Abstract
Objectives
To describe ambulatory care clinicians’ perspectives on the effect of e-prescribing systems on patient safety outcomes.
Study Design
We used a mixed-method study of clinicians and staff in 64 practices using one of six e-prescribing technologies in six U.S. states.
Methods
We used clinician surveys (web-based and paper) and focus groups to obtain clinicians’ perspectives on e-prescribing and patient safety.
Results
Providers highly valued having medications prescribed by other providers on the medication list and the ability to access patients’ medication lists remotely. Providers felt that there will always be prescription or medication errors and that the implementation of e-prescribing software changes rather than eliminates prescription or medication errors. New errors related to the dosing or scheduling of a medication, accidentally prescribing the wrong drug, or duplicate prescriptions.
Conclusions
Lessons from the ambulatory care trenches must be considered as technology moves forward so that the hypothesized patient safety gains will be realized.
Keywords: electronic prescribing, primary care, technology assessment
I. INTRODUCTION
The purpose of this study is to describe ambulatory care clinicians’ perspectives on the effect of electronic prescribing systems on patient safety.
II. BACKGROUND
According to the 2001 National Ambulatory Medical Care Survey, 61.9% of all outpatient office visits resulted in a clinician prescribing at least one medication.1 During 2001, an estimated 1.3 billion medications were prescribed during outpatient office visits with an estimated average of 2.4 prescriptions per medication-related office visit.1 The Institute of Medicine (IOM) report, To Err is Human, Building a Safer Health System, estimated that medication errors were responsible for more than 7,000 deaths annually.2 Given that at least $887 million is spent on preventable adverse drug events among Medicare recipients in the ambulatory setting,3 systems to prevent medication errors in ambulatory settings are sorely needed.
Electronic prescribing (e-prescribing) systems hold promise to improve the safety, quality, and efficiency of health care.4 While e-prescribing is the direct computer-to-computer transmission of prescription information from physician offices to pharmacies, these systems also allow for patient safety features including clinical decision support and sharing of patient pharmacy data across multiple prescribers. Great strides have been made to address the regulatory and high-level operational issues required to permit this form of prescribing. In 2004 only about half of U.S. states allowed e-prescribing, but by August 2007 all 50 states and Washington, D.C. had implemented regulations permitting this form of prescribing.5 Further, in 2006, 95% of software systems used by U.S. pharmacies have been certified on at least one electronic “highway” connecting physician offices to retail pharmacies.5 In 2006 and 2007, electronic prescribing transactions saw quarterly growth of 26% and 30%.5 While e-prescribing adoption increases in the U.S., a greater understanding of the role of e-prescribing technology solutions to improve patient-centered pharmacy care is warranted.
A large one-year study conducted to evaluate proposed standards for new e-prescribing transactions provided the opportunity to evaluate healthcare providers’ opinions about the role of e-prescribing applications in improving patient safety. This study summarizes qualitative and quantitative data collected via focus groups and surveys of 64 practices spread out across six states and using one of six different e-prescribing software systems. No study to date has been performed at this scale. Including multiple vendors in multiple practice settings provides a unique opportunity to fully understand perceptions of patient safety owing to electronic prescribing in primary care settings.
III. RESEARCH QUESTION
What are ambulatory care clinicians’ perspectives on the extent to which e-prescribing features influence patient safety outcomes?
IV. METHODS
A. Study sample
The Brown University Institutional Review Board (IRB) approved the study protocol. SureScripts, LLC, the nation’s largest e-prescribing network, identified states with the highest e-prescribing activity on their network in the fall of 2005. To provide geographic diversity while considering practical and logistical issues, we selected six states with the highest volume of e-prescribing transactions to be targeted for inclusion in the study: Florida, Massachusetts, New Jersey, Nevada, Rhode Island, and Tennessee. Within these states, SureScripts, LLC, identified physician software vendors with substantial activity who agreed to participate in the study: OnCallData, InstantDX, LLC, Gaithersburg, MD in Rhode Island, PocketScript, Zix Corporation, Dallas, TX; Rcopia in Massachusetts and New Jersey, DrFirst, Inc., Rockville, MD in Massachusetts, Care360, Medplus, Inc., Mason, OH in New Jersey and Florida, eMPOWERx, GoldStandard Multimedia, Inc., Tampa, FL in Florida, and Touchworks, AllScripts, LLC, Chicago, IL in Nevada and Tennessee. All physician software systems were required to assist in recruitment of ambulatory care practices with a patient-mix of at least 25% Medicare eligible patients. We developed participation agreements (approved by the Brown IRB) and provided recruitment packets and training of information in the recruitment packets for each company. The resulting practices represented a convenience sample, as companies approached practices with whom they had positive relations and who had participated in research previously. Thus, we are unable to estimate participation rates among potentially eligible practices. The data for the current study were derived from clinician surveys and focus groups. All data were collected before any changes to the electronic prescribing software were made to accommodate the electronic prescribing standards.
