Abstract
Buchang naoxintong capsule (BNC) is a traditional Chinese medicine approved for the treatment of cerebrovascular and cardiovascular diseases. However, little is known about the specific protective function or mechanism by which BNC protects against myocardial injury. This research was designed to investigate the cardioprotective effects of BNC in vitro model of hydrogen peroxide (H2O2)-induced H9c2 rat cardiomyoblasts. BNC intestinal absorption liquid was used in this study instead of drug-containing serum or extracting solution. Our study revealed that BNC preconditioning enhanced antioxidant function by increasing the activities of total-antioxygen capacity, total-superoxide dismutase, and catalase and by decreasing the production of reactive oxygen species and malondialdehyde. BNC preconditioning also activated extracellular signal-regulated kinases (ERK1/2) and inhibited apoptosis-related proteins such as poly ADP-ribose polymerase (PARP) and caspase-3. Additionally, preincubation with BNC reduced intracellular Ca2+ concentration, improved mitochondrial membrane potential, and decreased the apoptosis rate of H9c2 cells in a dose-dependent manner. These data demonstrated that BNC protects H9c2 cardiomyoblasts from H2O2-induced oxidative injury by increasing antioxidant abilities, activating ERK1/2, and blocking Ca2+-dependent and mitochondria-mediated apoptosis. Based on our results, the potency of BNC for protecting H9c2 cells from oxidative damage is comparable to that of trimetazidine.
1. Introduction
Oxidative stress plays a critical role in the pathophysiology of several major cardiovascular diseases such as atherosclerosis, hypertension, heart failure, and myocardial ischemical reperfusion injury [1, 2]. Significant oxidative stress causes excessive production of reactive oxygen species (ROS), which is an important event in the development of cardiovascular diseases. ROS accumulation may contribute to a number of cardiovascular disorders [3, 4]. Cellular sources of ROS come from the mitochondrial electron transport chain, xanthine oxidase, NADPH oxidase, lipoxygenase/cyclooxygenase, nitric oxide synthase, and autoxidation of various substances particularly catecholamines [5].
Increased ROS cause significant damage to myocardial cells, which can be neutralized by antioxidant molecules such as superoxide dismutase (SOD), catalase (CAT), and glutathione (GSH). These antioxidant molecules counteract oxidation and play vital roles in maintaining a stable intracellular environment. Moreover, ROS damage cellular membrane by causing lipid peroxidation. Malondialdehyde (MDA) is a major lipid peroxidation product and may reflect the degree of cellular injury [6].
Extracellular signal-regulated kinases (ERKs) have been reported to be activated by oxidative stress in some cell types and play important roles in many aspects of cellular function [7]. ERK1/2 activation by ROS in cardiomyocytes mediates a wide range of activities including metabolism, migration, inflammation, cell survival, and cell death [8]. Indeed, DNA microarray data showed that nearly 100 genes were involved in cellular responses to oxidative stress [9].
Buchang naoxintong capsule (BNC) consists of 16 various kinds of traditional Chinese medicines including Astragalus membranaceus, Salvia miltiorrhiza, Ligusticum, Radix paeoniae rubra, Szechwan lovage Rhizome, Semen persicae, Carthamus tinctorius L, Frankincense, myrrh, Spatholobus suberectus, Achyranthes Root, Cassia Twig, Mulberry Twig, earthworms, scorpions, and hirudo, which is an approved traditional Chinese medicine for stroke and angina [10]. BNC protected mice from atherosclerosis by reducing lipid concentrations and inhibiting maturation of dendritic cells [11]. BNC also increased the catalytic activity of the drug-metabolizing CYP2C19 enzyme [12]. The combination of BNC and clopidogrel enhanced the antiplatelet effect in patients with the CYP2C19∗2 gene mutation [13]. BNC has been shown to have protective effects in cardiac and vascular diseases. However, the cellular and molecular mechanisms of BNC cardioprotective activity have not yet been elucidated.
In this study, oxidative stress was induced by exposing H9c2 cells to H2O2, which is a well-established model [14]. Treatments consisted BNC intestinal absorption liquids rather than extraction solutions or drug-containing sera. Trimetazidine (TMZ), a common treatment for angina in cardiac patients, served as a control [15, 16].
2. Materials and Methods
2.1. Animals
Adult male Sprague Dawley rats weighing 220 ± 10 grams (g) were purchased from the Experimental Animal Center of Peking University Health Science Center, Beijing, China (certificate no. SCXK (Jing) 2009-0017). The experiment was approved by the local Committee on Animal Care and Use.
2.2. Materials
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), TMZ, and H2O2 solution (35 wt.% in water) were purchased from Sigma (USA). The JC-1 commercial kit was obtained from Beyotime (China). The 2′,7′-dichlorofluorescein diacetate (DCFH-DA) probe, the total-antioxygen capacity (T-AOC) kit, the total superoxide dismutase (T-SOD) kit, the CAT kit, and the MDA kit were obtained from Nanjing Jiancheng (China). BNCs (Med-drug Permit no. Z20025001) were obtained from Buchang Pharmaceutical Co. Ltd. Pharmaceutical standard materials for the liquid chromatography experiment were purchased from the National Institutes for Food and Drug Control in China. All chemicals were of analytical grade.
2.3. Preparation of BNC Intestinal Absorption Liquid and Treatment of Rat Intestines
The powder from 100 g BNC was dissolved in 2,000 mL 95% ethanol. This solution was heated until boiling for 2 hours (h) under reflux and then filtered. Water was added in the filtrate to make a 200-mL BNC extraction solution. The 200 mL BNC extraction solution was evaporated with a rotary evaporator until almost completely dry. Tyrode's buffer solution (NaCl 8.00 g, KCl 0.28 g, NaHCO3 1.00 g, NaH2PO4 0.05 g, MgCl2 0.10 g, CaCl2 0.20 g, glucose 1.00 g, pH 7.4) was added to bring the volume of BNC solution to 600 mL. Rats were maintained in fasting conditions for 12 h before the experiment. Anesthesia was provided, and the intestine of each rat was quickly removed. Intestines were washed with Tyrode buffer solution (0°C) and cut into four 14 cm segments. Each segment was turned inside-out and ligated to form a sac at one end. The sac filled with Tyrode buffer was incubated in Magnus' bath for 5 minutes (min) to reach equilibration. Buffer was then exchanged with BNC solution (25 mL), which was maintained at 37°C and continuously injected with O2/CO2 (95%/5%). Serosal-side solutions containing absorbed constituents (2 mL) were drained into tubes after 2 h. BNC intestinal absorption liquids were filtered with a microfiltrate membrane (0.22 μm) and stored at −20°C. The original concentration of BNC intestinal absorption liquid was 1 mg/mL (crude drug).
