Abstract
Seasonal influenza vaccination of nurses in Hong Kong fell from 57% in 2005 to 24% in 2012, paralleling concern for adverse reactions associated with vaccination. Decreased acceptance of vaccination was most prominent among nurses who had less work experience and more frequent contact with patients.
Keywords: seasonal influenza, vaccination, health care workers, influenza, viruses, nurses, Hong Kong
Despite the moderate effectiveness of influenza vaccination against seasonal infections (1), vaccination remains a key prevention strategy for enhancing population preparedness. Vaccination of health care workers serves a dual purpose: self-protection and reduction of transmission in health care settings. Worldwide, vaccination coverage among health care workers is extremely variable: 20%–40% in western Europe (2), 16%–60% in Australia (3), 63.5% in the United States (4), and 30% in Hong Kong (5). The main problems with vaccination studies are their incomparability and the changing patterns over time. To determine patterns in Hong Kong, we investigated an 8-year trend of vaccination coverage among nurses.
The Study
In Hong Kong, free yearly influenza vaccination has been offered to all health care workers in the public service since 2003, in the aftermath of severe acute respiratory syndrome. In collaboration with 3 local nurses associations, we administered postal surveys every 1–2 years, focusing on vaccination of nurses and the reasons for their acceptance or decline. The surveys were conducted in 2006, 2007, 2009, 2011, and 2012; during each of these 5 years, 2,500–3,000 questionnaires in the Chinese language were delivered by postal service. Coverage of the surveys ranged from 26% to 38% (Table 1). The surveys included core questions about whether respondents had been vaccinated before the past winter season and whether they planned to be vaccinated in the next year. An incentive, in the form of a book or cash coupon for 25 Hong Kong dollars (1 US$ = 7.8 Hong Kong dollars), was offered to respondents who returned a completed survey form before the end of a 1-month period. Approval of the Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong was obtained. Snapshot results of the survey in 2006, 2009, and 2011 have been published (6–8).
Table 1. General characteristics of questionnaire about influenza vaccination and nurses’ responses.
| Characteristic |
Date of survey |
| 2006 Sep–Oct | 2007 Oct–Nov | 2009 July–Aug | 2011 Mar–Apr | 2012 Feb–Mar | |
|---|---|---|---|---|---|
| General | |||||
| No. questionnaires delivered | 2,825 | 2,929 | 2,929 | 2,494 | 2,492 |
| Response rate, % | 38.2 | 26.9 | 27.7 | 28.4 | 26.6 |
| Total no. respondents | 903 | 739 | 779 | 477 | 651 |
| Male, % |
11.7 |
14.1 |
14.2 |
17.6 |
15.1 |
| Reasons for getting vaccinated, no. respondents* | 510 | 339 | 306 | 127 | 161 |
| Self-protection, % | 74 | 88 | 87 | 94 | 91 |
| Protecting others, % | 32 | 58 | 53 | 71 | 67 |
| Work requirement, % |
38 |
55 |
62 |
39 |
33 |
| Reasons for not getting vaccinated,* no. respondents | 377 | 397 | 451 | 350 | 490 |
| Concern about side effects, % | 42 | 55 | 62 | 70 | 56 |
| Ineffectiveness for self-protection, % | 50 | 57* | 51 | 45 | 50 |
| Ineffectiveness for protecting others, % | 9 | 22 | 14 | 13 | 23 |
| Lack of work requirement, % | 7 | 9 | 6 | 6 | 5 |
*A multiple-choice list was provided for respondents. Only common reasons specifically chosen by respondents in each survey are included in the table, in order of their preferences. Less than 5% chose “other” as their reason for getting vaccinated, whereas ≈20% chose “other” as their reason for not getting vaccinated.