B. Clinician surveys
Clinicians (n=157) completed surveys available via the web (75%) or paper (25%) in advance of or during the site-visit. The survey captured perceptions of the impact of e-prescribing on efficiency, workflow, and quality and clinician views on patient communication regarding medication issues (Appendix A). The survey included two questions regarding the impact of e-prescribing on patient safety and quality of care (Figures). We estimated the clinician responses to the drug alerting questions for each physician software system. Vendor-specific results are presented without identifying the name of the vendor. To provide context in which to evaluate differences in these proportions, we described the software in relation to frameworks on recommended best practices for e-prescribing software.6,7 Two trained interviewers who had received one-on-one instruction regarding the functionality of all of the software products independently evaluated each product in relation to the sixty recommendations. They coded each recommendation as being fully implemented, partially implemented, not at all implemented, or not applicable. Summary proportions for each conceptual domain were estimated from the sixty recommendations.
C. Focus Groups
Two highly trained research assistants held focus groups (with a meal provided) before hours, at lunch, or after hours at the discretion of each practice between April and August 2006. A total of 276 clinicians and staff members participated in 64 focus groups after providing written informed consent. A sign listing the main topics for discussion was placed on the table for participants to view (Table 1). We used an open-ended approach to elicit information about the benefits and drawbacks of e-prescribing, as well as the features often embedded with the e-prescribing software. Participants were encouraged to describe their experiences with e-prescribing software and to provide suggestions for improving e-prescribing. Probes included questions about what aspects of e-prescribing are valuable, what participants found difficult, suggested improvements in office procedures and software functionality, and other potentially valuable resources. Research assistants also used facilitative (e.g., “Can you tell me more about that?” or “Any other opinions?”) and clarifying (e.g., “When you say …, what do you mean by that?”) probes. Participants spontaneously addressed patient safety issues in the context of these discussions. Focus groups were recorded using two digital recorders with PZM microphones. Once all digital recordings were transcribed, research assistants double-checked every transcript for potential errors.
Table 1.
Focus Group Discussion Topics
|
Qualitative methods are useful for studying complex phenomena such as communication, thoughts, expectations, and meaning and for investigating people’s experiences.8–10 An extensive hierarchical coding structure was initially developed to handle the large volume of qualitative data (Appendix B). This initial structure was based on the focus group protocol and review of initial transcripts and was revised during active coding. Fifteen different parent nodes were defined to code all of the qualitative data. For this manuscript, we honed in on the analysis of two nodes: impact on clinical practice and software features because many e-prescribing software packages had additional features that may influence patient safety. Coders were instructed to include any comments regarding “patient safety” in a sub-node specifically for this purpose. We also evaluated text coded under “quality of care” as patient safety issues were sometimes referred to in the context of quality of care.
Coders were trained in coding definitions and overall coding structure. A code book defined all codes and their relationships. All quotes were derived from the focus groups and individual interviews. We did not include information on drug alerts as part of this analysis as the extensive nature of the findings related to drug alerts warranted a separate analysis.11
Consistency in the coding across team members was assured by extensive training, coding meetings, a common codebook, and group exercises. We also had two members of the coding team independently code approximately 20% of transcripts and compared reports to identify any areas of coding that were not consistently applied by coders and for which additional training was required. A qualitative data review of the double-coded transcripts revealed that passages coded by each coder commonly appeared twice, indicating effective coding among those transcripts by the research staff. Management and analysis of the data was conducted using NVivo qualitative analysis software (Version 7, QSR International, Melbourne, Australia).
