Abstract
Background:
It was aimed to compare the efficacy and adverse effects of levobupivacaine alone and in combination with fentanyl and sufentanil during transurethral resection of the prostate (TURP) under spinal anesthesia.
Materials and Methods:
In this prospective, randomized, double-blind trial, 60 patients undergoing elective TURP under spinal anesthesia were randomized into three groups. Ten milligrams of 0.5% levobupivacaine in Group-I, 7.5 mg 0.5% levobupivacaine combined with 25 μg fentanyl in Group-II and 7.5 mg 0.5% levobupivacaine with 2.5 μg sufentanil in Group-III were administered intrathecally.
Results:
The time for sensorial block to reach level T10 was 10.2 ± 2.0, 6.9 ± 1.7 and 7.0 ± 1.4 min in Group-I, II and III, respectively (P < 0.001). The maximum sensorial block level was T8 in all groups. The frequency of a complete motor block was higher in Group-I. The mean duration of motor block was shorter in Group-II and III than in Group-I (P < 0.001). There were no differences between groups regarding side effects (P > 0.05). The time for first analgesic request was shorter in Group-I than in the other two groups (P < 0.05). During the first postoperative 24-h period, 11 (58%) patients in Group-I, 9 (48%) patients in Group II and 9 (45%) patients in Group-III required an analgesic drug (P > 0.05).
Conclusion:
This study showed that combining lower dose levobupivacaine with fentanyl and sufentanil provides faster onset of sensorial block, lower frequency and shorter duration of motor block, and longer analgesia time in TURP under spinal anesthesia.
Keywords: Fentanyl, levobupivacaine, spinal anesthesia, sufentanil, transurethral resection of the prostate
INTRODUCTION
Spinal anesthesia is preferable for endoscopic urological surgery because it is convenient for early recognition of symptoms caused by overhydration, transurethral resection syndrome and bladder perforation.[1] Most candidates for transurethral resection of the prostate (TURP) are older and have preexisting cardiovascular and respiratory diseases. Therefore, it is important to limit the level of the block to reduce adverse cardiopulmonary effects in such patients.[2]
Levobupivacaine is the pure S (-) enantiomer of racemic bupivacaine and has low cardiotoxicity and less undesired effects on the central nervous system. Because of its significantly low side effects, levobupivacaine seems to be an attractive alternative to bupivacaine.[3,4] Opioids and local anesthetics administered together intrathecally have a potent synergistic effect, improving the quality of intraoperative and postoperative analgesia.[5] A combination of these agents allows for a reduction in the dose of both classes of drugs, lessening the likelihood of side effects attributable to each, which is particularly beneficial for geriatric patients.[6] Based on ‘combination wisdom,’ fentanyl was used widely with minidose bupivacaine in the mid-eighties. Sufentanil, an N-4 theinyl derivative of fentanyl, has significant differences in pharmacokinetic properties. A reduced dose of bupivacaine with sufentanil provides successful anesthesia and stability of cardiac output, which is especially important in the elderly.[7]
Highly lipid-soluble synthetic opioids such as sufentanil and fentanyl are being increasingly used along with very low concentrations of local anesthetic agents such as bupivacaine and ropivacaine to provide excellent relief from pain during labor.[8] But there are less studies conducted with combinations of levobupivacaine and opioids in endoscopic urological surgery. It was aimed to compare the efficacy and adverse effects of levobupivacaine alone and in combination with fentanyl and sufentanil during TURP under spinal anesthesia.
MATERIALS AND METHODS
This was a prospective, double-blind, randomized study. It was approved by the local ethics committee of Ankara Numune Training and Research Hospital (Ankara, Turkey; Chairperson Prof. E. Goka) on 14 November 2007. Written informed consent was obtained from all participants prior to the study. Sixty patients whose physical status scores according to American Society of Anesthesiologists (ASA) were I or II; who were between 40 and 80 years of age; and who were scheduled for elective TURP under spinal anesthesia were recruited. Patients without a history of chronic analgesic therapy, arthrosis or scoliosis, peripheral neuropathy, mental disturbance, infection at injection sites, obesity (body mass index > 30), amide hypersensitivity or coagulation defects were included in the study.
A visual analog scale (VAS) was used to measure pain scores, on a numerical scale from 0 to 10 where 0 defined no pain and 10 defined worst pain ever suffered. All patients were informed about pain evaluation and VAS scores preoperatively by one of the attending anesthesiologists. The VAS score was evaluated hourly until score declined below 4.
