Abstract
Objectives
To examine the relationship between the co-occurrence of mental health and substance use problems and socioeconomic status (SES).
Study design
A prospective longitudinal study of 808 males and females followed to age 30.
Methods
Survey data were used to derive latent classes (profiles) of mental health (depression, anxiety) and substance use (alcohol, nicotine, and marijuana [cannabis]) problems at age 27. Analyses examined the associations of these profiles with earlier educational attainment (high school diploma) and indicators of SES at age 30.
Results
Latent Class Analysis produced four profiles: a low disorder symptoms group, a licit substance use disorder symptoms group (alcohol and nicotine), a mental health disorder symptoms group, and a comorbid group. Earning a high school diploma by age 21 decreased the odds of belonging to the comorbid group or the licit substance use disorder symptoms group when compared to the low disorder symptoms group. These disorder profiles also were found to adversely impact subsequent adult SES. The adverse impact was more evident in income maintenance and wealth accumulation by age 30 than market or nonmarket labor force participation.
Conclusions
Earning a high school diploma lessens the risk of co-occurring mental health and substance use problems which contribute to economic instability in young adulthood. Findings underscore the importance of public health programs to reduce the incidence of mental health and substance use problems and their associated high costs to individuals and to society.
Keywords: Health inequalities, socioeconomic status, comorbidity, mental health, substance use disorder
Introduction
Research evidence shows an inverse association between socioeconomic status (SES) and adult mental health1-4 and substance use problems.5-7 Why SES is related to mental health and substance use problems is unclear. However, researchers offer two compelling hypotheses.1, 8-10 One hypothesis, related to social causation, posits that lower SES is a risk factor for mental health and substance use problems. In contrast, a social selection hypothesis suggests that preexisting psychiatric problems impair ones' ability to attain or retain higher SES status.
These hypotheses have been subjected to empirical tests.11-13 Yet, there have been very few studies of the relationship between SES and the co-occurrence of mental health and substance use problems, although the co-occurrence of mental health and substance use problems has been well documented.14-16 For example, in a U.S. population study, 28.3% of those with substance use problems reported having mental health problems (depression/anxiety) in the past year, compared to 8.7% of those without substance use problems.15 Given the debilitating and costly consequences of comorbid disorders,17, 18 it is important to understand their interrelationships and the SES predictors and consequences of their co-occurrence.
Prior studies also suggest that failure to consider the complex constellation of mental health and substance use problems together can limit our knowledge about their association with SES. Kessler et al.2 found that lower education was associated with increased comorbid mental health and substance use problems. However, education was not associated with mental health disorders in the absence of substance use. While this study underscores the importance of considering the co-occurrence of mental health and substance use problems in studies examining social causation, the study, being cross-sectional, does not help explain how variables in the analysis are temporally related.
Two prior studies have investigated social selection in the context of co-occurrence of mental health and substance use problems, and their findings are mixed. Jofre-Bonet et al.19 reported that men who smoked and had mental health problems experienced further reduction in wages relative to those who only smoked or only had mental health problems. In contrast, Vida et al.20 reported that there were no statistically significant differences in labor force participation for individuals with both depression and drug abuse problems compared to those only with depression.
There has been relatively little research on the impact of disorder co-occurrence on SES indicators other than labor force participation and labor income. For example, wealth -- often represented by home and/or car ownership,12 which is known to capture a unique dimension of socioeconomic status11-13 -- has not yet been fully examined in the health inequality literature.11, 12
The present study seeks to examine social causation and social selection hypotheses with particular attention to the interrelationships of mental health and substance use problems. Substance use problems include licit substances, such as alcohol and nicotine, as well as illicit substances, such as marijuana (cannabis). Specifically, we investigate the association between educational attainment at age 21 and different constellations of mental health and substance use problems at age 27, using a prospective, longitudinal design. We focus specifically on education (earning a high school diploma) as a predictor, which is a developmentally appropriate and important indicator of socioeconomic status in young adulthood when many young adults experience constant changes in other SES indicators such as income.10, 21, 22 We also investigate the association between the co-occurrence of mental health and substance use problems at age 27 and multiple SES indicators at age 30, including market labor force participation and labor income, as well as nonmarket household labor participation (conceptualized as constructive engagement), and wealth. To our knowledge, this is the first study to examine the impact of the co-occurrence of mental health and substance use problems on nonmarket household labor participation and wealth using prospective longitudinal data. These data, which span young adulthood to age 30, provide an opportunity to examine both a developmentally appropriate socioeconomic predictor, namely educational attainment, as well as the socioeconomic consequences in adulthood of mental health and substance use problems.23
Methods
Sample
Data are from the Seattle Social Development Project (SSDP), a theory-driven panel study examining an extensive range of developmental outcomes including socioeconomic status, mental health, and substance use. In September 1985, 18 Seattle elementary schools were identified that overrepresented students drawn from disadvantaged neighborhoods. The study population included all fifth-grade students in these schools (N = 1053). From this population, 808 students (77%) consented to participate in the longitudinal study and constitute the SSDP sample (for more information, see Hawkins et al.24). Sample retention rates have been consistently high (91% at age 30). The study was approved by the Human Subjects Review Committee at the University of Washington.
