Summary
We evaluated the effect of home telehealth on weight maintenance after a group-based weight loss programme. The home telehealth intervention comprised telephone counselling and home Internet-enabled digital video recorders (DVRs) with three channels of video programmes. The video content provided reinforcement and support to promote problem solving, prevent relapse, and sustain motivation. Eighty-eight obese or overweight African-American women were randomized to receive monthly telephone counselling (control) or the home telehealth intervention. The weight change during maintenance was not significant in either group (0.6 kg in the intervention group, 0.0 kg in the control group), and there was no significant difference between them. Changes in diet, physical activity, social support and self-efficacy during the maintenance period did not differ significantly between groups. DVR use was low: during the intervention, the number of valid DVR viewings ranged from zero to 42 per person. DVR use was positively associated with previous attendance at the weight loss classes. Home video-based telehealth is a new method of delivering a weight loss maintenance intervention to African-American women. It had no effect on weight maintenance in the present study.
Introduction
In the US, 78% of African-American women are classified as overweight or obese, with a body-mass index (BMI) ≥25 kg/m2.[1] This represents an important population because African-American women are disproportionately affected by diseases associated with overweight and obesity, such as hypertension and type 2 diabetes.[2]
Developing effective short-term weight loss interventions for African-Americans is difficult. However, maintaining any weight loss which occurs is even more difficult.[3, 4] We have investigated the use of video telehealth for weight maintenance. “Exercise Your Faith” is a telehealth weight maintenance programme for African-American women. It is delivered through an Internet-enabled digital video recorder (DVR) to African-American women at home. The programme was designed to maintain contact with participants over an extended period of time, to support problem solving, prevent relapse and sustain motivational efforts.
The aim of the present study was to evaluate the effect of video telehealth on weight maintenance.
Methods
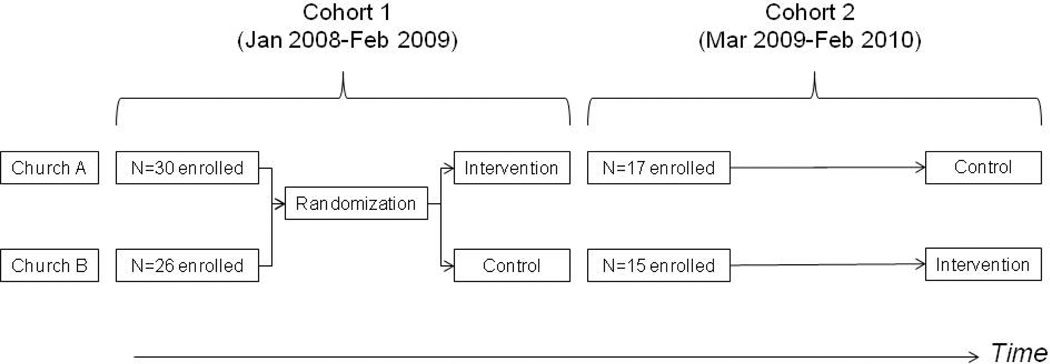
We conducted a randomized controlled trial to evaluate the effect of video telehealth on weight maintenance. We recruited overweight and obese African-American women from two community churches. Participants were recruited in two cohorts (Figure 1) which were randomized by church. All participants were provided with a group-based weight loss programme lasting 3 months before the weight maintenance phase began.
Figure 1.
Participants were recruited in two cohorts
The weight-loss programme comprised group-based instruction on lifestyle behaviours directed towards weight loss. The 60-min weekly classes included: (1) a didactic session led by an African-American instructor that included discussions of healthy eating and exercise goals; and (2) an exercise session in which a professional trainer led the class in aerobic activity. Objectives included reducing dietary fat to less than 30% of total daily calories, increasing dietary fibre to a minimum of 25 g daily and increasing fruit and vegetable consumption to at least five servings daily.
Following the weight loss programme, cohorts of women received video telehealth and telephone support for weight loss maintenance (intervention), or telephone support for weight loss maintenance (control). The weight maintenance phase lasted for 9 months. The study was approved by the appropriate ethics committee.