All patients were given intravenous midazolam premedication (0.01 mg/kg) and a crystalloid infusion (7 ml/kg) preoperatively. The patients were monitored with a Datex Ohmeda S/5 in the operation room. Non-invasive systolic, diastolic, mean arterial pressure, heart rate and peripheral oxygen saturation were measured and recorded at every 5 min until the end of surgery, and with 15-min intervals during recovery. Any clinically relevant hypotension (decrease in systolic arterial blood pressure by 30% or more compared with baseline values) was initially treated with an intravenous infusion of a 0.9% NaCl solution (250 ml over 5 min); if this proved to be ineffective, a bolus of 5 mg ephedrine was given intravenously. Bradycardia (<50 beats per minute) was treated with 0.5 mg atropine intravenously.
This study was conducted in a randomized and double-blind manner. Using a computer-generated random number sequence, patients were allocated into three groups (Group I, n = 20; Group II, n = 20; and Group III, n = 20) by an anesthesiologist. The same investigator prepared the drug solution before anesthesia. The anesthetic administrators and patients were blinded to the type of drug solution. The anesthesiologist who scored pain and the anesthesiologist who applied anesthesia were different. Spinal anesthesia was applied at the level of the L3-4 spinous process using a 25 G Quincke spinal needle. Ten milligrams 0.5% levobupivacaine (0.5% Chirocaine®; Abbott Laboratories, Abbott Park, Illinois, USA, 5 mg/ml) was applied in Group I. In Group II, 7.5 mg 0.5% levobupivacaine combined with 25 μg fentanyl (Fentanyl®; Abbott Laboratories, Abbott Park, Illinois, USA, 50 μg/ml) and in Group III, 0.5% levobupivacaine 7.5 mg combined with 2.5 μg sufentanil (Sufenta®; Janssen-Cilag, Australia, 5 μg/ml) were given in 30 s. Surgery was initiated when the sensorial block level reached the T10 dermatome. Sensorial block level was evaluated bilaterally in the midclavicular line by loss of sensation to pinprick and motor block level was evaluated using the Bromage scale (0 = no motor block, 3 = complete block).
The time for the sensorial block to reach level T10; the maximum sensorial block level; the time to reach maximum sensorial block; the two-segment regression time of the sensorial block; motor block level at the end of surgery; and duration of motor block, time to the first analgesic request after operation and use of supplemental analgesics perioperatively were recorded.
When spinal anesthesia was considered inadequate, 100 μg fentanyl was given intravenously. If additional doses were necessary, the patient was excluded from the study and general anesthesia was induced. The patients were observed in the recovery room for 1 h and then transferred to the in-patient clinic. VAS score, additional analgesic request, time of first analgesic administration and side effects (hypotension, bradycardia, pruritus and nausea – vomiting) were recorded at 1st, 3rd, 6th, 12th and 24th hours. Pruritus, nausea or vomiting was graded as none, mild or severe. Patients who had severe nausea and vomiting preoperatively and postoperatively were treated with 10 mg of metoclopramide. Severe pruritus was treated with 10 mg of diphenhydramine. Patients with a VAS score equal to or higher than 4 were treated with 75 mg of intramuscular diclofenac sodium.
Statistical analysis
Data analysis was performed using the SPSS 13.0 program. Descriptive statistics were presented as mean ± standard deviation (SD). Categorical studies were performed using χ2 - or Fisher's exact test. In this study, one-way analysis of variance test was used to compare whether there were differences between groups and repeated-measure analysis of variance test was used to compare whether there were intra-group differences. During multiple comparisons, in cases where differences were observed among groups, Tukey HSD test and Dunnett test were applied for the purpose of discovering the groups, which demonstrated differences. P < 0.05 was accepted as statistically significant. The Minitab 15.1 statistical package program was used for power analysis (n1 = 19, n2 = 19, n3 = 20, Δ = 6, SD = 5, α = 0.05). Consequently the power of the study was found to be 0.87.