Measures
Mental health and substance use disorder latent class indicators (age 27)
At age 27, major depressive symptoms, general anxiety disorder symptoms, alcohol use disorder symptoms, nicotine dependence symptoms, and marijuana (cannabis) use disorder symptoms were measured using the Diagnostic Interview Schedule (DIS),25 which assesses disorder symptoms based on the DSM-IV.26 Measures summed the number of symptoms reported for each mental health and substance use disorder in the past year at age 27. In line with earlier publications,14, 27, 28 our mental health and substance use variables were defined as a count of relevant problems rather than the presence or absence of a disorder diagnosis, allowing for more variability in the scaled responses.
Educational attainment: High school diploma (age 21)
Educational attainment was used as an indicator of SES at age 21; those who graduated from high school were coded 1, and those who did not graduate were coded 0. Educational attainment has been documented as an important marker in adulthood, which is highly predictive of health.21 It has been documented that the association between education and health is not linear, indicating that every year of additional schooling does not necessarily result in a monotonic increase in improved health. Rather, the impacts of education on health become evident when one completes a degree.29 Developmentally, the majority of participants at the age 21 survey had not completed their postsecondary education yet. High school completion has been considered to be an important marker in one's educational trajectory, which has been known to have enduring impacts on one's life.30, 31 It is highly associated with one's economic stability, as it is a minimum requirement for postsecondary education and many jobs.32
Adult socioeconomic status (age 30)
Three separate measures assessed different dimensions of adult socioeconomic status. Constructive engagement, a broad measure of labor force participation, was created by dividing a sum of the average number of hours per week involved in school and/or work by 10. Work included not only direct labor force participation but also nonmarket household labor participation (e.g., homemaker).24, 33Household income was defined as total household income level (in units of $1,000) divided by the total number of household members at age 30 to adjust for a household size and thus more accurately represent an individual's economic well-being.34 Household income was transformed using a natural logarithm to address its skewness. A measure of wealth was based on a sum of 5 Yes/No items, including (a) have personal checking account, (b) have IRA or pension plan, (c) own home or condo, (d) own a car, and (e) have savings account. These 5 indicators were intended to capture aspects of wealth established in earlier studies. 12, 13, 35, 36
Covariates
Covariates included baseline symptoms of psychopathology as measured by the internalizing (affective disorder and anxiety problems) and externalizing (attention deficit and hyperactivity, oppositional defiant, and conduct problems) scales of the Achenbach Child Behavior Checklist completed by teachers at ages 10 - 12;37, 38 baseline use of alcohol, tobacco and marijuana (cannabis) measured at ages 13 - 14 (not available earlier than age 13); childhood low-income status as indicated by students' eligibility for the school free lunch program at ages 10 - 12 (low income = 1); participants' gender (male = 1); 3 dummy variables representing each of 3 ethnic minority groups (African American, Asian American, and Native American, with Caucasian American as the reference group); and 2 dummy variables representing 2 intervention conditionsa (the full intervention group and the other intervention groups, with control group as the reference group).
Descriptive statistics of the study variables are shown in Table 1.
Table 1.
Descriptive statistics of the study variables.
| Variable (metric or range) | Mean/% | SD |
|---|---|---|
| Educational attainment, age 21 High school graduation | ||
| High school graduation | ||
| No (0) | 18.70 | -- |
| Yes (1) | 81.30 | -- |
| Mental health and substance use latent class indicators, age 27 | ||
| Major depression symptoms (0 - 9) | 1.50 | 2.96 |
| General anxiety symptoms (0 - 6) | 1.97 | 1.94 |
| Alcohol abuse and dependence symptoms (0 - 11) | 0.92 | 1.84 |
| Nicotine dependence symptoms (0 - 7) | 0.81 | 1.44 |
| Marijuana(cannabis) abuse and dependence symptoms (0 - 10) | 0.38 | 1.23 |
| Later adult socioeconomic status, age 30 | ||
| Constructive engagement (0 - 4) | 3.36 | 1.13 |
| Household income (in thousands) | 26.99 | 23.21 |
| Wealth (0 - 5) | 3.33 | 1.53 |
| Covariates | ||
| Baseline symptoms of psychopathology, ages 10 – 12 | ||
| Internalizing problems (z-scores), ages 10-12 | 0.01 | 0.49 |
| Externalizing behavior problems (z-scores), ages 10-12 | 0.01 | 0.63 |
| Baseline substance use, ages 13 - 14 | 0.00 | 0.79 |
| Childhood low-income status, ages 10 – 12 | 48.90 | -- |
| Gender (Male =1) | 51.00 | -- |
| Ethnic Group | ||
| Caucasian American | 47.20 | -- |
| African American | 25.60 | -- |
| Native American | 5.30 | -- |
| Asian American | 21.90 | -- |
| Intervention | ||
| Full intervention | 19.40 | -- |
| Other interventions | 53.23 | -- |
| Control | 27.36 | -- |
Analysis
We carried out Latent Class Analysis (LCA) of the multivariate co-occurrence of mental health and substance use problems using Mplus 5.2.42 Latent Class Analysis is a statistical tool to identify subgroups of individuals who share similar profiles in combinations of relevant indicators, thereby allowing examination of relationships between the subgroups and predictors and/or distal outcomes (see43-45 for more details about LCA). The 5 mental health and substance use disorder measures described above were included as indicators of the resulting categorical latent variable.
