Abstract
Background/Purpose:
Decreased strength of the hip musculature and altered mechanics of the lower extremity have been identified in individuals with patellofemoral pain (PFP). The aim of this study was to determine if a relationship exists between hip muscle strength and transverse and frontal plane motion at the hip and knee, and ipsilateral trunk flexion during a jump‐landing task in individuals with PFP.
Methods:
Fifteen individuals (10 females, 5 males) with PFP participated in this investigation. A three‐dimensional motion analysis system was utilized to assess trunk, hip, and knee kinematics during a jump‐landing task. An isokinetic dynamometer was utilized to assess concentric and eccentric strength of the hip musculature. Simple correlation analyses were performed to determine the relationships between hip muscle strength and peak frontal and transverse plane hip and knee kinematics and ipsilateral trunk flexion.
Results:
Decreased eccentric strength of the hip external rotators and abductors was significantly correlated to increased frontal plane motion at the hip and trunk, respectively (P<0.05).
Conclusions:
Based on these findings, eccentric strengthening exercises for the hip musculature may be an important component for clinicians to include when rehabilitating individuals with PFP who display increased frontal plane motion at the hip and trunk.
Level of Evidence:
2b
Keywords: anterior knee pain, biomechanics, hip musculature, jump
INTRODUCTION
Patellofemoral pain (PFP) is one of the most common chronic knee conditions reported among physically active individuals.1,2 The incidence has been reported to be as high as 15% percent among military populations and 8% among civilian populations.3,4 Although the prevalence of PFP is high among physically active individuals, its etiology is not well understood. Multiple biomechanical factors have been theorized to contribute to the development of PFP by altering the stresses within the patellofemoral joint. These factors include abnormal anatomical alignment, decreased strength of the hip and thigh musculature, and faulty lower extremity mechanics during dynamic activities.5,6 An increase in patellofemoral joint stress has been previously reported to occur with alterations in frontal and transverse plane motion at the hip and knee.7,8 In order to decrease this stress during dynamic activities, individuals need to maintain control of the lower extremity.
Researchers have speculated that decreased strength of the hip musculature may be a major contributor to control of the lower extremity during dynamic tasks.5,6 Individuals with PFP are reported to have decreased strength of the hip musculature, which may then lead to a lack of lower extremity dynamic control.9–15 Previous studies have produced conflicting evidence to support this proposed relationship between strength of the hip musculature and faulty lower extremity mechanics in healthy individuals.16–21 Far fewer studies have investigated the relationship between hip muscle strength and lower extremity mechanics in a PFP population as compared to the number of studies within a healthy population. These studies among individuals with PFP have also produced conflicting results.22,23 Dierks et al22 reported no association between isometric hip abduction strength and peak hip adduction angle at the beginning of a prolonged run in individuals with PFP but found a significant association between these two measures at the end of the prolonged run. Willson and Davis23 reported no associations between peak isometric hip abduction and external rotation strength and hip adduction and hip internal rotation excursions, respectively during a jumping task in individuals with PFP. Based on the conflicting results of these two studies, additional research is warranted to better understand if a relationship exists between hip muscle strength and lower extremity mechanics in individuals with PFP.
In addition to decreased strength of the hip musculature playing a role in faulty lower extremity mechanics, a decrease in hip muscle strength could also lead to poor dynamic control of the trunk. Research supports that individuals with weak hip abductors may laterally flex their trunk towards the weak side during dynamic movements in order to reduce the demands placed on the hip abductor musculature.24 This increase in lateral trunk flexion is thought to increase the knee abduction loads and could alter the stresses placed across the patellofemoral joint.6 To our knowledge, no investigations have determined if a relationships exists between frontal plane trunk motion and hip muscle strength in individuals with PFP. If a relationship exists, clinicians can use this information to guide rehabilitation programs for individuals with PFP.
