Abstract
Background:
Hip range of motion is an important component in assessing clinical orthopedic conditions of the hip, low back and lower extremities. However it remains unclear as to what constitutes the best tool for clinical measurement. The purpose of this study was to investigate the concurrent validity of passive range of motion (ROM) measurements of hip extension and hip internal and external rotation using a digital inclinometer and goniometer.
Design:
Criterion Standard
Setting:
Clinical research laboratory
Participants:
30 healthy subjects without pain, radicular symptoms or history of surgery in the low back or hip regions.
Main Outcome Measures:
Passive hip range of motion for extension, hip internal rotation and hip external rotation. A digital inclinometer and universal goniometer were utilized as the tools for comparisons between measurements.
Results:
There was a statistically significant difference (p < 0.05) between the goniometer and digital inclinometer in measured hip ROM except for measurements of right hip external rotation (p > 0.05). The mean difference between the goniometer and digital inclinometer in left hip extension, internal rotation and external rotation were 3.5°, 4.5° and 5.0° respectively. The mean difference between the two devices in right hip extension, internal rotation and external rotation were 2.8°, 4.2° and 2.6° respectively. On average, the difference between the goniometer and digital inclinometer in extension was 3.2°, internal rotation was 4.5° and external rotation was 3.8°. The digital inclinometer had greater measurement during EXT and ER. Furthermore, there was no statistically significant difference (p > 0.05) in hip ROM between the left and right side for either goniometric or digital inclinometer measurements.
Conclusions:
This results of this study indicate that a significant difference exists between the two devices in all measurements with exception of right hip extension. The differences were noted to be between 3–5 degrees for all planes measured. These findings suggest that caution should be used if these two devices are to be used interchangeably to quantify passive hip range of motion in either clinical practice or when comparing studies that utilize different instruments.
Level of Evidence:
2b
Keywords: Goniometry, hip; lumbar, passive range of motion; validity
INTRODUCTION
Hip range of range of motion is a commonly measured clinical variable utilized to quantitatively assess hip mobility. Hip range of motion is often assessed in conditions such as arthritis of the hip, femoral‐acetabular impingement, low back pain and overuse running injuries.1–4 Prior investigation examining the foot have provided evidence that static measures such as arch height can be predictive of dynamic foot posture during activities such as walking and jogging.5 In spite of the fact that many technological advances have been made in quantifying biomechanical variables in research, these advances have not been carried into the clinical realm with any regularity. An example would be in the measurement of range of motion where a common and valid tool utilized by clinicians remains the standard universal goniometer.6,7 This is likely a result of its relative ease of use, low cost and portability. A limitation with the goniometer is that the inter‐tester reliability of measurements are generally poor with Intraclass Correlation Coefficients (ICC) <0.50, however the intra‐tester reliability is good (ICC > 0.80).7–10
In addition to the goniometer, another device being used by some clinicians to measure range of motion is the digital inclinometer. The inclinometer is similar to the goniometer in that both are lightweight and portable. However, the inclinometer has significantly more associated cost. The inclinometer has been demonstrated to possess good to excellent reliability (ICC > .088) and concurrent validity with the universal goniometer (ICC > 0.85) in studies examining both the hip and shoulder.9,11 The use of the digital inclinometer for measurements of the hips has been noted to demonstrate good reliability in both healthy subjects and those with cerebral palsy.8,12
There are a few considerations that need to be addressed with regard to measuring hip range of motion in the clinic. One limitation of the universal goniometer is that it requires the use of two hands which makes stabilization of other body segments difficult, especially when only one practitioner is available.13 This is particularly an issue in measuring isolated hip and knee range of motion as it has been noted that soft tissue constraints and contributions of the lumbopelvic region may limit accurate values.2,14 A positive factor in utilizing the goniometer with hip measurement is that it demonstrates concurrent validity when compared to 2D video motion capture system.15 Two distinct advantages exist for the use of the inclinometer for range of motion measurements of the hip: 1) The use of the inclinometer only requires the use of one hand thus freeing the additional hand for stabilizing the trunk as needed, and 2) the inclinometer has been demonstrated to possess good inter‐rater reliability (ICC > 0.80).16
Currently, few studies exist that compare the inclinometer and the goniometer with regard to measuring hip range of motion. Of the two studies that specifically looked at the hip, disagreement was found in terms of interchangeability of the devices. Clapis et al found good interchangeability, but only measured hip extension, using the modified Thomas test.17 Bierma‐Zeinstra et al found the instruments to not be interchangeable and included hip rotation measures.18 Secondary to this lack of agreement and lack of specific literature regarding hip ROM measurements, it is important to add to the body of knowledge as to whether the two devices are similar for use in both clinical practice and for comparing values obtained for hip ROM between studies that used only one two devices being examined.
