Abstract
Restricted hip mobility has shown strong correlation with various pathologies of the hip, lumbar spine and lower extremity. Restricted mobility can consequently have deleterious effects not only at the involved joint but throughout the entire kinetic chain. Promising findings are suggesting benefit with skilled joint mobilization intervention for clients with various hip pathologies. Supervised home program intervention, while lacking specifically for the hip joint, are demonstrating promising results in other regions of the body. Application of an accompanying home program for the purpose of complementing skilled, in clinic intervention is advisable for those clients that respond favorably to such methodology.
Level of Evidence:
5
Keywords: Hip joint, Home program, Mobilization
PROBLEM
Hip mobility limitations have been suggested to be present in some conditions of the lumbar spine1–4 as well as in more distal lower extremity pathologies.5–7 Directly relevant to the hip itself these mobility limitations have been found in clients with osteoarthritis,8–10 sports related groin pain,11,12 and femoroacetabular impingement (FAI) and/or hip labral tear.10,13
Lower extremity range‐of‐motion (ROM) deficits are often noticed in clients with various hip joint pathologies. Clients with FAI and labral tear tend to exhibit reduced hip ROM for flexion, internal rotation, and/or adduction.14–18 Athletes with groin pain were also found to have limited hip ROM.11,12 Strong predictor variables for the presence of hip osteoarthritis include squatting as an aggravating factor,19 as well as limited hip internal rotation ROM.8,9,19 Additionally, decreased ROM of hip abduction has been suggested to predict the occurrence of future lower extremity injuries.20 Therefore, it is important to minimize the deleterious effects of limited ROM if possible.
Limitations in flexion and internal rotation ROM have been implicated as characteristic of hip pathology.14–18 Any sport that requires squatting, pivoting, plant and cut, and similar movements will approximate these positions. Other sport‐related activities do not frequently require this combination of movement. Upright running, for example, is such an example and is a particularly important skill requirement of most sports. Limited hip extension flexibility has been proposed as one possible cause of increased anterior pelvic tilt and lumbar lordosis during running.21,22 Currently, there are few published investigations regarding limited hip extension in running athletes. Additionally, the literature that is available does not clearly elucidate the reason for this limited hip extension, although it appears that the deficit in extension cannot be explained by muscle tightness alone.23 Therefore, careful assessment of the lumbar spine, pelvis, and hip should be undertaken in the running athlete lacking this motion in order to most appropriately intervene regarding their limitation(s).
When joint mobility restrictions limiting hip motions are discovered, an appropriate intervention to address these limitations is joint mobilization of the appropriate portions of the joint capsule, most likely the posterior, inferior and lateral portions.24,25 Achieving optimal client outcomes can be augmented with self‐mobilizations26 and muscle re‐education exercises in order to maintain treatment benefit. Furthermore, mobilization and muscle re‐education exercises have been suggested as part of a multi‐modal approach for hip pathology.27–30
Recent findings are suggestive of abnormal hip joint morphology in young athletes contributing to limited ROM, even those without pathology.31–34 The extent that these limitations in ROM are due to radiographic changes is not fully elucidated. Additionally, the extent to which joint ROM and mobility can be improved in a client with radiographic changes is not currently understood. The individual anatomical geometry of the proximal femur and acetabulum only partly influences restricted mobility and function. A hip with an abnormal radiographically illustrated morphology may not be destined for arthritic degeneration.35,36 The clinician must consider though whether joint mobilization is an appropriate component of the treatment plan. For the client with bony morphologic changes, mobilizations may be inappropriate. As with all employed interventions, client tolerance and re‐assessment to a trial of joint mobilization and muscle re‐education intervention is necessary (if it is even appropriate at all). The utilization of skilled joint mobilization interventions supplemented with an appropriately implemented self‐mobilization program may be of benefit for the client with mobility deficits.
