Abstract
Background:
Breast cancer is the most common type of cancer among women, and the second cause of cancer mortality after pulmonary cancer in this gender. Radiotherapy is one of the major treatments, which locally controls the disease and prohibits in recurrency. Radiation pneumonitis is one of the radiotherapy complications, which usually occurs within 1.5-3 months after radiotherapy. As there is no precise estimation concerning this complication in Isfahan, partial frequency of radiation pneumonitis and its association with the energy and treatment technique in patients with breast cancer were evaluated.
Materials and Methods:
This was an analytic cross-sectional study performed in 2010 in university referral center. A total of 382 patients with breast cancer, undergone surgery and referred for radiotherapy entered the study. A posterior and anterior and lateral X-Rays were taken as control images before starting radiotherapy and all X-Rays were repeated after 3-4 months post radiotherapy. The occurrence of radiotherapy pneumonitis was evaluated by the same radiologist. Data were analyzed through SPSS version 20.
Results:
Out of 382 patients undergone breast conservative surgery (BCS) or modified radical mastectomy (MRM), and radiotherapy, 60 patients had pneumonitis of whom 6 patients underwent BCS and were treated by tangential field (three cases by Co 60 and three cases by PH 9). The rest of radiotherapy pneumonitis patients (n = 54) underwent MRM of whom, 42 cases were treated by one-field and 12 by two-field treatment techniques.
Conclusion:
Incidence of radiotherapy pneumonitis was different with respect to the adopted technique (one-field, two-field and tangential) (P = 0.023), with the highest association with two-field radiotherapy.
Keywords: Breast cancer, breast conservative surgery, chest X-ray, energy field, modified radical mastectomy, radiotherapy pneumonitis
INTRODUCTION
Breast cancer is the most common type of cancer among women,[1,7,33] and the second cause of cancer mortality after pulmonary cancer in this gender.[2,33]
The age of its occurrence has diminished in the world and Iran.
Now, there are numerous treatments for this type of cancer, which have notably decreased its mortality. Post-surgery radiotherapy is the main part of treatment to locally control the disease and prohibit its recurrence.[3,7,8,21,26,32] When a treated patient's life gets longer, the treatment complications are more likely to occur. Complications resulted from radiotherapy are not an exception and should be noticed besides numerous treatment benefits of radiation.[13,23,24,29,30,32] One of these complications is radiotherapy pneumonitis usually occurring 1.5-3 months post radiotherapy and is characterized by some clinical signs and radiographic images.[4,14,15,19,2,3,4] Its incidence has been reported 1.2-35% in North America and west Europe.[5,6,27,29,31]
Breast cancer is the most common cancer in female in Isfahan, Iran.[30] Although there is some reports regarding its frequency, no studies has been carried out concerning frequency of pneumonitis resulted from radiotherapy in Isfahan. Seyed Alshohada Treatment Center is one of the major radiotherapy centers in Iran. Therefore, this study was conducted to investigate partial frequency of radiation pneumonitis and its association with the energy and treatment technique in patients with breast cancer in Seyed Alshohada Hospital in Isfahan during September 2010 to September 2011.
MATERIALS AND METHODS
This was an analytic cross-sectional study. Data were collected during September 2010 to September 2011 in Isfahan Seyed Alshohada Education and Treatment Center. According to our statistics specialists, Chi-square test was adopted to analyze the data.
A total of 382 female patients with breast cancer who had undergone surgery modified radical mastectomy or breast conservative surgery (MRM or BCS) and had been referred for radiotherapy were recruited. The only diagnostic methods for radiotherapy pneumonitis were supposed to be patient's clinical condition and Poosterior Anterior and Latral chest X-Rays, which were requested once as a baseline before starting radiotherapy and once as control 3-4 months after the last course of radiotherapy had finished. These baseline and control X-rays were investigated by a fixed radiologist in Seyed Alshohada Hospital for each patient and the occurrence of radiotherapy pneumonitis were evaluated according to a check-list of radiotherapy pneumonitis signs consists of ground glass pattern, opacification, diffuse haziness, and patchy consolidation. The radiologist just knew about the type of surgery, but not the treatment technique and the used energy for radiotherapy. Then, the needed data including patients’ age, the type of surgery (MRM and BCS), type of energy[10,11](Electron, Cobalt 60, Photon), treatment technique (one-field, two-field, tangential), sub-groups of energy[10,12] (E6, E8, E9, E10, E13, Co 60, PH6, PH9, PH12) and occurrence or not occurrence of radiotherapy pneumonitis were collected. Descriptive results were presented in tables and diagrams.