2.4. Liquid Chromatography
BNC intestinal absorption liquid was analyzed by Ultra Performance Liquid Chromatography (UPLC) with a Waters ACQUITY C18 column (2.1 mm × 150 mm, 1.7 μm). The mobile phase consisted of acetonitrile and 0.5% formic acid with gradient elution at a flow rate of 0.3 mL/min. The detection wavelengths were set at 235, 280, 324, and 400 nm. The injection volume was 2 μL and the column temperature was maintained at 30°C.
2.5. Cell Culture and Treatment
The H9c2 cell line was obtained from the Cell Resource Center of Peking Union Medical College in China. Cells were cultured in high-glucose DMEM (Invitrogen, USA) supplemented with 10% fetal calf serum (Hangzhou Sijiqing, China) and a combination of penicillin-streptomycin in a humidified 5% CO2 atmosphere at 37°C. Cells were nearly 80% confluent and then treated with different concentrations of BNC for 24 h before addition of 100 μM H2O2 for 1 h.
2.6. MTT Assay
The optimum concentration and application time for H2O2 and the protective effect of BNC on H9c2 cells were determined by MTT assay. Cells were dispersed by trypsinization and seeded at (8,000–10,000) cells/well in a 96-well plate overnight before being treated. Subsequently, 20 μL MTT solution (5 mg/mL) was added to each well and incubated at 37°C for 4 h. The supernatant was removed, and the insoluble formazan product was dissolved in 150 μL DMSO. Absorbance of each culture well was measured with a microplate reader (Molecular Devices, USA) at a wavelength of 570 nm.
2.7. Biochemical Analysis of H9c2 Cell Lysate
H9c2 cells were adjusted to 1 × 106 cell/mL after trypsinization, washed with phosphate-buffered saline (PBS) twice, and centrifugated at 1,500 rpm/min for 10 min. The supernatant were then removed. The precipitate obtained through centrifugation was crushed by ultrasonic wave, and the cell lysates were resuspended. T-AOC, T-SOD, CAT, and MDA were determined with a microplate reader (Molecular Devices, USA) according to the protocol of the detection kit. Protein content was measured with the BCA Bradford protein assay (Pierce, USA).
2.8. Detection of Intracellular ROS
Intracellular ROS was measured with the DCFH-DA probe. Digestive H9c2 cell suspensions were incubated with 10 μM DCFH-DA for 30 min and then washed three times with PBS to remove residual probe. The cellular fluorescence intensities were measured with a fluorescence microplate reader (Molecular Devices, USA). Excitation and emission wavelengths were set at 488 nm and 525 nm, respectively.
2.9. Detection of Apoptosis with Annexin V-PI
H9c2 cells were harvested with 0.25% trypsin, washed twice with cold PBS (4°C), and resuspended in 500 μL binding buffer. Cells were incubated with 10 μL Annexin V for 60 min in the dark at 4°C, and then with 5 μL propidium iodide for 5 min at room temperature. Fluorescence was analyzed with a FACStar Plus flow cytometer (Becton-Dickinson, USA).
2.10. Measurement of Cytosolic Ca2+ Concentration
Cytosolic Ca2+ was assessed with the cell-permeable and high-affinity fluorescent Ca2+ indicator Fluo-3/AM. H9c2 cells were collected with trypsin and centrifuged (1,000 rpm, 5 min). Cells were washed with PBS and incubated with 5 mM Fluo-3/AM dye for 40 min at 37°C. The concentration of Ca2+ was measured with a FACStar Plus flow cytometer (Becton-Dickinson, USA).
2.11. Measurement of Mitochondrial Membrane Potential (MMP)
H9c2 cells were harvested with trypsin and centrifuged (1000 rpm, 5 min). Medium (1 mL) and 5 μM JC-1 dye (1 mL) were added to the centrifugal precipitation for 20 min at 37°C. Cells were washed with dye buffer twice and detected with a FACStar Plus flow cytometer (Becton-Dickinson, USA). Mean FL2 fluorescence intensity indicated the mitochondrial membrane potential.
2.12. Western Blot Analysis
Protein samples were prepared from H9c2 cells with RIPA buffer (Beijing Baosai, China). Protein content was measured with the BCA Bradford protein assay. Cell lysates were separated by 10% SDS-PAGE and transferred onto PVDF membranes (Millipore, USA). Membranes were incubated with primary antibody (Cell Signaling Technology, USA) and then with HRP-conjugated secondary antibody (Zhongshanjinqiao, China). Proteins were detected with an enhanced chemiluminescence agent (Millipore, USA). β-actin (Cell Signaling Technology, USA) served as an internal control.
The antibodies included rabbit monoclonal antibodies against caspase-3 (1 : 1000), PARP (1 : 1000), ERK1/2 (1 : 1000), p-ERK1/2 (1 : 1000), β-actin (1 : 1000), and horseradish peroxidase-conjugated secondary antibodies (goat anti-rabbit, 1 : 2000).
2.13. Statistical Analysis
The experiment was performed at least 3 times, and all values are expressed as means ± standard deviation (SD). Data were compared by one-way ANOVA. Values of P < 0.05 were considered statistically significant.
3. Results
3.1. Qualitative Analysis of BNC Intestinal Absorption Liquid
Eleven constituents were detected in BNC extraction solution. These were calycosin, ligustilide, paeoniflorin, protocatechualdehyde, salvianolic acid B, senkyunolide A, tanshinone I, caffeic acid, ferulic acid, rosmarinic acid, and hydroxysafflor yellow A. Eight constituents in BNC intestinal absorption liquid were examined, which is consistent with BNC extraction solution except calycosin, ligustilide, and senkyunolide A. Results indicated that the composition of BNC intestinal absorption liquid was similar to that of BNC extraction solution (Figure 1).
Figure 1.