SOLUTION
There are various methods to self‐mobilize and/or re‐educate hip musculature for the client with either hip intra‐ or extra‐articular pathology. The goal with each of the self‐mobilization techniques is to improve capsule and potentially other connective tissue mobility. The goals of the combined techniques (self‐mobilization and muscle re‐education) are also to improve capsule and connective tissue mobility, as well as improve muscle re‐education. Additionally, often with these techniques the recruited muscles can assist with optimizing hip joint movement. In some cases, this improved joint movement may significantly alleviate the athlete or client’s symptoms. All of the techniques described in this clinical suggestion may be carried out in a clinical setting as clinician directed multi‐modal treatment including both therapeutic exercise and manual therapy interventions. With proper in‐clinic instructions selected clients may be able to enhance their treatment plan by performing a series of selected self‐mobilization techniques and end range exercises as part of a home rehabilitation program. These techniques are not, and should not, be employed as an alternative to a skilled intervention applied by a properly trained clinician. They are simply adjuncts to achieving the treatment goals of the clinician and client. Application of these techniques is beneficial after the clinician has performed them directly on the client in the clinic.
The authors have selected a variety of self‐hip mobilization techniques for possible integration into a home program. Clinicians should base their prescription of self‐hip mobilization based on a thorough clinical evaluation and examination as well as consideration of the client’s vocational, avocational, and athletic goals. While there is no direct evidence to support that hip self‐mobilizations are effective in their own right, tangential evidence demonstrates that prescriptive, supervised home programs to which the client adheres, result in improved outcomes compared to non‐supervised exercises.37–41
Client safety should be kept in mind when prescribing self‐hip mobilization techniques. Clinicians should consider the variables of mobilization including: force magnitude, force direction, and duration when sending a client home with a self‐mobilization technique. Contraindications to self‐hip joint mobilization include but are not limited to a history of fracture, recent surgery, anticoagulation medication, worsening of symptoms, generalized and local ligamentous laxity, and systemic illness. The client must be independent and safe with all of these techniques prior to their utilization.
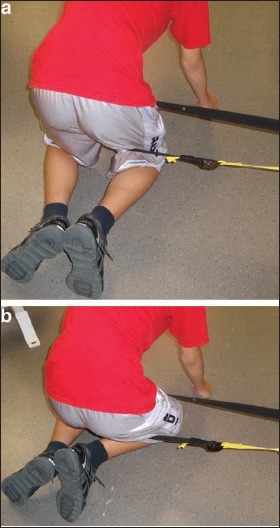
Hip Inferior‐Posterior Glide with/without Muscle Re‐Education in Hip Flexion
This self‐mobilization technique is likely most appropriate for the client with restricted hip flexion and adduction such as those with FAI and requires the use of a towel, some version of weight, a rope/strap, and a stable step close to a stable surface that the client can hold onto for balance. The client places their involved foot onto the step. The weight(s) are tied to the jump rope (in this case). The jump rope is then tied to the towel and the towel is wrapped around the client’s thigh and placed as close to the hip joint as possible. The client grasps both handles of jump rope in order to control weight and decrease/increase the load on the hip as tolerated (Figure 1). The amount of weight applied is dependent on the client tolerance, safety, goal of the exercise, and weight availability. Once the proper weight is established according to therapist‐determined guidelines, the client is instructed to perform a step‐up (Figure 2) or step‐back (Figure 3). The client should monitor for the sheet slipping down the thigh with the step‐up. If it is not possible to get the sheet tight enough to prevent it from slipping down the thigh and still remain comfortable, this technique should not be performed, or the client should start in greater hip flexion (Figure 3) and step‐up to the mid‐range (Figure 1). Volume of exercise performance should be individualized to the client.
Figure 1.

