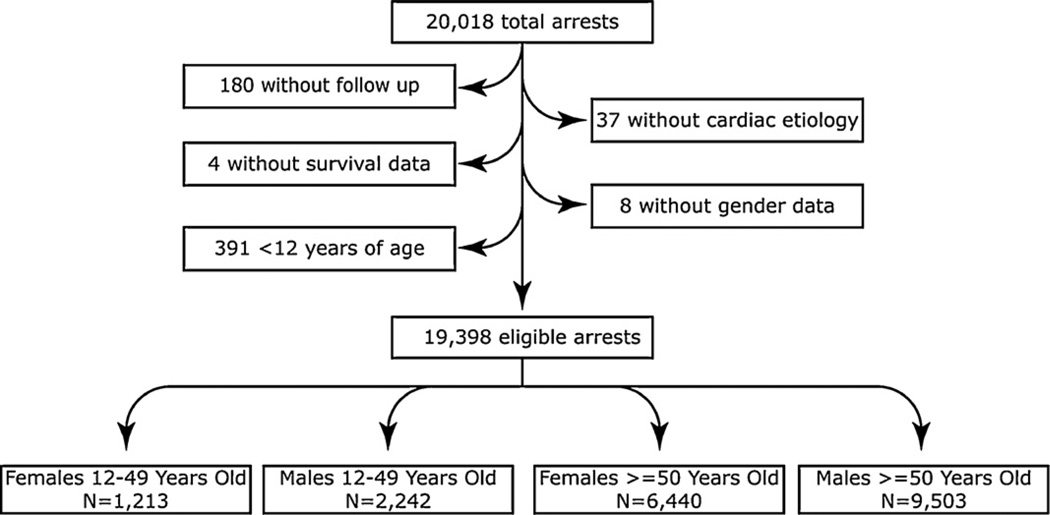
Initially, 20,018 patients were eligible for inclusion. Patients were excluded for not having a presumed cardiac etiology (n = 37), age <12 years (n = 391), missing sex data (n = 8), or missing survival to hospital discharge data (n = 184). A total of 19,398 patients were therefore included in the study sample (Fig. 1).
Fig. 1.
Final sample.
3.2. Stratified by sex
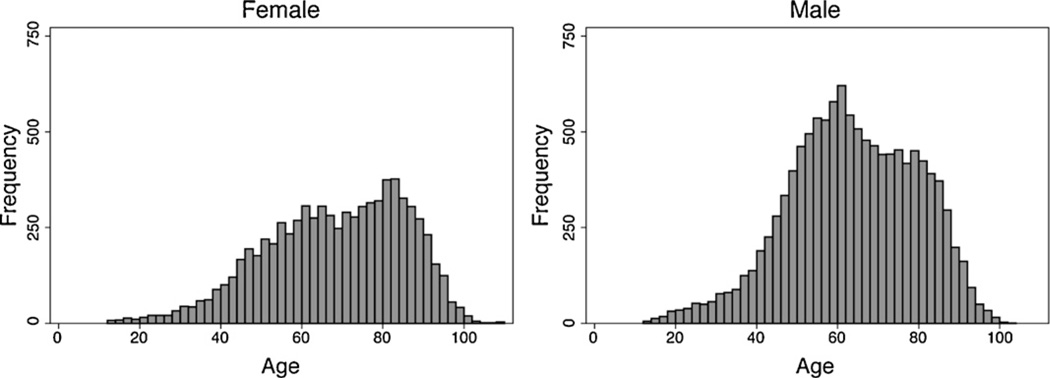
Table 1 displays demographic, clinical, and EMS characteristics of the patients stratified by sex. Of 19,398 patients, 7634 (39.5%) were female with a median age of 69 (interquartile range [IQR]: 56–82) years, and 11,707 (60.5%) were male with a median age of 63 (IQR: 52–75) years (Fig. 2). Overall, females were less likely to have an arrest witnessed by a bystander (females 44.8% vs. males 49.9%, p < 0.01), less likely to have an arrest occur in a public location (females 7.2% vs. 16.5%, p < 0.01), less likely to present with a shockable rhythm (females 16.5% vs. males 28.5%, p < 0.01) and less likely to have an automated external defibrillator (AED) used (females 26.2% vs. males 29.7%, p < 0.01). Bystander CPR was performed in similar proportions for both sexes (females 33.3% vs. males 33.7%). African-American females had the highest total percentage of cardiac arrest events when compared to African-American males (females 32.4% vs. males 25.1%). Overall females were more likely to have ROSC (females 34.9% vs. males 32.3%); however, they were less likely to survive to hospital discharge (females 7.7% vs. males 9.9%).
