Short abstract
Doctors and patients should be more aware of the long term risks of radiological investigations
Contemporary medicine relies heavily on radiological and mediconuclear investigations and procedures. However, the often essential information derived from such investigations is obtained at a risk that few doctors are fully aware of. Increased awareness among both doctors and patients would help reduce the number of inappropriate examinations and the avoidable biological burden on current and future generations. In this article, I outline the effect of ionising testing in our society, review the possible detrimental public health effect based on current estimates of risk, and discuss simple ways of achieving a more cautious approach.
Exposure to medical radiation
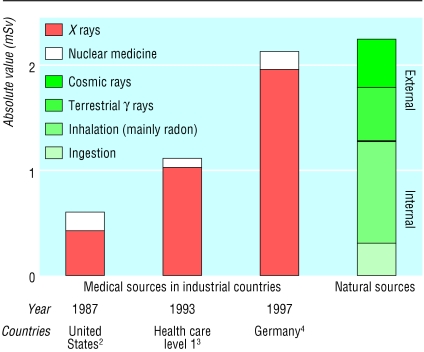
Use of radiation for medical examinations and tests is the largest manmade source of radiation exposure. The biological effect of radiation dose received is expressed in milliSievert (mSv). According to the latest estimation of the United Nations, an average of 2.4 mSv/year comes from natural sources.1 The medical sources of radiation were about one fifth of the natural radiation in 1987,2 close to half in 1993,3 and almost 100% of natural radiation in 1997 in most affluent countries (fig 1).4 In 1997, the German Federal Office for Radiation Protection reported 136 million x ray examinations and 4 million nuclear medicine diagnostic tests, resulting in a mean effective dose of 2.15 mSv per person per year.4
Fig 1.
Medical and natural sources of radiation
Figure 1.
3 Dimensional reconstruction of child's head from computed tomography data
Credit: PHILLIPPE PLAILLY/SPL
The use of procedures with a high load of radiation continues to grow steadily.5 The medical sources of radiation in industrialised countries may therefore soon be greater than natural sources. Ivan Illich wrote in 1976 (at the beginning of the imaging era): “Act so that the effect of your action is compatible with the permanence of genuine human life. Very concretely applied this could mean: Do not raise radiation levels unless you know that this action will not be visited upon your grandchild.”6 The contemporary practice of imaging seems to ignore this sound advice.
Possible risks posed by medical radiation
Current radiation protection standards and practices are based on the premise that any radiation dose, no matter how small, can result in detrimental health effects. These include long term development of cancer7,8 and genetic damage.8 The table gives the best risk estimates available.8,9 These estimates are, however, clouded by approximations and uncertainties for values below 50 mSv, leaving room for conflicting theories that a little radiation could even be beneficial (the hormesis theory)10 or that current risk estimates might be underestimates.11 Until the controversy is resolved, physicians must minimise radiation exposure by following the “do not harm” and “as low as reasonably achievable” principle.7-12
Table 1.
Estimated cancer risk and radiation dose for common imaging examinations
| Risk category* | Dose (mSv) | Equivalent No of chest radiographs |
|---|---|---|
| Zero | ||
| Magnetic resonance imaging | 0 | 0 |
| Ultrasonography | 0 | 0 |
| Negligible | ||
| Limb and joint radiography (except hip) | <0.01 | 0.5 |
| Chest radiography (single posteroanterior film) | 0.02 | 1 |
| Minimal (1 in 1 000 000 to 1 in 100 000) | ||
| Skull radiography | 0.07 | 3.5 |
| Very low (1 in 100 000 to 1 in 10 000) | ||
| Thoracic spine radiography | 0.7 | 35 |
| Lung scintigraphy | 1 | 50 |
| Renal scintigraphy | 1 | 50 |
| Thyroid scintigraphy | 1 | 50 |
| Lumbar spine radiography | 1.3 | 65 |
| Bone scintigraphy | 4 | 200 |
| Low (1 in 10 000 to 1 in 1 000) | ||
| Brain positron emission tomography (with F-18 fluorodeoxyglucose) | 5 | 250 |
| Equilibrium radionuclide cardioangiography | 6 | 300 |
| Barium enema | 7 | 350 |
| Chest computed tomography | 8 | 400 |
| Abdominal computed tomography | 10 | 500 |
| Pelvic computed tomography | 10 | 500 |
| Technetium 99m sestamibi scan | 10 | 500 |
| Thallium scan | 23 | 1150 |
| Interventional fluoroscopic procedures | 25 | 1250 |
| Gallium scan | 40 | 2000 |
Lifetime additional risk of fatal cancer/examination. Classes of risk are developed by the International Commission of Radiological Protection and endorsed by the European Commission on medical imaging guidelines,13
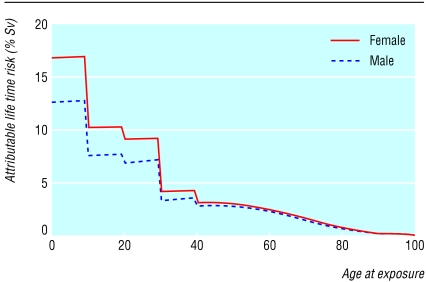
A better estimate of risk to an individual can be calculated from age and sex specific data (fig 2). Females are at slightly higher risk than males, and children are at substantially higher risk than adults because they have more rapidly dividing cells and a greater life expectancy. A 1 year old infant is 10-15 times more likely than a 50 year old adult to develop a malignancy from the same dose of radiation.12
Fig 2.
