Short abstract
Events that expose people to radiation are rare, but the threat of radiation injury is increasing. Doctors should know how to recognise and manage suspected exposure or contamination
After the attacks of 11 September 2001, use of sources of radiation by terrorists with the potential to cause human damage has become a greater threat.1-4 Various professionals have discussed whether malevolent use of these sources could result in radiation sickness or radiation injuries on a large scale and the possible results.5-7 Radiation sickness is the acute or delayed consequences of exposure of the whole body or a large part to high doses of ionising radiation capable of causing a set of non-specific clinical symptoms and haematological changes. Radiation injury is the acute or delayed consequences of exposure of a small part of the body to high doses of ionising radiation capable of causing burns or other localised organ pathology—for example, cataract, hypothyreosis, and pneumonia.
Responses to recent incidents involving radiation indicate that most general practitioners are uncertain about the health consequences of exposure to ionising radiation and the medical management of exposed patients.8-10
Clinical manifestations of pathological changes depend on the size of the exposed area of the body. The severity of symptoms depends on the absorbed dose of radiation by the exposed area of the body.
The medical community needs to consider this issue because of the need for emergency medical care after a possible use of radionuclear materials by terrorists.11,12
Medical education and postgraduate training programmes for primary care doctors worldwide seem to lack the appropriate information about radiation incidents as regards recognition, differential diagnosis, and first medical response.7,13,14 We aim to advise on the basic medical management of radiation sickness and radiation injuries, and to draw attention to information and training related to early recognition of and medical response to radiation accidents and radionuclear threats.
Methods
We collected information for this review from our own experience in teaching radiation emergency medicine at national and international training workshops and consulting and treating patients with radiation sickness or radiation injuries, discussions with other experts, reviewing publications of the World Health Organization and International Atomic Energy Agency,8-10,15-17 and from Medline searches using the terms “nuclear terrorism”, “radiological terrorism”, “radionuclear threat”, “radiation accidents”, “radiation incidents”, “radiation sickness”, “radiation injury”, “contamination”, “medical response”, and “medical management”.
Summary points
Doctors' unfamiliarity with radiation injuries means they are often misdiagnosed; medical training in this subject needs urgent improvement
Doctors should be aware of the acute and delayed effects of exposure to ionising radiation
Nausea, vomiting, diarrhoea, headache, weakness, and lymphocytopenia may indicate exposure to radiation
The higher the radiation dose to the whole body, the faster and more severe the reduction of blood cell counts
Clinical signs typical for radiation injury of the skin include erythema, depilation, dry and moist desquamation, blistering, ulceration, and necrosis
Doctors need up to date contact information about competent health and radiation protection services
Global statistics and main causes of radiation accidents
Radiation incidents—unintentional and unexpected events—are rare. To date, about 3000 people worldwide have been inadvertently exposed to whole body doses exceeding the average annual radiation dose from natural sources by one hundred times. At this dose, however, no clinical symptoms or signs can be observed. Symptoms appear at only 2-4 times higher doses of acute exposure to ionising radiation to a large part of the body.
Box 1: Radionuclear threats19,20
Explosion of “dirty bombs”—that is, conventional explosives bound with radioactive materials—may cause radiation sickness and radiation injuries to a lesser scale of several orders of magnitude than a nuclear bomb.1,6 Nevertheless, they might cause hundreds of deaths or severe injuries and environmental contamination by radioactive materials in a limited area
Dispersal of high activity radioactive materials into air conditioning, underground railways, drinking water, or food supplies.2,3 This method is most likely to cause damage to humans in large numbers and would be almost impossible to detect or stop immediately unless radiation in air, water, and food supplies is monitored continuously
Direct attacks on nuclear power plants or nuclear fuel reprocessing facilities are unlikely as they are well secured2,20
Use of nuclear weapons is unlikely but cannot be ruled out4,19
Locating a highly radioactive source in heavily populated places is possible but not feasible
Between 1944 and 2002, 134 deaths were registered from 420 incidents worldwide, including 28 radiation deaths among reactor operators and fire fighters in the Chernobyl disaster of 1986.18
Almost half of the radiation incidents occurred in industry, mainly in non-destructive material testing.10,12 Only a tenth of incidents were related to the diagnostic and therapeutic applications of radiation sources. Nevertheless, nearly half of all fatal exposures happened as a result of calibration errors in equipment used for medical exposures or because of insecure storage of spent sources for radiotherapy.