The purpose of this study was to compare the concurrent validity of the universal goniometer and digital inclinometer in measuring passive range of motion (ROM) of hip extension and hip internal and external rotation in healthy subjects. The authors hypothesized that there would be no differences in measurements of passive hip range of motion obtained using the two devices.
METHODS
A convenience sample of 30 volunteer subjects (13 males and 17 females; mean age 34.0+/‐ 13.1 years, mean height, 171.5 +/‐ 11.9 cm, and mean body mass, 72.0 +/‐ 13.9 kg) was utilized. All subjects were included if they reported no history of surgery of spine, hips, knees, or history of neurological insult to the musculoskeletal system and had no current acute pain of the hips, low back, or knees. All subjects were informed of the purpose of the study and signed an informed consent document prior to data collection. The human subject’s review board at Western Washington University approved the protocol for the study.
STUDY DESIGN
All data collection took place in a research institution. All testing was completed in a single session by the primary investigator. The investigator is a licensed physical therapist with 20 years of experience in the musculoskeletal practice environment. During evaluation, the investigator measured EXT, IR and ER of both left and right hip. A universal goniometer, followed by a digital inclinometer, was used to measure hip ROM in this order with all subjects. No practice or warm up was performed prior to measurements. The goniometer was a standard 31.75 cm by 4.445 cm clear plastic device with 1° increments and 360° scale with a bubble level at the end to ensure both vertical and horizontal alignment (Figure 1A). The digital inclinometer was a Digital Protractor Pro 3600 (Mitotoyo America, Aurora, IL, USA), that provide measurements to 0.01° (Figure 1B).
Figure 1.
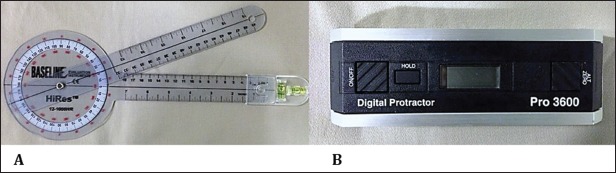
A) Goniometer with bubble level B) Digital Inclinometer (Digital Protractor Pro 3600, Mitotoyo America, Aurora, IL, USA).
During the EXT measurement, the subjects were positioned on their back and a Modified Thomas test was utilized.19 The hip being measured was positioned at the end of the treatment table and the tested leg was then cantilevered over the edge of table. The opposite leg was held passively by the subjects with the hip and knee in a flexed position against the chest. Instructions were provided for subjects to pull their knee straight toward their head in order to avoid any abduction at the hip. In addition, subjects were provided feedback, both verbal and tactile to maintain their low back flat against table to avoid lumbar extension and pelvic tilting throughout the evaluation. Each subject had a circular sticker placed over the lateral femoral condyle to assist with proper visual alignment and legs were measured alternately. The axis of rotation of the goniometer was positioned over the greater trochanter. The distal arm was aligned with the shaft of the femur while the proximal arm was aligned with the trunk (horizontal plane). The bubble level was used to determine that the proximal arm was parallel with the ground. The inclinometer measurement was taken from the anterior mid femur position with midpoint between the greater trochanter and lateral femoral condyle. Measurements were noted as negative if they were above the horizon (more flexed than neutral position) and positive if they fell below the horizontal position (more extended than neutral position).