Participants
The criteria for study inclusion were: (1) self-identification as an African-American or Black woman; (2) age 35–65 years; (3) BMI 25–50 kg/m2; (4) physician approval to safely exercise if any positive answers on Physical Activity Readiness Questionnaire [5]; (5) owns a television; and (6) has a working telephone line. Broadband Internet access was provided to those without it. Individuals were excluded if they: (1) planned to move from the Chicago area during the following year; (2) had a household member already in the study; (3) used illicit drugs or drank more than two alcoholic drinks daily; (4) were pregnant, nursing or planning pregnancy; (5) were currently participating in an organized weight loss programme or using pharmacotherapy for weight loss; and (6) used an assistive device for ambulation, or could not participate in exercise classes.
Participant flow
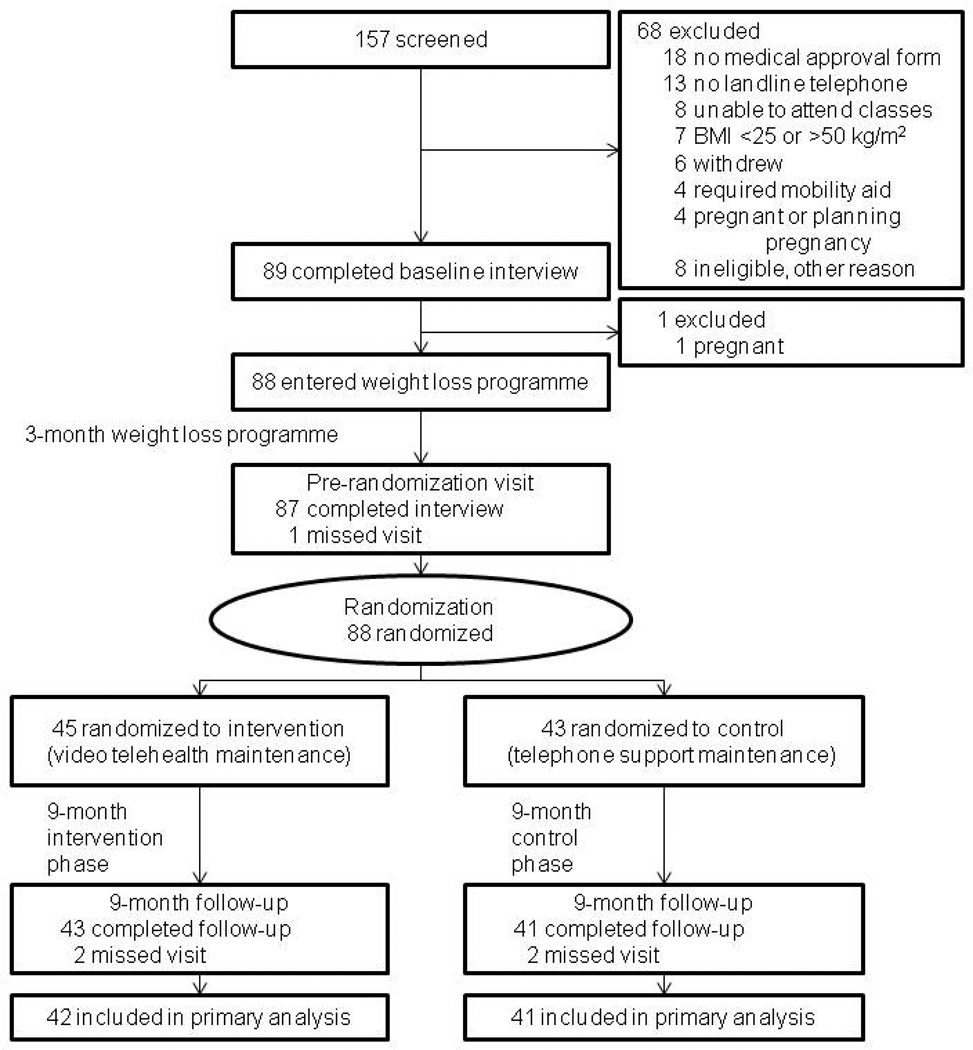
A total of 157 African-American women were screened for study inclusion (Figure 2). 89 women completed the baseline interview and 88 completed the weight-loss programme.
Figure 2.
Participant flow. Only participants with weight data at both the pre-randomization visit and the 9-month follow-up visit were included in the primary analysis.
For the first cohort, one church was randomized to each group using a software application (see Figure 1). The second cohort was switched so that women from the church which had received the control, received the intervention, and vice versa.