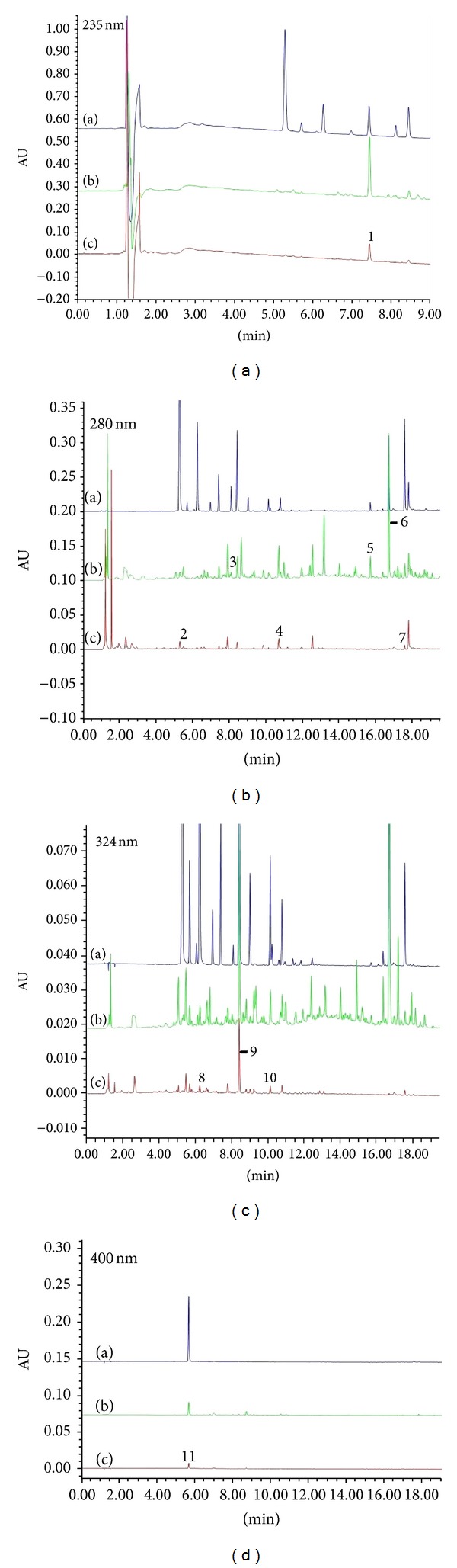
UPLC of Control (a), BNC extraction solution (b), and BNC intestinal absorption liquid (c). Chromatograms numbered from 1 to 11 represent paeoniflorin, protocatechualdehyde, calycosin, salvianolic acid B, senkyunolide A, ligustilide, tanshinone I, caffeic acid, ferulic acid, rosmarinic acid, and hydroxysafflor yellow A.
3.2. Working Concentration and Incubation Time of H2O2
Treatment with increasing concentrations of H2O2 (0, 5, 10, 25, 50, 100, 200, or 400 μM) for 1 h caused dose-dependent loss of cell viability. Incubation with 100 μM H2O2 at different time points (0, 0.5, 1, 2, 4, or 6 h) showed time-dependent reductions in viability. Treatment with 100 μM H2O2 for 1 h reduced cell viability, and survival rates were 57.87 ± 4.25% (Figure 2(a)) and 52.37 ± 3.90% (Figure 2(b)). Thus, cells were treated with this concentration in subsequent experiments.
Figure 2.
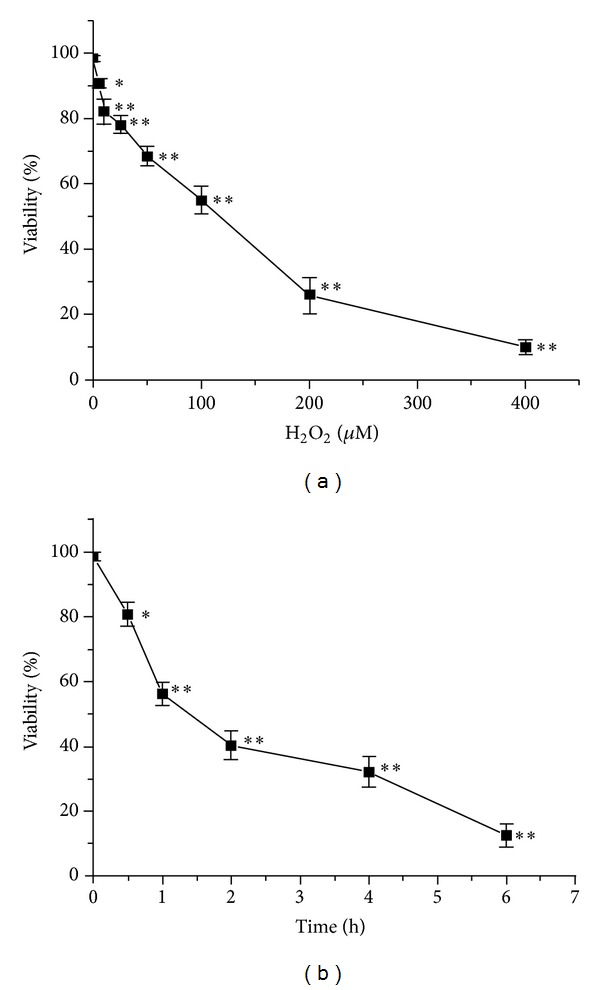
Determination of H2O2 working conditions. H9c2 cells were cultured with different concentrations of H2O2 for 1 h (a) or with 100 μM for different incubation times (b). Cell viability was detected by MTT assay. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control.
3.3. Effect of H2O2 on H9c2 Cell Viability
H9c2 cells were treated with H2O2 (100 μM) for 1 h in the absence or presence of BNC (0, 7.81, 15.63, 31.25, 62.50, 125, or 250 μg/mL). TMZ (10 μM) served as the control drug. Cell viability was measured by MTT assay (Figure 3(a)). Treatment with H2O2 significantly decreased the viability of H9c2 cells compared to control treatment. Pretreatment with 7.81, 15.63, 31.25, or 62.50 μg/mL BNC for 24 h increased cell viability, demonstrating a dose-dependent response. The results showed that 7.81, 15.63, 31.25, and 62.50 μg/mL BNC protected H9c2 cells from oxidative damage. H9c2 cells were incubated with 7.81, 15.63, 31.25, and 62.50 μg/mL BNC for 24 h, and none of these BNC solutions caused damage to H9c2 cells (Figure 3(b)).
Figure 3.