Table 1.
Characteristics of patients with out-of-hospital cardiac arrest stratified by gender (n = 19,398).
| Characteristics | Female (n = 7653) n (%) |
Male (n = 11,745) n (%) |
|---|---|---|
| Median age (IQR) | 69 (56–82) | 63 (52–75) |
| Race/ethnicitya | ||
| Black | 2483 (32.4) | 2950 (25.1) |
| Hispanic | 349 (4.6) | 688 (5.9) |
| White | 2812 (36.7) | 4807 (40.9) |
| Other | 186 (2.4) | 302 (2.6) |
| Witnessed by bystanderb | 3429 (44.8) | 5861 (49.9) |
| Witnessed by EMSc | 869 (11.4) | 1217 (10.4) |
| Arrest in public locationd | 549 (7.2) | 1934 (16.5) |
| Bystander CPR | 2545 (33.3) | 3961 (33.7) |
| Public AED usede | 2003 (26.2) | 3489 (29.7) |
| Initial rhythmf | ||
| Asystole | 3772 (49.3) | 4953 (42.2) |
| Pulseless electrical activity | 1644 (21.5) | 2062 (17.6) |
| VT/VF or unknown but shockable | 1263 (16.5) | 3344 (28.5) |
| Unknown but not shockable | 967 (12.6) | 1379 (11.7) |
| Return of spontaneous circulation | 2673 (34.9) | 3789 (32.3) |
| Survived to hospital discharge | 588 (7.7) | 1159 (9.9) |
Abbreviations: EMS = emergency medical services; CPR = cardiopulmonary resuscitation; AED = automated external defibrillator; VT = ventricular tachycardia; VF = ventricular fibrillation.
Unknown/missing: females 1823 (23.8%), males 2998 (25.5%).
Unknown/missing: females 2 (0%), males 2 (0%).
Unknown/missing: females 1 (0%), males 1 (0%).
Unknown/missing: females 151 (2.0%), males 350 (3.0%).
Unknown/missing: females 3 (0%), males 2 (0%).
Unknown/missing: females 7 (0.1%), males 7 (0.1%).
Fig. 2.
Distribution of out-of-hospital cardiac arrests by gender and age.
3.3. Stratified by sex and age
Table 2 displays patient demographic, event, and resuscitation characteristics stratified into four groups based on age and sex. For all male and female patients aged >50 years, white patients had the greatest percentage of cardiac arrest (Table 2). In the female 12–49 year old age group, African-Americans had the greatest percentage of arrests (37.4%, 95% CI: 34.7–40.1%). Similar to the sex stratified results, females in both age groups were less likely to have a witnessed arrest, arrest in a public location, have an AED used, and to have had a shockable presenting rhythm. Females in the 12–49 year old age group had a greater percentage of pulseless electrical activity (17.1%, 95% CI: 15.0–19.3) than males of the same age group (13.0%, 95% CI: 11.6–14.4). Additionally, females in the ≥50 year old age group presented more often with asystole (49.6%, 95% CI: 48.4–50.8) than males of the same age group (41.4%, 95% CI: 40.4–42.4). Females and males from both age groups had similar proportions of bystander CPR.
Table 2.