Weight maintenance -- intervention
Women in the intervention arm received monthly telephone support calls during the weight maintenance phase (average duration 10–12 min). E-mail and Listserv communication was also available for participants.
During their final weight loss class, participants were introduced to the home video-based programme for the maintenance phase with a demonstration of the DVR. Afterwards, they received DVRs with wireless adapters or wired connections for Internet access. A technician was available for home visit installation and instruction. As the recorders were typically connected to living room television sets, the videos could be viewed at routine television watching times. In addition, efforts were made to arrange space near the televisions for home exercise.
There were three channels of video content for participant viewing. One channel was informational and showed brief videos to reinforce healthy eating and physical activity (each video was approximately 5–20 min in duration). This channel included videos of the instructor (reminders, motivational talks and problem solving ideas); cooking and grocery shopping; narrative stories from participants recorded during the weight loss maintenance phase; and other programmes (e.g. SisterTalk, a health programme for African-American women).[6] The other two channels included exercise videos (beginning and advanced), such as “Sit and Be Fit” and “Walk Away the Pounds.” Participant DVR use was monitored every two weeks via server reports, including data on successful server connections, downloads and individual viewing durations.
Weight maintenance -- control
Women in the control arm received monthly telephone support calls during the weight maintenance phase (average duration 10–12 min).
Measurements
Measurements were made at baseline, following the 3-month weight loss programme, and at the end of the 9-month weight maintenance phase. Height was measured to the nearest 0.1 cm using a portable, calibrated stadiometer. Bodyweight was measured to the nearest 0.1 kg with the participant wearing light clothing and no shoes, using a portable, calibrated, digital scale.
Baseline demographic information obtained included age, income, highest education level, employment and marital status. Television-watching and computer use was assessed with the questions “How many hours of television do you usually watch each day?” and “How often do you use a computer at work or at home?”
The Block Brief 2000 Food Frequency Questionnaire (FFQ) included a 70-item food list. Participants were asked how often they ate each item in the past year and approximately how much they ate each time.[7] We used the short version of the International Physical Activity Questionnaire (IPAQ) to assess physical activity.[8] Participants were asked how many days per week and how much time per day they walked, engaged in moderate activity, or engaged in vigorous activity for at least 10 min at a time in the previous 7 days. In addition, they were asked how much time they spent sitting on a weekday during the previous 7 days. We calculated the average length of time per day spent in each type of activity, as well as the average length of time per day spent in all moderate to vigorous physical activity (MVPA), including walking.
The social support and self-efficacy questionnaires were based on measures developed by Sallis et al.[9, 10] To assess social support, participants were asked to rate how often family members and anyone else living in the household offered various forms of encouragement or discouragement for changes in diet or physical activity. They were then asked the same questions about friends, acquaintances and co-workers. Ratings were made on a 5-point scale (1=never to 5=very often). To assess diet and activity self-efficacy, participants were asked: “Rate how confident you are that you could really motivate yourself to do things like these consistently, for at least six months.” They responded using a 5-point scale (1=I know I cannot to 5=I know I can).
Statistical methods
We hypothesized that weight loss maintenance would be greater among women in the intervention group compared to the control group at the 9-month follow-up visit. We used two-sample t-tests to test for differences between groups in weight change and BMI change from randomization to 9-month follow-up. For our primary analysis, subjects in the intervention group were analysed together, independent of actual DVR use. However, we also conducted a secondary analysis including only intervention participants with a functioning DVR, as well as an intention-to-treat analysis in which the baseline weight was used to impute one missing weight value at the pre-randomization visit and 4 missing weight values at 9-month follow-up. In addition, we used an analysis of covariance to test for differences between groups in weight change, adjusting for baseline weight, weight change from baseline to randomization, baseline age, number of weight loss intervention classes attended, number of other adults in the household at baseline, TV viewing at randomization and cohort.
Changes in diet, social support and self-efficacy from randomization to follow-up were also analysed using two-sample t-tests. Participants who reported total energy <500 kcal/day or >5000 kcal/day were excluded from all analyses of dietary intake, since those records were considered invalid. For the physical activity variables, which were known to have non-normal distributions [11], we used Wilcoxon rank sum tests to test for differences between groups in change from randomization to 9-month follow-up.
To test for differences between groups at randomization, we used t-tests for most continuous variables, the Wilcoxon rank sum test for skewed income and physical activity variables, and chi-square tests for categorical variables. Spearman’s rank correlation coefficients were used to test for associations with DVR use among women in the intervention group and for associations with BMI change from randomization to follow-up.