The purpose of this investigation was to determine the relationship between concentric and eccentric strength of the hip musculature and frontal and transverse plane motion at the hip and knee during a jump‐landing task in individuals with PFP. A secondary purpose was to determine the relationship between concentric and eccentric hip muscle strength and ipsilateral trunk flexion during a jump‐landing task in individuals with PFP. The authors hypothesized that decreased strength of the hip abductors, extensors, and external rotators would be related to increased hip adduction, hip internal rotation, knee valgus, knee internal rotation, and ipsilateral trunk flexion.
METHODS
Subjects
Fifteen subjects with PFP (females=10; males=5; age=27.3 ± 4.1 years, height=171.3 ± 8.3 cm, mass=72.8 ± 17.4 kg; months with PFP=58 ± 65 months) volunteered to participate in this investigation. Participants were recruited via flyers posted around the university campus and through word of mouth. Interested participants were asked to contact the principal investigator to determine if he/she met the inclusion criteria for this investigation. Inclusion criteria included: 1) anterior or retropatellar knee pain present during at least two of the following activities‐ ascending/descending stairs, hopping/running, squatting, kneeling, and prolonged sitting; 2) insidious onset of symptoms not related to trauma; 3) pain on palpation of patellar facets; and 4) worst pain in the past week greater than 3 cm on a 10 cm visual analog scale. Inclusion criteria were adapted from Cowan et al (2002). Exclusion criteria included: 1) history of knee surgery; 2) clinical evidence of other trunk, hip, or knee pathology; 3) age greater than 40 or less than 18.
Procedures
All subjects reported to a research laboratory for a single testing session. Upon arrival to the research laboratory, all subjects read and signed an informed consent form approved by the University’s Institutional Review Board. The lower extremity affected or most affected by PFP was used during all data collection procedures. Prior to testing, demographics of age, height, weight and self‐report of PFP symptom duration were recorded for all subjects. Subjects also completed the Anterior Knee Pain Scale (AKPS)25 and a 10 cm visual analog scale (VAS) for “worst knee pain during the previous week”. The AKPS is a thirteen‐item self‐administered questionnaire that assesses knee function. A higher score on the AKPS suggests better perceived function, with a maximum score of 100. The anterior knee pain scale (AKPS) has previously been reported to be reliable and valid for use with a PFP population.26
Motion Analysis
A Flock of Birds® (Ascension Technologies, Inc., Burlington, VT) electromagnetic motion analysis system interfaced with a non‐conductive force plate (Bertex Corporation) was used to assess lower extremity kinematics and kinetics during a jump‐landing task. Kinematic and kinetic data were collected via Motion Monitor® software (Innovative Sports Training, Inc. Chicago, IL) at a sampling rate of 144 Hz and 1440 Hz, respectively. Electromagnetic sensors were placed on the subjects’ skin over the spinous process of C7, spinous process of L5, lateral aspect of the thigh, and anteromedial aspect of the proximal tibia. Each sensor was placed over an area of the least muscle mass to minimize potential sensor movement and secured using double sided tape, pre‐wrap, and athletic tape. Eight bony landmarks were digitized with the endpoint of a stylus on which a fifth receiver was mounted. The eight bony landmarks were: T12, xyphoid process, medial and lateral condyles of the femur, medial and lateral malleoli of the ankle, and left and right anterior superior iliac spine (ASIS) of the pelvis. T12 and the xyphoid process defined the thorax segment. Medial and lateral malleoli and femoral condyles were digitized to determine the ankle joint center and knee joint center, respectively. Left and right ASIS were digitized to determine the hip joint center of rotation using the Bell method.7
The jump‐landing task required subjects to jump forward from a 30‐cm high box, which was set at a distance of 50% of their height away from the force plate, land with the foot of their test leg on the force plate, and immediately rebound for maximal vertical height upon landing.