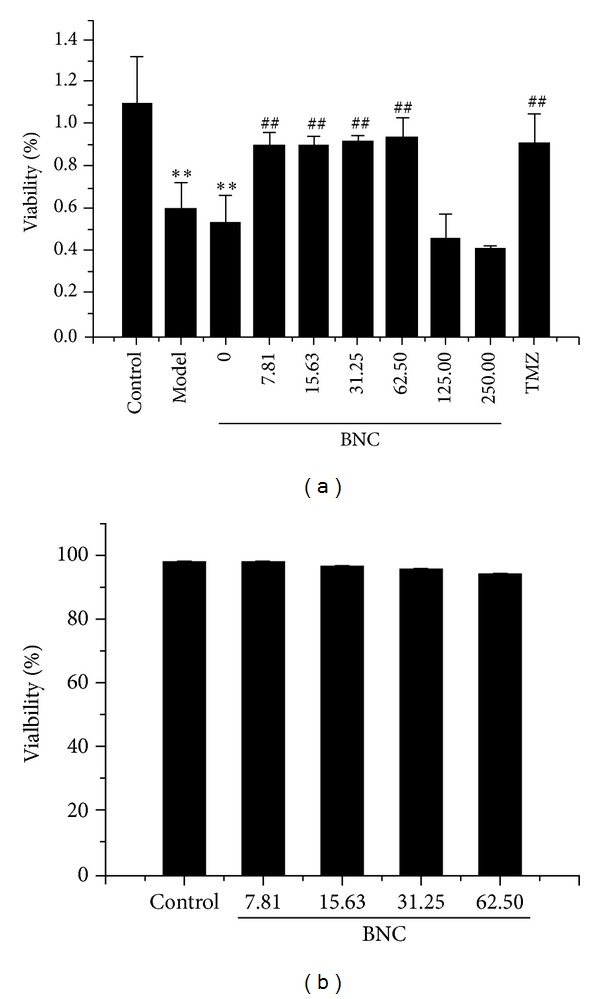
BNC rescued H2O2-induced loss of cell viability. H9c2 cells were pretreated with different concentrations of BNC (0, 7.81, 15.63, 31.25, 62.50, 125, or 250 μg/mL) for 24 h and then treated with 100 μM H2O2 for 1 h (a). H9c2 cells were preconditioned with different concentrations of BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) for 24 h (b). Cell viability was measured by MTT assay. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; ## P < 0.01 versus model.
3.4. Morphologic Changes in H9c2 Cells
The morphologies of H9c2 cells treated with H2O2 (100 μM) in the presence of BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) were observed with an inverted phase-contrast microscope (Olympus, Japan). Control H9c2 cells were normal with long fusiform shapes. H2O2 treatment induced distinctive morphological changes, such as cell shrinkage, irregular shape, and a wider intercellular gap. However, the proportion of abnormal cells in 15.63, 31.25, and 62.50 μg/mL BNC-pretreated groups decreased with increasing concentration of BNC (Figure 4).
Figure 4.
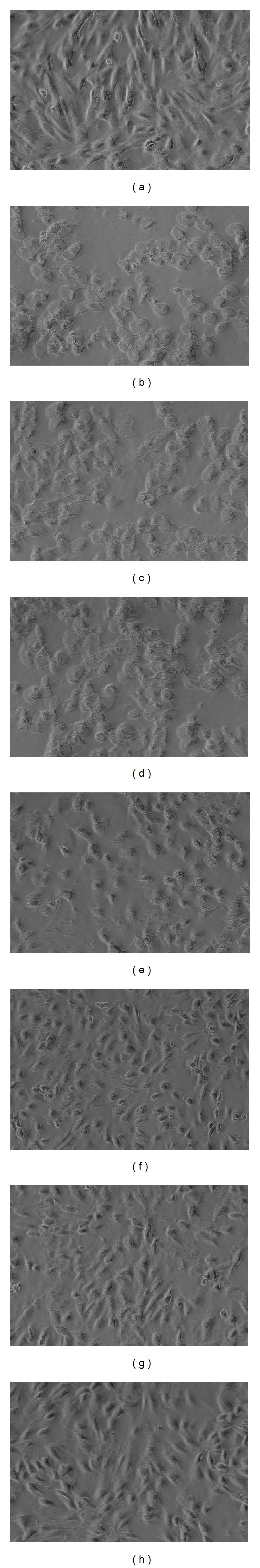
Changes in H9c2 cell morphology in response to H2O2 and/or BNC. (a) H9c2 cells without BNC or H2O2 (control); (b) H9c2 cells exposed to 100 μM H2O2 (model); ((c)–(h)) H9c2 cells pretreated with 0, 7.81, 15.63, 31.25, 62.50 μg/mL BNC or with 10 μM TMZ followed by treatment with 100 μM H2O2. Magnification: 200x.
3.5. BNC Protected H9c2 Cells from Damage Caused by H2O2-Induced Oxidative Stress
Oxidative stress has been implicated in the pathogenesis of myocardial injury. To determine whether BNC affects oxidative stress-related biochemical enzymes, the levels of oxidant and antioxidant enzymes, such as T-AOC, T-SOD, CAT, and MDA, were measured in H9c2 cell lysates. The activities of T-AOC, T-SOD, and CAT were increased in a dose-dependent manner in the BNC pretreatment group relative to the H2O2 group, whereas MDA production was reduced (Figure 5). These results confirmed that the in vitro antioxidant capacity of BNC was comparable to that of TMZ.
Figure 5.
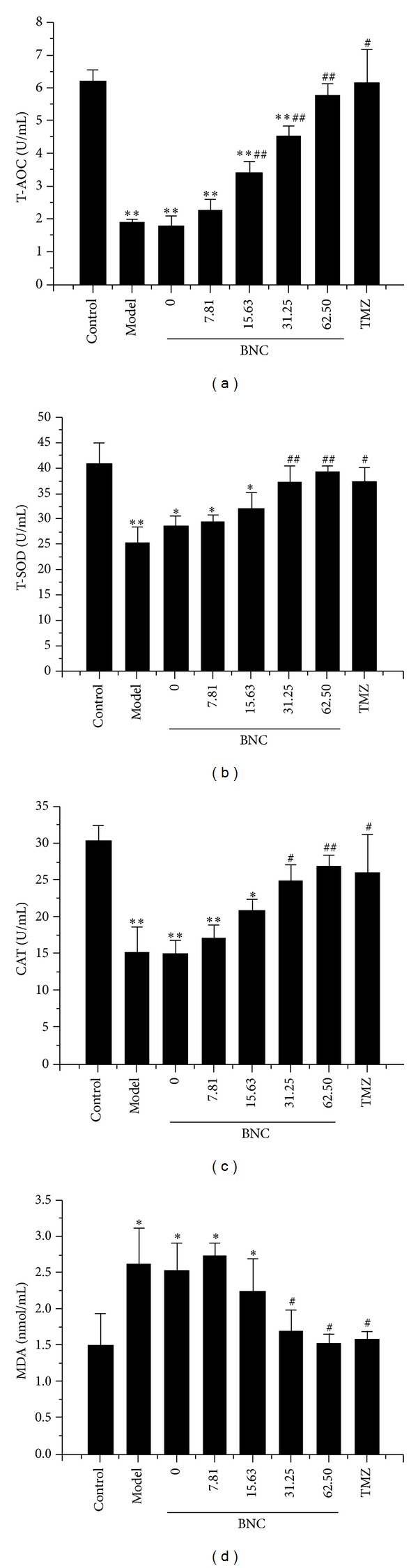
Protective effects of BNC via enhancing antioxidant function by increasing the activities of T-AOC, T-SOD, and CAT and decreasing the production of MDA detected by the T-AOC, T-SOD, CAT, and MDA assay kits. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model; # P < 0.05 versus model.