Attributable lifetime risk for a single small dose of radiation according to age at time of exposure. Radiogenic cancers have long latency periods, and the model may therefore overestimate the risk of fatal cancer in a population with a skewed age distribution, such as radiology or nuclear medicine patients
Need for more caution
In some hospitals patients are now more likely to get a total body scan than a thorough history and careful physical examination. Modern physicians are good at talking with complicated machines but not always as good at listening to patients. In their turn, patients often demand more examinations and feel reassured by high tech ones. The economic drive of expensive testing and doctors' legitimate concerns about medicolegal action if they don't use the latest investigations have done the rest.
Long term risks are not being weighed against the immediate short term diagnostic benefit. In many centres, patients have access to computed tomography without referral from a physician.14 Another problem is cumulative damage from serial follow up scans in patients with benign disease. Serial scanning has created concerns because of the radiation dose associated with computed tomography,14 especially in children.15 Scans of children are often done without adjusting dose to weight, resulting in up to 50% of the dose being unnecessary.16 A small individual risk is multiplied by millions of examinations a year worldwide, becoming an important population risk.16
Reducing radiation exposure
Few doctors know the level of radiation that their patients are exposed to during radiological investigations.17 One reason for this is that basic radiological information is often difficult to find and to understand. The obscure and non-standardised terminology makes it difficult for researchers—not to mention clinicians—to understand the dose and the risks connected to procedures.18 Thus we must increase radiological awareness among physicians as a medical but also social priority.13
The Euratom law establishes that the need for an examination should be justified before a patient is referred to a radiologist or nuclear medicine physician and that a non-ionising technique must be used whenever it will give grossly comparable information to an ionising investigation.19 The existing European law should be reinforced. The three measures described below could help this process.
Radiological prescribing licence
We know that up to a third of radiological examinations are totally or partially inappropriate.5,16 To avoid this misuse, doctors should be required to have a radiological “driving licence.” Penalty points could be given for inappropriate prescriptions—the higher the radiological dose of the inappropriate examination, the higher the penalty. For instance, a doctor could lose up to 50 prescription points for an inappropriate computerised tomogram in a child and 1 point for an inappropriate chest radiograph in a man. After a certain threshold (perhaps 1000 penalty points) the doctor would be forced to attend (and to pass) a radiobiology course. Doctors with repeated infractions could have their licence temporarily withdrawn.
Editorial transparency
Every scientific paper dealing with radiological testing should include a radiological table. The table would describe all tests reported in the article and give the cumulative radiological exposure for the study population. The explicit statement of risks is not only a part of good clinical practice but also of good scientific and editorial practice. It would make authors more aware of what they write, readers more aware of what they read, and both more aware of what they do.
Summary points
Medical radiation from x rays and nuclear medicine is the largest manmade source of radiation exposure in western countries
Doctors are insufficiently aware of the long term health risks associated with radiological imaging Long term risks are often ignored in cost effectiveness analysis of medical imaging
Radiological awareness could be increased by auditing prescriptions and more explicit informed consent forms
Journals should encourage reporting of radiation doses in papers
Explicit informed consent for each examination
Patients should be required to sign an explicit and transparent informed consent form for each radiological examination. The form should spell out the type of examination, the exposure in effective dose (mSv), the dose equivalent in number of chest radiographs, and the risks of fatal and non-fatal cancer and major genetic damage being transmitted to children. Because doctors will have to inform patients, they will by default be informed of what they are proposing. This will make them more likely to consider the risks as well as the benefits.