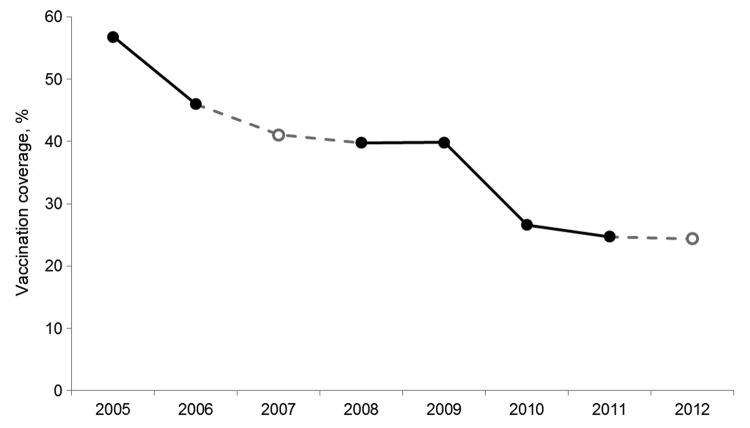
In Hong Kong, influenza vaccination is administered from October through February. In each of the years from 2005 through 2012, the vaccination rate for nurses before the previous winter season was captured. In 2007 and 2012, the percentage of nurses intending to be vaccinated was collected because surveys had not been organized in time to record the actual rate in those years. In 2005, the vaccination rate was 56.8%. It ranged from 50% to 60% irrespective of age, sex, professional rank (registered nurse or enrolled nurse), amount of work experience, and intensity of patient contact (always, sometimes, seldom, or never) (Table 2). A steady decline in vaccination of nurses was observed, more prominently after 2009; the prediction for 2012 was for vaccination of <25% of nurses (Figure). The rates have diversified between subgroups of nurses, despite similarity by sex and professional rank (Table 2). The largest decline in vaccination occurred among nurses with less work experience. Whereas 51% of those with <10 years’ experience were vaccinated in 2005, only 10% were vaccinated in 2012. Surprisingly, nurses always in contact with patients were less inclined to be vaccinated; during this period, the rate of vaccination coverage fell from 54% to 23%. Similarly, vaccination rates among those seldom or never in contact with patients also declined, from ≈60% in 2005 to ≈25% in 2010. Thereafter, the vaccination rate increased to ≈40% in those seldom in contact with patients but continued to fall to ≈20% among nurses not needing to work with patients.
Table 2. Influenza vaccination rates and characteristics of nurses, Hong Kong .
| Characteristic |
Year |
| 2005 | 2006 | 2007* | 2008 | 2009† | 2010 | 2011 | 2012* | |
|---|---|---|---|---|---|---|---|---|
| Total sample size | 903 | 739 | 739 | 779 | 477 | 477 | 651 | 639 |
| Winter influenza season | Mar–Jul‡ | Feb–Apr | Feb–May | Feb–Mar | Jan–Mar | Mar–-May | Jan–Mar | Jan-Mar |
| Predominant influenza virus strain | A(H3N2) | A(H1N1) | A(H3N2) | A(H1N1) | A(H1N1) | B | A(H1N1)2009 | B |
| Overall vaccination rate, % (95% CI) | 56.8 (53.6–60.0) | 46.0 (42.4–49.6) | 41 (37.6–44.7) | 39.8 (36.3–43.2) | 39.8 (35.4–44.2) | 26.6 (22.6–30.6) | 24.7 (21.4–28.1) | 24.4 (21.1–27.8) |
| Vaccination rate by subgroup | ||||||||
| Sex, no. (%) | ||||||||
| M | 106 (58) | 104 (44) | 104 (42) | 111 (44) | 84 (39) | 84 (33) | 98 (31) | 95 (29) |
| F | 797 (57) | 635 (46) | 635 (41) | 668 (39) | 393 (40) | 393 (25) | 553 (24) | 544 (24) |
| Age, y, no. ( %) | ||||||||
| ≤35 | 225 (52) | 104 (38) | 104 (30) | 85 (44) | 22 (36) | 22 (23) | 88 (15) | 86 (16) |
| 36–45 | 422 (59) | 363 (45) | 363 (40) | 318 (36) | 138 (32) | 138 (28) | 159 (25) | 155 (26) |
| >45 | 256 (57) | 272 (50) | 272 (47) | 376 (42) | 317 (44) | 317 (26) | 404 (27) | 398 (25) |
| Professional rank, no. (%) | ||||||||
| Registered nurse§ | 670 (57) | 558 (46) | 558 (41) | 636 (40) | 397 (40) | 397 (27) | 537 (24) | 527 (24) |
| Enrolled nurse# | 203 (55) | 163 (44) | 163 (39) | 124 (41) | 77 (38) | 77 (22) | 96 (27) | 94 (24) |
| Working experience, no. (%) | ||||||||
| <10 y | 146 (51) | 57 (42) | 57 (35) | 71 (44) | 21 (33) | 21 (19) | 80 (14) | 78 (10) |
| 11–20 y | 373 (58) | 275 (40) | 27 (35) | 240 (37) | 103 (30) | 103 (22) | 151 (22) | 147 (23) |
| >20 y | 356 (59) | 385 (51) | 385 (46) | 452 (41) | 353 (43) | 353 (28) | 416 (28) | 410 (28) |
| Patient contact, no. (%) | ||||||||
| Always | 679 (54) | 546 (42) | 546 (37) | 521 (39) | 311 (37) | 311 (26) | 447 (23) | 442 (23) |
| Sometimes | 79 (59) | 62 (60) | 62 (50) | 76 (37) | 41 (44) | 41 (34) | 64 (33) | 62 (27) |
| Seldom | 79 (68) | 71 (55) | 71 (55) | 83 (49) | 50 (44) | 50 (24) | 51 (39) | 47 (45) |
| Never | 59 (66) | 57 (53) | 57 (49) | 93 (40) | 7 (46) | 72 (26) | 87 (17) | 86 (17) |
*Planned vaccination as indicated by nurses in the preceding year. †Vaccination history based on nurses’ recall the following year. ‡Winter and summer seasons merged, giving an extended period of influenza activities. §Completed 3 yr of training in a recognized school and holds a degree/diploma in nursing or equivalent. #Completed 2 yr of training in a recognized training school under a hospital-based program.