The patients with a history of taking bleomycin, dactinomycin, and nitrous compounds of urea or with a history of chest X-ray due to any reason were excluded from the study. The existence of a background pulmonary disease before starting radiotherapy and smoking cigarettes or water pipe for a long time were other exclusion criteria. The SPSS 20 was used for statistical analysis.
RESULTS
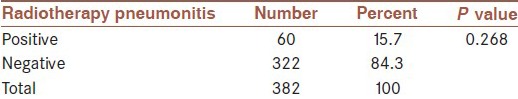
A total of 382 patients entered the study of whom three were male and 382 female patients with breast cancer undergoing surgery. Mean (±SD) age of the subjects was 48.5 ± 10.6 years. The youngest subject was 22 and the oldest was 80 years old. Out of 382 patients, 332 and 50 subjects underwent MRM and BCS respectively. From a total of 382 patients, undergone radiotherapy, 60 developed pneumonitis as a result of radiotherapy with the frequency distribution of 15.7% [Table 1].
Table 1.
Frequency distribution of radiotherapy pneumonitis
From 60 cases of radiotherapy pneumonitis, 6 subjects underwent BCS and were treated by tangential field (three cases by Co 60 and three cases by PH9).
The rest of radiotherapy pneumonitis patients (n = 54) underwent MRM of whom 42 were treated by one-field and 12 by two-field techniques respectively. The association between two types of conducted surgeries (BCS or MRM) was not significant (P = 0.454).
The association between type of energy (electron, Co, PH) and radiotherapy pneumonitis was not significant (P = 0.268).
The association between treatment technique (one-field, two-field, tangential) and radiotherapy pneumonitis was significant (P = 0.023). [Table 2 and 3].
Table 2.
Association between type of energy and radiotherapy pneumonitis
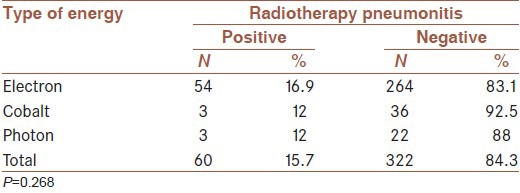
Table 3.
Association between the type of field and radiotherapy pneumonitis complication
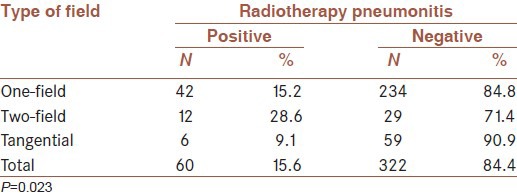
This association was more notable by two-field technique, than one-field and finally tangential technique respectively. Although the association between sub-groups of energy and pneumonitis was not significant, it was significant for the sub-groups of one-field technique (E6, E13, E8, E9, E10) (P = 0.876). The association was not significant for sub-groups of two-field technique (E8, E10, E13+ E10, E10+ E9, E9+ E13, E9+ E6, E9+ PH9, E13+ PH12, PH6, PH9, E6+ PH9) (P = 0. 665).
DISCUSSION
With regard to the obtained results, it was concluded that partial frequency of radiotherapy pneumonitis was 15.6% during September 2010 to September 2011 in the present study, which is laid in the observed statistics in other countries (1.2-35%)[16,18] and even is lower than their mean.
Among all studied factors, there was just a significant association between treatment technique (anterior one-field, anterior two-field, tangential) and radiotherapy pneumonitis.
There was no significant association between surgical techniques, types of energy, and the type of energy sub-groups. Therefore, selection of the an appropriate technique seems to be the most important factor, which can lead to positively or negatively affect radiotherapy pneumonitis incidence in addition to other important factors such as age, pulmonary, cardiac diseases, smoking and etc… influencing its incidence.[15,17] Some researchers have reported a higher incidence of pneumonitis as a result of concurrent radiotherapy and chemotherapy[8,9,21,28,31] so that this factor has been reported as the most effective element in the increase of pneumonitis incidence.