3.6. BNC Attenuated Intracellular ROS Generation
The generation of intracellular ROS by H2O2 promotes cellular damage. Intracellular ROS concentrations were measured with the DCFH-DA assay to determine if BNC attenuated cell death by reducing ROS generation. Intracellular ROS generation was significantly increased in H2O2-treated H9c2 cells. However, ROS generation was significantly reduced by BNC pretreatment in a concentration-dependent manner (Figure 6).
Figure 6.
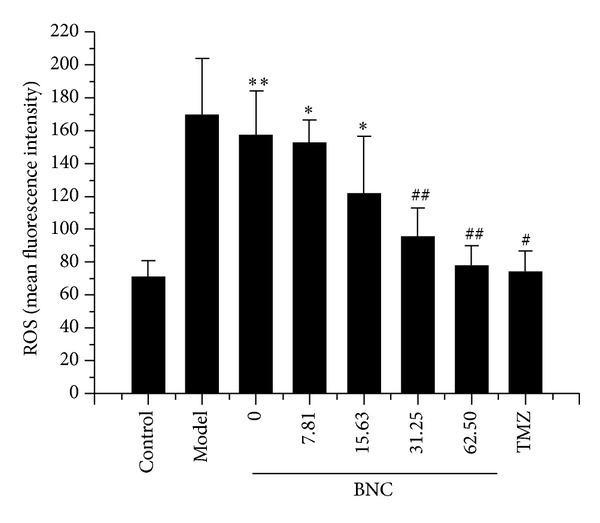
Protective effects of BNC due to reduced H2O2-induced generation of intracellular ROS measured by the DCFDA assay. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model; # P < 0.05 versus model.
3.7. BNC Protected H9c2 Cells from H2O2-Induced Apoptosis
The percentage of apoptotic cells was determined by Annexin V-FITC and PI staining to quantify the effects of BNC on H2O2-induced H9c2 apoptosis. The numbers of apoptotic cells were significantly increased upon treatment with 100 μM H2O2 in comparison to the untreated control group (24.54 ± 5.27% versus 2.05 ± 0.12%, P < 0.01). Cotreatment of H9c2 cells with 100 μM H2O2 and BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) for 24 h reduced the percentages of apoptotic cells to 16.56 ± 3.55%, 12.81 ± 2.64%, 9.48 ± 2.19%, and 7.18 ± 1.97%, respectively. The survival rates for the blank control group and the TMZ group were 23.19 ± 4.28% and 6.49 ± 1.32%, respectively (Figure 7). These experiments suggested that BNC protected cardiomyocytes by decreasing H2O2-induced early apoptosis. It also showed that BNC was equivalent to TMZ in protecting H9c2 cells from H2O2-induced apoptosis.
Figure 7.
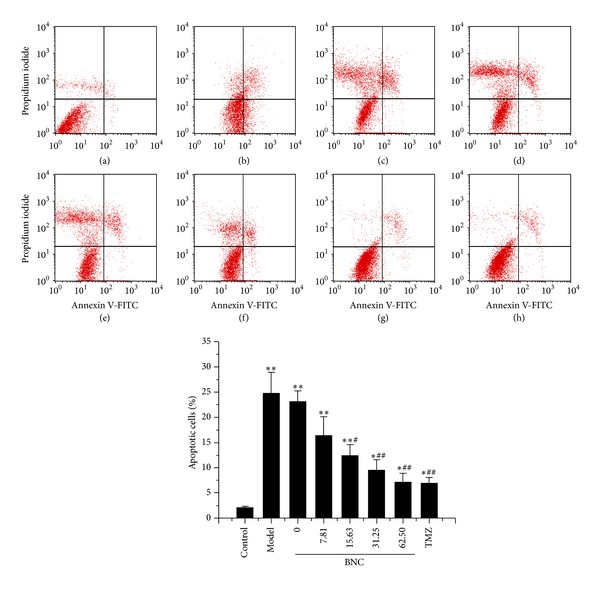
BNC protected H9c2 cells from H2O2-induced apoptosis, as detected by Annexin V-FITC and PI staining with FCM analysis. (a) H9c2 cells without BNC or H2O2 (control); (b) H9c2 cells exposed to 100 μM H2O2 (model); ((c)–(h)) H9c2 cells pretreated with 0, 7.81, 15.63, 31.25, 62.50 μg/mL BNC, or 10 μM TMZ followed by the treatment of 100 μM H2O2. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model; # P < 0.05 versus model.
3.8. BNC Decreased Cytosolic Ca2+ Concentrations
Intracellular Ca2+ accumulation and destruction of Ca2+ homeostasis are thought to initiate myocardial injury. Cytosolic Ca2+ concentrations were significantly higher in H2O2-treated H9c2 cells than in control cells, as measured by Fluo-3/AM staining. Furthermore, the cytosolic Ca2+ concentrations in H2O2-treated H9c2 cells pretreated with BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) were reduced in a dose-dependent manner (Figure 8).
Figure 8.
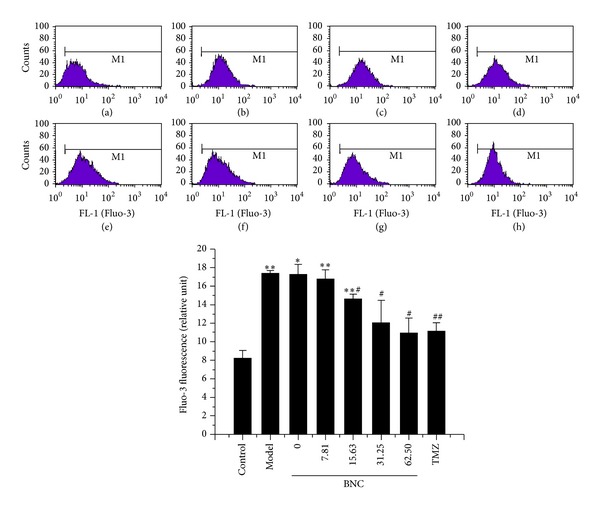
BNC reduced H2O2-induced cytosolic Ca2+ concentrations in H9c2 cells, as observed by Fluo-3/AM staining with FCM analysis. (a) H9c2 cells without BNC or H2O2 (control); (b) H9c2 cells exposed to 100 μM H2O2 (model); ((c)–(h)) H9c2 cells pretreated with 0, 7.81, 15.63, 31.25, 62.50 μg/mL BNC, or 10 μM TMZ followed by the treatment with 100 μM H2O2. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model; # P < 0.05 versus model.