No cases of terrorist action involing radioactive materials are known. Nevertheless, their possibility has to be taken into account and all possible precautionary measures are needed to prevent them (box 1).
Typical exposure scenario of recent radiation accidents
As the ionising radiation cannot be detected by human senses, affected people are usually unaware of their exposure. A typical scenario seen repeatedly in recent incidents was people finding shiny metallic objects, actually small radiation sources. The unrecognised sources were often put into pockets, causing severe radiation burns.9,21 Frequently these sources were taken home and the whole family or members of the same residence were exposed. Often the people concerned were collectors of scrap metal or worked as scrap metal dealers.10,12,22
Radiation sickness
Early clinical symptoms
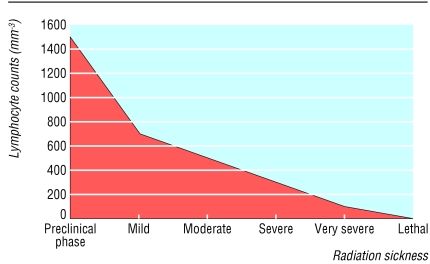
Symptoms of radiation sickness evolve over time in distinct phases. The duration of each phase and the time of its onset is inversely proportional to the dose.6,15 An initial prodromal phase, with symptoms such as nausea, vomiting, weakness and fatigue, typically develops in hours to days after exposure of the whole body to radiation exceeding 1 Gy. The circulating lymphocytes are one of the most radiosensitive cell lines that offer a useful laboratory tool to determine the severity of the radiation sickness early in observation. After whole body exposure above 0.5 Gy the rapid fall in lymphocyte number starts within hours. Their depletion is proportional to the dose between 1 and 10 Gy (corresponding to mild to lethal acute radiation sickness) (fig 1). Fever and diarrhoea may appear at doses above 4 Gy.15 After a latent phase, a period of the obvious illness follows, characterised by infection, bleeding (frequent gingival bleeding, epistaxis, petechia), and gastrointestinal symptoms. Granulocytes have two transient peaks (see fig A on bmj.com) after a mild to severe degree of exposure (2-5 Gy). The first peak (on the first day) is due to their demargination, and the second peak (10-15 days later) is due to release of differentiated granulocytes. If only granulocytes are counted on these days the dose and severity of acute radiation sickness may be underestimated. Counts of lymphocytes, granulocytes, and thrombocytes have to be assessed in parallel (box 2).
Fig 1.
Lymphocyte counts decrease within the first week after an acute whole body exposure, depending on the absorbed dose to the body and the consequent severity of (acute) radiation sickness
The risk of sepsis is the highest between the 25th and 35th days, due to deficiency in cellular immunity (see fig B on bmj.com). Because of delayed recognition of radiation sickness, sepsis was the primary cause of death in some recent radiation accidents (for example, of three Thai and two Egyptian patients in 2000). If the patient consults the doctor a few hours after a presumed or verified radiation exposure, blood counts can be performed every four to six hours on the first day and then repeated daily for about a month to facilitate the differential diagnosis and follow up the efficacy of treatment.
Box 2: Early clinical symptoms of fatal radiation exposure to the whole body (>10 Gy)
Nausea and persistent vomiting within minutes
Dizziness or transitory loss of consciousness within minutes
Explosive bloody diarrhoea within hours or days, for days
High fever (up to 41°C)
Hypotension
Erythema within hours (more expressed on uncovered body parts)
Neurological signs, disorientation, apathy, lethargy
Differential diagnosis
When a patient presents with malaise, nausea, and vomiting with increasing and continuing fatigue, the doctor usually considers food poisoning or a disease of infectious origin. It is important to find out similar cases in the family or at work and clarify any travel, accounting for the incubation of a likely infectious disease, as well as alimentary or work related toxicological exposures. Radioactive contamination of drinking water supplies by terrorists would lead to similar symptoms in large numbers of people in a well defined area.
Patients with work related or family links who have shown similar symptoms of prolonged malaise and fatigue, especially accompanied with simultaneous haematological signs of expressed neutropenia and thrombocytopenia, should alert the doctor to the possibility of a radiation exposure.