During IR and ER measurements, the subjects were positioned prone on the treatment table. The investigator passively flexed both knees to 90 degrees while both hips were positioned in neutral abduction for measuring IR. Next, the investigator passively moved the shank of both legs out for hip IR until reaching passive end feel of joint region. For ER, the investigator passively flexed one knee to 90 degrees and then moved the shank towards the midline and crossed leg over midline until reaching passive end feel. The non‐measured leg was positioned in extension on the table. The subject’s pelvis was stabilized by the assistant to the investigator during hip ER measures in order to prevent pelvic rotation. Additionally, the subjects that displayed greater ER (motion blocked by presence of opposite leg) had their non‐tested leg abducted slightly to allow for full measurement. The axis of rotation of the universal goniometer was placed at the tibial tuberosity. The mobile arm of the goniometer was aligned with the shaft of the tibia, and rotation was measured relative to the vertical axis, which was the stationary arm. The bubble was used to ensure that the stationary arm remained perpendicular to the ground when the measurement was taken. Measurements with the inclinometer were taken with the device placed at the midline of medial shaft of tibia between the medial malleolus and medial tibial condyle.
Each measurement was performed three times and the average of the three measurements was calculated and recorded.10,20 The order of the hip ROM measurements was randomized for each subject. In addition, the goniometer and inclinometer measurements were verbally given by the investigator and recorded by an assistant.
STATISTICAL ANALYSIS
All statistical analysis was performed using SPSS 20.0. A two‐way repeated measures analysis of variance (ANOVA) was conducted to determine whether differences in hip range of motion measurements existed between devices and direction (i.e. EXT, IR, ER). A paired t‐test was utilized to test significant differences between sides in each measurement device. Greenhouse‐Geisser correction was implemented if Mauchly’s test revealed that the data violated the assumption of sphericity. Simple effects analysis used paired t‐tests between goniometer and inclinometer at each level of EXT, IR, ER. Tukey post‐hoc procedures were conducted in the case of significant main effects. Alpha level was set to 0.05. In addition, prior to data collection during a pilot test session, the ICC was calculated using a two‐way mixed effects model in order to test the intra‐rater reliability between both the goniometer and inclinometer.
RESULTS
The average measure ICC value for the three tested motions obtained using the goniometer was 0.8 and the digital inclinometer was 0.9. Mauchly’s test revealed that sphericity was violated (p = .005). There was a significant device by direction interaction (F[1.67, 48.52] = 30.18, p < .001). Simple effects revealed significant differences between goniometer and inclinometer measurements of extension (t(29) = 5.06, p < .001), internal rotation (t(29) = –6.18, p < .001), and external rotation (t(29) = 4.60, p < .001). The mean difference between the goniometer and digital inclinometer in left hip extension, internal rotation and external rotation were 3.4°, 4.4° and 5.0° respectively (Table 1). The inclinometer exhibited greater angle measurement during EXT and ER. The average difference between the goniometer and digital inclinometer in extension was 3.2°, internal rotation was 4.5° and external rotation was 3.8°. Furthermore, there were no statistically significant differences (p > 0.05) in measurements of hip passive ROM between the left and right side using the different measurement devices (Figures 2 & 3).
Table 1.
Passive hip range of motion measurements.
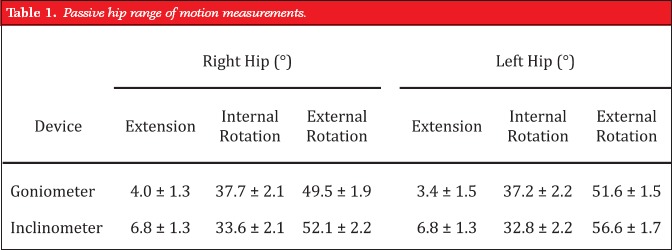 |
Figure 2.
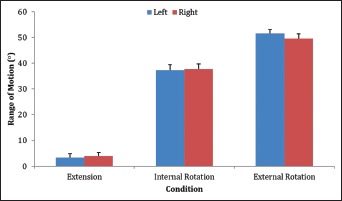
Hip range of motion measured by goniometer.
Figure 3.
