Abstract
Objectives
To examine the extent to which neighborhood socioeconomic status (SES) is associated with impaired fitness, independent of clinical characteristics and individual-level SES.
Background
Impaired physical fitness, a contributor to obesity and cardiovascular disease, has been associated with both an individual’s SES and with residence in disadvantaged neighborhoods.
Methods
2505 participants 25–42 years old examined in the Coronary Artery Risk Development in Young Adults (CARDIA) study in 1992–1993 underwent symptom-limited exercise stress testing. Physical fitness was considered impaired if metabolic equivalents were in the lowest gender-specific quintile. Neighborhood SES was determined for each census tract using 1990 Census data. Generalized estimating equations assessed the association between Neighborhood SES and physical fitness, before and after adjustments for individual SES, sociodemographic and clinical characteristics, and accounted for clustering within census tracts.
Results
Individuals in disadvantaged neighborhoods had lower educational attainment and income, and were more likely unemployed, black, and uninsured. The odds ratio (95% confidence interval) for impaired physical fitness in the lowest versus highest tertile of Neighborhood SES was 5.8, (3.7–7.3). These became 3.9 (2.7–5.7) after adjusting for individuals’ educational attainment, personal income, employment status, and ability to pay for basic needs; and 1.9 (1.2–2.9) after additional adjustment for other sociodemographic and clinical factors.
Conclusions
Features of one’s neighborhood of residence are relevant to cardiovascular health. A health policy perspective that looks beyond an individual’s characteristics may therefore be useful in identifying more effective interventions t o reduce the prevalence of low physical fitness and its consequences in young adults.
Keywords: epidemiology, physiology, follow-up studies
Poor physical fitness in young adults in the United States is common and is associated with a greater prevalence of obesity and the development of cardiovascular disease risk factors.1–4 Individuals’ educational attainment, occupation, and social class may be linked to behaviors that lead to low fitness and autonomic dysfunction.5–8 Recent work, however, also suggests that socioeconomic attributes of the setting or “context” in which one lives is associated with risk of mortality, impaired physical fitness, and autonomic dysfunction and may therefore contribute independently to poor cardiorespiratory health9–12 However, the extent to which attributes of one’s neighborhood of residence simply reflect the aggregate characteristics of its residents, or relate more directly to abnormal physical fitness is unclear. Therefore, we examined the extent to which residence in an economically disadvantaged neighborhood was associated with impaired fitness in young adults, independent of their personal resources, socioeconomic status, and clinical features.
METHODS
Study Population
The study population was derived from the Coronary Artery Risk Development in Young Adults (CARDIA), a population-based epidemiological study of 5,115 adults aged 18–35 years at baseline, which has been described in detail elsewhere.13 Briefly, in 1985–6 participants recruited by random selection of telephone numbers from designated census tracts in Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and by random selection from the membership list of a health care plan in Oakland, California. The sampling scheme was designed to achieve a balance at each of the 4 sites by race (black, white), sex, education (high school degree or less, more than high school), and age (18–24 years, 25 – 30 years). All subjects gave informed consent before entering the study and at each follow-up examination.
Exercise stress testing was conducted at year 7 (1992–93) at all Centers, a protocol violation at the Minneapolis study site resulted in stress test data that were not comparable to those at the other three study sites.14 The eligibility criteria for the current analysis therefore consisted of completion of stress testing at Birmingham, Chicago, or Oakland at the year 7 CARDIA examination in 1992–93 and availability of a valid residential address at Exam Year 10. A total of 2,505 individuals met these criteria and thus comprised the analytic sample. Baseline characteristics of these participants were similar to those not eligible for the current analysis (n=2539) with respect to age (25 ± 4 vs. 25 ± 4 years), BMI (26 ± 16 vs. 27 ± 16), and all other clinical and demographic features listed in Table 1.
Table 1.