Additional educational resources
Training materials on CD Roms
International Atomic Energy Agency and World Health Organization. Medical preparedness and response. training for radiation emergency preparedness and response. Vienna: IAEA, 2002 (Educational material, EPR-MEDICAL/T-2002/CD)
World Health Organization. Health aspects of biological, chemical and radionuclear threats. Geneva: WHO, 2003
Armed Forces Radiobiology Research Institute. Medical effects of ionising radiation. Bethesda: AFRRI, 1999
Websites
www.who.int/ionizing_radiation/en—this WHO/RAD (Radiation and Environmental Health) website provides information on WHO/REMPAN (Radiation Emergency Medical Preparedness and Assistance Network) and includes fact sheets (prepared in 2003) titled Radiological Dispersion Device (Dirty Bomb) and Health Protection Guidance in the Event of a Nuclear Weapon Explosion
www-rasanet.iaea.org/programme/emergency/technicalproducts.htm#medical—for documents from the International Atomic Energy Agency related to radiation emergency medical preparedness and response
www.afrri.usuhs.mil—for the Medical Management of Radiation Casualties Handbook
www.orau.gov/reacts—for information on training courses on handling of radiation incidents by emergency responders
Radiation injury of the skin
Erythema, oedema with pain, blistering, dry and wet desquamation (fig 2), ulceration, necrosis or depilation only in the exposed area of the body. Their time of appearance and severity depend on dose.
Fig 2.


Early blister with erythema of large inflammatory halo on rear side of right thigh on day 2, and an extended superficial erosion surrounded by large dusky inflammation on day 9 after 6.5 hour local exposure to iridium-192 source of 0.96 TBq (26 Ci)23
Local skin injuries evolve slowly (usually in weeks to months) and may become painful and difficult to treat with conservative methods. In the absence of history of a skin disease or any other specific information relating its origin to a thermal burn, an insect bite, chemical exposure or allergens, a badly healing dermatological lesion which has been unsuccessfully treated with conservative methods for a substantial period of time (or even with surgery), may be a sign of radiation injury. This should lead a doctor to consider the possibility of a local radiation exposure that could have occurred a few weeks or even months before.
Clinical suspicion
Local radiation injury or radiation sickness should be suspected if the patient:
Describes circumstances that might have led to exposure—for example, they saw but did not recognise the “radiation danger” sign on a package or container (see fig C on bmj.com)
Experiences nausea and vomiting, especially if accompanied with headache, fatigue, anorexia, diarrhoea, erythema, or other skin lesions that are not explained by other causes.
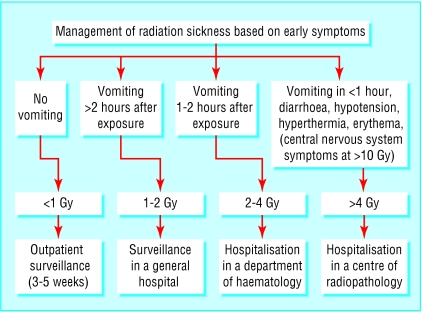
A patient with a presumed exposure may have changes in blood counts and skin lesions within 1-4 weeks, known to occur in a time sequence, depending inversely on the radiation dose (fig 3 and table A on bmj.com).
Fig 3.
Management of radiation sickness at different levels of medical care depending on the appearance of early symptoms and the estimated radiation dose to the whole body
Early management of contaminated patients
Before offering any care for victims use strict isolation precautions to protect yourself from contamination, dispose of contaminants, and control the spread of radioactivity.15,16 Immediately order complete and differential blood counts to assess severity of exposure. Swab nostrils and oral cavity and wounds to detect any internal contamination. Remove or change the patient's contaminated clothing. Decontaminate the patient with showers and by thoroughly washing open body surfaces. Collect and label urine and faeces of patients who have possible internal radioactive contamination. In case of risk of inhalation of radioactive iodine (after a nuclear incident) urgently seek advice from the health authority or radiation protection authority for use of stable iodine tablets.20
Strategy and safety aspects of the medical response to radiation injuries
If the patient involved in a radiation accident or a terrorist action with radioactive materials is in a life-threatening condition, save the patient's life, and stabilise his or her condition,6,11,15 and decontaminate (that is, use or request procedures13,16 to remove radioactive materials from the patient's body later).