Each subject completed three successful trials of the jump‐landing task. A successful trial was characterized by performing a bilateral landing in a fluid motion and landing with the entire foot of the test leg on the force plate and the foot of the non‐test leg off to the side of the force plate. Force plate data was collected solely to determine the time period for stance phase of the jump‐landing task.
Strength Testing
Concentric and eccentric torque of the hip abductors, hip external rotators, and hip extensors were assessed using an isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, NY). Order of strength testing was randomized for each subject. Subjects were allowed three submaximal practice repetitions prior to testing. No subjects needed more than three practice repetitions to perform the tests in a smooth manner. Five maximal test repetitions for hip abduction, external rotation, and extension were collected for each strength test. Each subject was provided two minutes of rest between each strength test. All strength testing was performed at 60 degrees/second. Intra‐session reliability (ICC2,1) for the testing protocol used in this investigation has previously been reported from our laboratory and ranged from 0.72–0.95.27
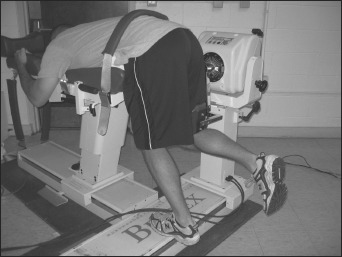
Hip abduction torque was assessed with participants in a side‐lying position with the test leg on top of the non‐test leg (Figure 1). The non‐test leg and trunk were stabilized using straps. The axis of rotation for the dynamometer was aligned medial to the ASIS at the level of the greater trochanter on the test leg. The lever arm applied resistance to the lateral aspect of the distal thigh superior to the lateral femoral condyle. The participant was instructed to exert maximal effort against the dynamometer in the direction of hip abduction during the entire strength test. Concentric and eccentric torque of the hip abductors was tested from 0 to 20 degrees of hip abduction.
Figure 1.

Hip Abduction Strength Test.
Hip external rotation torque was assessed with the participant in a seated position with the hip and knee flexed to 90 degrees (Figure 2). The upper thigh of the test leg and trunk were stabilized with straps. A bolster was placed between the participant’s knees in order to control for hip adduction. The axis of rotation for the dynamometer was aligned with the knee joint line. Concentric and eccentric strength testing was performed through a range of 5° of hip internal rotation (neutral) to 20 degrees of hip external rotation, allowing for 25 degrees of total hip internal and external rotation range of motion to occur.
Figure 2.

Hip External Rotation Strength Test.
For the hip extension test, participants were positioned so that their trunk was flexed to 90 degrees and their arms were wrapped around the chair of the Biodex in order to stabilize their trunk (Figure 3). The axis of rotation for the dynamometer was aligned with the greater trochanter of the femur on the test leg. The lever arm applied resistance on the posterior thigh just superior to the knee. The non‐test leg supported the body of the participant. The participants were instructed to exert maximal effort against the dynamometer in the direction of hip extension keeping their knee flexed at approximately 90 degrees. The torque of the hip extensors was tested concentrically and eccentrically from 90 degrees of hip flexion to 60 degrees of hip flexion.
Figure 3.
Hip Extension Strength Test.
Data Reduction and Analysis
Three‐dimensional coordinates of the digitized bony landmarks were calculated using Motion Monitor® software (Innovative Sports Training, Inc., Chicago, IL). A global reference system was defined using the right hand rule, in which the x‐axis was positive in the anterior direction, the y‐axis was positive to the left of each participant, and the z‐axis was positive in the superior direction. Lower extremity joint kinematics were calculated using the Euler rotation method. The order of rotation used to calculate trunk, hip, and knee joint rotations was Y, X, Z. The y‐axis corresponds to the flexion‐extension axis, the x‐axis corresponds to the abduction‐adduction axis, and the z‐axis corresponds to the internal‐external rotation axis.