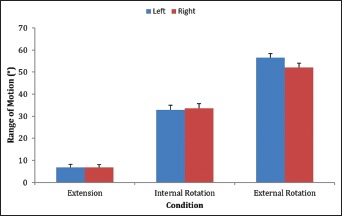
Hip range of motion measured by digital inclinometer.
In order to provide a visual presentation of the data between the goniometer and inclinometer, Bland‐Altman graphs were created (Figures 4, 5 & 6). These graphs present the mean difference (or bias) and the 95% limits of agreement between the two measurements.
Figure 4.
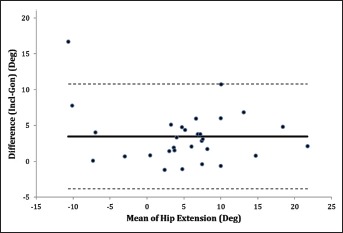
Hip Extension Bland‐Altman Graph. The solid lines represent the mean difference or bias (3.5°) between the goniometer and inclinometer and the dashed line represent the 95% limits of agreement (Upper Limit = 10.8°, Lower Limit = –3.9°).
Figure 5.
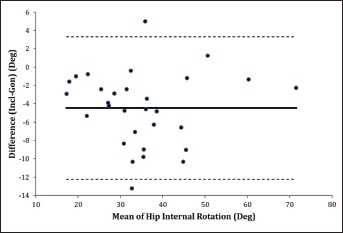
Hip Internal Rotation Bland‐Altman Graph. The solid lines represent the mean difference or bias (–4.5°) between the goniometer and inclinometer and the dashed line represent the 95% limits of agreement (Upper Limit = 3.3°, Lower Limit = –12.3°).
Figure 6.
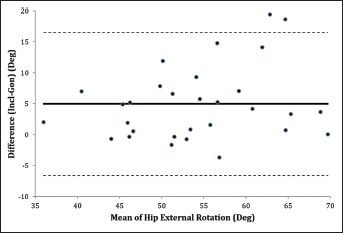
Hip External Rotation Bland‐Altman Graph. The solid lines represent the mean difference or bias (5°) between the goniometer and inclinometer and the dashed line represent the 95% limits of agreement (Upper Limit = 16.6°, Lower Limit = –6.6°).
DISCUSSION
The primary purpose of this study was to investigate the concurrent validity of the universal goniometer and digital inclinometer in order to determine whether the devices could be used interchangeably to assess hip ROM in healthy subjects. The current data demonstrated a statistically significant difference between the two devices. The digital inclinometer had greater measurement values during hip extension and external rotation.
For the goniometer and inclinometer the ICC’s were good to excellent at .80 and .90 respectively, when assessed in a pilot study prior to the actual data collection. This study was performed using only one examiner as other studies have demonstrated high intra‐examiner reliability with use of goniometer as compared with inter‐examiner reliability, which is generally noted to be low.8,10,21,22 These findings lend further support and agreement with other authors who had similar ICC findings during measurements of the hip and shoulder with the digital inclinometer.23–25These devices been found to have high intra‐tester reliability in some studies but contrasting results in others, thus leading to questions regarding the interchangeability of devices for measurement.9,11,18,22
The results of this study are important in that it is difficult to find studies that have examined the interchangeability of these two devices in measuring passive range of motion about the hip region. The two studies that have evaluated measurements about the hip using varied devices present results that contrast as to whether the two devices are concurrently valid.17,18 In addition, only one of the studies has looked at general ROM and hip rotation, making the current investigation an important addition to the literature. The fact that there is no consensus on the interchangeability of the devices indicates that caution needs to be utilized when comparing measured values of hip ROM obtained utilizing different devices. It also points out that a clinician should consistently measure using one or the other devices as both are reliable and valid, but not interchangeable. The choice regarding which device to utilize to measure ROM should be based on clinical availability, ease of use, clinician skill, and considerations for both reproducibility (validity) and reliability.