Consent forms would also help reduce pressure from patients for redundant examinations. The current culture has taught patients that the most expensive tests are likely to be the most effective. In a culture of shared responsibility, any useless risk—no matter how small—should be avoided.20
Conclusion
A real change in radiological practice is not likely to come from new technologies or new laws. We already have excellent technologies and good laws to defend high levels of safety for individuals and the population. We have to implement the law into clinical practice.
Contributors and sources: The main source for this review is the latest guidelines from the International Commission of Radiological Protection (2001). My views are based on 25 years of clinical and scientific work at the Institute of Clinical Physiology of the National Research Council in Pisa, where every day all types of imaging techniques coexist and compete to achieve the elusive target of a perfect diagnosis without risks or environmental burden and at the lowest possible cost.
Competing interests: None declared.
References
- 1.United Nations Scientific Committee on the Sources and Effects of Ionising Radiation. Report on the effects of atomic radiation to the general assembly, 2000. Medical radiation exposures. New York: UN, 2001.
- 2.National Council on Radiation Protection and Measurements. Ionising radiation exposure of the population of the United States. Bethesda, MA: NCRP, 1987. (Report No 93.)
- 3.United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionising radiation. New York: UN, 1996.
- 4.Regulla D, Griebel J, Nosske D, Bauer B, Brix G. Acquisition and assessment of patient exposure in diagnostic radiology and nuclear medicine. Z Med Phys 2003;13: 127-35. [DOI] [PubMed] [Google Scholar]
- 5.Hall EJ. Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol 2002;32: 700-6. [DOI] [PubMed] [Google Scholar]
- 6.Illich I. Medical nemesis. The expropriation of health. New York: Random House, 1976.
- 7.Berrington De Gonzalez A, Darby S. Risk of cancer from diagnostic x-ray: estimates for the UK and 14 other countries. Lancet 2004;363: 345-51. [DOI] [PubMed] [Google Scholar]
- 8.International Commission on Radiological Protection. Radiological protection in biomedical research. Oxford: Pergamon Press, 1991. [PubMed]
- 9.International Commission on Radiological Protection. Radiation and your patient: a guide for medical practitioners. A web module produced by Committee 3 of the ICRP. 2001 www.icrp.org/docs/Rad_for_GP_for_web.pdf. (accessed 12 February 2004).
- 10.Kaiser J. Hormesis. A healthful dab of radiation? Science 2003;302: 378. [DOI] [PubMed] [Google Scholar]
- 11.Davis GT, Bruwer AJ. Health effects of exposure to low levels of ionising radiation. N Engl J Med 1991;324: 7. [Google Scholar]
- 12.Cormack J, Towson JEC, Flower MA. Radiation protection and dosimetry in clinical practice. In: Murray IPC, Ell PG eds. Nuclear medicine in clinical diagnosis and treatment. Oxford: Churchill Livingstone, 1998: 1655.
- 13.European Commission. Radiation protection 118: referral guidelines for imaging. http://europa.eu.int/comm/environment/radprot/118/rp-118-en.pdf (accessed 11 Feb 2004).
- 14.Center for Devices and Radiological Health. Whole body scanning: using computed tomography. www.fda.gov/cdrh/ct (accessed 14 Nov, 2003).
- 15.Center for Devices and Radiological Health. Public health notification: reducing radiation risk from computed tomography for pediatric and small adult patients (2 Nov 2001). www.fda.gov/cdrh/safety.html (accessed 14 Nov, 2003).
- 16.Ron E. Ionising radiation and cancer risk: evidence from epidemiology. Pediatr Radiol 2002;32: 232-7. [DOI] [PubMed] [Google Scholar]
- 17.Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: questionnaire study. BMJ 2003;327: 371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morin RL, Gerber TC, McCollough CH. Radiation dose in computed tomography of the heart. Circulation 2003;107: 917-22. [DOI] [PubMed] [Google Scholar]
- 19.Council Directive 97/43/Euratom of 30 June 1997 on health protection of individuals against the dangers of ionising radiation in relation to medical exposure, and repealing Directive 84/466/Euratom. Official Journal of the European Communities L 180 1997. Jul 9: 0022-7.
- 20.Picano E. Stress echocardiography: a historical perspective. Am J Med 2003;114: 126-30. [DOI] [PubMed] [Google Scholar]