Abstract
Introduction:
Adolescents ranging in age from 11–15 (early‐mid adolescence) comprise the largest percentage of baseball and softball athletes in the United States. Shoulder and elbow injuries are commonly experienced by these athletes with baseball pitchers and softball position players most likely to be injured.
Common Injuries:
Physeal injury often termed “Little League” shoulder or elbow is common and should be differentiated from soft tissue injuries such as biceps, rotator cuff, or UCL injuries. Regardless of diagnosis, rehabilitation of these athletes’ shoulder and elbow injuries provide a unique challenge given their rapidly changing physical status.
Treatment:
Common impairments include alterations in shoulder range of motion, decreased muscle performance, and poor neuromuscular control of the scapula, core, and lower extremity. A criterion based, progressive rehabilitation program is presented. Discharge from formal rehabilitation should occur only when the athlete has demonstrated a resolution of symptoms, acceptable ROM, muscle performance, and neuromuscular control while progressing through a symptom free return to sport.
Prevention of Reinjury:
Reintegration into the desired level of sport participation should be guided by the sports medicine professional with a focus on long‐term durability in sport performance as well as injury prevention. A prevention program which includes parent, coach, and athlete education, regular screening to identify those athletes at the highest risk, and monitoring athletes for the development of risk factors or warning signs of injury over the course of participation is indicated.
Level of Evidence:
5
Keywords: Adolescent, throwing injuries, youth
INTRODUCTION
The majority of the 11.5 million athletes playing baseball in the United States compete at the high school and club level.1 High school participation in the throwing sports has increased over the past two decades. In 2013, softball and baseball ranked as the forth and third most popular high school sports for girls and boys, respectively.2 Participation in sports has been linked to many health benefits including improved cardiovascular, musculoskeletal, and psychosocial health but participation is also associated with a potential risk of injury.
Interscholastic injury rates are relatively low in softball and baseball when considering all position players over the course of a 12‐week season. Many adolescent athletes play multiple positions and participate on more than one team per year contributing to arm fatigue and the risk of overuse injuries.3,4 The shoulder has been reported as the joint most frequently injured followed by the elbow.5–7 The highest shoulder injury rates are found in baseball pitchers and softball position players.5 Baseball pitchers are also documented to suffer the most severe injuries requiring the greatest number of days lost from practice or competition.8–10
Adolescent athletes present a particular challenge when injured, as they are most often during or just after periods of rapid growth. Combined with the extreme stresses repetitive throwing motion imparts to immature bone and developing soft tissue these athletes present differently than our skeletally mature throwing athletes.11 The proposed stresses have been documented in magnitudes sufficient to change both soft tissue and bone and have been observed in athletes with arm pain and injury.5,12–15 The combination of repetitive throwing, weak physeal cartilage at growth centers, muscle tightness associated with rapid long bone growth, increased laxity of soft tissue structures, and decreased development of neuromuscular movement patterns may place the adolescent athlete at increased risk of upper extremity injury.15–19 These influences combined with established risk factors in all throwers may predispose the adolescent athlete to both common and unique injuries. Therefore, this clinical commentary will describe the risk factors and impairments associated with the most common adolescent baseball and softball upper extremity injuries and suggest treatment strategies to fully rehabilitate these athletes following injury. Secondarily, the clinical commentary will review the risk factors related to the development of adolescent throwing injuries to assist the clinician in developing prevention strategies and to assist in the accurate examination of these athletes.
Risk Factors for Overuse Upper Extremity Injuries
Overuse arm injuries are common in throwing athletes.20 There are numerous risk factors hypothesized to predispose throwers to arm injury and these factors can be classified as non‐modifiable or modifiable. Non‐modifiable risk factors include age, body mass index, height, coaching habits, and pitching performance satisfaction.10,21–23 Modifiable risk factors include pitching mechanics, frequency and volume as well as physical factors such as altered shoulder rotational ROM, decreased posterior shoulder flexibility, rotator cuff weakness and imbalance, and poor neuromuscular control of scapular, core, and lower extremity musculature.5,11,21,22,24–35 Modifiable factors are important, as these factors should be the emphasis of treatment and prevention programs.