RESULTS
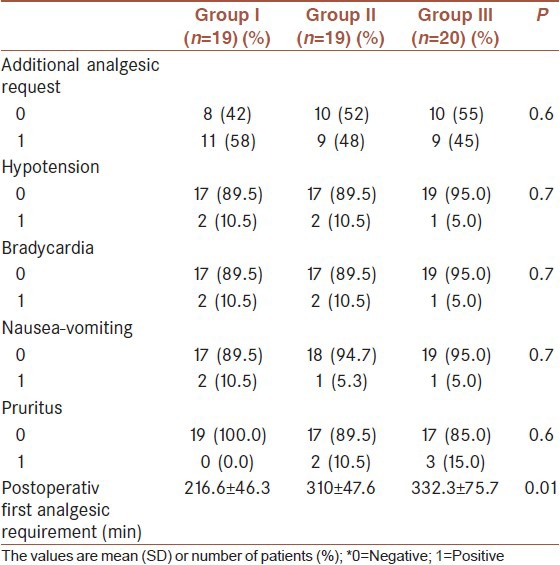
Patients’ characteristics were similar between the three groups (P > 0.05; Table 1). One patient who required general anesthesia due to insufficient spinal block in Group I and one patient whose surgical procedure changed in Group II were excluded from the study [Figure 1]. The mean time for sensorial block at the T10 dermatome was shorter in Group II and III than in Group I (P < 0.001). There were no differences between Group II and III (P > 0.05; Table 2). The maximum sensorial block level was T8 in all groups. The mean time to reach maximum sensorial block and two-segment regression time to sensorial block were not different between the three groups (P > 0.05; Table 2). Complete motor block at the end of surgery was evident in more patients in Group I than in Group II and III (P < 0.001; Table 2). There were no differences between Group II and III (P > 0.05; Table 2). The mean duration of motor block was longer in Group I than in the other two groups, but there was no difference between Group II and III (P < 0.001 and P > 0.05, respectively; Table 2). There was no difference regarding systolic arterial pressure, diastolic arterial pressure, mean arterial pressure and heart rate between the groups during the perioperative and postoperative periods (P > 0.05). Adverse effects are shown in Table 3. The time for first analgesic request was shorter in Group I than in the other two groups (P < 0.05; Table 3). During the postoperative 24 h, 11 patients in Group I (58%), 9 patients in Group II (48%) and 9 patients in Group III (45%) required analgesics.
Table 1.
Demographic data (mean±SD)
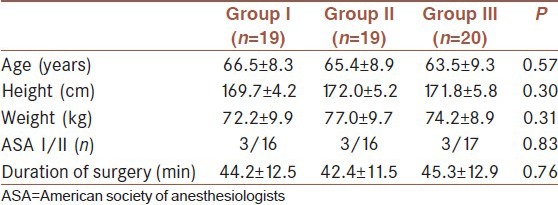
Figure 1.
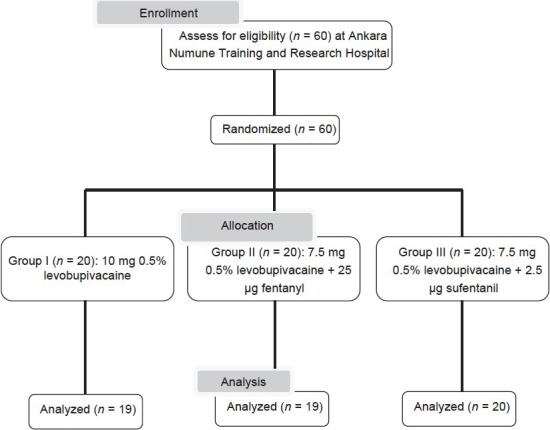
Consort diagram
Table 2.
Comparison of follow-up parameters among the groups (mean±SD)
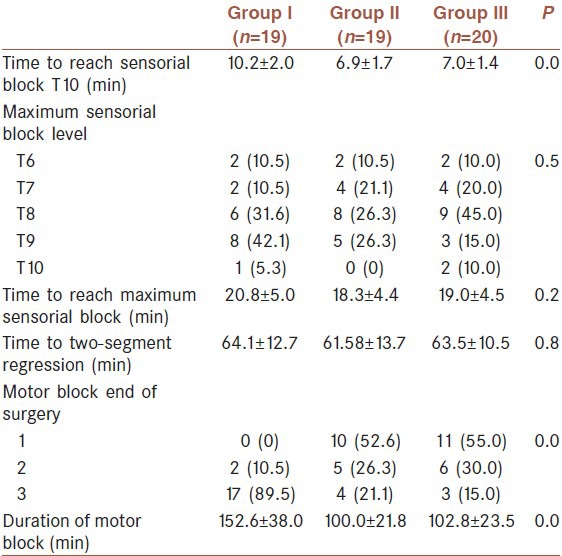
Table 3.