Inferior‐posterior glide with towel‐jump rope set‐up – start position.
Figure 2.

Inferior‐posterior glide with towel‐jump rope set‐up – finish position.
Figure 3.

Inferior‐posterior glide with towel‐jump rope set‐up – step‐back finish position.
If the clinician only wants the client to use this technique as a self‐mobilization, the client stays in the original starting position (Figure 1). If the weight becomes too heavy during the self‐mobilization, or if the clinician prefers the client perform more of an oscillatory technique versus a sustained mobilization, the client pulls up on the jump rope handles and “unload” the weight on the anterior thigh. The client can (if so instructed by the clinician) lift the weight up and lower in oscillatory manner similar to joint mobilizations performed by the clinician. The clinician must be satisfied that the client can perform these techniques safely and efficiently prior to their prescription.
Hip Inferior and Lateral Glides with Hip Flexion Movement
Research outcomes have demonstrated that clients with FAI have limited squatting motion compared to controls due to limited pelvic sagittal plane motion.42 The depth of squat has also been improved in clients with FAI post‐surgically, and theorized as a result of reduced acetabular coverage and an improved pelvic posterior inclination angle.43 Theoretically, improving capsular mobility (in cases of limitations) may be beneficial. Therefore, this technique is likely most beneficial for the client with limited hip flexion motion in a loaded position.
With the same set‐up as in the technique described in Figure 1, the client is asked to further flex their hip via moving their trunk/upper body down toward the floor (e.g. pelvic on femoral hip flexion). This same technique can be performed with a self‐lateral distraction mobilization in place of the inferior glide. Instead of weights (unless the client has access to a weighted pulley system and weight belt), a rope/jump rope or belt/strap can be tied to the end of the sheet or a weightlifting belt (Figure 4). A large knot (or the handles of the jump rope) is placed on the other side of a solid, closed door that is not currently being used or, as in Figure 4, the strap is tied to a solid non‐moving surface. The client can then perform the same movement described above to gain further hip flexion (via pelvic on femoral movement). Since this is a self‐mobilization technique without specific muscle re‐education, the volume of the exercise is more likely tolerated and can therefore be increased. Three sets of 30 repetitions twice a day is suggested.
Figure 4.

Pelvic on femoral flexion movement with laterally directed femur glide.
The client can also perform both of these pelvic on femoral techniques in a lunge or squat (Figures 5 & 6) position. Using the strap/rope set‐up the goal is to maintain a laterally directed distraction of the hip joint while the client performs the task (e.g. squatting or lunging).
Figure 5.

Pelvic on femoral flexion movement with laterally directed femur glide during squat.
Figure 6.

Pelvic on femoral flexion movement with laterally directed femur glide and muscle re‐education during squat.
Using the weighted pulley system can be advantageous when the goal is concurrent gains in mobility and muscle re‐education. The client performs the same movement as in Figure 5, except with the use of a weighted pulley system versus a solid strap. The client is instructed to use enough resistance to challenge the maintenance of a stance position. The client is instructed to maintain their position by pushing with their inside foot (client’s right foot in Figure 5) toward the pulley system. This cueing should require the client to dynamically activate their right hip abductor and/or external rotator muscles groups.
Hip Posterior Glide with/without Movement
This technique best selected for a client with posterior and lateral capsular restrictions and requires a solid bench or chair and good upper body strength to perform. The client places the involved knee on the solid supporting surface. This can be padded if necessary for comfort. The client grasps each side of the surface (flexing their hip to approximately 90°) and attempts to pull their trunk toward the surface, imparting a posterior glide to the hip joint (Figure 7). The client may rock their body posterior or posterior‐lateral in order to add movement during the mobilization (Figure 8). Posterior‐lateral motion will increase the stretch to the posterior‐lateral hip, as well as increase the likelihood of approximating the position of hip impingement. The clinician must therefore be careful to avoid impingement of the hip and properly instruct the client the importance of avoiding anterior hip symptoms. As in the above technique, a laterally directed distraction mobilization force can be utilized with the weight pulley system or the rope/sheet /belt (Figure 9).
Figure 7.

Unilateral weight‐bearing posterior glide.
Figure 8.

Unilateral weight‐bearing posterior‐lateral glide.
Figure 9.
Kneeling lateral hip distraction weight shift a) start position, b) finish position.
Active movement can also be utilized with a laterally directed distraction force for muscle re‐education (Figure 10). In this technique the self‐posterior glide is maintained via weight through the involved femur (either as shown or on a bench as in Figures 7 & 8), with a lateral glide via belt as the client moves into the same position as in Figure 9. This posterior‐lateral directed force is emphasized on clients who are determined to have restricted movements due to posterior and lateral capsular restrictions and may be selected in client’s with hip flexion and internal rotation motion deficits.
Figure 10.