V. RESULTS
A. Sample Characteristics
Overall, all software vendors fully implemented at least half of best practices recommendations (range: 63% to 82%; Table 2). All security and confidentiality recommendations were met by all vendors. The proportion of recommendations fully implemented for other domains displayed significant variation across software vendors.
Table 2.
Implementation of Best Practices Recommendations by E-prescribing Software (% of recommendations fully implemented)
| SOFTWARE VENDOR | ||||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| Overall recommendations fully implemented | 77 | 82 | 62 | 63 | 73 | 63 |
| Patient identification and data access | 100 | 100 | 100 | 50 | 75 | 100 |
| Current medications/medication history | 87.5 | 87.5 | 75 | 50 | 62.5 | 75 |
| Medication selection | 64 | 93 | 57 | 50 | 64 | 64 |
| Alerts and other messages to prescribers | 83 | 83 | 42 | 67 | 75 | 50 |
| Patient education | 100 | 50 | 100 | 100 | 100 | 100 |
| Data transmission and storage | 71 | 86 | 43 | 86 | 86 | 57 |
| Monitoring and renewals | 40 | 60 | 40 | 40 | 20 | 40 |
| Transparency and accountability | 50 | 0 | 50 | 100 | 100 | 0 |
| Prescriber-level feedback | 100 | 50 | 100 | 50 | 100 | 50 |
| Security and confidentiality | 100 | 100 | 100 | 100 | 100 | 100 |
Thirty percent of practices were solo practices, 30% were single specialty groups, and 19% were multi-specialty groups. Nearly 40% of the practices were family medicine and 45% were internal medicine. Patient case-mix included a mean of 43% (SD: 26%) eligible for Medicare. While focus groups (n=64 involving 276 participants) were comprised mostly of prescribers (physicians, residents, nurse practitioners, and physician assistants; 64%), medical assistants (12%), nurses, office managers, pharmacists, and other office staff also participated in the focus groups. Eighty percent of survey respondents were physicians.
B. Quantitative Analysis
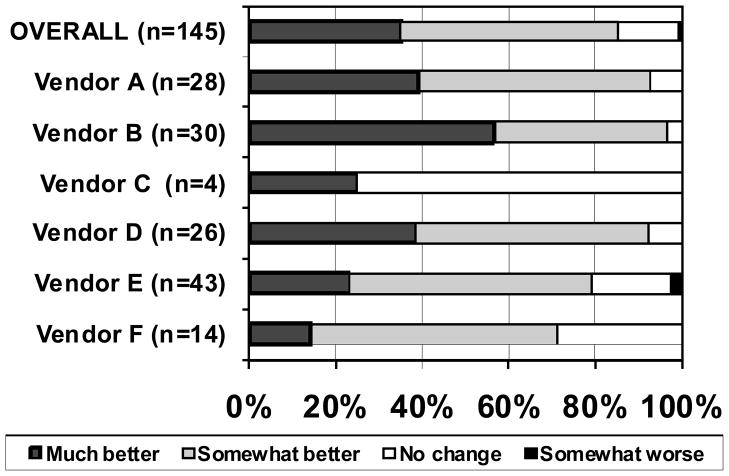
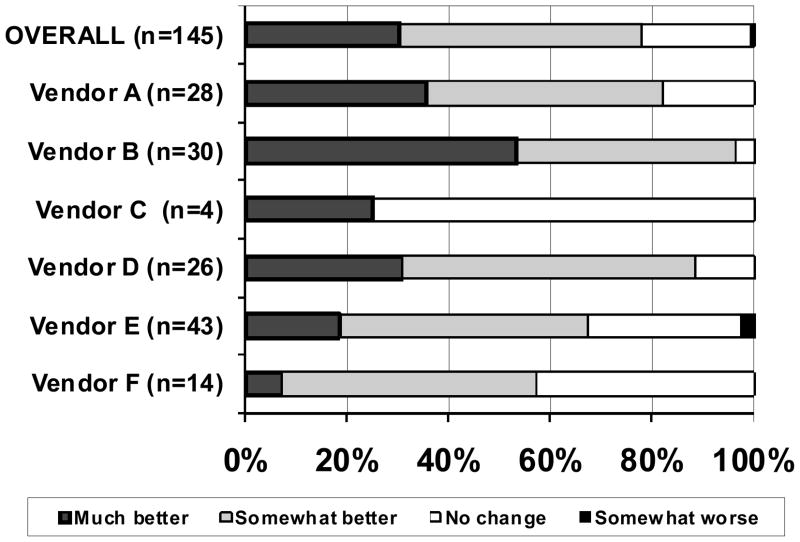
Of the 157 clinicians who completed the survey, 3 reported not using e-prescribing and 9 did not answer the two questions of interest (4 clinicians using software from Vendor D and 5 from Vendor E). Overall, 35% of responders felt that e-prescribing was much better than other methods in terms of patient safety, and an additional 50% reported that e-prescribing was somewhat better (Figure 1). There was variation across software vendor; the proportion of clinicians who felt that e-prescribing was somewhat or much better than other methods of prescribing ranged from 25% to over 95%. Only one clinician reported a negative view of e-prescribing in relation to each patient safety and quality of care. The proportion of clinicians who felt that e-prescribing was somewhat or much better than other methods of prescribing with respect to impact on quality care ranged from a little 25% to over 95% depending on software vendor; overall 78% of clinicians surveyed felt that e-prescribing was much or somewhat better (Figure 2).
Figure 1.
Perceptions of the impact of e-prescribing on patient safety, overall and by e-prescribing technology solution, % of sample