After choosing the optimal unconditional class solution based on multiple model fit statistics (see 44, 46-49 for more details about fit statistics), we re-estimated the chosen model, regressing latent class on educational attainment at age 21 (the main predictor) and all the covariates described above in a multinomial logistic regression. We then regressed each indicator of socioeconomic status at age 30 on the latent subgroups as well as the age 21 educational attainment predictor and all the covariates. The mean difference in each indicator of age 30 socioeconomic status across the latent class subgroups was tested using a Wald test.50 Of the original sample of 808, 83% had available data for the final analysis. Full-information maximum likelihood (FIML) estimation in Mplus was used to account for incomplete data.51-53
Of note, in earlier follow-up analyses of the SSDP study,24, 39, 40 we extensively examined whether there is a need to address potential cluster issues related to complex sampling design. As students moved along in their schooling, the unit of cluster assignment consisted of the series of classrooms to which students were assigned rather than a single classroom or school. We examined which subgroups of children shared the same sequence of classroom and/or school assignment, and identified 169 different sequences. This resulted in an average cluster size of 3.8, with an average ICC of .035 across dependent variables. Muthén and Satorra conducted a Monte Carlo study related to the clustering issue in general. The smallest ICC they examined was .05 and the smallest cluster size was 7. They concluded that “[f]or the smallest ICC and cluster size combination, the bias can be considered negligible”.41(p.303) Given that our cluster size and ICC value are smaller than the smallest corresponding values tested in Muthén and Satorra's study, we concluded that potential bias in standard errors is negligible in the present study and thus conducted analyses at the individual level.
Results
Profiles of mental health and substance use problems
In general, fit indices suggested that the model fit improved through the 4-class solution. As shown in Table 2, the model continued to improve from the 1 class through the 4-class solution (indicated by decreasing BIC and SABIC and statistical significance of the Lo-Mendell-Rubin adjusted likelihood ratio test and the bootstrapped likelihood ratio test). When an other class was added to the 4-class model, all the fit statistics worsened, and both likelihood ratio tests did not converge properly. These results indicate no improvement in model fit for the 5-class model compared to the 4-class model.48
Table 2.
Fit indices for latent class models, with the selected four-class model indicated by shading.
| Number of Classes | BICa | SABIC | Log likelihood | Number of parameters | Entropy (average class probabilities) | Adjusted LRT b,d (p-value) | BLRT c,d (p-value) |
|---|---|---|---|---|---|---|---|
| 1-class | 13529.00 | 13513.12 | -6747.96 | 5 | n/a | n/a | n/a |
| 2-class | 10462.49 | 10427.56 | -5194.86 | 11 | .95 (.99,.98) | < .001 | < .001 |
| 3-class | 9701.27 | 9647.29 | -4794.40 | 17 | .92 (.99,.97,.95) | < .001 | < .001 |
| 4-class | 9283.82 | 9210.79 | -4565.83 | 23 | .93 (.97,.97,.96,.95) | < .01 | < .001 |
| 5-class | 9476.78 | 9400.57 | -4659.00 | 24 | .84 (.82,.9,.87,1,.9) | e e | e e |
Note: Decrease greater than 6 indicates “strong” improvement in fit 70
Lo-Mendell-Rubin Adjusted Likelihood Ratio Test
Parametric Bootstrapped Likelihood Ratio Test
Lower p-value indicates that the k-class model is preferable over the k-1 class model
Not properly converged
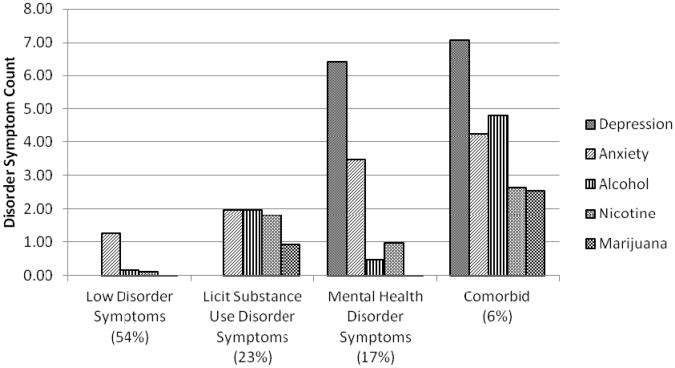
Figure 1 shows the average disorder symptoms of members of each latent profile group for the unconditional 4-class model. A large low disorder symptoms group (54%) showed virtually no symptoms of mental health or substance use problems other than a relatively low level of anxiety (mean = 1.26). A licit substance use disorder symptoms group (23%) mainly had alcohol disorder symptoms along with nicotine dependence disorder symptoms, relative to the other 3 subgroups. A mental health disorder symptoms group (17%) showed relatively high levels of depression symptoms and anxiety symptoms. Finally, a relatively small comorbid group (6%) showed elevated levels of all 5 mental health and substance use indicators. Details of these latent classes are also described in an earlier published study.54
Figure 1.