Participants’ Characteristics by Tertiles of the Neighborhood Socioeconomic Score: the CARDIA study, 1992–93 (N=2505)*
| Characteristics | Tertile, SES Range | P for trend |
||
|---|---|---|---|---|
| Lowest (n =835) |
Intermediate (n =836) |
Highest (n =834) |
||
| Demographic & Anthropomorphic Characteristics | ||||
| Age, mean years ± standard deviation (SD) | 31 ± 4 | 32 ± 4 | 32 ± 3 | <0.001 |
| Male sex, no. (%) | 344 (41) | 380 (45) | 408 (49) | 0.002 |
| Black race, no. (%) | 684 (82) | 406 (49) | 172 (21) | <0.001 |
| Waist Circumference (cm) | 85 ± 14 | 83 ± 13 | 80 ± 12 | <0.001 |
| Hip Circumference (cm) | 107 ± 12 | 105 ± 11 | 102 ± 9 | <0.001 |
| Body Mass Index† | 28 ± 6 | 26 ± 6 | 25 ± 5 | <0.001 |
| Marital Status | ||||
| Currently married | 311 (37) | 406 (49) | 445 (53) | <0.001 |
| Clinical History-no. (%) | ||||
| Diabetes | 34 (4) | 20 (2) | 20 (2) | 0.04 |
| Hypertension | 78 (9) | 67 (8) | 49 (6) | 0.008 |
| Current smoker | 288 (34) | 161 (19) | 118 (14) | <0.001 |
| Elevated cholesterol | 89 (11) | 112 (13) | 113 (14) | 0.07 |
| History of peripheral vascular disease | 7 (0.8) | 6 (0.7) | 2 (0.2) | 0.11 |
| History of asthma, emphysema, or bronchitis | 99 (12) | 92 (11) | 88 (11) | 0.40 |
| Fasting Blood Glucose and Lipid Levels: mean ± SD | ||||
| Glucose (mg/dL): | 81 ± 12 | 81 ± 10 | 83 ± 9 | <0.001 |
| Low density lipoprotein cholesterol (mg/dL) | 111 ± 31 | 110 ± 30 | 110 ± 29 | 0.57 |
| High density lipoprotein cholesterol (mg/dL) | 53 ± 12 | 53 ± 13 | 54 ± 13 | 0.03 |
| Triglycerides (mg/dL) | 70 ± 44 | 71 ± 45 | 72 ± 44 | 0.09 |
| Total cholesterol (mg/dL) | 178 ± 35 | 177 ± 33 | 179 ± 31 | 0.47 |
Chi-square test and the Mantel-Haenszel extension test were performed to detect linear trends across increasing tertiles of the Neighborhood SES score.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Exercise Variables
Using a symptom-limited exercise stress testing according to the modified Balke protocol,15 participants were asked to exercise to maximal exertion. Blood pressure and heart rate were obtained at baseline, at 2-minute intervals during stress testing, and at each minute into recovery for three minutes. Using a definition for fitness previously applied to this study population and in other studies,3, 16, 17 we considered physical fitness impaired if the maximum metabolic equivalent (one metabolic equivalent = 3.5 ml/kg/min of oxygen consumption) attained was in the lowest quintile for each gender.3, 16, 17 Abnormal heart rate recovery was defined as the failure of heart rate reduction by more than 12 beats per minute at one minute after peak exercise.18
Neighborhood Socioeconomic Score
Participants’ residential addresses at Exam Year 10 (1995–1996) were “geocoded” or mapped to census tracts, geographical units containing approximately 4000 residents, and linked to 1990 U.S. Census data.19, 20 The 1990 census was specifically used to ensure a temporal sequence in which the proposed exposure (neighborhood socioeconomic status) clearly preceded measurement of the outcome (physical fitness). This exposure was measured using a previously validated approach that incorporated six characteristics for each census tract: median household income; median value of housing unit; proportion of households receiving interest, dividend, or net rental income; the proportion of adults 25 years of age or older who had completed high school; proportion of adults 25 years of age or older who had completed college; and the proportion of employed persons 16 years of age or older in executive, managerial, or professional specialty occupation.21 The distribution for each census tract characteristic was standardized by dividing the mean value for each by its standard deviation. The Neighborhood Socioeconomic Score, a composite measure, was then created by summing the six standardized score values. For descriptive purposes and to ensure an adequate number of participants in each group for the analysis, Neighborhood SES scores were divided into tertiles.
