Smoking cessation interventions are widely underused in primary and secondary care despite being effective and easy to deliver (see earlier articles in this series). Smoking causes much greater harm than, say, hypertension (which is generally identified and managed entirely in primary care by health professionals working to agreed routine, systematic, and structured protocols), yet few primary healthcare teams manage smoking as methodically as they approach hypertension.
Maximising the delivery of cessation interventions to smokers wanting to quit can probably achieve more in terms of years of life saved and provide better value for money (see later article in this series) than almost any other simple medical intervention.
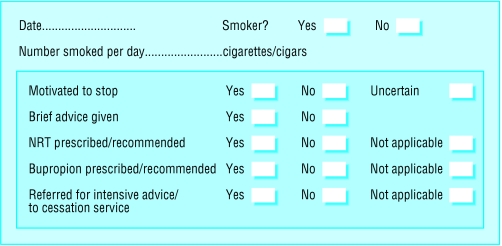
Figure 1.
Example of record sheet for noting information on smoking status and intervention. The sheet can be inserted into paper records; computer templates enable a similar electronic record to be kept
Smoking as a vital sign
The first step towards developing a systematic approach for the management of smoking is to treat smoking as a “vital sign.” To do this, health professionals must regularly inquire about patients' smoking status and have a methodical approach towards documenting and updating this in medical records. This information needs to be recorded in a prominent place so that it can be seen whenever medical records are accessed during consultations. In paper records, a summary card can be used, and, in electronic records, smoking status data should be lodged with other important summary information on a patient's health. Recording information where it is easily noticed prompts health professionals to raise the topic of smoking more frequently with patients.
The minimum information to record is whether the patient smokes and the date on which this was ascertained. It is also useful to record the average number of cigarettes smoked each day, not least because those who smoke more heavily are more likely to benefit from nicotine replacement therapy or bupropion therapy. Recording whether the smoker is interested in or motivated to try stopping smoking is also helpful: when health professionals raise the topic of smoking in future consultations, they can then tailor their messages to smokers' levels of motivation (see below).
Table 1.
Documentation of smoking in secondary care
| • Smoking status, number of cigarettes smoked, and motivation to stop should be ascertained at all visits |
| • Electronic and paper records should be adapted to facilitate and promote the recording of this information |
Figure 2.
Smokers' medical records should also be indexed so that they are readily identifiable and easy to retrieve. Without easy access to smokers' medical records, health professionals cannot effectively monitor their management of smoking. The simplest method for indexing smokers' medical records is to tag electronic records with one of the smoking status Read codes, but non-computerised general practices could use a simple card index. Monitoring longitudinal changes in patients' smoking behaviour and health professionals' delivery of cessation interventions is most appropriate in primary care because there is repeated contact between patients and primary healthcare teams. Health professionals can therefore treat smoking as a chronic disease, like asthma or diabetes.
Table 2.
The five “A”s for antismoking interventions in routine care
| • Ask about smoking at every opportunity |
| • Assess smokers' interest in stopping |
| • Advise against smoking |
| • Assist smokers to stop |
| • Arrange follow up |
The five “A”s approach
The five “A”s (ask, assess, advise, assist, arrange) summarise the role of health professionals in managing smoking. Health professionals are urged to ask all smokers about their smoking. Once smokers have been identified, it is important to assess their interest in stopping smoking with an open question such as “how do you feel about your smoking?” It is important to ask sensitively as some smokers feel defensive when doctors raise the issue, and this can make it difficult to ascertain patients' true views.
Managing smoking cessation needs to become a key part of routine practice for all clinicians. This article discusses strategies for incorporating effective antismoking interventions into routine clinical care
All smokers, irrespective of their motivation to stop, need to be advised against smoking in a clear, personalised, and non-judgmental way. When smokers are clearly interested in stopping, health professionals should assist them to do so. Specific action will depend on the individual's circumstances, but, where appropriate, smokers should be encouraged to set a date for stopping completely, to plan for likely problems, and to enlist the support of family and friends. Health professionals should discuss the use of nicotine replacement therapy or bupropion with heavier smokers and prescribe either treatment if this is appropriate (see earlier articles in this series).
Figure 3.