Results
A total of 88 African-American women were enrolled in the study. During the 3-month weight-loss programme, the mean weight loss was significant: −0.8 kg (95% CI −1.4 to −0.2).
There were no significant differences between the intervention and control groups in age, education, income, marital status or employment (see Table 1). There were no significant differences between groups in weight, television viewing, computer use (every day or less often), diet, physical activity or self-efficacy. Women in the intervention group reported significantly higher levels of encouragement of healthy eating from family at randomization (12.0 vs. 9.6, P=0.02).
Table 1.
Participant characteristics at randomization
| Intervention (n=45) |
Control (n=43) |
All women (n=88) |
|
|---|---|---|---|
| Mean age, y (SD) | 50 (7) | 49 (8) | 50 (8) |
| Mean duration of education, y (SD) | 15 (2) | 15 (2) | 15 (2) |
| College graduates (%) | 26 (58) | 22 (51) | 48 (55) |
| Median household income, $000/y (25th, 75th percentile)a | 65 (35, 75) | 55 (35, 75) | 55 (35, 75) |
| Married or living with a partner (%) | 21 (47) | 18 (42) | 39 (44) |
| Employed full-time (%) | 33 (73) | 25 (58) | 58 (66) |
| Mean TV viewing, h/day (SD)a | 2.5 (1.8) | 2.0 (1.1) | 2.3 (1.5) |
| Uses computer almost every day or daily (%)a | 34 (77) | 37 (86) | 71 (82) |
n=87 for income, TV viewing and computer use, because of missing data
DVR use
In six cases a DVR could not be installed in the participant's home, generally because the participant refused or because she could not be reached to schedule installation. In 11 cases, the DVR was installed, but regular automatic video downloading and data collection were not fully enabled. A total of 28 DVRs were completely installed (62% of the intervention group).
During the intervention, the number of valid DVR viewings ranged from zero to 42 per person. An information channel viewing was counted as valid if it was at least 1 min long, and an exercise channel viewing was counted as valid if it was at least 5 min long. Among the 24 women with at least one valid viewing from a channel, the median number of viewings was nine. In total, there were 172 exercise channel viewings and 144 information channel viewings.
DVR use was associated with class attendance during the prior weight loss programme. On average, women who attended more classes had more DVR viewings (r=0.41, P=0.005). Seventeen of the 25 women who attended at least half of the classes used the DVR at least once (68%), while only seven of the 20 women who attended fewer than half of the classes ever used the DVR (35%, P=0.03). There was a negative correlation between the number of DVR viewings and the number of adults in the household other than the participant (r=−0.30, P=0.05). There was no association between the number of DVR viewings and age, education, income or number of children in the household. There was no association between the number of DVR viewings and BMI, weight, TV viewing or computer use. There was also no significant association between the number of DVR viewings and weight loss, energy change or MVPA change. Self-reported television viewing did not change significantly from randomization to 9-month follow-up (mean change 0.1 hr/day, 95% CI −0.2 to 0.4). There was no significant difference between groups in TV viewing change (mean change 0.0 hr/day in the intervention group vs. 0.3 hr/day in the control group, P=0.27).
Weight and BMI change
The bodyweight and BMI change from randomization to 9-month follow-up are shown in Table 2. There was no significant difference in weight change between groups, regardless of whether intervention women without functioning DVRs were included in the analysis. Results were similar after adjusting for baseline weight, weight change from baseline to randomization, age, number of weight loss intervention classes attended, number of other adults in the household at baseline (0, 1, >1), TV viewing at randomization and cohort. Adjusted mean (SE) weight change was 0.1 (0.6) kg in the intervention group and −0.2 (0.6) kg in the control group (P=0.69). An intention-to-treat analysis using the baseline weight in place of missing values at randomization or follow-up also yielded similar conclusions: mean (SD) weight change was 0.5 (3.7) kg in the intervention group and −0.1 (3.8) kg in the control group (P=0.47, n=88).
Table 2.