Kneeling lateral hip distraction with active internal rotation movement.
In general, most researchers believe that FAI morphology is correlated with restricted posterior hip mobility, but the clinician must be mindful of the fact that posterior hip joint instability has also been described in these clients.44,45 It is theorized that the early interaction between the aspherical femoral head and the prominent acetabular rim acts as a fulcrum, making these hips more susceptible to traumatic posterior dislocation.45 Therefore, the clinician should select the appropriate client wisely; using this (and similar techniques) with caution. Clients with significant bony changes in their hip, undetermined end‐feels, and poor response to preliminary mobilization in the clinic are likely not appropriate candidates for these techniques.
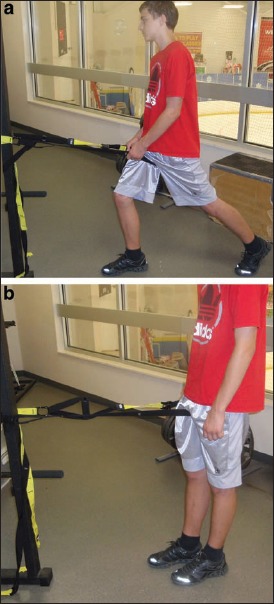
Hip Lateral Glide with/without Muscle Re‐Education
The client is standing upright for this technique. The self‐distraction is laterally directed. The technique can be utilized as a laterally directed self‐mobilization or laterally directed self‐mobilization with movement. The client stands with leg to be mobilized closest to the stable surface that the belt/strap is attached to (Figure 11a). Adducting that leg over the non‐involved leg can increase the lateral hip tension, but may also increase the risk of mechanical impingement. The client can either push their hips away from support surface or push shoulders and hips away with arm closest to the stable surface. Pushing the shoulders away as in Figure 11b also provides a stretch to the lateral trunk, hip and iliotibial band.
Figure 11.

Standing lateral hip distraction – a) start position, b) finish position.
For the standing self‐mobilization/muscle re‐education technique, the client starts with the involved leg adducted across midline as in Figure 11 (this time using a weighted pulley system) and then (using closed‐chain abduction of the involved leg) moves to the finish position (Figure 12). Performing this technique requires gluteus medius concentric muscle activation and returning to the starting position requires eccentric activity of the gluteus medius. Since this technique requires muscle activation and poor endurance of the gluteus medius has shown correlation to pathology,46 an initial exercise prescription should be in the range of 2–3 sets of 15–20 repetitions.
Figure 12.

Standing lateral hip distraction with muscle re‐education – a) start position, b) finish position.
Standing self‐mobilization without muscle re‐education can also be performed in various ranges of hip flexion, as well as in loaded or unloaded conditions. Similar to the technique in Figure 4, the client can utilize a lateral hip distraction while adding overpressure (Figure 13). This technique may be particularly beneficial for the client that cannot tolerate full weight‐bearing hip flexion and adduction, as in the kneeling and squatting techniques. In this technique the client uses their contralateral hand to pull the ipsilateral knee into adduction (as well as internal rotation if the foot is fixed on a stable surface). The lateral distraction can assist with overall capsular stretch. Adding the adduction will increase lateral hip stretch. The internal rotation may emphasize stretch to the posterior capsule. For the client with increased groin/hip pain with hip flexion, this technique may offer special benefit.27 This technique would particularly be beneficial for the client who is being treated with (and tolerating well) lateral and posterior hip distraction techniques. We have found this technique to be of particular benefit to the client who requires the lateral hip distraction with passive internal rotation movement.
Figure 13.

Standing lateral hip distraction with overpressure.
Hip Anterior Glide with Muscle Re‐Education
A less commonly described restriction, albeit important one to correct is a restricted anterior glide. Correcting an anterior glide is particularly important to the client lacking hip extension. For the client with a fairly significant restriction, the technique shown in Figures 14a & 14b could be employed. The client starts in flexion short of the restriction and (with an anterior glide force assisting the femoral head anterior) pulls their body forward creating hip extension. Muscle re‐education is utilized in such a case as the hip extensors are recruited to perform this motion. For the client lacking end‐range hip extension (or hip extension past neutral), the client can start in position shown in Figure 14b and step forward with their non‐involved leg. Achieving extension past neutral may be of particular importance to the running athlete. The clinician must pay particular attention to the lumbar spine in these clients. The client with restricted hip extension may involuntarily recruit lumbar spine extension instead of hip extension during such tasks.
Figure 14.
Standing anterior glide with active movement: a) start position, b) finish position.
Hip Long‐Axis Distraction
For the client with multi‐planar restricted capsular mobility, or the client requiring sustained overall capsular stretch, the supine long‐axis distraction (Figure 15) can be a particularly effective technique. Clients with osteoarthritis, for example, have demonstrated multi‐planar restrictions of ROM.8,9 The clinician should consider that, due to the geometry of the hip joint, this technique is essentially an inferior glide. For overall capsular mobilization, the lateral distraction techniques may be more beneficial on some clients. When the client responds favorably to long axis distraction during a clinic session, this technique may be a home program option. The uses of a weighted pulley system, heavy elastic tubing, or a belt attached to a solid surface are options. By positioning themselves in a supine position, strategically on the floor, the client may receive the distraction force in mid or end range hip abduction or hip rotation. Mid‐range hip distraction may help gate pain and relieve symptoms whereas targeted distraction at end range abduction or rotation may improve mobility. Using a belt requires the client to move up toward their head to provide the distraction force. Using a weighted pulley system requires careful monitoring of response by the client. As shown, this technique is likely to provide lower level distraction force. If the client tolerates, and the goal is to increase the distraction, the contralateral hip and knee can be flexed and the foot planted on the floor. The client can then push on the floor with this foot to slide their body up toward their head, increasing the distraction force. As with all techniques, overstretching is not suggested. Treatment should be stopped immediately if any numbness, tingling or other adverse responses occur.
Figure 15.