Individual Measures of Socioeconomic status
Using information provided at Exam Year 7 (1992–1993), we developed a series of indicators to reflect each participant’s individual SES in several dimensions (i.e., educational attainment, personal income, employment status, and ability to pay for basic needs)22. These variables were specifically selected to assist in disentangling the contribution of neighborhood socioeconomic status from that of the individual, and to represent the multi-dimensional effects of socioeconomic status on health more accurately in our analysis.22
Statistical Analysis
We examined the association between tertiles of neighborhood SES and impaired physical fitness in a number of ways. First, we evaluated the bivariate relationship between our measures, using the chi-square test and the Mantel-Haenszel extension test to detect linear trends across increasing tertiles of the Neighborhood SES score. Second, multivariable logistic regression models, using general estimating equations and confirmed by hierarchical linear modeling, accounted for clustering within each census tract. To determine the incremental independent association that may exist between the SES of participants’ neighborhood of residence and their physical fitness, we fitted a series of models containing different blocks of variables. The first assessed the unadjusted association between neighborhood SES and physical fitness. In two subsequent steps that confirmed the p resence of a persisting association, we introduced a block of variables containing multiple indicators of individual level SES, and one with demographic, social and clinical variables that included age, gender, race, marital status, current smoking, diagnosis of hypertension, history of diabetes mellitus, coronary artery disease, and peripheral vascular disease, self-reported ability to access health care, body mass index, resting heart rate, blood pressure, total cholesterol, high density lipoprotein cholesterol, low density lipoprotein cholesterol, triglycerides, and fasting glucose, and participants’ self-reported ability to access health care. Interaction terms between neighborhood SES and age, race, and individual level socioeconomic measures were specified a priori based on previous empirical work.9 Supplemental analyses stratified by age, gender, race, body mass index, and smoking status were performed to identify subgroups in which the relationship between neighborhood SES and physical fitness was particularly strong.
Plots of observed versus predicted values assessed model calibration and absence of collinearity was assured by calculation of variance inflation factors. All analyses performed in this paper were verified by two independent CARDIA statisticians and the manuscript was approved by the National Heart, Lung, and Blood Institute and the CARDIA publication and policy committee. Analyses were performed using SAS 9.1 (SAS Inc., Cary, North Carolina).
RESULTS
Baseline Characteristics
Tables 1 and 2 show the characteristics of the CARDIA participants at year 7, arranged by tertiles of the Neighborhood SES score. Those living in areas with a Neighborhood SES score in the lowest tertile had lower levels of educational attainment, lower incomes, and were more likely to be unemployed. Furthermore, these individuals rep orted greater difficulty paying for basics such as food and were less likely to carry health insurance. Diabetes, hypertension, and current tobacco smoking were also more prevalent in low SES neighborhoods.
Table 2.
Participants’ Socioeconomic status and Ability to Access Health Care, by Tertiles of the Neighborhood Socioeconomic Score: the CARDIA study, 1992–93 (N=2505)*
| Characteristics | Tertile, SES Range | P for trend |
||
|---|---|---|---|---|
| Lowest (n =835) |
Intermediate (n =836) |
Highest (n =834) |
||
| Number (%) | ||||
| Education Level | ||||
| Less than high school | 68 (8) | 16 (2) | 14 (2) | <0.001 |
| Graduated high school | 595 (71) | 527 (63) | 362 (43) | <0.001 |
| Some college | 172 (21) | 293 (35) | 458 (55) | <0.001 |
| Income Level | ||||
| Less than $16,000 | 235 (28) | 100 (12) | 56 (7) | <0.001 |
| $16,000 to $34,999 | 312 (37) | 255 (31) | 175 (21) | <0.001 |
| $35,000 to $49,999 | 166 (20) | 197 (24) | 135 (16) | 0.06 |
| $50,000 to $74,999 | 84 (10) | 182 (22) | 194 (23) | <0.001 |
| $75,000 or greater | 38 (5) | 102 (12) | 274 (33) | <0.001 |
| Employment | ||||
| Full time | 585 (70) | 647 (77) | 638 (77) | 0.003 |
| Difficulty paying for basic needs | ||||
| Very hard | 145 (17) | 71 (8) | 49 (6) | <0.001 |
| Somewhat hard | 219 (26) | 203 (24) | 151 (18) | <0.001 |
| Not hard | 471 (56) | 562 (68) | 634 (76) | <0.001 |
| Ability to access health care-no. (%) | ||||
| Has health insurance | 652 (78) | 693 (83) | 728 (87) | <0.001 |
| Identifies a regular source of care | 663 (79) | 711 (85) | 748 (90) | <0.001 |
| Has foregone care due to financial problems | 75 (9) | 91 (11) | 74 (9) | 0.95 |
Chi-square test and the Mantel-Haenszel extension test were performed to detect linear trends across 394 increasing tertiles of the Neighborhood SES score.