Profiles of mental health and substance use group.
Educational attainment at age 21, the latent class subgroups at age 27, and socioeconomic status at age 30
Initial regression results indicated that having a high school diploma significantly decreased the odds of belonging to any of the 3 mental health and/or substance use subgroups relative to the low disorder symptoms group. Relative to the low disorder symptom group, those with a high school diploma at age 21 had lower odds of belonging to the comorbid group (OR = .17, 95% CI = .08, .39), the mental health disorder symptoms group (OR = .44, 95% CI = .25, .76), or the licit substance use disorder symptoms group (OR = .45, 95% CI = .25, .79).
It is possible that baseline symptoms of psychopathology and earlier substance use may influence both educational attainment at age 21 and the latent class subgroups. Thus, the next set of analyses examined whether having a high school diploma predicted the 3 mental health and/or substance use subgroups above and beyond the baseline symptoms of psychopathology and earlier substance use. As shown in Table 3, results indicated that having a high school diploma at age 21 significantly decreased the odds of belonging to the comorbid group or the licit substance use group relative to the low disorder group, after controlling for the baseline symptoms of psychopathology and substance use.
Table 3.
Summary of multivariable multinomial logistic regression predicting the mental health and substance use latent classes.
| Variable | Mental health and substance use latent classes | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Licit substance use disorder symptoms a | Mental healthdisorder symptoms a | Comorbid a | ||||
|
|
|
|
||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Educational attainment, age 21 | ||||||
| High school graduation (Yes = 1) | 0.49 | (0.25, 0.96) | 0.60 | (0.32, 1.14) | 0.26 | (0.11, 0.62) |
| Baseline symptoms of psychopathology, ages 10 - 12 | ||||||
| Internalizing problems | 0.65 | (0.37, 1.12) | 1.25 | (0.80, 1.97) | 0.62 | (0.17, 2.24) |
| Externalizing behavior problems | 1.40 | (0.84, 2.32) | 1.40 | (0.88, 2.23) | 1.59 | (0.81, 3.12) |
| Baseline substance use, ages 13 - 14 | 1.21 | (0.86, 1.70) | 0.90 | (0.66, 1.22) | 1.29 | (0.87, 1.91) |
| Childhood low-income status (low income = 1) | 0.73 | (0.45, 1.21) | 1.78 | (1.06, 2.98) | 0.96 | (0.42, 2.18) |
| Gender (Male = 1) | 2.86 | (1.83, 4.48) | 0.96 | (0.60, 1.53) | 1.89 | (0.85, 4.22) |
| Ethnic minority group b | ||||||
| African American | 0.77 | (0.43, 1.38) | 0.68 | (0.36, 1.29) | 1.87 | (0.70, 5.00) |
| Native American | 1.53 | (0.54, 4.29) | 1.62 | (0.63, 4.14) | 2.88 | (0.78, 10.68) |
| Asian American | 0.68 | (0.37, 1.22) | 0.82 | (0.44, 1.53) | 0.21 | (0.00, 9.42) |
| Intervention status c | ||||||
| Full intervention group | 0.98 | (0.53, 1.80) | 0.83 | (0.40, 1.70) | 0.81 | (0.26, 2.55) |
| Other intervention groups | 0.93 | (0.56, 1.53) | 1.22 | (0.71, 2.09) | 0.75 | (0.28, 1.99) |
Note: Bold = significant at .05 level
referent = low disorder group
referent = Caucasian American
referent = control group
Table 4 shows the mean economic status of each LCA subgroup at age 30. Wald tests showed that those in the comorbid group (Wald x2 = 8.17) were significantly less constructively engaged in schooling, work, or housework at age 30 compared to young adults in the low disorder group. However, there was no significant difference in constructive engagement for the mental health disorder symptoms group (Wald x2= 3.84) or the licit substance use disorder symptoms group (Wald x2= .87) compared with the low disorder group. Household income at age 30 was significantly lower for all 3 disorder groups: the comorbid group (Wald x2 = 5.14), the mental health disorder symptoms group (Wald x2= 6.33), and the licit substance use disorder symptoms group (Wald x2= 10.71), compared to the low disorder symptoms group. Finally, the comorbid group (Wald x2= 22.64), the mental health disorder symptoms group (Wald x2 = 37.52), and the licit substance use disorder symptoms group (Wald x2= 28.92) each had a lower level of wealth at age 30 compared to those in the low disorder symptoms group.