3.9. BNC Rescued Loss of Mitochondrial Membrane Potential in H2O2-Treated H9c2 Cells
The loss of mitochondrial membrane potential is an important event of the apoptotic process. The JC-1 assay was used to determine whether mitochondria participated in H2O2-induced apoptosis. The mitochondrial membrane potential was markedly decreased in H9c2 cells treated with 100 μM H2O2 for 1 h, indicating that H2O2 treatment induced mitochondrial dysfunction (Figure 9). BNC pretreatment significantly reduced the loss of H2O2-induced mitochondrial membrane potential in a dose-dependent manner.
Figure 9.
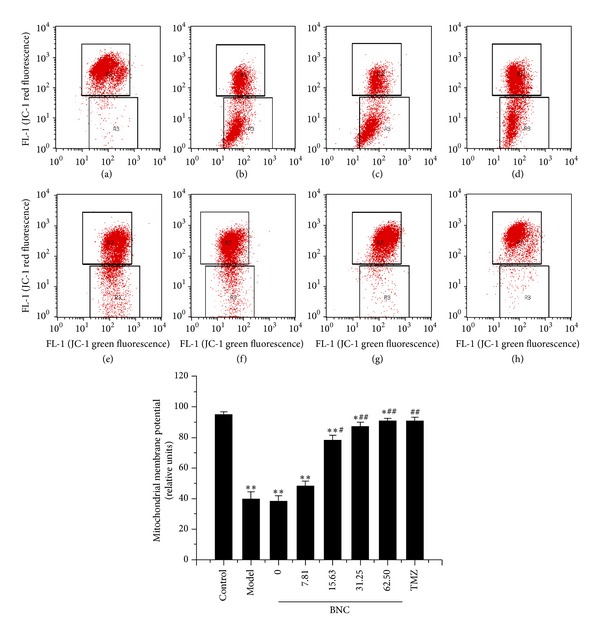
BNC attenuated H2O2-induced mitochondrial membrane potential loss in H9c2 cells, as assessed by JC-1 staining with FCM analysis. (a) H9c2 cells without BNC or H2O2 (control); (b) H9c2 cells exposed to 100 μM H2O2 (model); ((c)–(h)) H9c2 cells pretreated with 0, 7.81, 15.63, 31.25, 62.50 μg/mL BNC or 10 μM TMZ followed by treatment of 100 μM H2O2. Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model; # P < 0.05 versus model.
3.10. BNC Altered PARP and Caspase-3 Expression
PARP and caspase-3 activation are important biomarkers in the apoptotic process. Protein levels were examined by western blot analysis to investigate whether BNC protects H9c2 cells from H2O2-induced apoptosis. Caspase-3 activity was significantly increased in H9c2 cells treated with 100 μM H2O2 in comparison to control cells. Co-treatment of H9c2 cells with 100 μM H2O2 and BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) for 24 h significantly suppressed caspase-3 activity in a dose-dependent manner in comparison to H2O2-treated cells. Changes in PARP were also significantly altered. PARP cleavage was clearly detected in the H2O2 group, whereas PARP cleavage was not observed in the BNC group (Figure 10(a)). These results showed that BNC (7.81, 15.63, 31.25, or 62.50 μg/mL) prevented H2O2-induced apoptosis.
Figure 10.

Effects of BNC on expression of ERK1/2, p-ERK1/2, PARP, and caspase-3 in H9c2 cells treated with H2O2 (a) and effects of BNC on expression of ERK1/2 and p-ERK1/2 in the presence of ERK1/2 inhibitor, PD98059 (10 μM) (b). Protein expression was detected by western blot analysis. The ratio of p-ERK1/2/ERK1/2 significantly increased in response to BNC pretreatment (c). Values are expressed as mean ± SD from three independent experiments. **P < 0.01 versus control; *P < 0.05 versus control; ## P < 0.01 versus model.
3.11. BNC Induced Early Phosphorylation of ERK1/2
Mitogen-activated protein kinase (MAPK) family members were investigated to be involved in BNC-stimulated signaling. Protein lysates were collected and examined by western blot analysis for phospho-ERK1/2 and ERK1/2. Phosphorylation of ERK1/2 was moderately elevated after 1 h of H2O2 treatment (Figure 10(a)). However, pretreatment with BNC induced phosphorylation of ERK1/2 more rapidly, with increased band intensity present at 1 h. Expression of p-ERK1/2/ERK1/2 was significantly increased in cells preconditioned with BNC in comparison to the H2O2 group (Figure 10(c)). Pretreatment of cells with the highly selective ERK1/2 inhibitor, PD98059 (10 μM), indicated that ERK1/2 inhibition blocked the protective effect of BNC in H2O2-treated cells (Figure 10(b)).
4. Discussion
Oxidative stress in cardiomyocytes has an important role in the pathogenesis of many cardiovascular diseases, and ROS generated by oxidative stress are central to cardiac injury [17]. Studies have shown that mitochondria play prominent roles in the transduction and amplification of the apoptotic response in cardiomyocytes during oxidative stress [18, 19]. ROS promote the release of cytochrome c by increasing mitochondrial permeability. Pro-caspase-3 is downstream of cytochrome c in the apoptotic cascade and is cleaved by active caspase-9 to produce active caspase-3. In addition to caspases-6 and caspases-7, caspase-3 contributes to oligonucleosomal DNA fragmentation, which ultimately leads to apoptosis [20, 21]. Ca2+ is critical for cardiomyocyte contractility and for the signaling pathways in cardiac growth and remodeling. Cytosolic Ca2+ increases abnormally in cardiomyocytes as a consequence of ischemic reperfusion injury or other stresses, causing myocardial dysfunction and cell death. Increased Ca2+ activates calpains, leading to disruption of plasma membrane. Calpain activates the proapoptotic protein, BID. Calpain also cleaves autophagy protein 5, shifting the balance from autophagy to apoptosis [22]. We found that BNC inhibited H2O2-induced activation of PARP and caspase-3, reduced intracellular Ca2+ concentrations, and improved H2O2-induced impairment of the mitochondrial membrane potential. The present study clearly demonstrated that BNC inhibited H2O2-induced apoptosis by blocking Ca2+-dependent and mitochondria- dependent apoptosis.