Gender and age stratified characteristics of patients with out-of-hospital cardiac arrest.
| Characteristic | Females 12–49 (n = 1213) | Males 12–49 (n = 2242) | Females ≥50 (n = 6440) | Males ≥50 (n = 9503) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| Race/ethnicity* | ||||||||||||
| Black | 454 | 37.4 | 34.7–40.1 | 658 | 29.3 | 27.5–31.2 | 2029 | 31.5 | 30.4–32.6 | 2292 | 24.1 | 23.3–25.0 |
| Hispanic | 76 | 6.3 | 4.9–7.6 | 197 | 8.8 | 7.6–10.0 | 273 | 4.2 | 3.7–4.7 | 491 | 5.2 | 4.7–5.6 |
| White | 368 | 30.3 | 27.7–32.9 | 759 | 33.9 | 31.9–35.9 | 2444 | 38.0 | 36.8–39.1 | 4048 | 42.6 | 41.6–43.6 |
| Other | 21 | 1.7 | 1.0–2.5 | 50 | 2.2 | 1.6–2.8 | 165 | 2.6 | 2.2–2.9 | 252 | 2.7 | 2.3–3.0 |
| Unknown | 294 | 24.2 | 578 | 25.8 | 1529 | 23.7 | 2420 | 25.5 | ||||
| Witnessed by bystander* | 535 | 44.1 | 41.3–46.9 | 1121 | 50.0 | 47.9–52.1 | 2894 | 44.9 | 43.7–46.2 | 4740 | 49.9 | 48.9–50.9 |
| Unknown | 1 | 0.1 | 1 | 0.1 | 1 | 0.02 | 1 | 0.01 | ||||
| Witnessed by EMS* | 116 | 9.6 | 7.9–11.2 | 218 | 9.70 | 8.5–11.0 | 753 | 11.7 | 10.9–12.5 | 999 | 10.5 | 9.9–11.1 |
| Unknown | 0 | 0 | 1 | 0.1 | 0 | 0 | 0 | 0 | ||||
| Arrest in public location* | 133 | 11.0 | 9.2–12.7 | 520 | 23.2 | 21.4–24.9 | 416 | 6.5 | 5.9–7.1 | 1414 | 14.9 | 14.2–15.6 |
| Unknown | 36 | 3.0 | 2.0–3.9 | 85 | 3.8 | 3.0–4.5 | 115 | 1.8 | 1.5–2.1 | 265 | 2.8 | 2.5–3.1 |
| Bystander CPR* | 365 | 30.1 | 27.5–32.7 | 708 | 31.6 | 29.7–33.5 | 2180 | 33.9 | 32.7–35.0 | 3253 | 34.2 | 33.3–35.2 |
| Public AED used* | 314 | 25.9 | 23.4–28.4 | 663 | 29.6 | 27.7–31.5 | 1689 | 26.2 | 25.2–27.3 | 2826 | 29.7 | 28.8–30.6 |
| Unknown | 0 | 0 | 0 | 0 | 3 | 0.05 | 2 | 0.02 | ||||
| Initial rhythm* | ||||||||||||
| VF/VT, unknown shockable | 288 | 23.7 | 21.3–26.1 | 696 | 31.0 | 29.1–33.0 | 975 | 15.1 | 14.3–16.0 | 2648 | 27.9 | 27.0–28.8 |
| Pulseless electrical activity | 208 | 17.1 | 15.0–19.3 | 292 | 13.0 | 11.6–14.4 | 1436 | 22.3 | 21.3–23.3 | 1770 | 18.6 | 17.8–19.4 |
| Asystole | 576 | 47.5 | 44.7–50.3 | 1018 | 45.4 | 43.3–47.5 | 3196 | 49.6 | 48.4–50.8 | 3935 | 41.4 | 40.4–42.4 |
| Unknown, unshockable | 141 | 11.6 | 9.8–13.4 | 236 | 10.5 | 9.3–11.8 | 826 | 12.8 | 12.0–13.6 | 1143 | 12.0 | 11.4–12.7 |
| Unknown | 0 | 0 | 0 | 0 | 7 | 0.1 | 7 | 0.08 | ||||
| ROSC* | 430 | 35.4 | 32.8–38.1 | 631 | 28.10 | 26.3–30.0 | 2243 | 34.8 | 33.7–36.0 | 3158 | 33.2 | 32.3–34.2 |
| Unknown | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | ||||
| Survival to hospital discharge* | 141 | 11.6 | 9.8–13.4 | 250 | 11.20 | 9.8–12.5 | 447 | 6.9 | 6.3–7.6 | 909 | 9.6 | 9.0–10.2 |
Abbreviations: EMS = emergency medical services; CPR = cardiopulmonary resuscitation; AED = automated external defibrillator; VT = ventricular tachycardia; VF = ventricular fibrillation; ROSC = return of spontaneous circulation.