Table 4.
Mean economic status at age 30 by the mental health and substance use subgroups.
| Mental health and substance use latent classes | ||||
|---|---|---|---|---|
|
| ||||
| Low disorder | Licit substance use disorder symptoms | Mental health disorder symptoms | Comorbid | |
| Later adult socioeconomic status, age 30 | ||||
| Constructive engagement (0-4) | 3.61 | 3.49 | 3.34 | 2.72* |
| Income (in thousands) | 14.59 | 10.98* | 11.31* | 9.91* |
| Wealth (0-5) | 3.33 | 2.54* | 2.41* | 2.19* |
Note. Differences between group means are evaluated using Wald chi-square tests after adjusting for educational attainment at age 21, baseline symptoms of psychopathology, baseline substance use, childhood low-income status, gender, ethnic group, and intervention status
p < .05, compared to low disorder group.
Discussion
The present study assessed the longitudinal impact of earlier socioeconomic status, indicated by educational attainment, on the profiles of mental health and substance use problems, while simultaneously assessing the longitudinal impact of disorder profiles on multiple indicators of later adult socioeconomic status. We found 4 different latent profiles of mental health and substance use disorder symptoms in a community sample at age 27. In line with previous findings,15 our findings suggest that depression and anxiety mostly tend to co-occur with licit substance use disorder symptoms when part of a profile of broad comorbidity that also includes illicit substance use disorder symptoms.
The present study provides evidence supporting the social causation hypothesis. Our findings suggest that not having a high school diploma by age 21 was associated with later increases in comorbid mental health and substance use disorder symptoms and increases in licit substance use disorder symptoms. A variety of factors may explain these longitudinal associations. One possibility is that those without a high school diploma may experience greater exposure to other risk factors associated with mental health and substance use problems, such as high stress.55-57 Another possibility is that young adults without a high school diploma may be less likely to have access to quality mental health care or health insurance.58-60 Future public health studies are needed that carefully consider the ways in which mental health and substance use problems are intertwined in young adulthood when assessing possible explanatory mechanisms associated with effects of educational attainment.
Findings also provide evidence supporting the social selection hypothesis, suggesting that mental health and substance use disorder symptoms may have an adverse impact on one's later economic status. However, this impact varied somewhat across different indicators of adult economic status. There was no statistically significant difference in constructive engagement between young adults in the licit substance use group or the mental health disorder group and those in the low disorder group. Findings thus indicate that those in these groups may remain relatively constructively engaged in work or school. However, income maintenance and wealth building may be more difficult for those who have mental health problems, substance use problems, or both, compared to those with neither.
Prior literature regarding wealth accumulation may inform this somewhat varying association of the mental health and substance use disorder subgroups with different aspects of later socioeconomic status. Individuals' long-term economic stability, as indicated by accumulated savings rather than ones' labor participation, appears to contribute to ones' wealth building.61, 62 Perhaps those who experience mental health or substance use problems are less able to save money due to medical expenses associated with their disorders, even though they maintain labor force participation. In this way, the amount of “necessary consumption,” which interferes with the accumulation of wealth,63 may be very high for those with mental health and/or substance use problems. Thus, their labor force participation may be less likely to result in wealth accumulation.
Our results with respect to the comorbid group are particularly noteworthy given the costly and debilitating consequences of comorbid conditions and the relative paucity of studies examining SES and comorbidity. Comorbid symptoms were significantly related to SES indicators, both as a predictor and outcomes, in all analyses we conducted. These results stress the often interwoven nature of mental illness, drug abuse, and socioeconomic status.