The participant survey asked “how do electronic prescriptions (submitted by your computer directly to the pharmacy’s computer) compare to other prescription methods you use… in terms of patient safety?” From left to right, the dark grey bars represent the percentage of participants who responded “much better”, the light grey bars “somewhat better”, the white bars “no change”, and the black bars “somewhat worse.” No respondents indicated that electronic prescribing was “much worse” than other prescription methods in terms of patient safety.
Figure 2.
Perceptions of the impact of e-prescribing on quality of care, overall and by e-prescribing technology solution, % of sample
The participant survey asked “how do electronic prescriptions (submitted by your computer directly to the pharmacy’s computer) compare to other prescription methods you use… in terms of quality of care?” From left to right, the dark grey bars represent the percentage of participants who responded “much better”, the light grey bars “somewhat better”, the white bars “no change”, and the black bars “somewhat worse”. No respondents indicated that electronic prescribing was “much worse” than other prescription methods in terms of quality of care.
C. Qualitative Analysis
Among users of e-prescribing software, a recurring theme was the importance of the medication list feature in improving patient safety. This feature was seen as a major advantage of e-prescribing. Participants reported using this feature to perform medication reconciliation. One participant noted, “[a patient] was basically on everything the same thing he had before except for one… He didn’t remember, but I knew it from the list. … It helps in reduction of errors. It helps in compliance because you see when they get it and when they don’t get it.” Another highly-valued e-prescribing software feature was the ability to know what medications were prescribed by other providers. One participant claimed to “love the fact that you get the drugs that were prescribed in urgent care are already on the list because nine of out ten patients when they come in for their follow-up – which urgent care always tells them to do—they don’t remember which medicine they were put on.” Although participants clearly articulated the patient safety value of having a medication list at the point of prescribing, the accuracy of the lists was questioned by some. Complaints about short-term medications (such as antibiotics) remaining indefinitely on the lists varied among the specific e-prescribing software. Complaints about not having complete information on all of patients were common. Overall, participants greatly valued the ability to access medication lists remotely. Clinicians commented on the need to prescribe after hours or away from their patients’ records. Remote access to the medication list was believed to improve patient safety. Some participants reported printing the medication list for their patients. According to one participant, “it really helps because at least they can take it home and call us back and clarify any differences between the two.”