Supplementary analgesic use and side effects
DISCUSSION
The most important finding of the study was that reduction of the dose of levobupivacaine to 7.5 mg and combining it with 25 μg fentanyl or 2.5 μg sufentanil provided an adequate spinal anesthesia for TURP. Most patients undergoing TURP are elderly and frequently have cardiac, pulmonary or other diseases. Therefore, it is important to limit the block level to a lower segment to reduce cardiopulmonary adverse effects in such patients. The level of sensorial block required for endoscopic urologic surgery is the T10 dermatome. The principal determinants of extension and duration of anesthetic block depend on the type and concentration of the local anesthetic used for spinal anesthesia.[1] Using small doses of local anesthetics can limit the distribution of the spinal block but cannot provide an adequate level of sensorial block. Adjuvant agents such as opioids can be used to enhance analgesia and the success rate of spinal anesthesia.[9]
It has been well documented that a combination of bupivacaine with fentanyl or sufentanil has a synergistic analgesic effect when administered intrathecally.[10,11,12] But fewer studies have reported intrathecal usage levobupivacaine with fentanyl or sufentanil. Cuvas et al., compared the characteristics of the spinal block produced by combining 12.5 mg levobupivacaine and 11 mg levobupivacaine with 15 μg fentanyl. There were no differences between time to reach maximum sensorial block, two-segment regression and motor block level. The duration of motor block was shorter for levobupivacaine with fentanyl.[13] They used levobupivacaine in a higher dose but fentanyl in a lower dose than that in the present study. Girgin et al., compared the effectiveness of 7.5 mg levobupivacaine alone and 5 mg levobupivacaine combined with 25 μg fentanyl in ambulatory inguinal herniography. They reported rapid recovery of sensorial and complete motor block in the group levobupivacaine combined with fentanyl.[14] They used a lower dose of levobupivacaine but a higher dose of fentanyl compared with that in the present study.
In the present study, the time for sensorial block to reach level T10 and occurrence of complete motor block were higher and the mean duration of motor block was longer in Group I than in the other groups. There were no differences in two-segment regression time of sensorial block. Stewart et al., reported that when levobupivacaine was given intravascularly to healthy volunteers, no changes were found in stroke index, cardiac index, heart rate, PR interval, QRS duration and QT interval.[15] Leone et al., concluded that both levobupivacaine and ropivacaine seemed to be less neurotoxic and cardiotoxic than bupivacaine.[16] Erdil et al., compared the block durations and hemodynamic effects associated with intrathecal 15 μg fentanyl combined with levobupivacaine and bupivacaine in patients undergoing TURP. They reported that levobupivacaine with fentanyl had better hemodynamic stability and fewer side effects, so this combination was preferred for spinal anesthesia.[17] Lee et al., compared 2.6 ml levobupivacaine alone and 2.3 ml levobupivacaine with 15 μg fentanyl in spinal anesthesia for TURP. There were no significant differences between the two groups regarding hemodynamic changes and motor block. They concluded that further studies might be directed to find the optimal combination of levobupivacaine with an opioid maintaining maximal hemodynamic stability and less motor block.[18] In the present study, hemodynamic parameters were similar in all groups. In addition to the low doses of levobupivacaine and opioids, the lower mean age of the patients in the groups might have provided hemodynamic stability. Additionally, hydration before spinal anesthesia might have had positive effects on hemodynamic stability. Pruritus is the most frequent side effect observed with the use of intrathecal opioids. It may be generalized, but is more likely to be localized to the face, neck or upper thorax. Its incidence varies widely (0-100%) and is dose-related.[19] Motiani et al., compared the efficacy, safety and side effects of intrathecal 5 μg sufentanil or 25 μg fentanyl as adjuvants to 15 mg hyperbaric bupivacaine in patients undergoing lower limb surgery. They found 13.3% pruritus in the sufentanil group.[20] Kim et al., reported that intrathecally bupivacaine with fentanyl 25 μg or sufentanil 5 μg did not cause pruritus.[12] Demiraran et al., reported that the incidence of pruritus was significantly lower in the 1.5-μg sufentanil group when compared with the 2.5- and 5-μg groups.[21] In the present study, mild pruritus localized to the upper thorax was seen in two patients (10.5%) in Group II and three patients (15%) in Group III (P > 0.05). None of these patients needed treatment.