CONCLUSION
No significant association was observed between radiotherapy pneumonitis and the type of surgery and used energy, but there was a significant association between the applied technique (one-field, two-field, tangential) and radiotherapy pneumonitis (P = 0.023). As the number of subjects was low in some two-field sub-group, the precise association between the type of two-field energy and radiotherapy pneumonitis could not be detected. An independent study should be conducted on two-field cases and the energy used on them together with adequate sample size to investigate the association between two-field type of energy and radiotherapy pneumonitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tehran: Ministry of Health and Medical Education; 2005. National report on total number of cancers in 2005. [Google Scholar]
- 2.Wood WC, Muss HB, Solin LJ, Olopade OI. Cancr Principles and Practice of Oncology. 7th ed. Ch 33. USA: Lippincott Williams and Wilkins; 2005. Malignant tumors of the breast; p. 1415. [Google Scholar]
- 3.DeVita VT, Hellman S, Rosenberg SA. USA: Lippincott Williams and Wilkins; 2006. Cancer: Principles and Practice of Oncology: Lung Cancer; pp. 267–97. [Google Scholar]
- 4.Committee for radiation oncology studies. Criteria for radiation oncology in multidisciplinary cancer management: Report to the director of national cancer institute of health Philadelphia. American college of radiology. 1986 [Google Scholar]
- 5.Belka C, Camphausen KA. Why “radiation oncology”. Radiat Oncol. 2006;1:1. doi: 10.1186/1748-717X-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halperin EC, Perez CA, Brady LW, Wazer DE, Freeman C, Prosnitz LR. Fifth, Plus Integrated Content Website ed. USA: Lippincott Williams and Wilkins; 2007. Perez and Brady's Principles and Practice of Radiation Oncology; pp. 2–263. December 3, 2007. [Google Scholar]
- 7.Haskell CM. 5th ed. Philadelphia: WB Saunders Company; 2004. Cancer Treatment; pp. 1–6. [Google Scholar]
- 8.Hendee WR, Ibbott GS, Hendee EG. 3rd ed. Hoboken: Wiley and Sons Inc; 2005. Radiation Therapy Physics; pp. 73–6. [Google Scholar]
- 9.Khan FM. 3rd ed. Philadelphia: Lippincott Williams and Wilkins Company; 2003. The Physics of Radiation Therapy. [Google Scholar]
- 10.Hendee WR, Ibbott GS, Hendee EG. 3rd ed. Hoboken: Wiley and Sons Inc; 2005. Radiation Therapy Physics; pp. 44–112. [Google Scholar]
- 11.Karzmark CJ, Nunan CS, Tanbe E. New York: MC Graw Hill Inc; 1992. Medical Electron Accelerators. [Google Scholar]
- 12.Klein EE, Harms WB, Low DA, Willcut V, Purdy JA. Clinical implementation of a commercial multileaf collimator: Dosimetry, networking, simulation, and quality assurance. Int J Radiat Oncol Biol Phys. 1995;33:1195–208. doi: 10.1016/0360-3016(95)00198-0. [DOI] [PubMed] [Google Scholar]
- 13.Wood WC, Muss HB, Solin LJ, Olopade OI. Cancr Principles and Practice of Oncology. 7th ed. Ch 33. USA: Lippincott Williams and Wilkins; 2005. Malignant tumors of the breast; p. 1441. [Google Scholar]
- 14.McDonald S, Rubin P, Phillips TL, Marks LB. Injury to the lung from cancer therapy: Clinical syndromes, measurable endpoints, and potential scoring systems. Int J Radiat Oncol Biol Phys. 1995;31:1187–203. doi: 10.1016/0360-3016(94)00429-O. [DOI] [PubMed] [Google Scholar]
- 15.De Jaeger K, Seppenwoolde Y, Boersma LJ, Muller SH, Baas P, Belderbos JS, et al. Pulmonary function following high-dose radiotherapy of non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2003;55:1331–40. doi: 10.1016/s0360-3016(02)04389-4. [DOI] [PubMed] [Google Scholar]
- 16.Rancati T, Wennberg B, Lind P, Svane G, Gagliardi G. Radiother Oncol 2007. Vol. 82. Ireland: Elsevier; 2006. Early clinical and radiological pulmonary complications following breast cancer radiation therapy: NTCP fit with four different models; pp. 308–16. Available from: thegreenjournal.com . 2007 Jan p: 308-316. [DOI] [PubMed] [Google Scholar]
- 17.Stover DE, Kaner R. Cancer Principles and Practice of Oncology. 8th ed. Ch 636. USA: Lippincott Williams and Wilkins; 2008. Radiation Induced pulmonary toxicity; pp. 2669–2670. (2676-2677). [Google Scholar]