All kinematic data were filtered using a fourth‐order low‐pass Butterworth filter at 14.5 Hz. Kinematic and kinetic data were reduced using custom MATLAB software (MathWorks, Natick, Massachusetts). Frontal and transverse plane three‐dimensional peak knee and hip joint angles, and ipsilateral trunk flexion angles were determined during the stance phase of the jump‐landing task. The stance phase was defined as the period between initial ground contact with the force plate until takeoff for the rebound jump. Initial ground contact was the time when vertical ground‐reaction force exceeded 10 N as the subject landed on the force plate from a 30‐cm high platform. Takeoff was identified as the time when vertical ground reaction force dropped below 10 N following initial contact. Ipsilateral trunk flexion was defined relative to the world axis system while all hip and knee joint motions were defined relative to the proximal segment.
Peak data for the concentric and eccentric phases of the isokinetic strength testing was determined using custom Matlab software (Mathworks, Natick, MA). The concentric and eccentric phases were determined based on the direction of motion occurring. For example, during hip abduction, the concentric phase was the phase when the dynamometer arm moved from 0° to 20° of hip abduction and the eccentric phase was the phase when the dynamometer arm moved from 20° to 0° of hip abduction. All torque data (Nm) were normalized to body weight multiplied by height (%BW*H).28
Statistical Analysis
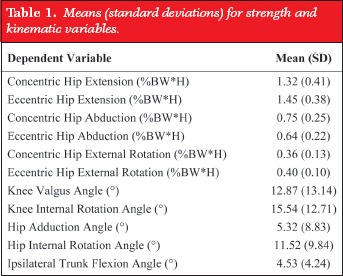
All data analyses were performed using SPSS version 16.0 (SPSS, Inc., Chicago, IL). Kinematic data (Table 1) were averaged over the three trials of the jump‐landing task for each subject. The average of the middle three trials for each strength test were used for data analysis to eliminate the possibility of learning (trial one) and fatigue effects (trial five). Prior to statistical analyses, all data were assessed for outliers (an outlier was defined as a value greater than three standard deviations beyond the mean). Relationships between each kinematic and strength variable were assessed using a series of simple correlational analyses. A priori alpha level was set at 0.05.
Table 1.
Means (standard deviations) for strength and kinematic variables.
 |
RESULTS
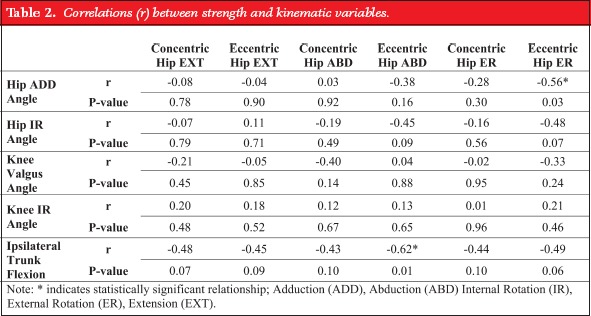
Descriptive statistics (means and standard deviations) for all kinematic and strength variables are presented in Table 1. No outliers were found and therefore all data points were included in the data set used for statistical analyses. Subjects, on average, reported their worst pain during the previous week as 5 cm on a 10 cm VAS and their current level of function as 72 out of 100 on the AKPS (higher score indicates better perceived function). Peak hip adduction angle during the stance phase of the jump‐landing task was moderately correlated with peak eccentric hip external rotation torque (r=‐0.56, P=0.03) (Figure 4). Peak ipsilateral trunk flexion during the stance phase of the jump‐landing task was moderately correlated with peak eccentric hip abduction torque (r=‐0.62, P=0.01) (Figure 5). These negative correlations indicate that decreased eccentric torque of the hip musculature is associated with increased frontal plane hip adduction and lateral trunk flexion to the same side (ipsilateral). Simple correlation analyses did not reveal additional significant relationships between the other kinematic and strength variables (Table 2).
Figure 4.