Our findings should be interpreted with some amount of caution given various methodological limitations. Data were collected using self-report surveys, potentially raising concerns about response bias. Additionally, dividing the sample into 4 latent subgroups created some small cell sizes when stratified by ethnic group. Statistically nonsignificant associations between ethnic group variables and the latent class subgroups may be due to a small number of participants in some cells. Replicating the Latent Class Analysis in different populations will be important to assess the generalizability of the classes identified in our study.64
This study also has important strengths. It used prospective data spanning 2 decades, allowing us to evaluate the temporal ordering of mental health and substance use problems and SES directly. Data are from a community sample, and a Latent Class Analysis approach was used that may have underutilized potential for the health inequality literature. We conducted a novel analysis of the social selection and social causation hypotheses with particular attention to the interrelationships of mental health and substance use problems. We also examined multiple aspects of adult economic status, including not only labor income, but also a broader measure of labor force participation, as well as wealth, which have not been widely studied in the health inequality literature. We are aware of no other studies incorporating each of these strengths.
The current findings underscore the importance of young adults' educational attainment for their future risk of mental health and substance use problems. As such, these findings support prevention efforts targeting high school completion. As noted in a brief by the American Public Health Association,65(p.1) “school dropout is much more than an educational crisis. It's a public health epidemic.” School dropout is often a long-term process rather than a single isolated event and child and adolescent social contexts have been identified that play crucial roles in this process.66, 67 For example, experiences in school have been linked to school dropout.66 School contexts have been also associated with substance use problems.68 As such, schools and education can provide institutional environments promoting health.67-69
Our results also suggest that young adults with mental health disorder symptoms and comorbid substance use problems have a harder time achieving long-term adult economic stability than young adults without these problems. In turn, such compromised economic stability at age 30 may potentially exacerbate pre-existing psychiatric problems later in one's adulthood. Public health policies and programs that mitigate the impact of mental health and/or substance use problems on economic stability, such as health insurance policies and financial assistance programs that help to defray costs associated with these problems, can also help to prevent the exacerbation of problems and higher costs to individuals and to society in the future.
Acknowledgments
Funding: This research was supported by grant #9R01DA021426-11 from the National Institute on Drug Abuse. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency. The National Institute on Drug Abuse played no role in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Footnotes
During the elementary grades, a portion of the sample participated in a multicomponent social development intervention promoting positive youth development. The intervention included a full intervention group (n = 156), partial intervention groups (n = 428), and the control group (n = 220) see Hawkins et al. 1999 39 and Hawkins et al. 200540 for more details. The potential effects of the intervention on outcomes were not a focus of the analyses presented here. However, to address possible confounding effects of the intervention on the associations examined in the current study, we included intervention status as a control variable.
Competing Interests: None
Ethical Approval: The study was approved by the Human Subjects Review Committee at the University of Washington (Application #26379-J; Approval date July/5/2011). Prior to age 18, parents of study participants gave informed consent (and the SSDP child provided assent). At each assessment since age 18, the study participants themselves gave informed consent to participate.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatr. 2005;75:3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol. 2003;38:229–37. doi: 10.1007/s00127-003-0627-2. [DOI] [PubMed] [Google Scholar]
- 4.Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 5.Kalaydjian A, Swendsen J, Chiu WT, Dierker L, Degenhardt L, Glantz M, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders, and remission in the National Comorbidity Survey Replication. Compr Psychiatry. 2009;50:299–306. doi: 10.1016/j.comppsych.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siahpush M, McNeill A, Borland R, Fong GT. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15:71–5. doi: 10.1136/tc.2004.008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. [Google Scholar]
- 8.Dohrenwend BP, Levav I, Shrout PE, Sharon S, Naveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–52. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 9.Sareen J, Afifi TO, McMillan KA, Asmundson GJ. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2011;68:419–27. doi: 10.1001/archgenpsychiatry.2011.15. [DOI] [PubMed] [Google Scholar]
- 10.Miech RA, Caspi A, Moffitt TE, Wright BRE, Silva PA. Low socioeconomic status and mental disorders: a longitudinal study of selection and causation during young adulthood. Am J Sociol. 1999;104:1096–131. [Google Scholar]
- 11.Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research - One size does not fit all. JAMA. 2005;294:2879–88. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 12.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 13.Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. Am J Prev Med. 2007;33:250–64. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 14.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 15.Kandel DB, Huang FY, Davies M. Comorbidity between patterns of substance use dependence and psychiatric syndromes. Drug Alcohol Depend. 2001;64:233–41. doi: 10.1016/s0376-8716(01)00126-0. [DOI] [PubMed] [Google Scholar]