The duration of postoperative analgesia with fentanyl and sufentanil was reported previously to be 1-4 and 2-5 h, respectively, after intrathecal administration as an adjunct to local anesthetics.[16] Nelson et al., compared the duration of analgesia and the side effects in labor analgesia. They reported that fentanyl and sufentanil can safely provide effective, long-lasting labor analgesia without motor block.[22] Motiani et al., reported that the duration of effective analgesia with intrathecal 5 μg sufentanil and 25 μg fentanyl as adjuvants to bupivacaine was longer than that with bupivacaine alone.[20] Kim et al., compared the efficacy of intrathecal 25 μg fentanyl and 5 μg sufentanil with that of low-dose diluted bupivacaine for TURP in elderly patients. They reported that the incidence of postoperative analgesic requirement was significantly lower and the time to first analgesic request was longer in the sufentanil group.[12] Bremerich et al., compared the sensory and motor block characteristics of fixed doses of intrathecal 10 mg hypertonic levobupivacaine and 10 mg bupivacaine combined with either intrathecal fentanyl (10 μg and 20 μg) or sufentanil (5 μg). They reported that 10 mg levobupivacaine combined with 5 μg sufentanil had a prolonged duration of effective analgesia compared with supplemental fentanyl.[23] In the present study, incidence of postoperative analgesic request was lower in the groups with levobupivacaine combined with fentanyl or sufentanil. The time for first analgesic request was shorter in the levobupivacaine-alone group than in the other two groups.
One limitation of this study might be the relatively low sample size. Especially the frequency of the side effects could have altered if the study would have been conducted with more patients. The other limitation is lack of VAS scoring postoperatively.
CONCLUSION
This study showed that reducing the dose of levobupivacaine to 7.5 mg and combining it with 25 μg fentanyl and 2.5 μg sufentanil provides faster onset of sensorial block, lower risk and shorter duration of motor block and longer analgesia time in spinal anesthesia for TURP.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Labbene I, Lamine K, Gharsallah H, Jebali A, Adhoum A, Ghozzi S, et al. Spinal anesthesia for endoscopic urological surgery – low dose vs. varying doses of hyperbaric bupivacaine. Middle East J Anesthesiol. 2007;19:369–84. [PubMed] [Google Scholar]
- 2.Gupta A, Axelsson K, Thörn SE, Matthiessen P, Larsson LG, Holmström B, et al. Low-dose bupivacaine plus fentanyl for spinal anesthesia during ambulatory inguinal herniography: A comparison between 6 mg and 7.5 mg of bupivacaine. Acta Anesthesiol Scand. 2003;47:13–9. doi: 10.1034/j.1399-6576.2003.470103.x. [DOI] [PubMed] [Google Scholar]
- 3.Glaser C, Marhofer P, Zimpfer G, Heinz MT, Sitzwohl C, Kapral S, et al. Levobupivacaine versus racemic bupivacaine for spinal anesthesia. Anesth Analg. 2002;94:194–8. doi: 10.1097/00000539-200201000-00037. [DOI] [PubMed] [Google Scholar]
- 4.Sanford M, Keating GM. Levobupivacaine: A review of its use in regional anaesthesia and pain management. Drugs. 2010;70:761–91. doi: 10.2165/11203250-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Kamphuis ET, Kuipers PW, Venrooij GE, Kalkman CJ. The effects of spinal anesthesia with lidocaine and sufentanil on lower urinary tract functions. Anesth Analg. 2008;107:2073–8. doi: 10.1213/ane.0b013e318187bc0e. [DOI] [PubMed] [Google Scholar]