Weight/BMI change from randomization to 9-month follow-up
| Value at randomization | Change, randomization to 9-month follow-up |
||||
|---|---|---|---|---|---|
| Intervention Mean (SD) |
Control Mean (SD) |
Intervention Mean (SD) |
Control Mean (SD) |
Difference between groups P-valuea |
|
| All participantsb | n=42 | n=41 | |||
| Weight, kg | 90.7 (15.9) | 93.3 (16.0) | 0.6 (3.9) | 0.0 (3.8) | 0.46 |
| BMI, kg/m2 | 34.0 (5.4) | 34.8 (6.0) | 0.2 (1.5) | 0.0 (1.5) | 0.47 |
| Intervention participants with DVRc | n=28 | n=41 | |||
| Weight, kg | 91.5 (17.4) | 93.3 (16.0) | 0.5 (4.1) | 0.0 (3.8) | 0.61 |
| BMI, kg/m2 | 34.5 (6.1) | 34.8 (6.0) | 0.1 (1.6) | 0.0 (1.5) | 0.62 |
From two-sample t-test.
Participants with weight measured at both randomization and follow-up.
Participants with weight measured at both randomization and follow-up, excluding intervention participants who did not use the DVR.
BMI change from randomization to follow-up was negatively correlated with BMI change during the weight loss phase (r=−0.35, P=0.001) and positively correlated with the number of classes attended (r=0.25, P=0.02). BMI change during the maintenance period was not associated with baseline age, education, income, number of children or other adults in the household. BMI change during maintenance was also not associated with BMI, weight, TV viewing or computer use at randomization, or with changes in energy intake or MVPA during maintenance.
Change in diet, physical activity, social support, and self-efficacy
Changes in diet from randomization to 9-month follow-up are shown in Table 3. Changes in consumption of energy, fat, saturated fat, fibre, fruits and vegetables did not differ significantly between groups. Changes in physical activity during the maintenance period are shown in Table 4. Overall MVPA change was similar in the two groups (P=0.49), but moderate activity levels were better maintained in the intervention group than in the control group (median=0.0 min/day vs. −3.6 min/day, P=0.01). There were no differences between groups for any of the social support or self-efficacy scales (Table 5).
Table 3.
Diet change from randomization to 9-month follow-up. Only participants with valid diet data at baseline, randomization and 9-month follow-up were included in the analyses. Food frequency questionnaires with energy <500 kcal or >5000 kcal were excluded from the analysis.
| Value at randomization | Change, randomization to 9-month follow-up |
||||
|---|---|---|---|---|---|
| Intervention Mean (SD) n=38 |
Control Mean (SD) n=37 |
Intervention Mean (SD) |
Control Mean (SD) |
Difference between groups P-valuea |
|
| Energy, kcal/day | 1498 (475) | 1496 (709) | −36.2 (463.8) | 7.6 (506.4) | 0.70 |
| Fat, % kcal | 38.4 (7.7) | 36.7 (7.5) | −1.1 (8.2) | 1.6 (5.4) | 0.11 |
| Saturated fat, % kcal | 11.9 (2.5) | 11.7 (2.8) | −0.1 (2.4) | 0.4 (2.1) | 0.31 |
| Fiber, g/1000 kcal | 13.1 (4.5) | 12.5 (5.0) | −0.1 (4.9) | −0.3 (3.8) | 0.90 |
| Fruits, daily frequency | 1.9 (0.9) | 1.6 (0.8) | 0.0 (0.9) | −0.2 (0.8) | 0.31 |
| Vegetables, servings/day | 4.4 (2.4) | 4.0 (2.5) | −0.5 (2.9) | 0.1 (1.4) | 0.29 |
From two-sample t-test
Table 4.
Physical activity change from randomization to 9-month follow-up
| Value at randomization | Change, randomization to 9-month follow-up | ||||
|---|---|---|---|---|---|
| Intervention Median (25th, 75th percentile) n=40 |
Control Median (25th, 75th percentile) n=40 |
Intervention Median (25th, 75th percentile) |
Control Median (25th, 75th percentile) |
Difference between groups P-valuea |
|
| MVPAb, min/day | 45.7 (31.8, 88.6) | 57.9 (29.3, 128.6) | −6.6 (−26.4, 9.3) | −11.4 (−47.9, 16.8) | 0.49 |
| Walking, min/day | 21.4 (10.0, 32.1) | 17.1 (6.8, 60.0) | −5.0 –(17.9, 2.9) | 0.7 (−15.7, 19.3) | 0.17 |
| Moderate activity, min/day | 7.9 (2.5, 14.6) | 8.6 (3.2, 30.0) | 0.0 (−6.1, 10.0) | −3.6 (−17.1, 0.4) | 0.01 |
| Vigorous activity, min/day | 17.1 (5.0, 25.7) | 15.0 (5.7, 34.3) | −4.3 (−17.1, 0.0) | −6.4 (−21.4, 12.1) | 0.76 |
| Sitting on weekday, min/day | 360 (240, 450) | 240 (120, 390) | 60 (−120, 135) | 0 (−120, 75) | 0.36 |
From Wilcoxon rank sum test. Only participants with complete physical activity data at baseline, randomization, and 9-month follow-up were included in the analysis.