Injuries to the Adolescent Throwing Shoulder
Pathologies commonly seen in the adult throwing shoulder include internal impingement, irritation of the undersurface of the rotator cuff, and Superior Labral Anterior‐Posterior (SLAP) lesions. These injuries, although possible, are less commonly seen in the younger adolescent athlete (13–15 year old). The incidence of rotator cuff pathology in individuals under 20 years of age is documented to be approximately 1%.36 The prevalence of SLAP tears was 18% in high school baseball players with the relative risk of developing a SLAP tear estimated at 1.4 times greater than for junior high school players (4.8% prevalence).23
Anterior/superior shoulder pain related to rotator cuff/biceps pathology, labral pathology and/or proximal humeral epiphyseal injury are more common complaints in the 13–16 year old throwing athletes. Proximal humeral epiphysiolysis occurred with similar frequency between all junior and high school baseball pitchers and position players.23 Windmill softball pitchers often present with anterior shoulder pain related to labral injury or biceps pathology.37,38
Impairments in Adolescent Athletes’ with Throwing Shoulder Injuries
Immature athletes presenting with shoulder pain often demonstrate similar problems. The athlete often complains of a gradual onset in glenohumeral pain while throwing.39 The athlete, parent, or coach note altered performance related to decreased velocity and accuracy during throwing.39 These athletes are challenging as they often have increased joint laxity combined with poor flexibility and a reduction in range of motion (ROM).40,41 The injured athlete also most often presents with pain on resisted external rotation, a reduction in rotator cuff strength/endurance, and poor scapular control.24,25,40,42
Other impairments appear more specific to exact pathology and can be helpful in the differential diagnosis, creation of an individual treatment plan, and prognosis for the athlete. Proximal humeral epiphysiolysis or “Little League shoulder” should be suspected in throwing athletes complaining of anterior/lateral shoulder pain with activity, within the ages of 11–15, and those athletes who are at their peak growth velocity. Athletes often present with a concomitant increase in volume or intensity of throwing. These athletes often complain of aching at the superolateral aspect of the shoulder and tenderness on palpation at the growth plate. Throwing athletes demonstrating vague anterior shoulder pain risk and the stated intrinsic and extrinsic factors present with a high pre test probability of Little Leagues shoulder. The clinical examination of these athletes not often definitive and diagnosis must be confirmed through imaging studies.
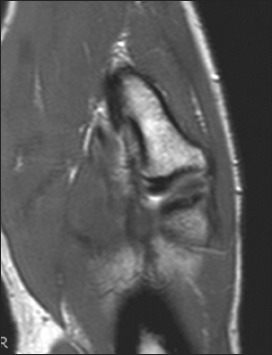
Radiographs demonstrate widening of the proximal humeral physis and changes in the appearance of the bone including sclerosis, fragmentation, and cystic changes.41 (Figure 1) Athlete’s presenting with deep shoulder pain on maximal cocking, intermittent popping or catching during rotational movements, loss of external rotation strength with accompanying atrophy in the infraspinous fossa should be suspected of possible SLAP pathology.43 Physical examination using a cluster of specific tests,44 a possible intra‐articular diagnostic injection,45 and an MRI might be used to confirm the diagnosis. Although beyond the scope of this paper to describe all labral specific special tests, a recent review examining the clinical utility of orthopedic tests documented the biceps load II had the highest levels of sensitivity and specificity for diagnosis of SLAP pathology.44 Other tests commonly used in isolation or combination to examine labral pathology in throwers includes the O’Brien’s sign, biceps load I, and the relocation test. These tests demonstrate equivocal utility based on review of the literature.44
Figure 1.

Widening of the proximal humeral physis and changes in the appearance of the bone including sclerosis, fragmentation, and cystic changes.
Injuries to the Adolescent Throwing Elbow
Repetitive throwing imparts a tensile stress and on the medial elbow and a compressive force at the lateral elbow.46 These forces are distributed among musculotendonous, capsuloligamentous, and bony structures. Twenty‐eight percent of all youth pitchers report a history of elbow pain.21 UCL reconstructions have doubled in high school baseball players10 but UCL injury is not the most frequent injury sustained by the youngest adolescent throwers. In the skeletally immature athlete the physis at the medial epicondyle is weaker than the UCL and other dynamic restraints of the elbow.46 The same forces creating the UCL pathology in older more physically mature athletes are hypothesized to be responsible for the development of medial elbow epicondylar pain reported in 11–15 year old throwers.47,48
“Little League Elbow” is a term used to encompass most of the medial elbow problems reported by youth/adolescent players.46 Medial epicondylear apophysitis is a common pathology related to repetitive valgus stress at the elbow.49 The incidence of medial epicondylar injury in early adolescence has been reported to be from 4 to 39%.47 The spectrum of pathology at the medial epicondyle can vary from irritation to the origin of the flexor pronator mass through fragmentation and avulsion of the medial epicondyle.