- 6.Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G. Minidose bupivacaine–fentanyl spinal anaesthesia for surgical repair of hip fracture of aged. Anesthesiology. 2000;92:6–10. doi: 10.1097/00000542-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kaur M, Katyal S, Kathuria S, Singh P. A comparative evaluation of intrathecal bupivacaine alone, sufentanil or butorphanol in combination with bupivacaine for endoscopic urological surgery. Saudi J Anaesth. 2011;5:202–7. doi: 10.4103/1658-354X.82804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akkamahadeur P, Srinivas HT, Siddesh A, Kadli N. Comparison of efficacy of sufentanil and fentanyl with low-concentration bupivacaine for combined spinal epidural labour analgesia. Indian J Anaesth. 2012;56:365–9. doi: 10.4103/0019-5049.100819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Low dose bupivacaine–fentanyl spinal anesthesia for transurethral prostatectomy. Anaesthesia. 2003;58:526–30. doi: 10.1046/j.1365-2044.2003.03153.x. [DOI] [PubMed] [Google Scholar]
- 10.Marandola M, Antonucci A, Tellan G, Fegiz G, Fazio A, Scicchitano S, et al. Subarachnoid sufentanil as a sole agent vs standard spinal bupivacaine in transurethral resection of the bladder. Minerva Anesthesiol. 2005;71:83–91. [PubMed] [Google Scholar]
- 11.Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000;91:1452–6. doi: 10.1097/00000539-200012000-00029. [DOI] [PubMed] [Google Scholar]
- 12.Kim SY, Cho JE, Hong JY, Koo BN, Kim JM, Kil HK. Comparison of intrathecal fentanyl and sufentanil in low-dose dilute bupivacaine spinal anaesthesia for transurethral prostatectomy. Br J Anaesth. 2009;103:750–4. doi: 10.1093/bja/aep263. [DOI] [PubMed] [Google Scholar]
- 13.Cuvas O, Basar H, Yeygel A, Turkyılmaz E, Sunay MM. Spinal anesthesia for transurethral resection operations: Levobupivacaine with or without fentanyl. Middle East J Anesthesiol. 2010;20:547–52. [PubMed] [Google Scholar]
- 14.Girgin NK, Gurbet A, Turker G, Bulut T, Demir S, Kilic N, et al. The combination of low-dose levobupivacaine and fentanyl for spinal anaesthesia in ambulatory inguinal herniography. J Int Med Res. 2008;36:1287–92. doi: 10.1177/147323000803600616. [DOI] [PubMed] [Google Scholar]
- 15.Stewart J, Kellett N, Castro D. The central nervous system and cardiovascular effects of levobupivacaine and ropivacaine in healthy volunteers. Anesth Analg. 2003;97:412–6. doi: 10.1213/01.ANE.0000069506.68137.F2. [DOI] [PubMed] [Google Scholar]
- 16.Leone S, Di Cianni S, Casati A, Fanelli G. Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008;79:92–105. [PubMed] [Google Scholar]
- 17.Erdil F, Bulut S, Demirbilek S, Gedik E, Gulhas N, Ersoy MO. The effects of intrathecal levobupivacaine and bupivacaine in the elderly. Anaesthesia. 2009;64:942–6. doi: 10.1111/j.1365-2044.2009.05995.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee YY, Muchhal K, Chan CK, Cheung AS. Levobupivacaine and fentanyl for spinal anaesthesia: A randomized trial. Eur J Anaesthesiol. 2005;22:899–903. doi: 10.1017/S0265021505001523. [DOI] [PubMed] [Google Scholar]
- 19.Chaney MA. Side effects of intrathecal and epidural opioids. Can J Anaesth. 1995;42:891–903. doi: 10.1007/BF03011037. [DOI] [PubMed] [Google Scholar]
- 20.Motiani P, Chaudhary S, Bahl N, Sethi AK. Intrathecal sufentanil versus fentanyl for lower limb surgeries – a randomized controlled trial. J Anaesth Clin Pharmacol. 2010;26:507–13. [PMC free article] [PubMed] [Google Scholar]
- 21.Demiraran Y, Ozdemir I, Kocaman B, Yucel O. Intrathecal sufentanil (1.5 μg) added to hyperbaric bupivacaine (0.5%) for elective cesarean section provides adequate analgesia without need for pruritus therapy. J Anesth. 2006;20:274–8. doi: 10.1007/s00540-006-0437-2. [DOI] [PubMed] [Google Scholar]
- 22.Nelson KE, Rauch T, Terebuh V, D’angelo R. A comparison of intrathecal fentanyl and sufentanil for labor analgesia. Anesthesiology. 2002;96:1070–3. doi: 10.1097/00000542-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Bremerich DH, Fetsch N, Zwissler BC, Meininger D, Gogarten W, Byhahn C. Comparison of intrathecal bupivacaine and levobupivacaine combined with opioids for caesarean section. Curr Med Res Opin. 2007;23:3047–55. doi: 10.1185/030079907X242764. [DOI] [PubMed] [Google Scholar]