The balance between ROS production and clearance of endogenous antioxidants is destroyed during oxidative stress, resulting in upregulation of endogenous antioxidants. Major endogenous antioxidants present in cardiomyocytes include SOD, CAT, GSH, glutathione peroxidase, ubiquinone, and vitamins. Our results suggested that BNC protected H2O2-induced injury by enhancing antioxidant abilities, such as increasing T-AOC, T-SOD, and CAT activities and decreasing ROS and MDA content.
MAPKs are serine/threonine protein kinases involved in cellular proliferation, differentiation, and death [23, 24]. Activation of the ERK1/2 MAPK subfamily in cardiac myocytes regulates expression of many genes and relates to the development of cellular hypertrophy. Activation of ERK1/2 in response to H2O2 is mediated through the Ras/Raf1/Mek pathway [25]. ERK1/2 activation may promote inflammation and result in necrosis by up-regulating interleukin-1β [26]. ERK1/2 activation may also inhibit apoptosis by down regulating Bad and up-regulating Bcl-2 [27]. Our research indicated that BNC exerted a protective effect against oxidative stress-mediated injury in H9c2 cells by inducing early phosphorylation of ERK1/2 (Figure 11).
Figure 11.
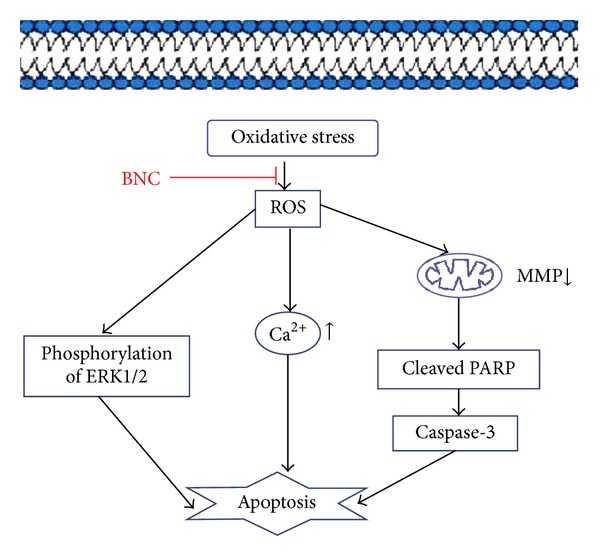
Schematic representation of BNC-mediated protection from H2O2-induced oxidative injury in H9c2 cells.
BNC is a traditional Chinese medicine for the treatment of cerebrovascular and cardiovascular diseases. BNC intestinal absorption liquid was used in this study instead of drug-containing serum and extraction solution. Traditional Chinese medicines are usually consumed orally. Thus, the small intestine is a major absorption site for herbal medicines. However, herbal mixtures contain multiple ingredients, and complicated herb-herb interactions can occur during intestinal absorption [28]. The process for producing intestinal absorption liquids imitates the complicated absorption process of traditional Chinese medicine. Absorbed constituents from the digestive tract may produce therapeutic effects [29]. UPLC analysis further confirmed that the compounds in BNC intestinal absorption liquids are similar to the compounds present in BNC extraction solution. Our studies lay a foundation for illuminating the cardioprotective effect of BNC preconditioning on oxidative stress damage. However, further studies need to be performed to understand and develop new strategies for cardioprotection during oxidative stress.
TMZ is a clinically effective antianginal drug that has direct cytoprotective effects on the myocardium. TMZ reduces oxygen free radical production at the cellular level [30], reduces intracellular calcium overload, and improves mitochondrial metabolism [31]. Mesenchymal stem cells that were preconditioned with TMZ before implantation significantly enhanced the recovery of myocardial function by increasing gene and protein expression levels of HIF-1, survivin, p-Akt, and Bcl-2. Our data demonstrated that H2O2-induced impairment was attenuated in TMZ-preconditioned H9c2 cells. These results are consistent with previous studies. These data indicated that the potency of BNC for protecting H9c2 cells from oxidative damage is similar to that of the positive control, TMZ.
5. Conclusion
BNC protected H9c2 cardiomyocytes from H2O2-induced oxidative injury by enhancing antioxidant abilities, activating ERK1/2 signaling, inhibiting apoptosis-related signal transduction pathways, reducing intracellular Ca2+ concentrations, and improving mitochondrial membrane potential. This research provides evidence that BNC exerted a protective effect on cardiovascular damage and the potency of BNC for protecting H9c2 cells from oxidative injury is comparable to that of trimetazidine.
Acknowledgments
This study was supported by the National High Technology Research and Development Program of China (no. 2011YZX09201-201-26) and National Science Foundation for Young Scientists of China (no. 81203005 and 81202793).
References
- 1.Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. Journal of Hypertension. 2000;18(6):655–673. doi: 10.1097/00004872-200018060-00002. [DOI] [PubMed] [Google Scholar]
- 2.Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circulation Journal. 2009;73(3):411–418. doi: 10.1253/circj.cj-08-1102. [DOI] [PubMed] [Google Scholar]
- 3.Crow MT, Mani K, Nam YJ, Kitsis RN. The mitochondrial death pathway and cardiac myocyte apoptosis. Circulation Research. 2004;95(10):957–970. doi: 10.1161/01.RES.0000148632.35500.d9. [DOI] [PubMed] [Google Scholar]
- 4.Simon HU, Haj-Yehia A, Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5(5):415–418. doi: 10.1023/a:1009616228304. [DOI] [PubMed] [Google Scholar]
- 5.Halliwell B. Reactive oxygen species in living systems: source, biochemistry, and role in human disease. The American Journal of Medicine C. 1991;91(supplement 3):S14–S22. doi: 10.1016/0002-9343(91)90279-7. [DOI] [PubMed] [Google Scholar]
- 6.Dhalla NS, Elmoselhi AB, Hata T, Makino N. Status of myocardial antioxidants in ischemia-reperfusion injury. Cardiovascular Research. 2000;47(3):446–456. doi: 10.1016/s0008-6363(00)00078-x. [DOI] [PubMed] [Google Scholar]
- 7.Aikawa R, Komuro I, Yamazaki T, et al. Oxidative stress activates extracellular signal-regulated kinases through Src and Ras in cultured cardiac myocytes of neonatal rats. Journal of Clinical Investigation. 1997;100(7):1813–1821. doi: 10.1172/JCI119709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adderley SR, Fitzgerald DJ. Oxidative damage of cardiomyocytes is limited by extracellular regulated kinases 1/2-mediate induction of cyclooxygenase-2. The Journal of Biological Chemistry. 1999;274(8):5038–5046. doi: 10.1074/jbc.274.8.5038. [DOI] [PubMed] [Google Scholar]