The athlete with apophysitis often presents with a gradual onset of discomfort during the throwing motion with aching following activity depending on the progression of the problem. Athletes often report a dramatic increase in volume or intensity of training preceding the increase in medial elbow discomfort. Complaint of decreased throwing velocity and problems with accuracy that may be related to loss of grip strength are not uncommon. The medial epicondyle is tender to palpation and may be enlarged. Patients with more involved pathology may present with acute motion loss and pain with extremes of elbow motion. Radiologic examination often demonstrates fragmentation at the condyle or avulsion near the apophysis (Figures 2A & B). The definitive diagnosis of medial epicondylear apophysitis can only be made with a combination of careful subjective and objective clinical examination and confirming radiologic studies.
Figure 2.

A. Fragmentation at the condyle or avulsion near the apophysis. B. After surgical repair.
Adolescent athletes may present with lateral elbow pain related to compression forces at the radiocapitellar joint. Panner’s disease and osteochondritis dissecans (OCD) are similar in symptom presentation including stiffness and pain at the lateral elbow.50The differentiation between Panners and OCD of the capitellum may be the age of presentation and the persistent mechanical symptoms associated with loose body presence seen with OCD.50 (Figure 3) Panners disease is commonly seen in younger athletes (<10 years old) without a history of trauma, and has a good prognosis with expected full recovery of function. Osteochondritis dissecans of the capitellum often presents with more severe pain and limitations.51 The pathology is theorized as related to a disruption in subchondral blood flow to the capitellum.51 The radial head is secondarily involved as the pathology advances in the throwing adolescent. Loose bodies from the injured capitellum and radial head have been reported, and are the cause of the mechanical symptoms typical with this pathology. This condition often presents itself in athletes 13 years of age or older. The athlete often complains of pain at late cocking through acceleration when compressive forces at the elbow are greatest.51 Tenderness and pain at the lateral elbow especially during extremes of elbow motion are consistently found in these throwers.51 A loss of elbow extension of up to 30 degrees is not uncommon.51
Figure 3.
Osteochondritis dissecans of the capitellum.
Impairments in Throwing Athletes presenting with Elbow Injuries
The precipitating factors for the development of elbow pain in youth athletes appear to be multifactorial. Modifiable physical factors hypothesized in the development of elbow injuries include rapid growth velocity,4 asymmetrical loss of internal rotation,5 scapular dyskinesis,52 decreased kinetic chain activation/control,52 and decreased coordination and neuromuscular control.53 Competition factors including catching, pitching, or playing both catcher and pitcher,54 playing on multiple teams and leagues, aggregate pitch count over 80 pitches per game or participation during 8 months per year,22 performance of the slider pitch type,21 pitching with arm fatigue,22 and pitching with improper mechanics. Each of these factors alone or in combination increase a players risk for serious elbow injuries.55,56
Non‐Operative Treatment of Upper Extremity Injuries to Adolescent Athletes
A detailed examination of the injured athlete includes a complete history (including self report scores such as Quick Disabilities of the Arm, Shoulder and Hand Score (DASH) and SPORT Module, Kerlin‐Jobe Orthopaedic Clinic (KJOC) or Functional Arm Scale for Throwers (FAST), physical examination (including baseline Beighton scores, humeral torsion, and shoulder ROM) and specific review of practice and competition habits in order to isolate precipitating factors and current impairments upon which to focus treatment. The adolescent athlete is monitored for changes in height, weight, BMI and changes in flexibility throughout the rehabilitation process. Impairments should be then prioritized based on context of the diagnosis, magnitude, and likely causative association with the involved tissues. Table 1 summarizes the common impairments, athlete presentation, treatment focus and goals during the phased rehabilitation continuum.
Table 1.
Phases and Progression of Rehabilitation
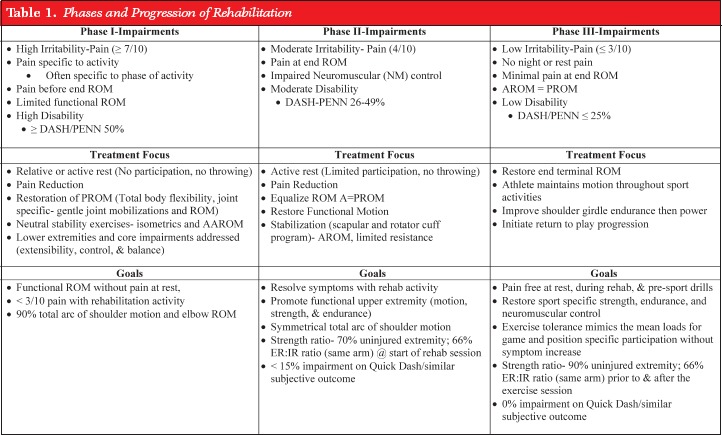 |
The basis for initial phase of treatment in the adolescent athlete with an overuse arm begins with relative or active rest. The stress of throwing is removed from the irritated tissue and treatments are implemented that are designed to decrease inflammation, gently increase ROM and flexibility, and support tissue healing.57 The sports medicine professional monitors the athlete’s response to the initial treatment and designs a program to restore necessary flexibility including joint mobilizations and gentle ROM.57 The lower extremities and core are incorporated into the rehabilitation program in order to enhance sport specific neuromuscular control and flexibility. Specific treatments are designed to address athlete specific impairments. For example, the athlete presenting with poor lower extremity flexibility will focus on enhanced dynamic stretching and functional movement patterns. (Figure 4). Once the athlete has full ROM without pain at rest, <3/10 pain with rehabilitation activity and 90% total arc of shoulder motion and elbow ROM the athlete can progress to the second phase of the rehabilitation program.