Association of Impaired Physical Fitness with Neighborhood SES Score
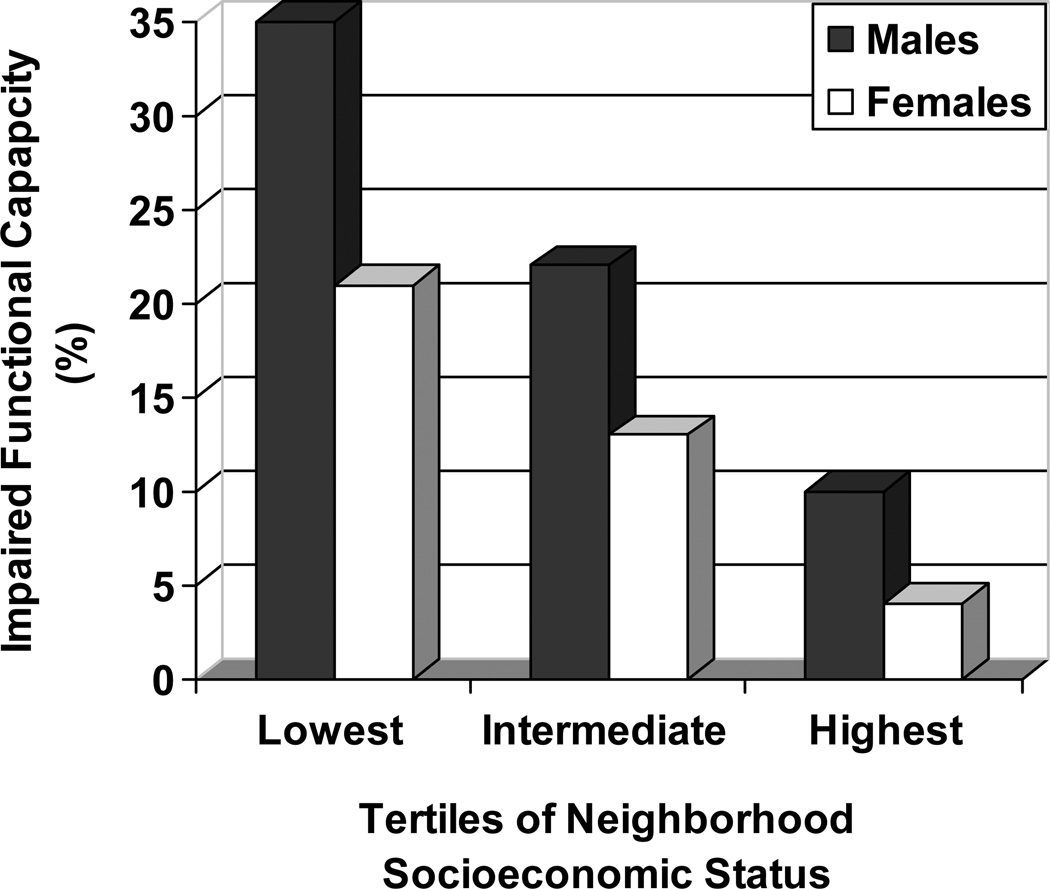
As the Neighborhood SES score decreased, maximum metabolic equivalents (METs) declined (p for trend < 0.001). Similarly, there was a dose dependent relationship between impaired physical fitness and low Neighborhood SES score among both males and females (Figure 1). Individuals residing in areas in the lowest tertile of the Neighborhood SES score had higher mean resting diastolic blood pressure and lower mean peak heart rate.
Figure 1. Association between Tertiles of Neighborhood Socioeconomic Status and Impaired Functional Capacity by Gender.
Note a dose dependent relationship between impaired physical fitness and low Neighborhood SES score among both males and females.