- 9.Napoli C, de Nigris F, Palinski W. Multiple role of reactive oxygen species in the arterial wall. Journal of Cellular Biochemistry. 2001;82(4):674–682. doi: 10.1002/jcb.1198. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Wang WR, Lin R, et al. Buyang Huanwu decoction ameliorates coronary heart disease with Qi deficiency and blood stasis syndrome by reducing CRP and CD40 in rats. Journal of Ethnopharmacology. 2010;130(1):98–102. doi: 10.1016/j.jep.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J, Zhu H, Wang S, et al. Naoxintong protects against Atherosclerosis through lipid-lowering and inhibiting maturation of dendritic cells in LDL receptor knockout mice fed a high-fat diet. Current Pharmaceutical Design. 2013;19(33):5891–5896. doi: 10.2174/1381612811319330008. [DOI] [PubMed] [Google Scholar]
- 12.Chen H, Zhang Y, Wu X, Li C, Wang H. In vitro assessment of cytochrome P450 2C19 potential of Naoxintong. Evidence-Based Complementary and Alternative Medicine. 2012;2012:6 pages. doi: 10.1155/2012/430262.430262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen H, Yu G, Sun H, Wu X, Wang H. Comparison of adjunctive naoxintong versus clopidogrel in volunteers with the CYP2C19*2 gene mutation accompanied with qi deficiency and blood stasis constitution. Evidence-Based Complementary and Alternative Medicine. 2011;2011:10 pages. doi: 10.1155/2011/207034.207034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coyle CH, Martinez LJ, Coleman MC, Spitz DR, Weintraub NL, Kader KN. Mechanisms of H2O2-induced oxidative stress in endothelial cells. Free Radical Biology and Medicine. 2006;40(12):2206–2213. doi: 10.1016/j.freeradbiomed.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Danchin N. Clinical benefits of a metabolic approach with trimetazidine in revascularized patients with angina. The American Journal of Cardiology. 2006;98(5):8J–13J. doi: 10.1016/j.amjcard.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Wisel S, Khan M, Kuppusamy ML, et al. Pharmacological preconditioning of mesenchymal stem cells with trimetazidine (1-[2,3,4-trimethoxybenzyl]piperazine) protects hypoxic cells against oxidative stress and enhances recovery of myocardial function in infarcted heart through Bcl-2 expression. Journal of Pharmacology and Experimental Therapeutics. 2009;329(2):543–550. doi: 10.1124/jpet.109.150839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kevin LG, Novalija E, Stowe DF. Reactive oxygen species is mediators of cardiac injury and protection: the relevance to anesthesia practice. Anesthesia and Analgesia. 2005;101(5):1275–1287. doi: 10.1213/01.ANE.0000180999.81013.D0. [DOI] [PubMed] [Google Scholar]
- 18.Suleiman MS, Halestrap AP, Griffiths EJ. Mitochondria: a target for myocardial protection. Pharmacology and Therapeutics. 2001;89(1):29–46. doi: 10.1016/s0163-7258(00)00102-9. [DOI] [PubMed] [Google Scholar]
- 19.Dedkova EN, Blatter LA. Measuring mitochondrial function in intact cardiac myocytes. Journal of Molecular and Cellular Cardiology. 2012;52(1):48–61. doi: 10.1016/j.yjmcc.2011.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franklin JL. Redox regulation of the intrinsic pathway in neuronal apoptosis. Antioxidants and Redox Signaling. 2011;14(8):1437–1448. doi: 10.1089/ars.2010.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorn GW., II Apoptotic and non-apoptotic programmed cardiomyocyte death in ventricular remodelling. Cardiovascular Research. 2009;81(3):465–473. doi: 10.1093/cvr/cvn243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy E, Steenbergen C. Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiological Reviews. 2008;88(2):581–609. doi: 10.1152/physrev.00024.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrington TP, Johnson GL. Organization and regulation of mitogen-activated protein kinase signaling pathways. Current Opinion in Cell Biology. 1999;11(2):211–218. doi: 10.1016/s0955-0674(99)80028-3. [DOI] [PubMed] [Google Scholar]
- 24.Sugden PH, Clerk A. Oxidative stress and growth-regulating intracellular signaling pathways in cardiac myocytes. Antioxidants and Redox Signaling. 2006;8(11-12):2111–2124. doi: 10.1089/ars.2006.8.2111. [DOI] [PubMed] [Google Scholar]
- 25.Capodici C, Pillinger MH, Han G, Philips MR, Weissmann G. Integrin-dependent homotypic adhesion of neutrophils. Arachidonic acid activates Raf-1/Mek/Erk via a 5-lipoxygenase-dependent pathway. Journal of Clinical Investigation. 1998;102(1):165–175. doi: 10.1172/JCI592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang ZQ, Wu DC, Huang FP, Yang GY. Inhibition of MEK/ERK 1/2 pathway reduces pro-inflammatory cytokine interleukin-1 expression in focal cerebral ischemia. Brain Research. 2004;996(1):55–66. doi: 10.1016/j.brainres.2003.09.074. [DOI] [PubMed] [Google Scholar]
- 27.Roux PP, Blenis J. ERK and p38 MAPK-activated protein kinases: a family of protein kinases with diverse biological functions. Microbiology and Molecular Biology Reviews. 2004;68(2):320–344. doi: 10.1128/MMBR.68.2.320-344.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y, Wang J, Yuan L, Zhou L, Jia X, Tan X. Interaction of the main components from the traditional Chinese drug pair Chaihu-Shaoyao based on rat intestinal absorption. Molecules. 2011;16(11):9600–9610. doi: 10.3390/molecules16119600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu JY, Lee KF, Sze CW, et al. Intestinal absorption and bioavailability of traditional Chinese medicines: a review of recent experimental progress and implication for quality control. Journal of Pharmacy and Pharmacology. 2013;65(5):621–633. doi: 10.1111/j.2042-7158.2012.01608.x. [DOI] [PubMed] [Google Scholar]
- 30.Kutala VK, Khan M, Mandal R, et al. Attenuation of myocardial ischemia-reperfusion injury by trimetazidine derivatives functionalized with antioxidant properties. Journal of Pharmacology and Experimental Therapeutics. 2006;317(3):921–928. doi: 10.1124/jpet.105.100834. [DOI] [PubMed] [Google Scholar]
- 31.Dedkova EN, Seidlmayer LK, Blatter LA. Mitochondria-mediated cardioprotection by trimetazidine in rabbit heart failure. Journal of Molecular and Cellular Cardiology. 2013;59:41–54. doi: 10.1016/j.yjmcc.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]