Figure 4.
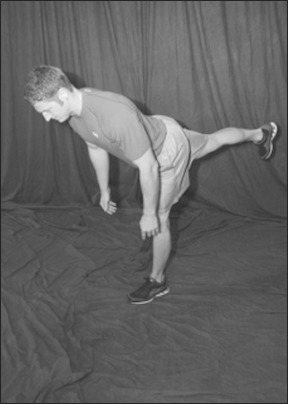
Dynamic lower extremity stretch, as an example.
The second phase of the rehabilitation program is designed to resolve all symptoms while promoting functional upper extremity motion, strength, and endurance and to advance stability and control of the scapula, core and lower extremities. Specific sleeper (Figure 5) and cross body stretches (Figure 6) to enhance posterior shoulder flexibility are implemented. A total arm care strength and endurance program with techniques including hold relax, contract relax, and rhythmic stabilization are initiated to ensure good neuromuscular recruitment and control are initiated.57 The authors criteria for advancement to phase III of the rehabilitation program include pain free performance of all rehabilitation activities, demonstration of symmetrical total arc of shoulder motion,26,57 improving strength as measured by hand held dynamometer (HHD) to 70% of the uninjured extremity,57 and functional scores that indicate less than 15% impairment on the Quick Dash or similar subjective outcome score. Additionally, the ratio of external rotation (ER): internal rotation (IR) shoulder strength within the same extremity should begin to approach the normative ratio of 66% as measured by HHD or isokinetically based on clinical availability.58,59
Figure 5.
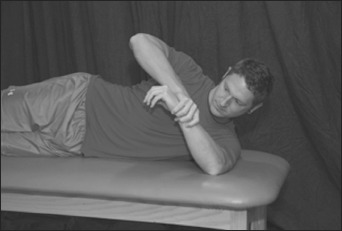
The sleeper stretch, traditionally performed at 90 degrees.
Figure 6.
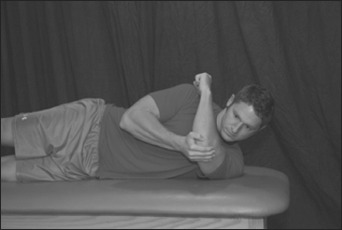
The sidelying crossbody stretch.
This phase of rehabilitation emphasizes the restoration of sport specific strength, endurance, and neuromuscular control at the expected level of demand and participation. The athlete must remain pain free and continue to maintain symmetrical motion with the increased workload. Addition of activities requiring the athlete to perform sport specific motions while transitioning from concentric to eccentric loads is critical to prepare the athlete to return to activity. The activity focus during this phase is on plyometric drills, advanced core control, and lower extremity balance activities. The goals for the athletes exercise tolerance and requirements are set to mimic the mean loads required for game and position specific participation.60,61 Measures of shoulder strength (90% uninjured arm) and ER:IR strength ratios (66%)59 are documented prior to and after performance of the exercise session. The athlete progresses to the return to sport phase of the rehabilitation program after attainment of exercise goals while maintaining 90% of pre workout strength. Additional requirements include maintenance of pain free symmetrical ROM, 0% disability on basic Quick Dash outcome score, and good compliance and knowledge of the home exercise program.