For smokers who want counselling and behavioural support, health professionals should also arrange for this to be provided, if possible from a specialist cessation service.
Implementing the approach
Success in integrating the five “A”s approach into routine clinical care will vary. In primary care, for example, patients visit doctors for a wide variety of reasons and general practitioners are, perhaps understandably, reluctant to raise the issue of smoking in all consultations..
Conversely, cardiologists and respiratory physicians will probably ask about smoking status in the vast majority of first consultations. Health professionals, therefore, should be encouraged to raise the issue of smoking with patients as often they believe is possible while recognising that discussing smoking is sometimes better left for subsequent consultations.
One way is to ensure that inquiring about smoking status and updating medical records is routine and systematic. If clinicians consider it inappropriate to raise the issue of smoking at all consultations, they should inquire and update records of smoking status at least annually. This gives clinicians the opportunity to select consultations in which to discuss smoking, taking into account patients' expectations of whether the issue should be tackled.
Table 3.
General practitioners' reasons for not giving smoking advice
| • Patients are often not motivated to stop |
| • Patients often don't listen to advice |
| • Stopping smoking is often not a priority for smokers |
| • Lack of time |
| • Unwanted advice can annoy patients |
| • Difficult to impress on patients the importance of not smoking |
| • Do not know how to deal with smokers who are not motivated to stop |
Health professionals often cite pressure of time, among other things, as a reason for not intervening against smoking more frequently. Smoking can be one of several important health issues that need tackling in a single, short consultation. The crucial difference between individual smokers is their motivation to stop. Smokers vary greatly in their motivation and, to make best use of limited time, health professionals should tailor their approach to the motivational level of the individual smoker (see the chapter on motivation earlier in this series). As only about a fifth of smokers who attend general practitioners intend to try to stop smoking, it makes no sense for general practitioners to give all smokers they meet detailed information about how to stop. Non-motivated smokers need to be encouraged to change their attitudes to smoking before being urged to take action to quit.
Tailoring advice to motivation
Health professionals in both primary and secondary care can be encouraged to advise and assist smokers in a manner appropriate to their motivation to stop.
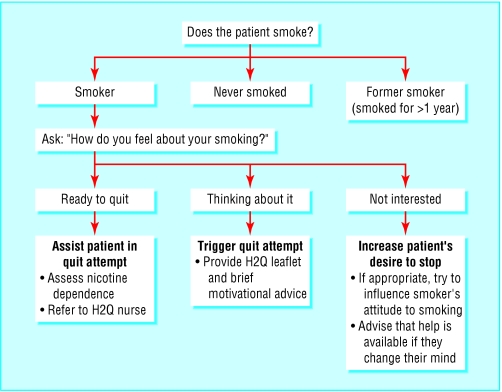
Figure 4.
Opportunistic assessment of smokers' motivation: Help 2 Quit approach. Adapted from the Help 2 Quit cessation service, Shropshire County Primary Care Trust
Primary care
“Help 2 Quit” (H2Q) is a smoking cessation service that encourages general practitioners to use their routine consultations opportunistically to intervene against smoking. They are encouraged to identify each smoker's level of motivation for trying to quit as soon as possible after raising the issue of smoking with them, and to use this as a base for subsequent discussions on smoking. The primary objective of this method is to offer support to those who are ready to quit and improve their chances of success. H2Q uses a simplified version of the “stages of change” (see earlier article) to tailor the intervention to the smoker. Although little empirical evidence exists to support the use of this approach, it fits well with clinical practice, including patients' expectations of how doctors should respond to their smoking.