Improved legibility was also perceived as a major benefit of e-prescribing. However, participants felt that there will always be prescription or medication errors, and that the implementation of e-prescribing software would change rather than eliminate errors. A major type of error related to the dosing or scheduling of a medication. Other types of errors included accidentally prescribing the wrong drug or duplicate prescriptions. As one participant reported: “I’ve seen things where the staff handled a refill request and picked the wrong drug, a similar sounding name…I could have very easily prescribed the wrong drug or the wrong dosage.” Participants reported that errors occurred because of difficulty distinguishing between items in menus or because of errors selecting options. Factors leading to selecting the wrong agents included the small size of hand-held devices and columns too close together on the display. As one participant noted about a prescription “ somehow got switched… the viewing screen on that handheld is small, and it was a combination medicine. I couldn’t see all the components… he was getting one that contained aspirin instead of Acetaminophen. He was somebody who shouldn’t be getting aspirin. And he had a serious complication from that.” Participants suggested ordering medications in ascending or descending order to prevent mistakes. Participants reported that medication errors stemming from e-prescribing were typically caught by the pharmacists, error checking within the e-prescribing software, or patients. Table 3 summarizes key issues emerging from the focus groups.
Table 3.
Summary of Key Advantages and Concerns of E-prescribing on Patient Safety that Emerged from the Focus Groups
| Patient safety advantages | Patient safety concerns |
|---|---|
| Value in doing medication reconciliation at point of prescribing | Validity and completeness of the information regarding medication |
| Knowing medications prescribed by other providers | Accidentally prescribing duplicate medications |
| Remote access to patients’ medication lists so when prescribing new medications offsite it is done with knowledge of medication regimen | Drop down menu issues resulting in wrong drug or dose being prescribed |
| Ability to share list of medications with patients so they can use it at home to check against actual medicines | Small screen size on handheld devices leads to wrong drug or dose being prescribed |
| Reduces errors due to illegibility of handwriting | Order of drop down menus leads to wrong drug or dose being prescribed |
VI. DISCUSSION
This multi-state, multi-vendor study confirms the value of e-prescribing for patient safety. Consistent with a recent study based on only one e-prescribing product in one state,12 our study found that the majority of clinicians reported at least some improvements in patient safety and quality of care with e-prescribing. Our study extends previous work by identifying the concerns of users regarding new forms of medication errors resulting from e-prescribing. Participants provided clear areas for improvement, as well as suggestions for preventing medication errors.
An estimated 7.6% of outpatient prescriptions have prescribing errors,13 and 4.1% of new e-prescriptions and 2.1% of refill e-prescriptions require pharmacist intervention.14 Our findings echo the work by Gandhi et al.13 who argued that basic computerized prescribing systems may not be adequate to reduce errors. Our participants noted problems with dosages and directions which agrees with interviews with pharmacy personnel.15 An audit of pharmacist medication interventions found that 32% of e-prescriptions requiring intervention was due to missing information and 17.7% was due to dosing errors.14 While these data support the notion that more advanced systems with dose and frequency checking are needed to prevent potentially harmful errors, the extent to which such systems will be over-ridden remains unknown.11 Another strategy to reduce errors in instructions and dosing include the development and implementation of standards for terminology to code clinical drugs (RxNorm) and standards for medication instructions (structured and codified SIG). Indeed, a recent expert panel concluded that lack of unambiguous drug identifiers in proposed standards suggests that more work is needed.16
Our study demonstrated that specific aspects of the software and hardware (such as screen size, drop down menus, and order of choices) may contribute to the selection of wrong dose and drugs. Best practices should be identified by understanding the relation of errors with characterizations of the software and hardware used for e-prescribing using methods such as those conceptualized by Bell et al,6 operationalized via consensus method with an expert panel,7 and evaluated in a field study.17 The human factors engineering approach to the development of tools such as e-prescribing may identify potentially dangerous usability flaws.18,19
Participants in our study believed the availability of a medication list as part of the e-prescribing software improved patient safety. Our finding that participants used the medication list to reconcile medications with their patients confirms previous work that using e-prescribing systems in a standardized way to ensure accurate medication lists leads to significant patient safety gains.20 However, in another setting, when such data were provided, they were only accessed 0.6% of clinical encounters involving prescriptions.21 Our participants reported that medication lists were often incomplete or they did not have information on all of their patients. This is not surprising, as the extent to which bidirectional flow of medication history data from comprehensive data sources is highly variable and is hampered by product limitations and external challenges related to implementation including state variations in regulation of data and sharing of information across providers.22 Our data suggest that clinicians believe that further patient safety gains could be realized if comprehensive, accurate medication lists were available at the point of prescribing.