Providing care for a patient in a life threatening condition always has priority over decontamination from radioactive materials or those actions required for the safety of others involved (medical staff, emergency rescue teams) or related to the wider public and environment.
If the contaminated patient is not in a life threatening condition, consult a radiation specialist (recommended or assigned by the health authority), decontaminate first, take blood for differential diagnosis, and then treat the patient as required.
Note that radiation alone does not produce immediate life threatening symptoms, and a person exposed to radiation or contaminated with radioactive materials does not present a direct health risk to the doctor.
General practitioners should have the necessary telephone numbers readily available. Telephone numbers of the relevant health authority and radiation protection service for consultation in emergency radiation medicine or verification of the suspected radiation sickness, injury, or contamination should be updated regularly.
How would the United Kingdom cope?
Worldwide, medical use of radiation and poor or absent control of industrial sources of radiation are still the most likely causes of incidental exposure to ionising radiation affecting workers and the public. National legislation on the registration of radioactive sources, and better control and contingency planning, have considerably reduced the risk of such exposure in the United Kingdom. This is not to say that such incidents cannot still occur in the United Kingdom, and, coupled with the increased probability that terrorists might use radioactive materials, these risks certainly make this article relevant here.
In the United Kingdom two main kinds of possible terrorist activity might expose the public to radiation. Firstly, terrorists might trigger events that seem not to be deliberate, for which site-specific or transport emergency plans already exist and are in the public domain. Secondly, terrorists might release radioactive material, intending to cause public alarm and panic as well as irradiation. This might include “dirty bombs” that disperse radioactive material by using conventional explosives or devices that release radioactivity to the environment over time and cause insidious irradiation. In the event of slow release of radioactivity it would be particularly important that medical personnel could recognise and diagnose the early effects of radiation.
In England and Wales, the Health Protection Agency provides advice on this and other aspects of major health emergencies to the Department of Health, NHS, and regional directors of public health (www.hpa.org.uk). The Scottish Executive provides similar guidance (www.show.scot.nhs.uk/emergencyplanning/Documents/annex_j.htm) that reflects the findings of recent Scottish consultation on increasing general practitioners' recognition and reporting of unusual and unexplained illnesses. The Department of Health's website also provides material on emergency plans and responses for major incidents (www.dh.gov.uk/PolicyAndGuidance/EmergencyPlanning).
In the event of such an incident, health professionals will be expected to advise the public. The United Kingdom has one of the longest established and best developed systems of public protection after radiation incidents, including early countermeasures (nrpb.org/radiation_incidents/advice.htm). These plans are not well known by health professionals, however, who are therefore poorly placed to advise their patients. Some parts of the world, such as Russia and Japan, have highly specialised dedicated organisations for the treatment of radiation injury. The United Kingdom will rely on its general NHS resources. All NHS bodies, including primary care trusts, now have to have plans that comply with the document Planning for Major Incidents: the NHS Guidance (HSC 1998/197), which was updated in 2002. In addition to knowledge on managing radiation injury, the NHS units designated to receive contaminated or irradiated casualties need simple guidance on expected types and numbers of injury.
Chris J Kalman consultant in occupational medicine, Lanarkshire Acute Hospitals NHS Trust, Coatbridge ML5 4TD
(chris.kalman@laht.scot.nhs.uk)
Supplementary Material
 Three figures, a table, and a box giving further details are on bmj.com
Three figures, a table, and a box giving further details are on bmj.com
We thank Mayer Zaharia (Instituto de Enfermedades Neoplásicas, Lima, Peru) for the photos of local radiation injuries of the Peruvian radiological accident victim of 1999.
Contributors: All authors searched and reviewed references and prepared and revised the manuscript. IT and KV initiated and drafted the paper. BG and IT prepared the figures. GS contributed to the summary and the introduction. IT is guarantor.
Funding: None.
Competing interests: None declared.