Moderate to vigorous physical activity, sum of time spent walking or in moderate or vigorous activity.
Table 5.
Social support and self-efficacy change from randomization to 9-month follow-up
| Value at randomization | Change, randomization to 9-month follow-up |
||||
|---|---|---|---|---|---|
| Intervention Mean (SD) n=41 |
Control Mean (SD) n=40 |
Intervention Mean (SD) |
Control Mean (SD) |
Difference between groups P-valuea |
|
| Social support scales | |||||
| Healthy eating encouragement, familyb | 12.0 (4.5) | 9.6 (4.4) | −0.9 (5.4) | 0.7 (3.5) | 0.12 |
| Healthy eating discouragement, familyc | 7.9 (3.2) | 8.1 (3.3) | 0.5 (3.0) | −0.3 (3.4) | 0.28 |
| Healthy eating encouragement, friendsb | 10.7 (4.9) | 10.8 (4.5) | −0.4 (4.0) | −1.2 (3.6) | 0.36 |
| Healthy eating discouragement, friendsc | 7.1 (3.2) | 6.8 (3.1) | 0.3 (2.7) | 0.0 (2.9) | 0.61 |
| Exercise, familyd | 8.3 (3.4) | 7.7 (3.7) | −0.4 (3.5) | −0.5 (3.3) | 0.96 |
| Exercise, friendsd | 7.6 (3.5) | 7.3 (3.7) | −0.3 (3.8) | −0.1 (4.2) | 0.78 |
| Self-efficacy scalese | |||||
| Healthy eating | 4.1 (0.7) | 3.9 (0.7) | −0.2 (0.7) | 0.0 (0.8) | 0.12 |
| Exercise | 3.8 (0.8) | 3.6 (0.9) | −0.5 (0.9) | −0.2 (1.1) | 0.11 |
From two-sample t-test. Only participants with complete social support/self-efficacy data at baseline, randomization and follow-up were included in the analyses
Theoretical range: 4 (low encouragement) to 20 (high encouragement)
Theoretical range: 3 (low discouragement) to 15 (high discouragement)
Theoretical range: 3 (low support) to 15 (high support)
Mean of 3 items with responses on a scale from 1 (I know I cannot) to 5 (I know I can)
Discussion
The present study examined weight loss maintenance support to African-American women provided through home video telehealth. There was no difference in weight maintenance after nine months among video telehealth participants compared with the control group. This may have been related to limited DVR use, lack of efficacy of video-based support or other barriers to weight loss maintenance. Ideally, a video telehealth programme would be less affected by some of the barriers that prevent women from attending face-to-face classes, such as work, transportation and child care. However, other problems, such as sustaining motivation, plentiful access to high caloric foods, and an environment that favours sedentary behaviour, probably affect people receiving either face-to-face or video telehealth support.
Weight regain is a common problem following weight loss treatment.[4] Our results are consistent with other interventions specifically designed for African-American women, and reflect the difficulty in obtaining and maintaining weight loss in this population.[12–15] Successful weight maintenance probably requires social support and well-developed problem solving and self-regulatory skills.[16]
Like the Internet use group of the WLM trial [17], our DVR programming was designed to encourage behavioural and self-management skills and provide culturally relevant nutrition and physical activity programming. Participants were sent information and exercise programmes weekly to sustain engagement in the intervention. Unfortunately, 21 of the participants (47%) did not engage in DVR viewing, despite access to the service in the home. Furthermore, participants were offered the opportunity to communicate with an instructor by email and with the group as a whole using a Listserv, but they made little use of these options (data not shown). Similar results have been observed in other telehealth studies including African-Americans.[18]
One important finding from the present study is that women who attended more weight loss classes during the pre-randomization phase were also more likely to utilize the home DVR during the maintenance period. People who enrolled in the study but remained absent from classes may not have been committed to weight loss opportunities, and less motivated to participate in the technology-based approach to weight maintenance. We also suspect that greater preparation was necessary in introducing women to the video telehealth programme.