Figure.
Rates of influenza vaccination among nurses, before the respective winter seasons, Hong Kong, 2005–2012. Closed circles indicate data based on nurses’ recall a year later; open circles indicate data based on nurses’ plans to get vaccinated the next year.
Overall, self-protection was the main reason for receiving seasonal influenza vaccination, increasing from 74% in 2006 to >90% in 2011 and 2012 (Table 1). The proportion of nurses who indicated that “protecting others” was their reason for vaccination almost doubled since 2006, reflecting nurses’ improved understanding of infection control principles. Lack of a work requirement for vaccination was not a main reason for not getting vaccinated because vaccination is not mandatory in Hong Kong. For nurses who refused to be vaccinated, the main reason was “concern for side effects,” as indicated by 42% in 2006, 70% in 2011, and 56% in 2012. A smaller proportion of respondents indicated refusal to be vaccinated because of “ineffectiveness for self-protection” and “ineffectiveness for protecting others.”
Apparently, attitudes of nurses could be influenced by prevailing epidemic situations locally and internationally. Elsewhere, increased vaccination during the 2009 influenza A(H1N1) pandemic has been reported (9), a phenomenon similar to that in Hong Kong after the 2003 outbreak of severe acute respiratory syndrome (6). Our serial surveys indicated a peak rate of 57% in 2005, which fell to 46% in the next year. For some experienced nurses (>20 years’ experience, ages >45 years), vaccination coverage rate was ≈50% in 2006, when outbreaks of infectious diseases, notably avian influenza, became evident in neighboring mainland China (10). The gradual decline of vaccination coverage paralleled the relatively quiet years; it followed the usual bimodal seasonal peaks until influenza A(H1N1)pdm09 virus emerged. Before this new epidemic, the vaccination rate was 40%, comparable to the rate determined by another study of health care workers in Hong Kong (11). In retrospect, by the time seasonal vaccination was offered toward the end of 2009, the first wave of A(H1N1)pdm09 infection had already subsided. Vaccination coverage in the next year fell to 30%. In addition to the seasonal vaccine, a new monovalent vaccine against A(H1N1)pdm09 virus was introduced at the same year end. The new vaccine was accepted by only 14.2% of the nurses, as indicated by our 2011 survey results (8). The association of A(H1N1)pdm2009 vaccine with Guillain-Barré syndrome was a deterrent to vaccination, despite the minimal increased risk (1 case/1 million vaccinees) (12), especially in light of the mild nature of influenza disease caused by A(H1N1)pdm09 virus. The incorporation of A(H1N1)pdm09 virus in the trivalent vaccine at the end of 2010 could be one reason for the precipitous fall in vaccination coverage (8).
Our study had some limitations. The small sample size and focus on nurses, most of whom were in the public service, imply that generalization of the results to all health care workers would need to be made with caution. Also, repeated administration of the same survey might have led some respondents to choose a desirable rather than an appropriate answer. In addition, although the profile of respondents has remained similar, minor changes in characteristics might have occurred, making interpretation of longitudinal patterns difficult.
Conclusions
Influenza vaccination among health care workers is a complex issue. Our results suggest that whereas self-protection was the main reason for choosing seasonal influenza vaccination, concern about side effects was the main reason for refusing to be vaccinated. A balance of these 2 factors varies with time and is associated with the epidemic condition perceived by the nurses in this study. To enhance societal preparedness, influenza vaccination coverage among health care workers should be maintained at a high level. Those who are at highest risk for virus transmission, i.e., those on the front line and in frequent contact with patients, should be the primary focus of vaccination campaigns. The temporal trend of health care workers’ acceptance of seasonal influenza vaccination was evidently not uniform. For future vaccination strategies, measures for improving vaccination coverage should be tailored to the needs of subcategories of health care workers, including nurses, as defined by their potential for virus transmission.