References
- 1.Helfand I, Forrow L, Tiwari J. Nuclear terrorism. BMJ 2002;324: 356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timins JK, Lipoti JA. Radiological terrorism. N J Med 2003;100: 14-21. [PubMed] [Google Scholar]
- 3.Yehezkelli Y, Dushnitsky T, Hourvitz A. Radiation terrorism: the medical challenge. Isr Med Assoc J 2002;4: 530-4. [PubMed] [Google Scholar]
- 4.Kilpatrick JJ. Nuclear attacks. RN. 2002;65: 46-51. [PubMed] [Google Scholar]
- 5.Gonzalez AJ. Securing radioactive sources against terrorism: an international perspective. Health Phys Soc Newsl 2002;30: 3-5. [Google Scholar]
- 6.Mettler FA, Voelz GL. Current concepts: major radiation exposure: what to expect and how to respond. N Engl J Med 2002;346: 1554-61. [DOI] [PubMed] [Google Scholar]
- 7.Turai I, Veress K, Günalp B, Souchkevitch G. Major radiation exposure. N Engl J Med 2002;347: 946. [PubMed] [Google Scholar]
- 8.Meineke V, van Beuningen D, Sohns T, Fliedner TM. Medical management principles for radiation accidents. Mil Med 2003;168: 219-22. [PubMed] [Google Scholar]
- 9.International Atomic Energy Agency and World Health Organization. Follow-up of delayed health consequences of acute accidental radiation exposure: lessons to be learned from their medical management. Vienna: IAEA, 2002: 129. (IAEA-TecDoc-1300.)
- 10.Turai I, Crick M, Ortiz-Lopez P, Nogueira de Oliveira C, Wrixon AD. Response to radiological accidents: the role of the International Atomic Energy Agency. Radioprot 2001;36: 459-75. [Google Scholar]
- 11.Leikin JB, McFee RB, Walter FG, Edsall K. A primer for nuclear terrorism. Dis Mon 2003;49: 485-516. [DOI] [PubMed] [Google Scholar]
- 12.Turai I, Veress K. Radiation accidents: occurrence, types, consequences, medical management, and the lessons to be learned. Centr Eur J Occup Envir Med 2001;7: 3-14. [Google Scholar]
- 13.Gower-Thomas K, Lewis MH, Shiralkar S, Snow M, Galland RB, Rennie A. Doctors' knowledge of radiation exposure is deficient. BMJ 2002;324: 919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turai I, Veress K. Experience gained in teaching of, and training in radiohygiene. Népegészségügy 1993;74: 203-6. (In Hungarian with English abstract and headings.) [Google Scholar]
- 15.International Atomic Energy Agency and World Health Organization. Diagnosis and treatment of radiation injuries. Vienna: IAEA, 1998: 49. (Safety Reports Series No 2.)
- 16.International Atomic Energy Agency. Assessment and treatment of external and internal radionuclide contamination. Vienna: IAEA, 1996: 62. (IAEATecDoc-869.)
- 17.International Atomic Energy Agency and World Health Organization. How to recognise and initially respond to an accidental radiation injury [leaflet and poster]. Vienna: IAEA, 2000.
- 18.Ricks R. REAC/TS Registry of radiation accidents, 1944-2000. Oak Ridge: REAC/TS, 2001.
- 19.Hogan DE, Kellison T. Nuclear terrorism. Am J Med Sci 2002;323: 341-9. [DOI] [PubMed] [Google Scholar]
- 20.Souchkevitch G, Turai I. Radiation emergency response. Geneva: World Health Organization, 2002: 27. (Internal guidance WHO/PHE/RAD/02.06.)
- 21.Cosset JM, Jikia D, Peter RU, Souchkevitch G, Turai I. Health consequences among the Lilo accident victims; medical monitoring in Georgia, France and Germany. Vienna: IAEA, 2002, 49-55. (IAEA TecDoc 1300.)
- 22.Turai I, Günalp B, Ergen K. The Istanbul accident: a case report of the mixed (acute and protracted) radiation exposure: main consequences and the medical management. In: Fliedner T, Feinendegen LE, Hopewell JW, eds. Chronic irradiation: tolerance and failure in complex biological systems. Br J Radiol 2002;26(suppl): S80-2. [Google Scholar]
- 23.Zaharia M, Pinillos-Ashton L, Picon C, Heredia A, Berger ME, Goans RE, et al. Medical follow-up of the localized radiation injuries of the victim of the Peruvian radiation accident. Vienna: IAEA, 2002: 57-65. (IAEA TecDoc 1300.)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.