p < 0.01.
Although females were less likely to arrest in public, have a witnessed arrest, or have a shockable rhythm, females in the 12–49 year old age group were more likely to have ROSC than their age-matched male counterparts, while proportions of patients with ROSC were relatively similar across sex groups in the ≥50 years of age group (Table 2). Although females overall had decreased survival to hospital discharge, when age stratified, females in the 12–49 year old age group had similar a proportion of survival to hospital discharge when compared to age-matched males (females 12–49 = 11.6%, 95% CI: 9.8–13.4 vs. males 12–49 = 11.2%, 95% CI: 9.8–12.5), while males in the older age group were more likely to survive compared to females (females ≥50 = 6.9%, 95% CI: 9.0–10.2 vs. males ≥50 = 9.6%, 95% CI 9.0–10.2).
3.4. Adjusted models stratified by sex and age
An initial regression using age as a continuous variable demonstrated an association between female sex and increased survival (odds ratio [OR] 1.23, 95% CI: 1.09–1.39), while older age (≥50 years) was associated with decreased survival (OR 0.98, 95% CI: 0.98–0.99) (Table 3). We tested whether there was effect modification between female sex and age, which was found to be significant (p < 0.01). As a result, we chose to perform age-stratified regressions to compare younger females with younger males and older females to older males to test the independent effect of sex on survival to hospital discharge, while adjusting for age.
Table 3.
Results of the hierarchical multivariable logistic regression for survival to hospital discharge.
| Characteristics | All ages (n =19,398) | 12–49 years of age (n = 3455) | ≥50 years of age (n = 15,943) | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Female | 1.23 | (1.09–1.38) | 1.55 | (1.20–2.00) | 1.18 | (1.03–1.35) |
| Age | 0.98 | (0.98–0.99) | 1.00 | (0.99–1.02) | 0.98 | (0.97–0.98) |
| Race/ethnicity | ||||||
| Black | 0.76 | (0.66–0.87) | 0.70 | (0.51–0.96) | 0.77 | (0.65–0.91) |
| Hispanic | 0.72 | (0.55–0.95) | 0.64 | (0.37–1.10) | 0.75 | (0.56–1.01) |
| White | Reference | |||||
| Other | 1.01 | (0.71–1.44) | 0.65 | (0.27–1.56) | 1.09 | (0.75–1.60) |
| Public arrest | 1.42 | (1.28–1.57) | 1.42 | (1.15–1.74) | 1.41 | (1.25–1.58) |
| Witnessed by bystander | 2.43 | (2.12–2.77) | 2.06 | (1.55–2.74) | 2.53 | (2.18–2.95) |
| Witnessed by EMS | 2.17 | (1.85–2.54) | 1.59 | (1.10–2.31) | 2.35 | (1.97–2.80) |
| Bystander CPR | 1.32 | (1.17–1.49) | 1.21 | (0.94–1.57) | 1.37 | (1.19–1.57) |
| Public AED used | 1.07 | (0.94–1.21) | 1.00 | (0.77–1.31) | 1.09 | (0.95–1.26) |
| Shockable rhythm | 6.39 | (5.70–7.16) | 7.83 | (6.03–10.16) | 5.93 | (5.21–6.74) |
Abbreviations: EMS = emergency medical services; CPR = cardiopulmonary resuscitation; AED = automated external defibrillator; VT = ventricular tachycardia; VF = ventricular fibrillation.