The results of the current study indicate that significant differences in measurements between the universal goniometer and digital inclinometer. This finding was consistent with other existing literature questioning the interchangeability of the two devices.18,22 It should be noted that the current data demonstrated a difference of up to 3.4° (hip extension), 5° (hip ER) and 4.4° (hip IR) between the goniometer and inclinometer. This is similar to the findings of Mullaney et al who noted a difference between the devices of 3–5° in measuring shoulder rotation.22 They recommended not using the devices interchangeably. Other authors have noted that the devices are interchangeable when being used for measurements of the hip, cervical spine, and shoulder region.9,11,26 It could be surmised that in light of these different findings that the body region being measured needs to be taken into consideration.
With respect to the measurements of hip extension, the current findings with measurements utilizing the modified Thomas test were not in agreement with other findings. The current data revealed mean hip extension values of 3.4° and 4.0° for left and right hip, respectively with goniometer; and 6.8° bilaterally with the inclinometer. Ferber et al reported EXT measurements of 10.6°, Harvey et al 11.9°, Young et al 13.7° and Wang et al between 2° and 14°.27–30 A reason for the difference between the current study and the above studies could have been the age and activity level. All of the studies demonstrating with greater ROM findings examined younger subjects, runners, or elite athletes. These subjects may have possessed either age related, inherent, or training induced enhanced mobility in hip extension as compared to the subjects in the current study. In addition, particular sports may require greater hip extension in order to be successful and avoid injury or participation in certain activities may create neuromuscular adaptations resulting in greater hip extension mobility. The subjects in the current study were “healthy normal.”
With regard to IR values, the current data were in accordance with the majority of existing literature. Mean values for hip IR were 33.2° and 37.5° for the inclinometer and universal goniometer, respectively. This is consistent with the values reported in the literature for hip IR that range from 29.8° to 36°.31–35 Where the current data differed were in the measurements of hip ER, 54.5° to 55.5° for the inclinometer and goniometer, respectively. These values were greater than measurements reported by previous authors, that ranged between 30.43° to 48°. The smallest value of 30.43° was noted by Van Dillen et al31 and was measured in a prone position similar to the position used in the current study. The largest value of 48° was measured in the supine position by Malliaras.33 Kouyoumdjian et al noted in their study of 120 adults ranging in age from 20–60 years of age that body mass index, age and gender were the deciding factors in values of hip rotation.36 It is imperative that the methodology utilized by researchers in future studies are aware of the significant differences in values obtained through positioning as Simoneau noted a difference of approximately 9° between seated (36°) and prone (45°).32 The greater ER values between the current investigation and other’s findings may be explained as a result of differences in subject’s activity level or strictness of criteria as to what constituted pelvic stabilization. It is important to acknowledge that gender, age, subject measurement position, and whether active or passive ROM was measured can all influence values.
STUDY LIMITATIONS
The main limitation during data collection was stabilization of the pelvis during measurements. As other authors have noted, stabilizing the pelvis during the modified Thomas test, and for passive hip ROM in general, is very important in order to achieve consistency during hip measurement.2,19 Other authors have used various techniques to increase or objectigy stabilization such as utilizing a blood pressure cuff under lumbar spine region to provide feedback for subjects, utilizing separate assistant to hold knee to chest region, and asking subjects to actively flatten the lumbar region.15,37 Those procedures were not administered during this study as the verbal and tactile cues were observed to be sufficient and more likely to be carried out in a regular practice setting. It was noted however that many subjects had a tendency to pull their knee toward ipsilateral shoulder and into external rotation and abduction (ABD) with the modified Thomas test. This positioning had to be corrected with instructions to bring knee toward the head as the ER/ABD position was noted to give a false recording of increased hip extension during the pilot study. The use of the inclinometer also allowed for much easier use of tactile feedback providing a distinct advantage over goniometer.
Furthermore, the investigator was not blinded to the measurements, which could have enhanced reliability. However, a second investigator was recording all the measurements while the principal investigator read the measurements. Lastly, it is possible that always performing the goniometric measurements first followed by the inclinometer measures second may have resulted in increased PROM measurements due to an order effect.