There was a strong association between the Neighborhood SES score and impaired physical fitness, whereby the probability of impaired physical fitness increased as the Neighborhood SES score decreased (lowest versus highest tertile of the Neighborhood SES score, 27% vs. 7%). This association was attenuated, but remained statistically significant as blocks of variables representing either individual socioeconomic indicators or demographic, social and clinical variables were introduced (Table 3). Moreover, this finding remained consistent in models stratified on selected demographic, anthropometric or behavioral characteristics. A second supplemental analysis confined to individuals remaining at the same address between years 0 and 7 (Table 3) and years 7 and 10 (n = 2086) demonstrated similar findings with the multivariate adjusted odds ratio (95% confidence interval) for impaired physical fitness in the lowest versus highest tertile of Neighborhood SES 1.7, (1.10–2.8) and 1.9, (1.3–2.8) for the intermediate (2nd) versus highest tertile. Of the interactions tested, none achieved statistical significance.
Table 3.
Association of Impaired Physical Fitness and the Neighborhood Socioeconomic Score in All Subjects and By Prespecified Subgroups: the CARDIA study, 1992–93†
| Number (%) of those with Impaired Physical Fitness |
Odds ratios (95% confidence intervals) for lowest and intermediate Tertiles versus highest Tertile (referent) |
|||
|---|---|---|---|---|
| Lowest Tertile (n =835) |
Intermediate Tertile (n =836) |
Highest Tertile (n =834) |
||
| All Subjects (n=2,505) | ||||
| Unadjusted | 423 (17) | 5.2 (3.7–7.3) | 2.8 (2.0–4.0) | 1.0 |
| Adjusted for participants’ SES and all characteristics shown in Table 2§ | - | 3.9 (2.7–5.7) | 2.5 (1.7–3.6) | 1.0 |
| Adjusted for clinical characteristics only‡ | - | 2.1 (1.4–3.2) | 1.9 (1.3–2.7) | 1.0 |
| Adjusted for all variables* | - | 1.9 (1.2–2.9) | 1.8 (1.2–2.7) | 1.0 |
| Multivariable Adjusted Stratified Analysis | ||||
| Age | ||||
| <35 years (n=1752) | 288 (16) | 1.5 (0.94–2.5) | 1.5 (1.0–2.4) | 1.0 |
| ≥35 years (n= 753) | 135 (18) | 2.4 (1.2–5.1) | 2.1 (1.1–4.1) | 1.0 |
| Gender | ||||
| Male (n=1132) | 245 (22) | 2.1 (1.3–3.5) | 2.0 (1.3–3.2) | 1.0 |
| Female (n=1373) | 178 (13) | 1.7 (0.83–3.4) | 1.7 (0.89–3.3) | 1.0 |
| Race | ||||
| White (n=1243) | 95 (8) | 2.1 (0.85–5.1) | 2.0 (1.1–3.6) | 1.0 |
| Black (n=1262) | 328 (26) | 1.6 (1.0–2.7) | 1.6 (0.95–2.6) | 1.0 |
| Body Mass Index | ||||
| <30 (n=1965) | 193 (10) | 2.1 (1.2–3.6) | 1.9 (1.1–3.1) | 1.0 |
| ≥30 (n=540) | 230 (43) | 1.2 (0.60–2.1) | 1.5 (0.82–2.8) | 1.0 |
| Current smoker | ||||
| Yes (n=567) | 146 (26) | 1.6 (0.75–3.2) | 2.7 (1.3–5.3) | 1.0 |
| No (n=1938) | 277 (14) | 2.2 (1.4–3.7) | 1.6 (1.0–2.5) | 1.0 |
| Moved from exam year 0 to 7 | ||||
| Yes (n = 822) | 142 (17) | 2.4 (1.2–5.2) | 1.9 (0.92–3.9) | 1.0 |
| No (n = 1683) | 281 (17) | 1.5 (0.91–2.6) | 1.7 (1.1–2.6) | 1.0 |
Impaired Physical fitness was defined as lowest quintile.
Adjusted for all characteristics shown in Table 2 and marital status.
Adjusted for age, gender, race, systolic and diastolic blood pressure, history of hypertension, hypercholesterolemia, diabetes, peripheral vascular disease, asthma, emphysema, chronic bronchitis, fasting glucose, low density lipoprotein cholesterol, high density lipoprotein cholesterol, total cholesterol, and triglycerides.