- 16.Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–89. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- 17.Jane-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25:515–36. doi: 10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- 18.Merikangas KR, Kalaydjian A. Magnitude and impact of comorbidity of mental disorders from epidemiologic surveys. Curr Opin Psychiatry. 2007;20:353–8. doi: 10.1097/YCO.0b013e3281c61dc5. [DOI] [PubMed] [Google Scholar]
- 19.Jofre-Bonet M, Busch SH, Falba TA, Sindelar JL. Poor mental health and smoking: interactive impact on wages. J Ment Health Policy Econ. 2005;8:193–203. [PubMed] [Google Scholar]
- 20.Vida R, Brownlie EB, Beitchman JH, Adlaf EM, Atkinson L, Escobar M, et al. Emerging adult outcomes of adolescent psychiatric and substance use disorders. Addict Behav. 2009;34:800–5. doi: 10.1016/j.addbeh.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 21.Wadsworth MEJ. Health inequalities in the life course perspective. Soc Sci Med. 1997;44:859–69. doi: 10.1016/s0277-9536(96)00187-6. [DOI] [PubMed] [Google Scholar]
- 22.Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. In: Stewart J, Adler N, editors. Biology of Disadvantage: Socioeconomic Status and Health. Oxford: Blackwell; 2010. pp. 5–23. [DOI] [PubMed] [Google Scholar]
- 23.Cerda M, Sagdeo A, Galea S. Comorbid forms of psychopathology: key patterns and future research directions. Epidemiol Rev. 2008;30:155–77. doi: 10.1093/epirev/mxn003. [DOI] [PubMed] [Google Scholar]
- 24.Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Effects of social development intervention in childhood fifteen years later. Arch Pediatr Adolesc Med. 2008;162:1133–41. doi: 10.1001/archpedi.162.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robins L, Helzer JE, Croghan J, Williams JBW, Spitzer RL. NIMH Diagnostic Interview Schedule Version III. Rockville, MD: National Institute of Mental Health; 1981. [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 27.Kramer JR, Chan G, Dick DM, Kuperman S, Bucholz KK, Edenberg HJ, et al. Multipledomain predictors of problematic alcohol use in young adulthood. J Stud Alcohol Drugs. 2008;69:649–59. doi: 10.15288/jsad.2008.69.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadek N, Bona J. Subsyndromal symptomatic depression: a new concept. Depress Anxiety. 2000;12:30–9. doi: 10.1002/1520-6394(2000)12:1<30::AID-DA4>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 29.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci. 2010;1186:56–68. doi: 10.1111/j.1749-6632.2009.05340.x. [DOI] [PubMed] [Google Scholar]
- 30.Natsuaki MN, Ge XJ, Wenk E. Continuity and changes in the developmental trajectories of criminal career: examining the roles of timing of first arrest and high school graduation. J Youth Adolesc. 2008;37:431–44. [Google Scholar]
- 31.Kenkel D, Lillard D, Mathios A. The roles of high school completion and GED receipt in smoking and obesity. J Labor Econ. 2006;24:635–60. [Google Scholar]
- 32.Laird J, Lew S, DeBell M, Chapman C. Dropout Rates in the United States: 2002 and 2003 (NCES 2006-062) Washington, DC: National Center for Education Statistics, Department of Education; 2006. [Google Scholar]
- 33.Kosterman R, Hawkins JD, Abbott RD, Hill KG, Herrenkohl TI, Catalano RF. Measures of positive adult behavior and their relationship to crime and substance use. Prev Sci. 2005;6:21–33. doi: 10.1007/s11121-005-1250-0. [DOI] [PubMed] [Google Scholar]
- 34.Datta G, Meerman J. Household income or household income per capita in welfare comparisons. Rev Income Wealth. 1980;26:401–18. [Google Scholar]
- 35.Arber S, Ginn J. Gender and inequalities in health in later life. Soc Sci Med. 1993;36:33–46. doi: 10.1016/0277-9536(93)90303-l. [DOI] [PubMed] [Google Scholar]
- 36.Macintyre S, McKay L, Der G, Hiscock R. Socio-economic position and health: what you observe depends on how you measure it. J Public Health Med. 2003;25:288–94. doi: 10.1093/pubmed/fdg089. [DOI] [PubMed] [Google Scholar]
- 37.Achenbach TM. CBCL 4-18: YSR and TRF Profiles. Burlington, VT: University of Vermont Press; 1991. [Google Scholar]
- 38.Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont Press; 1983. [Google Scholar]
- 39.Hawkins JD, Catalano RF, Kosterman R, Abbott RD, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med. 1999;153:226–34. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- 40.Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch Pediatr Adolesc Med. 2005;159:25–31. doi: 10.1001/archpedi.159.1.25. [DOI] [PubMed] [Google Scholar]
- 41.Muthén BO, Satorra A. Complex sample data in structural equation modeling. Sociol Methodol. 1995;25:267–316. [Google Scholar]
- 42.Muthén LK, Muthén BO. Mplus User's Guide. 5th. Los Angeles: Muthén & Muthén; 1998-2007. [Google Scholar]
- 43.Clogg CC, Petkova E, Haritou A. Statistical methods for comparing regressioncoefficients between models. Am J Sociol. 1995;100:1261–93. [Google Scholar]
- 44.Collins LM, Lanza ST. Latent Class and Latent Transition Analysis Hoboken. New Jersey: Wiley; 2010. [Google Scholar]
- 45.Hagenaars JA, McCutcheon AL. Applied Latent Class Analysis. Cambridge; New York: Cambridge University Press; 2002. [Google Scholar]
- 46.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24:882–91. [PubMed] [Google Scholar]
- 47.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13:195–212. [Google Scholar]
- 48.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equation Model. 2007;14:535–69. [Google Scholar]
- 49.Tofighi D, Enders CK. Identifying the correct number of classes in a growth mixture model. In: Hancock GR, editor. Mixture Models in Latent Variable Research. Greenwich, CT: Information Age; 2007. pp. 317–41. [Google Scholar]
- 50.Muthén BO, Asparouhov T. Wald test of mean equality for potential latent class predictors in mixture modeling. 2007 http://www.statmodel.com/download/MeanTest1.pdf.