Where counselling and behavioural support is not available, health professionals should consider providing follow up themselves or through another member of their team; this may be particularly convenient for smokers if pharmacotherapy for nicotine addiction is being prescribed and they cannot attend a specialist service
General practitioners tend to prefer to discuss smoking when patients present with smoking related problems, and they would generally avoid discussing smoking at all with some patients (for example, bereaved patients)
Secondary care
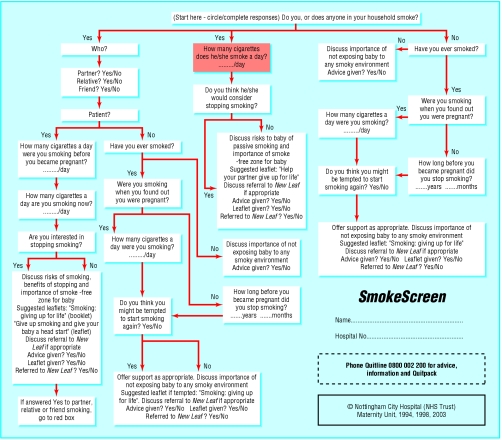
In the H2Q approach, general practitioners are urged to treat more motivated and less motivated smokers differently: motivated smokers are given specific advice about quitting that would be inappropriate for those not interested in stopping. In Nottingham, midwives have developed a mechanism for incorporating inquiry and intervention into their routine work. When pregnant women attend their booking appointment for antenatal care, midwives use an algorithm to ask a series of questions about smoking.
Figure 5.
Flow chart for midwives inquiring about smoking at booking. From Nottingham City Hospital NHS Trust (see bmj.com for larger version)
As 80% of pregnant women believe that stopping smoking is the most important lifestyle change they can make to improve their babies' health, inquiring about smoking at all booking appointments is unlikely to upset many pregnant women. Midwives ask the women about smoking status, whether they live with smokers (including partners), and finally whether they or other smokers they live with are interested in quitting.
All smoking related data from manual records are entered into an electronic database for monitoring purposes. Midwives then respond to women in an appropriate way for their motivation level, and those who are interested in receiving extra support in quitting are referred to the local cessation service for behavioural counselling.
Table 4.
Key points
| • Smoking cessation interventions are simple, cheap, and effective but are not yet widely part of routine care |
| • Clinicians must develop and use routine and systematic approaches to inquiring about and recording patients' smoking status |
| • Cessation interventions need to be adapted to smokers' levels of motivation |
| • Cessation interventions need to be audited and monitored |
Monitoring management of smoking
All medical care systems sometimes experience some inertia or resistance to change. The fact that effective smoking cessation interventions have not been adopted into routine care despite their availability for over 20 years shows that this is especially true in relation to smoking cessation.
It is therefore important to monitor and audit the implementation and delivery of these services. This can be relatively simple when information about smoking is recorded electronically. For example, most general practice computer systems in the United Kingdom use Read codes, which allow clinicians to record data on smoking status simply and accurately.
Recently, new Read codes describing the three categories of smokers' motivation (and used by H2Q) have been approved, and these can now be used by any general practice computer system to record individual smokers' motivation to quit in medical records. Use of these Read codes and information on patient management from medical records provides a means for monitoring how primary care health professionals respond to smokers with differing levels of motivation.
In the Help 2 Quit approach, general practitioners are urged to treat more motivated and less motivated smokers differently: motivated smokers are given specific advice about quitting that would be inappropriate for those not interested in stopping
The ABC of smoking cessation is edited by John Britton, professor of epidemiology at the University of Nottingham in the division of epidemiology and public health at City Hospital, Nottingham. The series will be published as a book in the late spring.
The adapted figure showing the “Help 2 Quit” approach is published with permission from K Lewis, and the flow chart for midwives with permission of Nottingham City Hospital (NHS Trust).
Competing interests: TC has been paid for speaking at a conference by GlaxoSmithKline, a drug company that manufactures treatments for nicotine addiction; he has also done consultancy work on one occasion for Pharmacia. See first article in this series (24 January 2004) for the series editor's competing interests.
Further reading and resources
- • Butler CC, Pill R, Stott NC. Qualitative study of patients' perceptions of doctors' advice to quit smoking: implications for opportunistic health promotion. BMJ 1998;316: 1878-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • Coleman T, Murphy E, Cheater FC. Factors influencing discussions about smoking between general practitioners and patients who smoke: a qualitative study. Br J Gen Pract 2000;50: 207-10. [PMC free article] [PubMed] [Google Scholar]
- • Rollnick SR, Mason P, Butler C. Health behaviour change: a guide for practitioners. London: Churchill Livingstone, 1999.
- • West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Thorax 2000;55: 987-99. [DOI] [PMC free article] [PubMed] [Google Scholar]