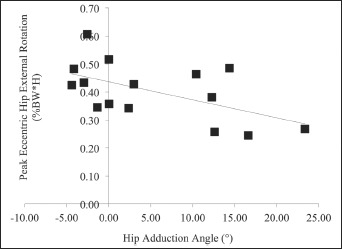
Hip Adduction Angle vs. Peak Eccentric Hip External Rotation Torque.
Figure 5.
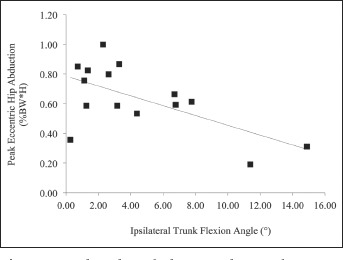
Ipsilateral Trunk Flexion Angle vs. Peak Eccentric Hip Abduction Torque.
Table 2.
Correlations (r) between strength and kinematic variables.
 |
DISCUSSION
The purpose of this study was to determine the relationship between isokinetic strength of the hip musculature and frontal and transverse plane motion of the hip and knee and ipsilateral trunk flexion in patients with PFP. The hypotheses of this study were not fully supported based on the results from this investigation; however, decreased eccentric strength of the hip external rotators and abductors was significantly correlated to increased frontal plane motion at the hip and trunk in individuals with PFP. Previous research has consistently reported a decrease in strength of the hip musculature in individuals with PFP;9–15 however there is a lack of research investigating how this decreased strength may relate to faulty lower extremity and trunk kinematics, however, there is a lack of research investigating how decreased strength may relate to faulty lower extremity and trunk kinematics. While most investigations have evaluated isometric strength of the hip musculature in individuals with PFP, this study is novel in that concentric and eccentric torque of the hip musculature is correlated with trunk and lower extremity kinematics.
Based on the results of the current study, a decrease in the eccentric torque producing capabilities of the hip abductors is related to an increase in frontal plane motion of the trunk towards the affected or most affected side of pain. Although patients with PFP may use this increased frontal plane motion at the trunk as a compensation for decreased strength of the hip abductors, this may be leading to additional faulty compensations down the kinetic chain. For example, an individual who laterally flexes the trunk on a fixed lower extremity will likely have an increase in the valgus moment at the knee.6 The potential for an increase in knee valgus and in turn an increase in patellofemoral joint stress due to increased frontal plane trunk motion, warrants the use of strengthening exercises for the hip musculature in individuals with PFP who display increased frontal plane motion at the hip and trunk.
In addition to the relationship between hip muscle strength and frontal plane motion at the trunk, there was also a significant relationship between hip muscle strength and frontal plane motion at the hip. Decreased eccentric strength of the hip external rotators was significantly correlated to increased hip adduction during the jump‐landing task. Although we would expect the hip abductors to play a larger role in controlling hip adduction motion, we only found a relationship between strength of the hip external rotators and hip adduction motion. This may best be explained by understanding the muscles that could have contributed to the hip external rotation torque production during the isokinetic test. The posterior fibers of the gluteus maximus have been reported to act as hip external rotators from 0 to 90 degrees of flexion along with the posterior fibers of the gluteus medius.29 The gluteus medius and maximus also play a role in frontal plane stability of the pelvis.6 Based on the actions of the gluteus medius and maximus, a decrease in eccentric strength of these muscles may be driving the negative relationship between hip external rotation strength and hip adduction angle during the jump‐landing task.
Two previous studies have investigated the relationship between hip muscle strength and lower extremity kinematics in individuals with PFP.22,23 The first study correlated hip external rotation and abduction strength to lower extremity kinematics prior to and following a prolonged run in individuals with PFP.22 The investigators reported a significant negative relationship between hip abduction strength and hip adduction angle following a prolonged run but not prior to the prolonged run.22 In a subsequent study, Willson and Davis23 reported no significant relationships between hip abduction or external rotation strength and frontal or transverse motion at the hip during a single leg landing task. Based on the conflicting results of the two previous investigations along with the results from our investigation, additional research is warranted to better understand if a relationship exists between strength of the hip musculature and kinematics of the trunk and lower extremity in individuals with PFP.