- 18.Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991;21:355–60. doi: 10.1016/0360-3016(91)90782-y. [DOI] [PubMed] [Google Scholar]
- 19.Seppenwoolde Y, Lebesque JV, de Jaeger K. Comparing different NTCP models that predict ithe incidence of radiation pneumonits. normal tissue complication probability. Int J Radiat Oncol Biol Phys. 2004;58:1636. doi: 10.1016/s0360-3016(02)03986-x. [DOI] [PubMed] [Google Scholar]
- 20.Järvenpää R, Holli K, Pitkänen M, Hyödynmaa S, Rajala J, Lahtela SL, et al. Radiological pulmonary findings after breast cancer irradiation: A prospective study. Acta Oncol. 2006;45:16–22. doi: 10.1080/02841860500334921. [DOI] [PubMed] [Google Scholar]
- 21.Wennberg B, Gagliardi G, Sundbom L, Svane G, Lind P. Early response of lung in breast cancer irradiation: Radiologic density changes measured by CT and symptomatic radiation pneumonitis. Int J Radiat Oncol Biol Phys. 2002;52:1196–206. doi: 10.1016/s0360-3016(01)02770-5. [DOI] [PubMed] [Google Scholar]
- 22.Movsas B, Raffin TA, Epstein AH, Link CJ., Jr Pulmonary radiation injury. Chest. 1997;111:1061–76. doi: 10.1378/chest.111.4.1061. [DOI] [PubMed] [Google Scholar]
- 23.Libshitz HI, Shuman LS. Radiation-induced pulmonary change: CT findings. J Comput Assist Tomogr. 1984;8:15–9. doi: 10.1097/00004728-198402000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Ikezoe J, Takashima S, Morimoto S, Kadowaki K, Takeuchi N, Yamamoto T, et al. CT appearance of acute radiation-induced injury in the lung. AJR Am J Roentgenol. 1988;150:765–70. doi: 10.2214/ajr.150.4.765. [DOI] [PubMed] [Google Scholar]
- 25.Mah K, Poon PY, Van Dyk J, Keane T, Majesky IF, Rideout DF. Assessment of acute radiation-induced pulmonary changes using computed tomography. J Comput Assist Tomogr. 1986;10:736–43. doi: 10.1097/00004728-198609000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Bell J, McGivern D, Bullimore J, Hill J, Davies ER, Goddard P. Diagnostic imaging of post-irradiation changes in the chest. Clin Radiol. 1988;39:109–19. doi: 10.1016/s0009-9260(88)80003-5. [DOI] [PubMed] [Google Scholar]
- 27.Park KJ, Chung JY, Chun MS, Suh JH. Radiation-induced lung disease and the impact of radiation methods on imaging features. Radiographics. 2000;20:83–98. doi: 10.1148/radiographics.20.1.g00ja0483. [DOI] [PubMed] [Google Scholar]
- 28.Choi YW, Munden RF, Erasmus JJ, Park KJ, Chung WK, Jeon SC, et al. Effects of radiation therapy on the lung: Radiologic appearances and differential diagnosis. Radiographics. 2004;24:985–97. doi: 10.1148/rg.244035160. [DOI] [PubMed] [Google Scholar]
- 29.Guckenberger M, Baier K, Polat B, Richter A, Krieger T, Wilbert J, et al. Dose-response relationship for radiation-induced pneumonitis after pulmonary stereotactic body radiotherapy. Radiother Oncol. 2010;97:65–70. doi: 10.1016/j.radonc.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 30.Tahzibi M, Baba zade S, Fazeli Z, et al. Evalutation of age chenges in breast cancer patients referring to seyed al shohada and milad hospital, Isfahan, Iran. Irani J Breast Dis. 2011;4:47–51. [Google Scholar]
- 31.Arrieta O, Gallardo-Rincón D, Villarreal-Garza C, Michel RM, Astorga-Ramos AM, Martínez-Barrera L, et al. High frequency of radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with concurrent radiotherapy and gemcitabine after induction with gemcitabine and carboplatin. J Thorac Oncol. 2009;4:845–52. doi: 10.1097/JTO.0b013e3181a97e17. [DOI] [PubMed] [Google Scholar]
- 32.Vogelius IS, Westerly DC, Cannon GM, Mackie TR, Mehta MP, Sugie C, et al. Intensity-modulated radiotherapy might increase pneumonitis risk relative to three-dimensional conformal radiotherapy in patients receiving combined chemotherapy and radiotherapy: A modeling study of dose dumping. Int J Radiat Oncol Biol Phys. 2011;80:893–9. doi: 10.1016/j.ijrobp.2010.12.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Costanza ME, Chen WY. Factors that modify breast cancer risk in women. UPTODATE. Literature review current through. 2013. Feb, [Last updated 2012 Nov 15]. http://www.uptodate.com/contents/factors-that-modify-breast-cancer-risk-in-women/contributors .