Phase IV of the rehabilitation program focuses on sport specific drills and reintegration into sport activities. The specific interval throwing program (ITP) is designed to be sport and position specific based on the available literature.60–65 A focused warm up program that will be reproduced as the athlete returns to full participation is used prior to each interval throwing session. The throwing distance begins at 45 feet and the athlete’s strength and flexibility are measured (HHD/ isokinetic device and goniometer/ inclinometer are used to quantify clinical impairments based on clinic availability) prior to and after the first throwing session at the new distance as they progress through the program. The athlete should maintain 90% of their pre session strength and flexibility after execution of the ITP. The athlete progresses through the stages of the ITP as suggested unless they experience pain with or after throwing, a reduction in strength or ROM, or if they have arm soreness lasting 24 hours. The athlete remains at the current stage until soreness and pain resolve with performance and strength/ ROM stabilize with throwing. Successful return to sport includes ensuring the athlete is progressing toward previous performance level, demonstrates durability and reproducibility of proper mechanics, utilizes appropriate rest, and is competent in an appropriate in season program. Athletes should be monitored throughout the process and the authors recommend frequent communication between the athlete, parents, coaches, and rehabilitation professionals to offer support during return to full competition and reduce the risk of reinjury. Prior to discharge, the athlete’s throwing mechanics should be evaluated using video analysis to educate athletes and coaches and assist the athlete to correct errors and provide the basis for a safe return to sport.
Prevention of Throwing Injuries in the Adolescent Athlete
The goal of community screening is to prevent initial and subsequent arm injuries in adolescent throwing athletes. The most important tenants of the prevention program are: education, identification of those athletes at the highest risk, full rehabilitation of current and past injuries, and monitoring athletes for the development of risk factors or warning signs of injury.66
The focus of education is the dissemination of current recommendations and information to coaches, athletes, and parents. USA baseball guidelines for game pitch count and rest days should be the basis for advice for adolescent baseball participation.67 Pitch counts guidelines for windmill softball players has been recommended38, however to the authors’ knowledge, actual pitch count limits for softball have not been established and high school softball rules do not address game or seasonal pitch counts.3 For both softball and baseball athletes, recommendations include avoiding continued participation during episodes of pain or fatigue.22 Advising athletes to avoid year round participation and recommending several periods of rest throughout the year to ensure safe participation are recommended.4,22
Preseason screening is key to identify athletes at risk including a review of patient history, current symptoms, self reported outcome and monitoring of physical factors including height, weight, passive ROM (shoulder internal rotation, shoulder external rotation, shoulder horizontal adduction and elbow extension ROM), shoulder strength, Beighton score, lower extremity and core control during single and double leg function. Athletes with a Beighton score of greater than 268 are monitored closely by the schools athletic trainer and are advised to perform a rotator cuff endurance program 2–3 times per week. Athletes deemed at risk based on their ROM, strength, lower extremity or core performance are instructed in a specific exercise program to address their impairments and they are monitored closely by their physical therapist or athletic trainer for the performance of the exercise program and the development of pain or changes in performance.
Athletes sustaining an injury are evaluated and rehabilitated thoroughly following a criterion‐based program detailed earlier. The athlete should be screened for height, weight, ROM, humeral torsion, arm strength/ endurance, scapular dyskinesis, and lower extremity and core performance to determine priority impairments for treatment. Upon discharge, the athlete should be contacted on a monthly basis to track exposure, performance, and the development of pain or injury for a minimum of 1 year. Athletes also are incorporated into the regular screening program.
CONCLUSION
Injuries in the adolescent thrower have become a significant health concern with reports of increased frequency of need for surgery and significant time loss. Athletes sustaining these injuries are at risk for future injury and cessation of participation. Knowledge of common risk factors, impairments, and effective interventions in these athletes may prevent or minimize the impact of these injuries.