One methodological difference that should be considered when comparing this investigation to previous investigations is that strength of the hip musculature was assessed isokinetically during concentric and eccentric contractions. Much of the previous literature investigating the relationship between lower extremity kinematics and hip muscle strength in either a patient or healthy population has utilized isometric strength assessments of the hip musculature. Isokinetic strength during concentric and eccentric contractions was investigated in this study because during dynamic tasks, muscles are contracting concentrically and eccentrically; therefore, measures of strength during concentric and eccentric contractions may be more clinically meaningful than measures of isometric strength. Future studies should investigate which strength measures explain more of the variance in lower extremity kinematics during dynamic tasks.
The authors of this study acknowledge that there are limitations to this investigation. One limitation to this investigation is the lack of a control group. A control group was not utilized in this investigation due to previous literature already providing support for strength and kinematic differences between healthy individuals and those with PFP.9–15,22,23 Another limitation is the unequal numbers of males and females and low number of subjects who participated in this investigation. To ensure the correlational analyses were not influenced by gender, separate one‐way analyses of variance were performed to determine if there were significant differences between males and females for all variables of interest. There were no gender differences (P>0.05), which may be driven by the low subject numbers; however, due to the lack of gender differences, the correlational analyses were performed without regard to gender. Also, due to the moderate r‐values reported for our significant findings, the results do not appear to be influenced by the low subject number. However, the lack of significant findings for the additional kinematic and hip muscle strength variables may be attributed to the low subject number. For example, the results for ipsilateral trunk flexion may be viewed as clinically meaningful, although not statistically significant, as all r‐values show a negative relationship and range from 0.43–0.49. A final limitation of this investigation was the range of motion limits and positioning utilized for assessing strength of the hip musculature. As previously stated, the rationale for assessing concentric and eccentric contractions was to replicate how the muscles contract during functional tasks, however, it should be noted that our testing procedures did not exactly replicate the range of motion and joint positions that occurred during the jump‐landing task. The range of motions used during strength testing was decided upon based on the level of comfort of the participant during pilot testing. Although there may be limits in the ability to generalize these results to functional tasks due to the small range of motion used to assess strength, the authors feel that the internal validity of the results is high due to all subjects performing the tests through the same arcs of motion. Future investigations should determine if set ranges of motion during strength testing influences the relationship between strength and lower extremity kinematics.
CONCLUSION
The findings of this investigation support an association between eccentric strength of the hip musculature and frontal plane motion at the trunk and hip. Based on these results and the results from prior studies reporting alterations in lower extremity strength and kinematics in individuals with PFP, it is important for clinicians to evaluate strength of the hip musculature along with lower extremity mechanics during dynamic tasks in indviduals with PFP.9–15,22,23 It is also important to note the r‐values for significant correlations were moderate in this study. Thus, future research should investigate additional biomechanical variables, such as neuromuscular control, in order to better understand the multiple factors that influence faulty mechanics in individuals with PFP. Gaining a clear understanding of all biomechanical factors influencing lower extremity mechanics during dynamic tasks will aid clinicians in developing more effective intervention programs for individuals with PFP.