Our study is not without limitations. While non-response bias is possible, we do not know if participants were overly supportive of e-prescribing, or overly negative. It is likely that this convenience sample captured participants who are representative of the most experienced e-prescribing users in primary care settings. Because they were not new users, it may be that these participants liked the software enough to continue using it. Second, the data included in this report are from a geographically diverse group of physician practices using one of six e-prescribing products. The variability in the e-prescribing software may give rise to interesting hypotheses to be explored in future research. Concerns may exist over the purposeful sampling in this study. Yet, for qualitative analysis, purposefully selecting an informative sample is a valid approach and can increase the quality and information of the data. Nevertheless, even among e-prescribing users who are familiar with the technology, the findings did not appear to be overly optimistic regarding the impact of e-prescribing on patient safety in the ambulatory care setting.
VII. CONCLUSIONS
Regardless of e-prescribing software vendor, physicians representing diverse practice characteristics and locations overwhelmingly agree that functionality included in many e-prescribing systems offers a patient safety advantage relative to other forms of prescribing. Given the conservative estimate of 530,000 preventable ADEs occurring in outpatient settings,23 clinicians must have full knowledge of the current drug regimen to avoid preventable ADEs. While e-prescribing may be one method to improve patient safety related to medication errors, it is important to further identify and promote best practices to minimize a new generation of medication errors resulting from the adoption of this technology.
Synopsis
Using qualitative data from focus groups in 64 practices and surveys, this study describes what aspects of e-prescribing clinicians deem important towards improving patient safety.
Summary for non-clinicians
In the US, e-prescribing in clinical practice is not ubiquitous. Understanding what clinicians value from e-prescribing toward improving patient safety may help stimulate adoption. Clinicians viewed the following aspects to be most beneficial for patient safety:
E-prescribing enabled remote access to medication lists.
E-prescribing allowed clinicians to see what other providers were prescribing their patients.
While e-prescribing eliminated hand-writing errors in the prescribing process, clinicians feared a new generation of errors related to the technology.
Acknowledgments
Funding source: This study was funded by the Agency for Healthcare Research and Quality, Department of Health and Human Services (Grant # 1 U18 HS016394-01 entitled Maximizing the effectiveness of e-prescribing between physicians and community pharmacies).
VIII. REFERENCES
- 1.Cherry DK, Burt CW, Woodwell DA. National Ambulatory Medical Care Survey: 2001 Summary. Adv Data. 2003;337:1–44. [PubMed] [Google Scholar]
- 2.Institute of Medicine. To Err is Human: Building a Safer Health Care System. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 3.Field TS, Gilman BH, Subramanian S, Fuller JC, Bates DW, Gurwitz JH. The costs associated with adverse drug events among older adults in the ambulatory setting. Medical Care. 2005;43(12):1171–1176. doi: 10.1097/01.mlr.0000185690.10336.70. [DOI] [PubMed] [Google Scholar]
- 4.eHealth Initiative. [Accessed November 23, 2008.];Electronic Prescribing: Toward Maximum Value and Rapid Adoption. 2004 Available at: www.ehealthinitiative.org/assets/documents/eHIFullReport-ElectronicPrescribing2004.pdf.
- 5.SureScripts, LLC. [Accessed November 23, 2008.];National Progress Report on E-prescribing. 2007 Available at: www.surescripts.com/pdf/National-Progress-Report-on-Eprescrbing-1.pdf.