C statistic for the final model= 0.86
DISCUSSION
In this population-based epidemiological study of relatively healthy young adults, a composite measure of the socioeconomic status of participants’ neighborhood of residence was strongly associated with impaired physical fitness independent of characteristics that reflected their personal socioeconomic standing or other demographic, social, or clinical factors that might have confounded this relationship. These findings have significant public policy and clinical implications and may be useful in addressing the disparity gap in cardiovascular health outcomes. From an epidemiological perspective, our results support use of a multi-level approach to cardiovascular risk assessment and intervention that takes into account one’s living environment in addition to individual level clinical and socioeconomic measures.2–4
Lack of fitness is prevalent among young adults in the United States,2–4 with an estimated 24.4% of the population reporting no leisure time physical activity in a recent national survey.23 While personal health behaviors and beliefs are closely related to one’s physical health and may therefore explain much of this trend,5, 6 it is also plausible that the attributes of an individual’s residential space and the opportunities available to maintain health and well-being may contribute in important ways. The economic vitality of an area, for example, is thought to have an important influence on the “built environment”, particularly on the availability of space and physical structures (e.g., tennis or basketball courts, tracks, swings) for physical activity.24 Previous work provides consistent support for a strong association between greater physical activity (and thus improved physical fitness) and the availability of recreational facilities, opportunities to be active, and the aesthetic qualities of communities.25 Moreover, the accessibility and actual use of these resources may be further constrained in economically disadvantaged areas especially if residents have concerns for their personal safety while in public places.26 Urban planning and policy decisions also influence the level of physical activity even when facilities are available. Increased traffic congestion in neighborhood streets, reduced lighting on streets and in public spaces, and limited side-walk continuity have been associated with a lower prevalence of walking and cycling by individuals residing in deprived neighborhoods.27
This study addresses several limitations of previous work and adds to an emerging understanding of the relevance of contextual factors to cardiovascular health. First, previous studies examining associations between contextual factors and cardiovascular outcomes fail to incorporate individual level measures of socioeconomic status, an approach that has the potential to introduce residual confounding related to the multiple conceptual dimensions of SES.9, 12 Second, unlike other work relying on self-reported measures such as physical activity questionnaires, which are prone to recall bias, we used objective measures of functional capacity to provide a more accurate estimate of physical fitness. Third, given that individuals residing in economically disadvantaged neighborhoods typically have a higher prevalence of cardiovascular risk factors such as hypertension, diabetes mellitus, and obesity, accounting for some of the association between contextual factors and health outcomes,11 we conducted the current analysis using a large sample of relatively young healthy adults with few comorbid conditions. Statistical adjustment for these and other cardiovascular risk factors, when present, further reduced concerns about potential confounding. Finally, unlike previous population-based studies that involve middle aged to older adults, the CARDIA participants were 25–42 years old at the time of data collection. Studies in younger populations are important, especially if associations such as those between contextual characteristics and physical fitness at an earlier age contribute to disparities in cardiovascular health that arise later in life.
The strong association between neighborhood S ES and physical fitness was considerably attenuated once adjusted for clinical characteristics (Table 3). This confirms the independent association between neighborhood SES and impaired physical fitness. However, given the cross-sectional nature of this study it is not clear whether the clinical variables that attenuated the affect of neighborhood SES are mediators in this pathway or are truly independent of neighborhood SES. Nevertheless, these results emphasize the importance of risk factor modification since changing environmental contextual factors may be more difficult.