In our study email prompting had a limited effect (data not shown), possibly due to the fact that the video content was not directly accessible from a hyperlink in the message. Telephone encouragement from the instructor was helpful for some participants (data not shown). It has been argued that “supportive accountability” may improve video telehealth utilization when the source of support is perceived as a trustworthy expert.[19] In addition, other adults in the household may compete for television use, resulting in lesser utilization of the weight maintenance video content. However, some participants did note a positive effect on other family members (particularly children) also viewing the videos.
The present study had certain strengths. First, the participants were African-American women, who have been infrequently included in previous telehealth studies. Second, intervention materials were viewed on television sets, making it easier to integrate them into daily routines. Third, the Internet-enabled DVRs allowed us to collect detailed information on whether the DVRs were functioning correctly (connecting to the server and downloading content) and on each participant’s viewing habits (video viewed, view duration and time of day). In comparison, DVD (“disc”) interventions typically rely on self-report to establish fidelity.
There were also significant limitations to the study, including a small sample size and the lack of utilization of the technology which occurred.
In summary, we did not observe an improvement in weight maintenance in the video telehealth group. There was limited home video DVR use. Other approaches have been found to be successful in improving weight loss, and studies are needed to identify their role in weight maintenance among African-American women.
Acknowledgements
The study was supported by NIH grant NIDDK R21 DK078352. We thank Sandra Franklin and the participating women and churches.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132:2087–20102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 3.Bray GA, Bouchard C. Handbook of Obesity : Clinical Applications. 2nd ed. New York: Marcel Dekker; 2004. [Google Scholar]
- 4.Hill JO, Thompson H, Wyatt H. Weight maintenance: what's missing? J Am Diet Assoc. 2005;105(5 Suppl 1):S63–S66. doi: 10.1016/j.jada.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Cardinal BJ, Esters J, Cardinal MK. Evaluation of the revised physical activity readiness questionnaire in older adults. Med Sci Sports Exerc. 1996;28:468–472. doi: 10.1097/00005768-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Gans KM, Kumanyika SK, Lovell HJ, et al. The development of SisterTalk: a cable TV-delivered weight control program for black women. Prev Med. 2003;37:654–667. doi: 10.1016/j.ypmed.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. 1990;1:58–64. doi: 10.1097/00001648-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 9.Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR. The development of selfefficacy scales for health related diet and exercise behaviors. Health Educ Res. 1988;3:283–292. [Google Scholar]
- 10.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 11.Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ) See http://www.ipaq.ki.se/scoring.pdf (last checked 12 March 2013)
- 12.Stolley MR, Sharp LK, Oh A, Schiffer L. A weight loss intervention for African American breast cancer survivors, 2006. Prev Chronic Dis. 2009;6:A22. [PMC free article] [PubMed] [Google Scholar]
- 13.Walcott-McQuigg JA, Chen SP, Davis K, Stevenson E, Choi A, Wangsrikhun S. Weight loss and weight loss maintenance in African-American women. J Natl Med Assoc. 2002;94:686–694. [PMC free article] [PubMed] [Google Scholar]
- 14.Martin PD, Dutton GR, Rhode PC, Horswell RL, Ryan DH, Brantley PJ. Weight loss maintenance following a primary care intervention for low-income minority women. Obesity (Silver Spring) 2008;16:2462–2467. doi: 10.1038/oby.2008.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Djuric Z, Mirasolo J, Kimbrough L, et al. A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. J Natl Med Assoc. 2009;101:552–564. doi: 10.1016/s0027-9684(15)30940-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnes AS, Goodrick GK, Pavlik V, Markesino J, Laws DY, Taylor WC. Weight loss maintenance in African-American women: focus group results and questionnaire development. J Gen Intern Med. 2007;22:915–922. doi: 10.1007/s11606-007-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 18.Gustafson DH, McTavish FM, Stengle W, et al. Use and Impact of eHealth System by Low-income Women With Breast Cancer. J Health Commun. 2005;10(Suppl 1):195–218. doi: 10.1080/10810730500263257. [DOI] [PubMed] [Google Scholar]
- 19.Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res. 2011;13:e30. doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]