REFERENCES
- 1. Devereaux M, Lachman S. Patellofemoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18:18–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DeHaven KE, Lintner DM. Athletic injuries: Comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224 [DOI] [PubMed] [Google Scholar]
- 3. Milgrom C, Kerem E, Finestone A, Eldad A, Shlamkovitch N. Patellofemoral pain caused by overactivity. A prospective study of risk factors in infantry recruits. J Bone Joint Surg. 1991;73A 1041–1043 [PubMed] [Google Scholar]
- 4. Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: A two‐year prospective study. Am J Sports Med. 2000;28(4):480–489 [DOI] [PubMed] [Google Scholar]
- 5. Powers CM. The influence of altered lower‐extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646 [DOI] [PubMed] [Google Scholar]
- 6. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51 [DOI] [PubMed] [Google Scholar]
- 7. Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of Q angle and tendofemoral contact. J Bone Joint Surg. 1984;66A (5):715–724 [PubMed] [Google Scholar]
- 8. Lee T, Morris G, Csintalan R. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693 [DOI] [PubMed] [Google Scholar]
- 9. Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12–18 [DOI] [PubMed] [Google Scholar]
- 10. Boling MC, Padua DA, Alexander CR. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. J Athl Train. 2009;44(1):7–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33 (11):671–676 [DOI] [PubMed] [Google Scholar]
- 12. Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801 [DOI] [PubMed] [Google Scholar]
- 13. Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–238 [DOI] [PubMed] [Google Scholar]
- 14. Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19 [DOI] [PubMed] [Google Scholar]
- 15. Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. Aug 2007;39(8):1227–1232 [DOI] [PubMed] [Google Scholar]
- 16. Jacobs CA, Uhl TL, Mattacola CG, Shapiro R, Rayens WS. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train. Jan‐Mar 2007;42(1):76–83 [PMC free article] [PubMed] [Google Scholar]
- 17. Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. May 2006;38(5):945–952 [DOI] [PubMed] [Google Scholar]
- 18. Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41–50 [DOI] [PubMed] [Google Scholar]
- 19. Hollman JH, Ginos BE, Kozuchowski J, Vaughn AS, Krause DA, Youdas JW. Relationships between knee valgus, hip‐muscle strength, and hip‐muscle recruitment during a single‐limb step‐down. J Sport Rehabil. Feb 2009;18(1):104–117 [DOI] [PubMed] [Google Scholar]
- 20. Lawrence RK 3rd, Kernozek TW, Miller EJ, Torry MR, Reuteman P. Influences of hip external rotation strength on knee mechanics during single‐leg drop landings in females. Clin Biomech (Bristol, Avon). Jul 2008;23(6):806–813 [DOI] [PubMed] [Google Scholar]
- 21. Baldon RD, Lobato DFM, Carvalho LP, Santiago PRP, Benze BG, Serrao FV. Relationship Between Eccentric Hip Torque and Lower‐Limb Kinematics: Gender Differences. J Appl Biomech. Aug 2011;27(3):223–232 [DOI] [PubMed] [Google Scholar]
- 22. Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38(8):448–456 [DOI] [PubMed] [Google Scholar]
- 23. Willson JD, Davis IS. Lower extremity strength and mechanics during jumping in women with patellofemoral pain. J Sport Rehabil. Feb 2009;18(1):76–90 [DOI] [PubMed] [Google Scholar]
- 24. Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ. Changing sidestep cutting technique reduces knee valgus loading. Am J Sports Med. Nov 2009;37(11):2194–2200 [DOI] [PubMed] [Google Scholar]
- 25. Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. J Arthroscopic Rel Surg. 1993;9 (2):159–163 [DOI] [PubMed] [Google Scholar]
- 26. Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid. Arch Phys Med Rehab. 2004;85 815–822 [DOI] [PubMed] [Google Scholar]
- 27. Hawkey TJ, Halverson SD, Padua DA, Guskiewicz KM. Reliability of three different strength testing protocols for hip abduction, extension, and external rotation strength. J Athl Train. 2004;39 (2):S116 [Google Scholar]
- 28. Bazett‐Jones DM, Cobb SC, Joshi MN, Cashin SE, Earl JE. Normalizing hip muscle strength: establishing body‐size‐independent measurements. Arch Phys Med Rehabil. Jan 2011;92(1):76–82 [DOI] [PubMed] [Google Scholar]
- 29. Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther. 2010;40(2):82–94 [DOI] [PubMed] [Google Scholar]