Our study has several limitations. Despite the magnitude of the association between neighborhood SES and physical fitness reported here, our cross-sectional cohort study design does not permit us to conclude that this relationship is causal. Indeed, unmeasured confounders at both the individual and neighborhood levels may have influenced our results despite the use of more than 20 variables identified through previous work to influence physical fitness, represent key dimensions of socioeconomic status, or potentially serve to confound recognition of a relationship between Neighborhood SES score and fitness. Generalizability of the study findings to other settings is a second concern. Although the CARDIA sample was representative of cities in which the study was conducted and is generally representative of other young adults in the U.S., continued investigation in this area is warranted. Third, our study was conducted in relatively young healthy adults and lacked data on hard endpoints such as death or myocardial infarction. However, previous investigators have shown a strong association between neighborhood of residence and mortality in middle aged to older adults9, 28–30. Fourth, our measure of neighborhood socioeconomic status may not have fully captured the true socioeconomic status of an individual’s environment. Misclassification, however, would most likely have underestimated the true association between Neighborhood SES and physical fitness. Moreover, we were reassured by the excellent internal consistency of the 6 variables comprising this score (Cronbach's alpha = 0.91), an indication that they tapped the same construct. Fifth, because of lack of accessibility to individual’s addresses we could only use geocoding information that was available on year 10 (1995–1996) rather than year 7 (1992–1993). However, given that socioeconomic data was obtained from 1990 census the temporality of the association between neighborhood SES and impaired physical fitness was preserved. Finally, our study reports an association between neighborhood of residence and physical fitness that existed during the 1990s. Given insights from an extensive literature based in social epidemiology over the past two centuries, however, the importance of social and economic conditions as fundamental causes of disparities in health seems certain.31 While the strength of such an association related to specific outcomes may change over time, we conclude that the exposure itself remains an important consideration with major epidemiological, clinical, and policy implications that cannot be ignored.
Despite numerous public health interventions, cardiovascular health disparities remain prevalent in the United States.32, 33 Additional efforts to recognize a full range of factors that promote these disparities and the mechanisms through which these factors exert their influence are needed to make headway in addressing this persistent problem. Although interventions focused on the individual such as smoking cessation, lipid control, and hypertension management have been instrumental, addressing features of the environment in which one lives provides another opportunity to tackle disparities in cardiovascular health. From a clinical standpoint, a better understanding among physicians that neighborhood characteristics reflect important health exposures and that these characteristics (including the availability, accessibility and safety of local activity spaces) should be considered when developing recommendations for increased physical exercise may do much to address the persisting issue of health disparities.
ACKNOWLEDGMENTS
The authors are grateful to Dr. Ana V. Diez Roux (Professor, Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor) and Dr. Katharine A. Kirk (Emeritus Professor, Department of Biostatistics and Division of Preventive Medicine, University of Alabama at Birmingham, Birmingham) for their thorough and most helpful criticisms of the manuscript.
FUNDING SOURCE
M.H.S. is supported in part by the National Institutes of Health, National Institute of Child Health and Human Development, Multidisciplinary Clinical Research Career Development Programs Grant K12 HD049091 and the National Institutes of Health Loan Repayment Program.
D.L. is supported by a career development award from the Veterans Administration Health Services Research and Development Service RCD-03028-1 and by Program Grant R25T CA111898, the National Cancer Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
None
References
- 1.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 2.Kimm SY, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002;347(10):709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 3.Carnethon MR, Gidding SS, Nehgme R, et al. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290(23):3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 4.Carnethon MR, Gulati M, Greenland P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. JAMA. 2005;294(23):2981–2988. doi: 10.1001/jama.294.23.2981. [DOI] [PubMed] [Google Scholar]
- 5.Popkin BM, Siega-Riz AM, Haines PS. A comparison of dietary trends among racial and socioeconomic groups in the United States. N Engl J Med. 1996;335(10):716–720. doi: 10.1056/NEJM199609053351006. [DOI] [PubMed] [Google Scholar]