REFERENCES
- 1. Lawson BR, Comstock RD, Smith GA. Baseball‐related injuries to children treated in hospital emergency departments in the United States, 1994–2006. Pediatrics. 2009;123(6):e1028–34 [DOI] [PubMed] [Google Scholar]
- 2. Associations NFoSHS 2012–2013 High school athletics participation survey. National Federation of State High School Associations; 2013 [Google Scholar]
- 3. Associations NFoSHS 2010–2011 High school athletics participation survey. National Federation of State High School Associations; 2011 [Google Scholar]
- 4. Valovich McLeod TC, Decoster LC, Loud KJ, Micheli LJ, Parker JT, Sandrey MA, et al. National Athletic Trainers’ Association Position Statement: Prevention of Pediatric Overuse Injuries. J Ath Training. 2011;46(2):206–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. The American journal of sports medicine. 2011;39(9):1997–2006 [DOI] [PubMed] [Google Scholar]
- 6. Collins CL, Comstock RD. Epidemiological features of high school baseball injuries in the United States, 2005–2007. Pediatrics. 2008;121(6):1181–7 [DOI] [PubMed] [Google Scholar]
- 7. American Academy of Pediatrics: Committee on Sports Medicine and Fitness Risk of Injury From Baseball and Softball in Children. Pediatrics. 2001;107(4):782–4 [DOI] [PubMed] [Google Scholar]
- 8. Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005–2007. Am J Sports Med. 2009;37(9):1798–805 [DOI] [PubMed] [Google Scholar]
- 9. Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder Injuries in US High School Baseball and Softball Athletes, 2005–2008. Pediatrics. 2010;125:497–501 [DOI] [PubMed] [Google Scholar]
- 10. Petty DH, Andrews JR, Fleisig GS, Cain L. Ulnar Collateral Ligament Reconstruction in High School Baseball Players. Am J Sports Med. 2004;32(5):1158–64 [DOI] [PubMed] [Google Scholar]
- 11. Werner SL, Gill TJ, Murray TA, Cook TD, Hawkins RJ. Relationships between Throwing Mechanics and Shoulder Distraction in Professional Baseball Pitchers. Am J Sports Med. 2001;29(3):354–8 [DOI] [PubMed] [Google Scholar]
- 12. Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. The American journal of sports medicine. 2005;33(11):1716–22 [DOI] [PubMed] [Google Scholar]
- 13. Shanley E, Noonan TJ, Hawkins RJ, Schlegel TF, Thigpen CA. The influence humeral torsion on shoulder range of motion and GIRD in youth, adolescent, and professional pitchers. Journal of Orthopaedic and Sports Physcial Therapy. 2012;47(1). [Google Scholar]
- 14. Sweitzer BA, Thigpen CA, Shanley E, Stranges G, Wienke JR, Storey T, et al. A comparison of glenoid morphology and glenohumeral range of motion between professional baseball pitchers with and without a history of SLAP repair. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28(9):1206–13 [DOI] [PubMed] [Google Scholar]
- 15. Carson WG Jr., Gasser SI. Little Leaguer’s shoulder. A report of 23 cases. The American journal of sports medicine. 1998;26(4):575–80 [DOI] [PubMed] [Google Scholar]
- 16. Myer GD, Faigenbaum AD, Ford KR, Best TM, Bergeron MF, Hewett TE. When to initiate integrative neuromuscular training to reduce sports‐related injuries and enhance health in youth? Current sports medicine reports. 2011;10(3):155–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walton J, Paxinos A, Tzannes A, Callanan M, Hayes K, Murrell GA. The unstable shoulder in the adolescent athlete. The American journal of sports medicine. 2002;30(5):758–67 [DOI] [PubMed] [Google Scholar]
- 18. Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33(11):1716–22 [DOI] [PubMed] [Google Scholar]
- 19. Caine D, Maffulli N, Caine C. Epidemiology of injury in child and adolescent sports: injury rates, risk factors, and prevention. Clinics in sports medicine. 2008;27(1):19–50, vii [DOI] [PubMed] [Google Scholar]
- 20. May MM, Bishop JY. Shoulder injuries in young athletes. Pediatric radiology. 2013;43 Suppl 1:S135–40 [DOI] [PubMed] [Google Scholar]
- 21. Lyman S, Fleisig GS, Andrews JR, Oskinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463–8 [DOI] [PubMed] [Google Scholar]
- 22. Olsen II SJ, Fleisig GS, Dun S, Loftice J, JR A. Risk Factors for Shoulder and Elbow Injuries in Adolescent Baseball Pitchers. Am J Sports Med. 2006;34(6):905–12 [DOI] [PubMed] [Google Scholar]
- 23. Han KJ, Kim YK, Lim SK, Park JY, Oh KS. The effect of physical characteristics and field position on the shoulder and elbow injuries of 490 baseball players: confirmation of diagnosis by magnetic resonance imaging. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2009;19(4):271–6 [DOI] [PubMed] [Google Scholar]