Within the 12–49 year old age group, female sex was associated with an increased odds of survival to discharge (OR 1.55, 95% CI: 1.20–2.00) (Table 3), while the association with age was not significant (OR 1.00, 95% CI: 0.99–1.02). African-American patients had a decreased association with survival (OR 0.70, 95% CI: 0.51–0.96). Consistent with our initial models, arrests that occurred in public, were witnessed by bystanders or EMS, and had a shockable presenting rhythm were all positively associated with survival (Table 3).
In the ≥50 year old age group, female sex was still associated with increased survival to hospital discharge, although the magnitude of effect was decreased (OR 1.18, 95% CI: 1.03–1.35). Again, consistent with prior models, those arrests that occurred in public, were witnessed by bystanders or EMS, or had a shockable presenting rhythm were all positively associated with survival. Bystander CPR, although significant in the overall models, was only significantly associated with survival to hospital discharge in the older age group (OR 1.37, 95% CI: 1.19–1.57).
The increased odds of survival for female sex in the 12–49 year old age group persisted in a complete case analysis (OR 1.51, 95% CI: 1.12–2.02). The association of female sex and increased survival also persisted in the fully adjusted models until 55 years of age (Appendix Table 2).
4. Discussion
We examined the association between age and sex and survival to discharge for patients with OHCA in a large out-of-hospital cardiac arrest registry from a broad, heterogeneous United States population. We found that female sex was independently associated with increased survival among patients aged 12–49 years. In contrast, females had a smaller association with survival after the age of 50 years, which only persisted until the age of 55 years. Our work, in combination with three other recent large-scale studies,6–8 has important research implications that may lead to a potential new area of research in the role of female sex hormones in cardiac arrest resuscitation.
There is a growing body of evidence suggesting that females of childbearing age are more likely to survive a cardiac arrest event, despite being more likely to have arrest characteristics that are associated with poor outcomes (unwitnessed arrest, private location, non-shockable rhythm).2,3 Similar to our results, two recent studies from Japan have demonstrated a survival benefit after out of hospital cardiac arrest for females of childbearing age.6,7 Akahane et al. analyzed the largest study sample to date, over 300,000 cardiac arrests from Japan over a 3-year time period. This study found a significant survival benefit among females, although the presenting rhythm at the time of arrest was not included as a confounding variable within their regression analysis. A subgroup analysis on patients who had ventricular fibrillation or ventricular tachycardia upon presentation did not demonstrate the same age dependant survival benefit that we have reported. Within this subgroup of patients with shockable presenting rhythms, the youngest females of childbearing age did not show a survival benefit after OHCA when compared to age-matched males (20–29 years old) but a benefit in older females continued until the age of 80. Although Kitamura et al. did not perform a subgroup analysis of patients with ventricular tachycardia or ventricular fibrillation, they did include presenting rhythm within their regression analysis and did not observe a survival benefit in older women. Further analysis within the Japanese database is necessary to determine why there is observed variability in these age groups before these results can be compared to our US population.
Although we have found results similar to the study by Kitamura et al, our research is the first to examine the association between sex and age across multiple U.S. cities and from vastly different healthcare settings and patient populations. The CARES patient population was significantly more heterogeneous in terms of race and ethnicity and characteristics of the EMS system as compared to the relatively homogenous Japanese population.6 We found that African-American and Hispanic patients were independently associated with a decreased likelihood of survival (African American OR 0.80 (95% CI 0.69–0.93); Hispanic OR 0.77, 95% CI 0.59–1.00) even after adjusting for patient and event characteristics. This is consistent with prior research that has shown that racial disparities in survival exist in OHCA and may be dependent on delays to recognition of cardiac arrest,21,22 decreased likelihood of receiving CPR and having an AED used21–27 and delays to thrombolytics and cardiac catheterization.28–30 Future research, using CARES, will need to be conducted to better understand the interaction between socioeconomics, race, and age on cardiac arrest survival.