- 6.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345(11):790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 8.Hemingway H, Shipley M, Brunner E, et al. Does autonomic function link social position to coronary risk? The Whitehall II study. Circulation. 2005;111(23):3071–3077. doi: 10.1161/CIRCULATIONAHA.104.497347. [DOI] [PubMed] [Google Scholar]
- 9.Shishehbor MH, Litaker D, Pothier CE, et al. Association of socioeconomic status with functional capacity, heart rate recovery, and all-cause mortality. JAMA. 2006;295(7):784–792. doi: 10.1001/jama.295.7.784. [DOI] [PubMed] [Google Scholar]
- 10.Berkman LF. Tracking social and biological experiences: the social etiology of cardiovascular disease. Circulation. 2005;111(23):3022–3024. doi: 10.1161/CIRCULATIONAHA.104.509810. [DOI] [PubMed] [Google Scholar]
- 11.Diez Roux AV. Persistent social patterning of cardiovascular risk: rethinking the familiar. Circulation. 2005;111(23):3020–3021. doi: 10.1161/CIRCULATIONAHA.105.542845. [DOI] [PubMed] [Google Scholar]
- 12.Tonne C, Schwartz J, Mittleman M, et al. Long-term survival after acute myocardial infarction is lower in more deprived neighborhoods. Circulation. 2005;111(23):3063–3070. doi: 10.1161/CIRCULATIONAHA.104.496174. [DOI] [PubMed] [Google Scholar]
- 13.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 14.Sidney S, Sternfeld B, Haskell WL, et al. Seven-year change in graded exercise treadmill test performance in young adults in the CARDIA study. Cardiovascular Risk Factors in Young Adults. Med Sci Sports Exerc. 1998;30(3):427–433. doi: 10.1097/00005768-199803000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Sidney S, Haskell WL, Crow R, et al. Symptom-limited graded treadmill exercise testing in young adults in the CARDIA study. Med Sci Sports Exerc. 1992;24(2):177–183. [PubMed] [Google Scholar]
- 16.Blair SN, Kampert JB, Kohl HW., 3rd Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276(3):205–210. [PubMed] [Google Scholar]
- 17.Wei M, Kampert JB, Barlow CE, et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA. 1999;282(16):1547–1553. doi: 10.1001/jama.282.16.1547. [DOI] [PubMed] [Google Scholar]
- 18.Cole CR, Blackstone EH, Pashkow FJ, et al. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341(18):1351–1357. doi: 10.1056/NEJM199910283411804. [DOI] [PubMed] [Google Scholar]
- 19.Diez Roux AV, Jacobs DR, Kiefe CI. Neighborhood characteristics and components of the insulin resistance syndrome in young adults: the coronary artery risk development in young adults (CARDIA) study. Diabetes Care. 2002;25(11):1976–1982. doi: 10.2337/diacare.25.11.1976. [DOI] [PubMed] [Google Scholar]
- 20.Henderson C, Diez Roux AV, Jacobs DR, Jr, et al. Neighbourhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: the CARDIA study. J Epidemiol Community Health. 2005;59(4):322–328. doi: 10.1136/jech.2003.018846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 22.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Chronic Disease Prevention & Health Promotion Behavioral Risk Factor Surveillance System. [Accessed April 4, 2007];2002 at http://apps.nccd.cdc.gov/brfss/Trends/trendchart.asp?qkey=10020&state=US). In;
- 24.Gordon-Larsen P, Nelson MC, Page P, et al. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 25.Humpel N, Owen N, Leslie E. Environmental factors associated with adults' participation in physical activity: a review. Am J Prev Med. 2002;22(3):188–199. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- 26.Huston SL, Evenson KR, Bors P, et al. Neighborhood environment, access to places for activity, and leisure-time physical activity in a diverse North Carolina population. Am J Health Promot. 2003;18(1):58–69. doi: 10.4278/0890-1171-18.1.58. [DOI] [PubMed] [Google Scholar]
- 27.Saelens BE, Sallis JF, Frank LD. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. Ann Behav Med. 2003;25(2):80–91. doi: 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- 28.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol. 1999;149(10):898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 29.Rogot E, Sorlie PD, Johnson NJ, et al. A mortality study of 1.3 million persons by demographic, social and economic factors: National Institute of Health. 1992 Report No.: 92–3297. [Google Scholar]
- 30.Makuc D, Feldman JJ, Kleinman J, et al. Health Status and Well-being of the Elderly. New York: Oxford University Press; 1990. Sociodemographic differentials in mortality; pp. 155–171. [Google Scholar]
- 31.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No:80–94. [PubMed] [Google Scholar]
- 32.United States. Healthy people 2010 : understanding and improving health. 2nd ed. Washington, DC: US Dept. of Health and Human Services : For sale by the USGPO. Supt. of Docs; 2000. Dept. of Health and Human Services. [Google Scholar]
- 33.United States. Public Health Service. Surgeon General's report on physical activity and health. Pittsburgh, PA: From the Centers for Disease Control and Prevention; 1996. Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (U.S.), President's Council on Physical Fitness and Sports (U.S.) [Google Scholar]