- 24. Byram IR, Bushnell BD, Dugger K, Charron K, Harrell FE, Jr., Noonan TJ. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. The American journal of sports medicine. 2010;38(7):1375–82 [DOI] [PubMed] [Google Scholar]
- 25. Hurd WJ, Kaplan KM, ElAttrache NS, Jobe FW, Morrey BF, Kaufman KR. A profile of glenohumeral internal and external rotation motion in the uninjured high school baseball pitcher, part II: strength. Journal of athletic training. 2011;46(3):289–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wilk KE, Meister K, Andrews JR. Current Concepts in the Rehabilitation of the Overhead Throwing Athlete. Am J Sports Med. 2002;30(1):136–51 [DOI] [PubMed] [Google Scholar]
- 27. Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38(1):21–6 [DOI] [PubMed] [Google Scholar]
- 28. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–20 [DOI] [PubMed] [Google Scholar]
- 29. Burkhart SS, Morgan CD, Kibler WB. The Disabled Throwing Shoulder: Spectrum of Pathology Part III: The SICK Scapula, Scapular Dyskinesis, the Kinetic Chain, and Rehabilitation. Arthroscopy. 2003;19(6):641–61 [DOI] [PubMed] [Google Scholar]
- 30. Hurd WJ, Kaplan KM, Eiattrache NS, Jobe FW, Morrey BF, Kaufman KR. A profile of glenohumeral internal and external rotation motion in the uninjured high school baseball pitcher, part I: motion. Journal of athletic training. 2011;46(3):282–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lyman S, Fleisig GS, Waterbor JW, Funkhouser EM, Pulley L, Andrews JR, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–10 [DOI] [PubMed] [Google Scholar]
- 32. Reinold MM, Wilk KE, Macrina LC, Sheheane C, Dun S, Fleisig GS, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36(3):523–7 [DOI] [PubMed] [Google Scholar]
- 33. Tyler TF, Nicholas SJ, Lee SJ, Mullaney M, McHugh MP. Correction of posterior shoulder tightness is associated with symptom resolution in patients with internal impingement. Am J Sports Med. 2010;38(1):114–9 [DOI] [PubMed] [Google Scholar]
- 34. Urbin MA, Fleisig GS, Abebe A, Andrews JR. Associations between timing in the baseball pitch and shoulder kinetics, elbow kinetics, and ball speed. The American journal of sports medicine. 2013;41(2):336–42 [DOI] [PubMed] [Google Scholar]
- 35. Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD, 2nd, Harker P, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39(2):329–35 [DOI] [PubMed] [Google Scholar]
- 36. Itoi E, Tabata S. Rotator cuff tears in the adolescent. Orthopedics. 1993;16(1):78–81 [DOI] [PubMed] [Google Scholar]
- 37. Rojas IL, Provencher MT, Bhatia S, Foucher KC, Bach BR, Jr., Romeo AA, et al. Biceps activity during windmill softball pitching: injury implications and comparison with overhand throwing. The American journal of sports medicine. 2009;37(3):558–65 [DOI] [PubMed] [Google Scholar]
- 38. Barrentine SW, Fleisig GS, Whiteside JA, Escamilla RF, Andrews JA. Biomechanics of Windmill Softball Pitching with Implications About Injury Mechanics at the Shoulder and Elbow. J Orthop Sports Phys Ther. 1998;28:405–14 [DOI] [PubMed] [Google Scholar]
- 39. Zaremski JL, Krabak BJ. Shoulder injuries in the skeletally immature baseball pitcher and recommendations for the prevention of injury. PM & R : the journal of injury, function, and rehabilitation. 2012;4(7):509–16 [DOI] [PubMed] [Google Scholar]
- 40. Reinold MM, Gill TJ. Current Concepts in the Evaluation and Treatment of the Shoulder in Overhead Throwing Athletes, Part 1: physical characteristics and clinical examination. Sports Health; 2010;2(1):39–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mariscalco MW, Saluan P. Upper extremity injuries in the adolescent athlete. Sports medicine and arthroscopy review. 2011;19(1):17–26 [DOI] [PubMed] [Google Scholar]
- 42. Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, Nicholas SJ. Muscle Strength and Range of Motion in Adolescent Pitchers With Throwing‐Related Pain: Implications for Injury Prevention. Am J Sports Med. 2008;36(11):2173–8 [DOI] [PubMed] [Google Scholar]
- 43. Abrams JS, Bradley JP, Angelo RL, Burks R. Arthroscopic management of shoulder instabilities: anterior, posterior, and multidirectional. Instructional course lectures. 2010;59:141–55 [PubMed] [Google Scholar]
- 44. Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta‐analysis of individual tests. British journal of sports medicine. 2012;46(14):964–78 [DOI] [PubMed] [Google Scholar]
- 45. Tobola A, Cook C, Cassas KJ, Hawkins RJ, Wienke JR, Tolan S, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons …’ [<etal/>.]. 2011;20(7):1147–54 [DOI] [PubMed] [Google Scholar]