Supine long axis distraction.
DISCUSSION
The aforementioned self‐hip mobilizations are meant to be integrated by the clinician into a multimodal therapeutic home exercise program for the client. Little evidence exists to describe the efficacy of these self‐hip mobilizations or to demonstrate one technique’s value over another. The authors’ endorsement of these self‐selected hip mobilizations is based on anecdotal observations and a shared opinion of benefit that exists in the absence of evidence. Therefore clinicians are strongly encouraged to utilize these techniques as adjunct to other treatment techniques and not in absence of interventions supported by higher‐level evidence (e.g. in clinical manual therapy techniques).26–29 In addition, as with all home exercise prescription, the client must completely understand the indications/contraindications/precautions/concerns with the technique. Proper performance of the technique in the clinic at least 1–2 times with independence is suggested prior to HEP implementation.
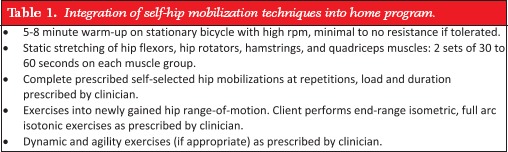
Table 1 outlines how these self‐hip mobilization techniques can be integrated into a home program. First, the client needs to perform a metabolic warm‐up using cardio fitness equipment or by walking or jogging outside. This warm‐up may involve several minutes on a stationary bicycle or an elliptical trainer. For the client with pain during the combined motions of flexion and adduction/internal rotation the elliptical trainer/walking/jogging are more appropriate choices compared to the bicycle. Once the warm‐up is complete, the client should spend several minutes carrying out several 30–60 second static stretches of the hip joint in order to prepare the hip joint for the self‐selected mobilization technique. Following the static stretches, the client should perform the prescribed self‐mobilization techniques with the correct load, position, and duration as prescribed by the clinician. Following the self‐joint mobilizations, it is critical that the client perform several repetitions of dynamic exercises, isometric end‐range exercises, and isotonic exercises through the end ranges of their hip motions to re‐educate the musculature and assist with maintaining the newly gained ROM. Finally, several dynamic drills can be performed to achieve neuromuscular control in the new hip ranges. Although it is unknown if this protocol is effective in improving ROM, the use of a protocol is warranted as it allows for consistent application of the hip self‐mobilization techniques and helps avoid unwarranted practice variations in home program dosing and prescription.
Table 1.
Integration of self‐hip mobilization techniques into home program.
 |
Finally, although it remains unknown if self‐mobilization for the hip is of significant benefit to the client with hip mobility deficits, it does allow for some carry over of manual techniques outside of the clinic setting. This may improve home program adherence, functional outcomes, and client independence in the management of their hip joint mobility deficits.41
REFERENCES
- 1. Reiman MP, Weisbach PC, Glynn PE. The hips influence on low back pain: a distal link to a proximal problem. J Sport Rehabil. 2009;18(1):24–32 [DOI] [PubMed] [Google Scholar]
- 2. Devin CJ, McCullough KA, Morris BJ, Yates AJ, Kang JD. Hip‐spine syndrome. J Am Acad Orthop Surg. 2012;20(7):434–442 [DOI] [PubMed] [Google Scholar]
- 3. Burns SA, Mintken PE, Austin GP. Clinical decision making in a patient with secondary hip‐spine syndrome. Physiother Theory Pract. 2011;27(5):384–397 [DOI] [PubMed] [Google Scholar]
- 4. Burns SA, Mintken PE, Austin GP, Cleland J. Short‐term response of hip mobilizations and exercise in individuals with chronic low back pain: a case series. J Man Manip Ther. 2011;19(2):100–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reiman MP, Bolgla LA, Lorenz D. Hip functions influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehabil. 2009;18(1):33–46 [DOI] [PubMed] [Google Scholar]