- 51.Acock AC. Working with missing values. J Marriage Fam. 2005;67:1012–28. [Google Scholar]
- 52.Buhi ER, Goodson P, Neilands TB. Out of sight, not out of mind: strategies for handling missing data. Am J Health Behav. 2008;32:83–92. doi: 10.5555/ajhb.2008.32.1.83. [DOI] [PubMed] [Google Scholar]
- 53.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- 54.Herrenkohl TI, Lee JO, Kosterman R, Hawkins JD. Family influences related to adult substance use and mental health problems: a developmental analysis of child and adolescent predictors. J Adolesc Health. 2012;51:129–35. doi: 10.1016/j.jadohealth.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30:241–56. [PubMed] [Google Scholar]
- 56.Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress - Does stress account for SES effects on health? In: Adler NE, Marmot M, McEwen B, Stewart J, editors. Socioeconomic Status and Health in Industrial Nations - Social, Psychological, and Biological Pathways. New York: New York Academy of Sciences; 1999. pp. 131–44. [DOI] [PubMed] [Google Scholar]
- 57.Grzywacz JG, Almeida DM, Neupert SD, Ettner SL. Socioeconomic status and health: a micro-level analysis of exposure and vulnerability to daily stressors. J Health Soc Behav. 2004;45:1–16. doi: 10.1177/002214650404500101. [DOI] [PubMed] [Google Scholar]
- 58.Congressional Budget Office. How many people lack health insurance and for how long? http://www.cbo.gov/doc.cfm?index=4210. Accessed January 17, 2012.
- 59.Roy-Byrne PP, Joesch JM, Wang PS, Kessler RC. Low socioeconomic status and mental health care use among respondents with anxiety and depression in the NCS-R. Psychiatr Serv. 2009;60:1190–7. doi: 10.1176/ps.2009.60.9.1190. [DOI] [PubMed] [Google Scholar]
- 60.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use ofmental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 61.Modigliani F, Brumberg R. Utility analysis and the consumption function: An interpretation of cross-section data. In: Kurihara KK, editor. Post-Keynesian Economics. New Brunswick, NJ: Rutgers University Press; 1954. pp. 388–436. [Google Scholar]
- 62.Blau FD, Graham JW. Black-White differences in wealth and asset composition. Quart J Econ. 1990;105:321–39. [Google Scholar]
- 63.Keister LA, Moller S. Wealth inequality in the United States. Annu Rev Sociol. 2000;26:63–81. [Google Scholar]
- 64.Bauer DJ, Curran PJ. The integration of continuous and discrete latent variable models: potential problems and promising opportunities. Psychol Methods. 2004;9:3–29. doi: 10.1037/1082-989X.9.1.3. [DOI] [PubMed] [Google Scholar]
- 65.American Public Health Association. The health, well-being and educational success of school-age youth and school-based health care. http://www.schoolbasedhealthcare.org/wp-content/uploads/2011/09/APHA4_article_Health_Rev_9_14_FINAL2.pdf. Accessed December 13, 2011.
- 66.Alexander KL, Entwisle DR, Kabbani NS. The dropout process in life course perspective: early risk factors at home and school. Teach Coll Rec. 2001;103:760–822. [Google Scholar]
- 67.Health Care 2020. London: DTI; 2000. Foresight. [Google Scholar]
- 68.World Health Organization. Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2009/2010 Survey. Copenhagen: WHO; 2012. [Google Scholar]
- 69.World Health Organization. Promoting Health Through Schools. WHO Technical Report Series Geneva: World Health Organization; 1997. [Google Scholar]
- 70.Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–63. [Google Scholar]