This study added further evidence that intra‐rater reliability is good to excellent with both of the devices utilized but did not examine inter‐rater reliability. Future research should use multiple examiners with suggestion to perform a pre‐measurement training session to increase likelihood of good ICC’s. Additionally, the use of examiners with different degrees of experience is recommended as Elveru et al. note greater reliability with increased clinical practice.38
CONCLUSION
Significant differences were found between the PROM hip measurement values obtained with a standard goniometer and a digital inclinometer in all measured hip motions, with exception of right hip extension. The differences were noted to be between 3–5 degrees for all planes measured with the digital inclinometer demonstrating greater measurement values during EXT and ER. Although both devices demonstrate validity for measuring hip ROM, the current results indicate that the two devices are not concurrently valid in measurements of the hip EXT, IR and ER. These findings suggest that caution should be used if the devices are to be used interchangeably in order to quantify hip passive range of motion.
REFERENCES
- 1. Holm I, B Bolstad, T Lutken, et al. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248 [DOI] [PubMed] [Google Scholar]
- 2. Nussbaumer S, M Leunig, JF Glatthorn, et al. Validity and test‐retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord. 2010;11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cibulka MT, DR Sinacore, GS Cromer, et al. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila Pa 1976). 1998;23:1009–1015 [DOI] [PubMed] [Google Scholar]
- 4. Zifchock RA, I Davis, J Higginson, et al. Side‐to‐side differences in overuse running injury susceptibility: a retrospective study. Hum Mov Sci. 2008;27:888–902 [DOI] [PubMed] [Google Scholar]
- 5. Franettovich MM, TG McPoil, T Russell, et al. The ability to predict dynamic foot posture from static measurements. J Am Podiatr Med Assoc. 2007;97:115–120 [DOI] [PubMed] [Google Scholar]
- 6. Hayes K, JR Walton, ZR Szomor, et al. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289–294 [DOI] [PubMed] [Google Scholar]
- 7. Watkins MA, DL Riddle, RL Lamb, et al. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71:90–96; discussion 96–97 [DOI] [PubMed] [Google Scholar]
- 8. Herrero P, P Carrera, E Garcia, et al. Reliability of goniometric measurements in children with cerebral palsy: a comparative analysis of universal goniometer and electronic inclinometer. A pilot study. BMC Musculoskelet Disord. 2011;12:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clapis PA, SM Davis, RO Davis. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother Theory Pract. 2008;24:135–141 [DOI] [PubMed] [Google Scholar]
- 10. Boone DC, SP Azen, CM Lin, et al. Reliability of goniometric measurements. Phys Ther. 1978;58:1355–1360 [DOI] [PubMed] [Google Scholar]
- 11. Kolber MJ, WJ Hanney. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. Int J Sports Phys Ther. 2012;7:306–313 [PMC free article] [PubMed] [Google Scholar]
- 12. Boyd BS. Measurement properties of a hand‐held inclinometer during straight leg raise neurodynamic testing. Physiotherapy. 2012;98:174–179 [DOI] [PubMed] [Google Scholar]
- 13. Gajdosik RL, RW Bohannon. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67:1867–1872 [DOI] [PubMed] [Google Scholar]
- 14. Peeler JD, JE Anderson. Reliability limits of the modified Thomas test for assessing rectus femoris muscle flexibility about the knee joint. J Athl Train. 2008;43:470–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moreside JM, SM McGill. Quantifying normal 3D hip ROM in healthy young adult males with clinical and laboratory tools: hip mobility restrictions appear to be plane‐specific. Clin Biomech (Bristol, Avon). 2011;26:824–829 [DOI] [PubMed] [Google Scholar]
- 16. Kolber MJ, F Vega, K Widmayer, et al. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother Theory Pract. 2011;27:176–184103109/09593985.2010.481011. [DOI] [PubMed] [Google Scholar]
- 17. Clapis PA DS, Davis RO. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiotherapy Theory and Practice. 2008;24:135–141 [DOI] [PubMed] [Google Scholar]