- 6. Cliborne AV, Wainner RS, Rhon DI, et al. Clinical hip tests and a functional squat test in patients with knee osteoarthritis: reliability, prevalence of positive test findings, and short‐term response to hip mobilization. J Orthop Sports Phys. Ther. 2004;34(11):676–685 [DOI] [PubMed] [Google Scholar]
- 7. Currier LL, Froehlich PJ, Carow SD, et al. Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short‐term response to hip mobilization. Phys Ther. 2007;87(9):1106–1119 [DOI] [PubMed] [Google Scholar]
- 8. Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514 [DOI] [PubMed] [Google Scholar]
- 9. Birrell F, Croft P, Cooper C, et al. Predicting radiographic hip osteoarthritis from range of movement. Rheumatology (Oxford). 2001;40(5):506–512 [DOI] [PubMed] [Google Scholar]
- 10. Agricola R, Heijboer MP, Bierma‐Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2012 [DOI] [PubMed] [Google Scholar]
- 11. Nevin F, Delahunt E. Adductor squeeze test values and hip joint range of motion in Gaelic football athletes with longstanding groin pain. J Sci Med Sport. 2013 [DOI] [PubMed] [Google Scholar]
- 12. Taylor CJ, Pizzari T, Ames N, Orchard JW, Gabbe BJ, Cook JL. Groin pain and hip range of motion is different in Indigenous compared to non‐indigenous young Australian football players. J Sci Med Sport. 2011;14(4):283–286 [DOI] [PubMed] [Google Scholar]
- 13. Kubiak‐Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124 [DOI] [PubMed] [Google Scholar]
- 14. Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88(7):1448–1457 [DOI] [PubMed] [Google Scholar]
- 15. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris‐Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop. 2009;467(3):638–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Prather H, Hunt D, Fournie A, Clohisy JC. Early intra‐articular hip disease presenting with posterior pelvic and groin pain. Pm R. 2009;1(9):809–815 [DOI] [PubMed] [Google Scholar]
- 17. Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1041–1047 [DOI] [PubMed] [Google Scholar]
- 18. Song Y, Ito H, Kourtis L, Safran MR, Carter DR, Giori NJ. Articular cartilage friction increases in hip joints after the removal of acetabular labrum. J Biomech. 2012;45(3):524–530 [DOI] [PubMed] [Google Scholar]
- 19. Sutlive TG, Lopez HP, Schnitker DE, et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. J Orthop Sports Phys Ther. 2008;38(9):542–550 [DOI] [PubMed] [Google Scholar]
- 20. Dallinga JM, Benjaminse A, Lemmink KA. Which screening tools can predict injury to the lower extremities in team sports?: a systematic review. Sports Med. 2012;42(9):791–815 [DOI] [PubMed] [Google Scholar]
- 21. Bach DK, Green DS, Jensen GM, Savinar‐Nogue E. A comparison of muscular tightness in runners and nonrunners and the relation of muscular tightness to low back pain in runners. J Orthop Sports Phys Ther. 1985;6(6):315–323 [DOI] [PubMed] [Google Scholar]
- 22. Klein KK, Roberts CA. Mechanical problems of marathoners and joggers. Cause and solution. Am Correct Ther J. 1976;30(6):187–191 [PubMed] [Google Scholar]
- 23. Wang SS, Whitney SL, Burdett RG, Janosky JE. Lower extremity muscular flexibility in long distance runners. J Orthop Sports Phys Ther. 1993;17(2):102–107 [DOI] [PubMed] [Google Scholar]
- 24. Loudon JK, Manske RC, Reiman MP. Clinical mechanics and kinesiology. Champaign, IL: Human Kinetics; 2013 [Google Scholar]
- 25. Cook CE. Orthopedic Manual Therapy: An Evidence Based Approach. 2nd ed. Upper Saddle River, New Jersey: Pearson Education, Inc; 2012 [Google Scholar]
- 26. Wright AA, Hegedus EJ. Augmented home exercise program for a 37‐year‐old female with a clinical presentation of femoroacetabular impingement. Man Ther. 2012;17(4):358–363 [DOI] [PubMed] [Google Scholar]