Acknowledgments
We thank Dennise Tam, K.W. To, Brenda Lee, Steven Poon, and Johnny Chan for their help with administering the questionnaire surveys and analyzing the results; Mandy Li for data entry and maintenance of the database; and members of Hong Kong Nurses General Union, Nurses Branch and Enrolled Nurses Branch of Hong Kong Chinese Civil Servants Association for their participation in the surveys.
We also acknowledge the funding support of the Hong Kong Mood Disorder Centre for the surveys.
Biography
Dr Shui Shan Lee is professor of infectious diseases at the Stanley Ho Centre for Emerging Infectious Diseases, The Chinese University of Hong Kong. His primary research interests are infectious disease epidemiology and HIV treatment optimization.
Footnotes
Suggested citation for this article: Lee SS, Wong NS, Lee S. Declining influenza vaccination coverage among nurses, Hong Kong, 2006–2012. Emerg Infect Dis [Internet]. 2013 Octl [date cited]. http://dx.doi.org/10.3201/eid1910.130195
References
- 1.Treanor JJ, Talbot HK, Ohmit SE, Coleman LA, Thompson MG, Cheng PY, et al. Effectiveness of seasonal influenza vaccines in the United States during a season with circulation of all three vaccine strains. Clin Infect Dis. 2012;55:951–9. 10.1093/cid/cis574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seale H, Macintyre CR. Seasonal influenza vaccination in Australian hospital health care workers: a review. Med J Aust. 2011;195:336–8. 10.5694/mja11.10067 [DOI] [PubMed] [Google Scholar]
- 3.Mereckiene J, Cotter S, D’Ancona F, Giambi C, Nicoll A, Lévy-Bruhl D, et al. VENICE project gatekeepers group. Differences in national influenza vaccination policies across the European Union, Norway and Iceland 2008–2009. Euro Surveill. 2010;15:19700 . [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Influenza vaccination coverage among health-care personnel: 2011–12 influenza season, United States. MMWR Morb Mortal Wkly Rep. 2012;61:753–7 . [PubMed] [Google Scholar]
- 5.Chor JS, Pada SK, Stephenson I, Goggins WB, Tambyah PA, Clarke TW, et al. Seasonal influenza vaccination predicts pandemic H1N1 vaccination uptake among healthcare workers in three countries. Vaccine. 2011;29:7364–9 . 10.1016/j.vaccine.2011.07.079 [DOI] [PubMed] [Google Scholar]
- 6.Tam DKP, Lee SS, Lee S. Impact of severe acute respiratory syndrome and the perceived avian influenza epidemic on the increased rate of influenza vaccination among nurses in Hong Kong. Infect Control Hosp Epidemiol. 2008;29:256–61. 10.1086/527507 [DOI] [PubMed] [Google Scholar]
- 7.To KW, Lee S, Chan TO, Lee SS. Exploring determinants of acceptance of pandemic influenza A (H1N1) 2009 vaccination in nurses. Am J Infect Control. 2010;38:623–30. 10.1016/j.ajic.2010.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poon CM, Lee SS, Lee S. Early uptake of seasonal influenza vaccines incorporated with pH1N1 strain among regularly vaccinated healthcare workers. Journal of Infection Prevention. 2012;13:200–5. 10.1177/1757177412458959 [DOI] [Google Scholar]
- 9.Arda B, Durusoy R, Yamazhan T, Sipahi OR, Taşbakan M, Pullukçu H, et al. Did the pandemic have an impact on influenza vaccination attitude? A survey among health care workers. BMC Infect Dis. 2011;11:87. 10.1186/1471-2334-11-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu H, Feng Z, Zhang X, Xiang N, Huai Y, Zhou L, et al. Human influenza A (H5N1) cases, urban areas of People's Republic of China, 2005–2006. Emerg Infect Dis. 2007;13:1061–4. 10.3201/eid1307.061557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, et al. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009;339:b3391. 10.1136/bmj.b3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wise ME, Viray M, Sejvar JJ, Lewis P, Baughman AL, Connor W, et al. Guillain-Barré syndrome during the 2009–2010 H1N1 influenza vaccination campaign: population-based surveillance among 45 million Americans. Am J Epidemiol. 2012;175:1110–9 . 10.1093/aje/kws196 [DOI] [PMC free article] [PubMed] [Google Scholar]