- 6.Bell DS, Cretin S, Marken RS, Landman AB. A conceptual framework for evaluating outpatient electronic prescribing systems based on their functional capabilities. J Am Med Inform Assoc. 2004 Jan-Feb;11(1):60–70. doi: 10.1197/jamia.M1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell DS, Marken RS, Meili RC, Wang CJ, Rosen M, Brook RH. RAND Electronic Prescribing Expert Advisory Panel. Recommendations for comparing electronic prescribing systems: results of an expert consensus process. Health Aff (Millwood) 2004 Jan-Jun;(Suppl Web Exclusives):W4-305-17. doi: 10.1377/hlthaff.w4.305. [DOI] [PubMed] [Google Scholar]
- 8.Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. The Lancet. 2001;358:397–400. doi: 10.1016/S0140-6736(01)05548-9. [DOI] [PubMed] [Google Scholar]
- 9.Sofaer S. Qualitative methods: what are they and why use them? Health Services Research. 1999;34:1101–1118. [PMC free article] [PubMed] [Google Scholar]
- 10.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311:42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lapane KL, Waring ME, Schneider KL, Dubé C, Quilliam BJ. A mixed method study of the value of drug alerts at point of e-prescribing in primary care. J Gen Intern Med. 2008;23(4):442–6. doi: 10.1007/s11606-008-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weingart SN, Simchowitz B, Shiman L, Brouillard D, Cyrulik A, Davis RB, Isaac T, Massagli M, Morway L, Sands DZ, Spencer J, Weissman JS. Clinicians’ assessments of electronic medication safety alerts in ambulatory care. Arch Intern Med. 2009 Sep 28;169(17):1627–32. doi: 10.1001/archinternmed.2009.300. [DOI] [PubMed] [Google Scholar]
- 13.Gandhi TK, Weingart SN, Seger AC, Borus J, Burdick E, Poon EG, et al. Outpatient prescribing errors and the impact of computerized prescribing. J Gen Intern Med. 2005 Sep;20(9):837–41. doi: 10.1111/j.1525-1497.2005.0194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warholak TL, Rupp MT. Analysis of community chain pharmacists’ interventions on electronic prescriptions. J Am Pharm Assoc 2003. 2009 Jan-Feb;49(1):59–64. doi: 10.1331/JAPhA.2009.08013. [DOI] [PubMed] [Google Scholar]
- 15.Rupp MT, Warholak TL. Evaluation of e-prescribing in chain community pharmacy: best-practice recommendations. J Am Pharm Assoc 2003. 2008 May-Jun;48(3):364–70. doi: 10.1331/JAPhA.2008.07031. [DOI] [PubMed] [Google Scholar]
- 16.Bell DS, Schueth AJ, Guinan JP, Wu S, Crosson JC. Evaluating the technical adequacy of electronic prescribing standards: Results of an expert panel process. AMIA Annu Symp Proc. 2008 Nov 6;:46–50. [PMC free article] [PubMed] [Google Scholar]
- 17.Wang CJ, Marken RS, Meili RC, Straus JB, Landman AB, Bell DS. Functional characteristics of commercial ambulatory electronic prescribing systems: a field study. J Am Med Inform Assoc. 2005 May-Jun;12(3):346–56. doi: 10.1197/jamia.M1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beuscart-Zéphir MC, Pelayo S, Bernonville S. Example of a Human Factors Engineering approach to a medication administration work system: Potential impact on patient safety. Int J Med Inform. 2009 Sep 7; doi: 10.1016/j.ijmedinf.2009.07.002. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Niès J, Pelayo S. From users involvement to users’ needs understanding: A case study. Int J Med Inform. 2009 Aug 4; doi: 10.1016/j.ijmedinf.2009.06.007. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Stock R, Scott J, Gurtel S. Using an electronic prescribing system to ensure accurate medication lists in a large multidisciplinary medical group. Jt Comm J Qual Patient Saf. 2009 May;35(5):271–7. doi: 10.1016/s1553-7250(09)35038-2. [DOI] [PubMed] [Google Scholar]
- 21.Simonaitis L, Belsito A, Overhage JM. Enhancing an ePrescribing system by adding medication histories and formularies: the Regenstrief Medication Hub. AMIA Annu Symp Proc. 2008 Nov 6;:677–81. [PMC free article] [PubMed] [Google Scholar]
- 22.Grossman JM, Gerland A, Reed MC, Fahlman C. Physicians’ experiences using commercial e-prescribing systems. Health Aff (Millwood) 2007 May-Jun;26(3):w393–404. doi: 10.1377/hlthaff.26.3.w393. Epub 2007 Apr 3. [DOI] [PubMed] [Google Scholar]
- 23.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older person in the ambulatory setting. JAMA. 2003;289(94):1107, 1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]