- 27. Cook KM, Heiderscheit B. Conservative management of a young adult with hip arthrosis. J Orthop Sports Phys Ther. 2009;39(12):858–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. MacDonald CW, Whitman JM, Cleland JA, Smith M, Hoeksma HL. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: A case series. J Orthop Sports Phys Ther. 2006;36(8):588–599 [DOI] [PubMed] [Google Scholar]
- 29. Hoeksma HL, Dekker J, Ronday HK, et al. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004;51(5):722–729 [DOI] [PubMed] [Google Scholar]
- 30. Abbott JH, Robertson MC, Chapple C, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–534 [DOI] [PubMed] [Google Scholar]
- 31. Agricola R, Bessems JH, Ginai AZ, et al. The development of Cam‐type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–1106 [DOI] [PubMed] [Google Scholar]
- 32. Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam‐type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444 [DOI] [PubMed] [Google Scholar]
- 33. Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93(19):e111(111–110). [DOI] [PubMed] [Google Scholar]
- 34. Yuan BJ, Bartelt RB, Levy BA, Bond JR, Trousdale RT, Sierra RJ. Decreased range of motion is associated with structural hip deformity in asymptomatic adolescent athletes. Am J Sports Med. 2013;41(7):1519–1525 [DOI] [PubMed] [Google Scholar]
- 35. Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow‐up. J Bone Joint Surg Br. 2009;91(2):162–169 [DOI] [PubMed] [Google Scholar]
- 36. Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93(5):580–586 [DOI] [PubMed] [Google Scholar]
- 37. Mannion AF, Helbling D, Pulkovski N, Sprott H. Spinal segmental stabilisation exercises for chronic low back pain: programme adherence and its influence on clinical outcome. Eur Spine J. 2009;18(12):1881–1891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142(9):776–785 [DOI] [PubMed] [Google Scholar]
- 39. McCarthy CJ, Mills PM, Pullen R, et al. Supplementation of a home‐based exercise programme with a class‐based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis. Health Technol Assess. 2004;8(46):iii–iv, 1–61 [DOI] [PubMed] [Google Scholar]
- 40. McCarthy CJ, Mills PM, Pullen R, Roberts C, Silman A, Oldham JA. Supplementing a home exercise programme with a class‐based exercise programme is more effective than home exercise alone in the treatment of knee osteoarthritis. Rheumatology (Oxford). 2004;43(7):880–886 [DOI] [PubMed] [Google Scholar]
- 41. Roddy E, Zhang W, Doherty M, et al. Evidence‐based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee‐the MOVE consensus. Rheumatology (Oxford). 2005;44(1):67–73 [DOI] [PubMed] [Google Scholar]
- 42. Lamontagne M, Kennedy MJ, Beaule PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop. 2009;467(3):645–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lamontagne M, Brisson N, Kennedy MJ, Beaule PE. Preoperative and postoperative lower‐extremity joint and pelvic kinematics during maximal squatting of patients with cam femoro‐acetabular impingement. J Bone Joint Surg Am. 2011;93 Suppl 2:40–45 [DOI] [PubMed] [Google Scholar]
- 44. Berkes MB, Cross MB, Shindle MK, Bedi A, Kelly BT. Traumatic posterior hip instability and femoroacetabular impingement in athletes. Am J Orthop (Belle Mead NJ). 2012;41(4):166–171 [PubMed] [Google Scholar]
- 45. Steppacher SD, Albers CE, Siebenrock KA, Tannast M, Ganz R. Femoroacetabular impingement predisposes to traumatic posterior hip dislocation. Clin Orthop Relat Res. 2013;471(6):1937–1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Marshall PW, Patel H, Callaghan JP. Gluteus medius strength, endurance, and co‐activation in the development of low back pain during prolonged standing. Hum Mov Sci. 2011;30(1):63–73 [DOI] [PubMed] [Google Scholar]