It has been postulated that the observed sex and age difference in survival may be related to the elevated levels of female sex hormones in women of childbearing age.31 Basic science research has shown that female estrogen and progesterone act directly on vascular endothelial cells to decrease the development of cerebral edema, decrease the inflammatory-cascade, and have a protective effect on the neuronal and cardiac systems, thus leading to reduced reperfusion injury and post-cardiac arrest fatality.9–14 The possible neuroprotective role of female sex hormones is currently being studied in the setting of traumatic brain injury, stroke, global cerebral ischemia, and spinal cord injury. While there are phase II clinical trials underway using a single dose of estrogen for both traumatic brain injury and hemorrhagic shock, there has only been one large Phase III multi-centered, randomized clinical controlled trial conducted to assess the effect of progesterone on neurological outcomes from traumatic brain injury.32 In cardiac arrest, there have been no published clinical trials conducted in humans that examine the efficacy of female hormones on cardiac arrest survival. The growing body of evidence suggests that the role of female sex hormones may be a promising area of research in resuscitation science.
Our study has several potential limitations. The CARES registry includes patients with non-traumatic out-of-hospital arrest for whom CPR was performed and alternative (i.e., non-cardiac) causes of the arrest cannot be clearly demonstrated. Because CARES does not include specific variables related to etiology, it is possible that our results reflected young females arresting from causes that are inherently more survivable and not due to a protective effect of female sex hormones. For example, young females are more likely to develop venous embolic disease,33 attempt suicide by non-traumatic mechanisms,34,35 or be at risk for complications related to pregnancy (e.g., ectopic pregnancy). These etiologies may be associated with higher survival than etiologies of primary cardiac origin. Additionally, the 12–49 years of age cohort included a larger male to female ratio than the 50 years of age and older cohort. This may reflect differential selection bias between the two groups, or may suggest that female hormones in and of themselves contribute to the prevention of cardiac arrest.
We were also unable to collect hormone levels at the time of cardiac arrest within our study population, and therefore cannot draw direct comparisons between serum hormone concentrations and survival. A limitation of the dataset is that individual-level race/ethnicity was missing or coded as “unknown” in approximately 24% of the sample; as such, we chose to impute race/ethnicity rather than to systematically restrict the dataset or categorize these data as “unknown”. Multiple imputation has been shown to be an appropriate statistical approach for handling data in similar instances. Also, due to the limitations of how CARES data are collected, we were not able to account for response intervals, presence of comorbidities, or EMS/hospital treatments that may have contributed to survival. However, we did use hierarchical modeling to help adjust for underlying variations within communities included in this study.
5. Conclusion
This is the first study to be conducted across multiple sites in the U.S., composed of heterogeneous racial/ethnic populations, that shows a significant association between age, sex, race/ethnicity and survival to hospital discharge. Further research needs to be conducted on the pathophysiologic mechanisms of age and sex in OHCA, including the potential use of female sex hormones as a pharmacologic intervention to increase the dismal rate of survival from cardiac arrest.
Supplementary Material
Acknowledgment
This research was supported, in part, by an Independent Scientist Award (K02 HS017526) from the Agency for Healthcare Research and Quality to Dr. Haukoos.
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2012.09.011.
Presented, in part, at the Western Regional Meeting of the Society for Academic Emergency Medicine, February 24–26, 2011, Keystone, CO, and the Society for Academic Emergency Medicine Annual Meeting, June 1–5, 2011, Boston, MA.