- 18. Bierma‐Zeinstra SM, AM Bohnen, R Ramlal, et al. Comparison between two devices for measuring hip joint motions. Clin Rehabil. 1998;12:497–505 [DOI] [PubMed] [Google Scholar]
- 19. Kendall FP ME, Provance P. Muscles, Posture and Pain. 4th ed. Baltimore, MD: Williams and Wilkins, 1993 [Google Scholar]
- 20. Ekstrand J, M Wiktorsson, B Oberg, et al. Lower extremity goniometric measurements: a study to determine their reliability. Arch Phys Med Rehabil. 1982;63:171–175 [PubMed] [Google Scholar]
- 21. van Trijffel E, RJ van de Pol, RA Oostendorp, et al. Inter‐rater reliability for measurement of passive physiological movements in lower extremity joints is generally low: a systematic review. J Physiother. 2010;56:223–235 [DOI] [PubMed] [Google Scholar]
- 22. Mullaney MJ, MP McHugh, CP Johnson, et al. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theory Pract. 2010;26:327–333 [DOI] [PubMed] [Google Scholar]
- 23. Herrero P, P Carrera, E Garcia, et al. Reliability of goniometric measurements in children with cerebral palsy: a comparative analysis of universal goniometer and electronic inclinometer. A pilot study. BMC Musculoskelet Disord. 2011;12:15510.1186/1471–2474‐12–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kolber MJ HW. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. International Journal of Sports Physical Therapy. 2012;7:306–311 [PMC free article] [PubMed] [Google Scholar]
- 25. Boyd BS. Measurement properties of a hand‐held inclinometer during straight leg raise neurodynamic testing. Physiotherapy. 2012;98:174–17910.1016/j.physio.2011.04.352. [DOI] [PubMed] [Google Scholar]
- 26. Wolfenberger VA, Q Bui, GB Batenchuk. A comparison of methods of evaluating cervical range of motion. J Manipulative Physiol Ther. 2002;25:154–160 [DOI] [PubMed] [Google Scholar]
- 27. Ferber R, KD Kendall, L Farr. Changes in knee biomechanics after a hip‐abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011;46:142–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Harvey D. Assessment of the flexibility of elite athletes using the modified Thomas test. Br J Sports Med. 1998;32:68–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Young W CP, Otago L, Liddell D. Relationship Between a Modified Thomas Test and Leg Range of Motion in Australian‐Rules Football Kicking J. Sport Rehabil. 2003;12:343–350 [Google Scholar]
- 30. Wang SS, SL Whitney, RG Burdett, et al. Lower extremity muscular flexibility in long distance runners. J Orthop Sports Phys Ther. 1993;17:102–107 [DOI] [PubMed] [Google Scholar]
- 31. Van Dillen LR, NJ Bloom, SP Gombatto, et al. Hip rotation range of motion in people with and without low back pain who participate in rotation‐related sports. Phys Ther Sport. 2008;9:72–8110.1016/j.ptsp.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Simoneau GG, KJ Hoenig, JE Lepley, et al. Influence of hip position and gender on active hip internal and external rotation. J Orthop Sports Phys Ther. 1998;28:158–164 [DOI] [PubMed] [Google Scholar]
- 33. Malliaras P, A Hogan, A Nawrocki, et al. Hip flexibility and strength measures: reliability and association with athletic groin pain. Br J Sports Med. 2009;43:739–744 [DOI] [PubMed] [Google Scholar]
- 34. Roach KE, TP Miles. Normal hip and knee active range of motion: the relationship to age. Phys Ther. 1991;71:656–665 [DOI] [PubMed] [Google Scholar]
- 35. Nussbaumer S, M Leunig, JF Glatthorn, et al. Validity and test‐retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord. 2010;11:19410.1186/1471–2474‐11–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kouyoumdjian P, R Coulomb, T Sanchez, et al. Clinical evaluation of hip joint rotation range of motion in adults. Orthop Traumatol Surg Res. 2012;98:17–2310.1016/j.otsr.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 37. Schache AG, PD Blanch, AT Murphy. Relation of anterior pelvic tilt during running to clinical and kinematic measures of hip extension. Br J Sports Med. 2000;34:279–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Elveru RA, JM Rothstein, RL Lamb. Goniometric reliability in a clinical setting. Subtalar and ankle joint measurements. Phys Ther. 1988;68:672–677 [DOI] [PubMed] [Google Scholar]