- 46. Frush TJ, Lindenfeld TN. Peri‐epiphyseal and Overuse Injuries in Adolescent Athletes. Sports health. 2009;1(3):201–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cain EL Jr., Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. The American journal of sports medicine. 2003;31(4):621–35 [DOI] [PubMed] [Google Scholar]
- 48. Lawrence JT, Patel NM, Macknin J, Flynn JM, Cameron D, Wolfgruber HC, et al. Return to Competitive Sports After Medial Epicondyle Fractures in Adolescent Athletes: Results of Operative and Nonoperative Treatment. The American journal of sports medicine. 2013 [DOI] [PubMed] [Google Scholar]
- 49. Gugenheim JJ Jr., Stanley RF, Woods GW, Tullos HS. Little League survey: the Houston study. The American journal of sports medicine. 1976;4(5):189–200 [DOI] [PubMed] [Google Scholar]
- 50. Kobayashi K, Burton KJ, Rodner C, Smith B, Caputo AE. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. The Journal of the American Academy of Orthopaedic Surgeons. 2004;12(4):246–54 [DOI] [PubMed] [Google Scholar]
- 51. Baker CL 3rd, Romeo AA, Baker CL, Jr. Osteochondritis dissecans of the capitellum. The American journal of sports medicine. 2010;38(9):1917–28 [DOI] [PubMed] [Google Scholar]
- 52. Sciascia A, Kibler WB. The Pediatric Overhead Athlete: What is the Real Problem? Clin in Sports Med; 2006;16:471–7 [DOI] [PubMed] [Google Scholar]
- 53. Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports health. 2012;4(5):419–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. The American journal of sports medicine. 2004;32(1):79–84 [DOI] [PubMed] [Google Scholar]
- 55. Davis JT, Limpisvasti O, Fluhme D, Mohr KJ, Yocum LA, Elattrache NS, et al. The effect of pitching biomechanics on the upper extremity in youth and adolescent baseball pitchers. Am J Sports Med. 2009;37(8):1484–91 [DOI] [PubMed] [Google Scholar]
- 56. Fortenbaugh D, Fleisig GS, Andrews JR. Baseball pitching biomechanics in relation to injury risk and performance. Sports health. 2009;1(4):314–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Rehabilitation of the Overhead Athlete’s Elbow. Sports health. 2012;4(5):404–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ivey FM Jr., Calhoun JH, Rusche K, Bierschenk J. Isokinetic testing of shoulder strength: normal values. Archives of physical medicine and rehabilitation. 1985;66(6):384–6 [PubMed] [Google Scholar]
- 59. Ellenbecker TS, Davies GJ. The application of isokinetics in testing and rehabilitation of the shoulder complex. Journal of athletic training. 2000;35(3):338–50 [PMC free article] [PubMed] [Google Scholar]
- 60. Axe MJ, Snyder‐Mackler L, Konin JG, Strube MJ. Development of a distance‐based interval throwing program for Little League‐aged athletes. Am J Sports Med. 1996;24(5):594–602 [DOI] [PubMed] [Google Scholar]
- 61. Axe MJ, Windley TC, Snyder‐Mackler L. Data‐Based Interval Throwing Programs for Collegiate Softball Players. J Ath Train. 2002;37(2):194–203 [PMC free article] [PubMed] [Google Scholar]
- 62. Love S, Aytar A, Bush H, Uhl TL. Descriptive analysis of pitch volume in southeastern conference baseball pitchers. North American journal of sports physical therapy : NAJSPT; 2010;5(4):194–200 [PMC free article] [PubMed] [Google Scholar]
- 63. Hill JL, Humphries B, Weidner T, Newton RU. Female collegiate windmill pitchers: influences to injury incidence. Journal of strength and conditioning research / National Strength & Conditioning Association. 2004;18(3):426–31 [DOI] [PubMed] [Google Scholar]
- 64. Shanley E, Michener LA, Ellenbecker TS, Rauh MJ. Shoulder range of motion, pitch count, and injuries among interscholastic female softball pitchers: a descriptive study. International journal of sports physical therapy. 2012;7(5):548–57 [PMC free article] [PubMed] [Google Scholar]
- 65. Reinold MM, Wilk KE, Reed J, Crenshaw K, Andrews JR. Interval sport programs: guidelines for baseball, tennis, and golf. The Journal of orthopaedic and sports physical therapy. 2002;32(6):293–8 [DOI] [PubMed] [Google Scholar]
- 66. Shanley E, Michener LA, Ellenbecker TS, Rauh MJ. Incidence of Shoulder and Elbow Injuries in High School Softball and Baseball Players. Journal Athletic Training. 2011;45(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Official Site of USA Baseball: This is USA Baseball. 2003
- 68. Cameron KL, Duffey ML, DeBerardino TM, Stoneman PD, Jones CJ, Owens BD. Association of generalized joint hypermobility with a history of glenohumeral joint instability. Journal of athletic training. 2010;45(3):253–8 [DOI] [PMC free article] [PubMed] [Google Scholar]