Conflict of interest statement
The authors report no conflicts of interest.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resuscitation.2012.09.011.
References
- 1.Lloyd-Jones D, Adams R, Carnethon R, et al. Heart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 2.Perers E, Abrahamsson P, Bång A, et al. There is a difference in characteristics and outcome between women and men who suffer out of hospital cardiac arrest. Resuscitation. 1999;40:133–140. doi: 10.1016/s0300-9572(99)00022-2. [DOI] [PubMed] [Google Scholar]
- 3.Polentini MS, Pirrallo RG, McGill W. The changing incidence of ventricular fibrillation in Milwaukee Wisconsin (1992–2002) Prehosp Emerg Care. 2006;10:52–60. doi: 10.1080/10903120500366961. [DOI] [PubMed] [Google Scholar]
- 4.Kim C, Fahrenbruch CE, Cobb LA, Eisenberg MS. Out-of-hospital cardiac arrest in men and women. Circulation. 2001;104:2699–2703. doi: 10.1161/hc4701.099784. [DOI] [PubMed] [Google Scholar]
- 5.Wigginton JG, Pepe PE, Bedolla JP, DeTamble LA, Atkins JM. Sex-related differences in the presentation and outcome of out-of-hospital cardiopulmonary arrest: a multiyear, prospective, population-based study. Crit Care Med. 2002;30:S131–S136. doi: 10.1097/00003246-200204001-00002. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura T, Iwami T, Nichol G, et al. Reduction in incidence and fatality of out-of-hospital cardiac arrest in females of the reproductive age. Eur Heart J. 2010;31:1365–1372. doi: 10.1093/eurheartj/ehq059. [DOI] [PubMed] [Google Scholar]
- 7.Akahane M, Ogawa T, Koike S, et al. The effects of sex on out-of-hospital cardiac arrest outcomes. Am J Med. 2011;124:325–333. doi: 10.1016/j.amjmed.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Topjian AA, Localio AR, Berg RA, et al. Women of child-bearing age have better inhospital cardiac arrest survival outcomes than do equal-aged men. Crit Care Med. 2010;38:1254–1260. doi: 10.1097/CCM.0b013e3181d8ca43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurn PD, Macrae IM. Estrogen as a neuroprotectant in stroke. J Cereb Blood Flow Metab. 2000;20:631–652. doi: 10.1097/00004647-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Jover-Mengual T, Miyawaki T, Latuszek A, et al. Acute estradiol protects CA1 neurons from ischemia-induced apoptotic cell death via the PI3K/Akt pathway. Brain Res. 2010;1321:1–12. doi: 10.1016/j.brainres.2010.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lebesgue D, Chevaleyre V, Zukin RS, Etgen AM. Estradiol rescues neurons from global ischemia-induced cell death: multiple cellular pathways of neuroprotection. Steroids. 2009;74:555. doi: 10.1016/j.steroids.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hutchens MP, Nakano T, Kosaka Y, et al. Estrogen is renoprotective via a nonreceptor-dependent mechanism after cardiac arrest in vivo. Anesthesiology. 2010;112:395. doi: 10.1097/ALN.0b013e3181c98da9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruediger R, Noppens JK. Estradiol after cardiac arrest and cardiopulmonary resuscitation is neuroprotective and mediated through estrogen receptor-β. J Cereb Blood Flow Metab. 2009;29:277. doi: 10.1038/jcbfm.2008.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuhar P, Lunder M, Drevensek G. The role of gender and sex hormones in ischemic-reperfusion injury in isolated rat hearts. Eur J Pharmacol. 2007;561:151–159. doi: 10.1016/j.ejphar.2007.01.043. [DOI] [PubMed] [Google Scholar]
- 15.Mcnally B, Stokes A, Crouch A, Kellermann AL Group FTCS. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2010;54:1–12. doi: 10.1016/j.annemergmed.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 16.Anderson SE, Must A. Interpreting the continued decline in the average age at menarche: results from two nationally representative surveys of U.S. girls studied 10 years apart. J Pediatr. 2005;147:753–760. doi: 10.1016/j.jpeds.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Murabito JM, Yang Q, Fox C, Wilson PW, Cupples LA. Heritability of age at natural menopause in the Framingham Heart Study. J Clin Endocrinol Metab. 2005;90:3427–3430. doi: 10.1210/jc.2005-0181. [DOI] [PubMed] [Google Scholar]
- 18.Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research – Part 2: Multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 19.Newgard CD, Haukoos JS. Measuring quality with missing data: the invisible threat to national quality initiatives. Acad Emerg Med. 2010;17:1130–1133. doi: 10.1111/j.1553-2712.2010.00883.x. [DOI] [PubMed] [Google Scholar]
- 20.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–324. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329:600–606. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 22.Cowie MR, Fahrenbruch CE, Cobb LA, Hallstrom AP. Out-of-hospital cardiac arrest: racial differences in outcome in Seattle. Am J Public Health. 1993;83:955–959. doi: 10.2105/ajph.83.7.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–1150. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 24.Sayegh AJ, Swor R, Chu KH, et al. Does race or socioeconomic status predict adverse outcome after out of hospital cardiac arrest: a multi-center study. Resuscitation. 1999;40:141–146. doi: 10.1016/s0300-9572(99)00026-x. [DOI] [PubMed] [Google Scholar]
- 25.Feero S, Hedges JR, Stevens P. Demographics of cardiac arrest: association with residence in a low-income area. Acad Emerg Med. 1995;2:11–16. doi: 10.1111/j.1553-2712.1995.tb03071.x. [DOI] [PubMed] [Google Scholar]
- 26.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 27.Reinier K, Thomas E, Andrusiek DL, et al. Socioeconomic status and incidence of sudden cardiac arrest. Can Med Assoc J. 2011;183:1705. doi: 10.1503/cmaj.101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001;344:1443–1449. doi: 10.1056/NEJM200105103441906. [DOI] [PubMed] [Google Scholar]
- 29.Gibler WB, Armstrong PW, Ohman EM, et al. Persistence of delays in presentation and treatment for patients with acute myocardial infarction: the GUSTO-I and GUSTO-III experience. Ann Emerg Med. 2002;39:123–130. doi: 10.1067/mem.2002.121402. [DOI] [PubMed] [Google Scholar]
- 30.Liu JM, Yang Q, Pirrallo RG, Klein JP, Aufderheide TP. Hospital variability of out-of-hospital cardiac arrest survival. Prehosp Emerg Care. 2008;12:339–346. doi: 10.1080/10903120802101330. http://dx.doi.org/10.1080/10903120802101330. [DOI] [PubMed] [Google Scholar]
- 31.Wigginton JG, Pepe PE, Idris AH. Rationale for routine and immediate administration of intravenous estrogen for all critically ill and injured patients. Crit Care Med. 2010;38:S620–S629. doi: 10.1097/CCM.0b013e3181f243a9. [DOI] [PubMed] [Google Scholar]
- 32.Wright DW, Kellermann AL, Hertzberg VS, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49:391–402. 402.e1–402.e2. doi: 10.1016/j.annemergmed.2006.07.932. [DOI] [PubMed] [Google Scholar]
- 33.Moores L, Bilello KL, Murin S. Sex and gender issues and venous thromboembolism. Clin Chest Med. 2004;25:281–297. doi: 10.1016/j.ccm.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 34.Varnik A, Kolves K, van der Feltz-Cornelis CM, et al. Suicide methods in Europe: a gender-specific analysis of countries participating in the “European Alliance Against Depression”. J Epidemiol Community Health. 2008;62:545–551. doi: 10.1136/jech.2007.065391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ojima T, Nakamura Y, Detels R. Comparative study about methods of suicide between Japan and the United States. J Epidemiol. 2004;14:187–192. doi: 10.2188/jea.14.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.