Abstract
We report here the cases of two females with Graves' disease who developed insulin autoimmune syndrome after treatment with methimazole. The patients exhibited a sudden altered mental state after treatment with methimazole for approximately 4 weeks. Patients had hypoglycemia with serum glucose below 70 mg/dL, and laboratory findings showed both high levels of serum insulin and high titers of insulin autoantibodies. The two women had never been exposed to insulin or oral antidiabetic agents, and there was no evidence of insulinoma in imaging studies. After glucose loading, serum glucose, and total insulin levels increased abnormally. One of the patient was found to have HLA-DRB1*0406, which is known to be strongly associated with methimazole-induced insulin autoimmune syndrome. After discontinuation of methimazole, hypoglycemic events disappeared within 1 month. Insulin autoantibody titer and insulin levels decreased within 5 months and there was no further development of hypoglycemic events. We present these cases with a review of the relevant literature.
Keywords: Graves disease, Insulin autoimmune syndrome, Methimazole
INTRODUCTION
Insulin autoimmune syndrome, also known as Hirata disease, is a relatively rare condition characterized by fasting hypoglycemia, high serum insulin concentrations, and presence of insulin autoantibodies in individuals who have not been previously injected with insulin. The mechanism of spontaneous hypoglycemia in insulin autoimmune syndrome is due to excess free insulin released from insulin autoantibody complexes several hours after a glucose load. Hirata et al. [1] first described spontaneous hypoglycemia with insulin autoimmunity in 1970, suggesting that the association of insulin autoimmune syndrome and Graves' disease in 1974 [2]. Over 50% of patients who are diagnosed with insulin autoimmune syndrome have previously received drugs containing a sulfhydryl group, which has been proposed to be related to the production of insulin autoantibodies by chemical and immunological reactions with insulin molecules [3]. Patients with Graves' disease who have been treated with methimazole, which also contains a sulfhydryl group, are predisposed to development of insulin autoimmune syndrome [4].
Almost all cases of methimazole-induced insulin autoimmune syndrome are reported in East Asia, especially in Japan [5]. In general, insulin autoimmune syndrome exhibits a strong genetic predisposition. Specifically, it has been reported that insulin autoimmune syndrome is strongly associated with HLA-DRB1*0406, DQB1*0302, and DQA1*0301 [6]. Among the three genetic variants of HLA-DRB1 (DRB1*0403, DRB1*0406, and DRB1*0407), only DRB1*0406 is exclusively associated with an elevated risk of developing insulin autoimmune syndrome [7]. The DRB1*0406 genotype is relatively common in East Asians, which explains why insulin autoimmune syndrome is most common in East Asians [7]. In the case of methimazole-induced insulin autoimmune syndrome, it is also known that a specific allelic combination of Bw62/Cw4/DR4 (including DRB1*0406) is a major genetic risk factor [8]. Although there have been three previously reported cases of methimazole-induced insulin autoimmune syndrome in Koreans [9-11], none examined the role of genetic predisposition. Herein, we report two cases of methimazole-induced insulin autoimmune syndrome, including a case where HLA genotyping revealed HLA-DRB1*0406.
CASE REPORTS
Case 1
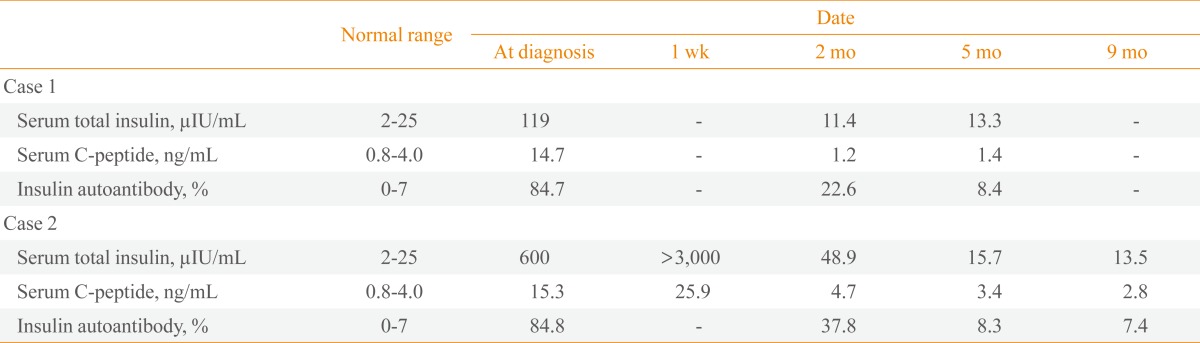
A 52-year-old woman presented at our hospital with heat intolerance, palpitation, and chest discomfort persisting for 2 months. Physical examination revealed thyroid gland enlargement but no exophthalmos. Thyroid function test indicated hyperthyroidism with thyroid stimulating hormone (TSH) <0.05 µIU/mL (normal range, 0.4 to 4.1), free thyroxine (free T4) 5.71 ng/dL (normal range, 0.70 to 1.80), and triiodothyronine (T3) 375 ng/dL (normal range, 87 to 184). The level of thyroid stimulating immunoglobulin was 60.8% (normal range, 0 to 15). A thyroid scan demonstrated an increase of 20-minute thyroid uptake of 99mTc. A diagnosis of Graves' disease was made and the patient was started on methimazole 30 mg/day. Four weeks after beginning methimazole treatment, she suffered general weakness and sweating that disappeared with food intake. The patient visited the emergency room because of confusion, irritability, and inappropriate verbal responses. She had no history of diabetes mellitus or exposure to insulin or oral antidiabetic agents. The patient's younger brother had a medical history of hyperthyroidism; however, there was no family history of diabetes mellitus. The patient's initial serum glucose level was 34 mg/dL. Laboratory studies including complete blood cell count with differential, chemistry profile, and electrolytes were all within normal limits. Thyroid function study revealed TSH <0.05 µIU/mL, free T4 0.77 ng/dL, and T3 146 ng/dL. Hemoglobin A1c (HbA1c) was 5.8%. The total serum insulin concentration was 119 µIU/mL (normal range, 2 to 25) and serum C-peptide was 14.7 ng/mL (normal range, 0.8 to 4.0). Insulin autoantibody was measured by radioimmunoassay at 84.7% (normal range, 0 to 7). Percent 125I-insulin binding was not measured. A computed tomography (CT) scan revealed a small cyst of the pancreas tail, which had no contrast enhancement. There was no evidence of insulinoma or extrapancreatic neoplasm. The result of 75-g oral glucose tolerance test showed an abnormal increase of total serum insulin levels with delayed hypoglycemia developing after 240 minutes with symptoms of sweating and dizziness (Table 1). A diagnosis of methimazole-induced insulin autoimmune syndrome was made based on the high serum concentration of total insulin, fasting hypoglycemia, and the presence of insulin autoantibodies. Methimazole was discontinued, and consumption of six or more small meals throughout the day with low carbohydrate was recommended. Hypoglycemic attacks subsided within 1 week and there were no further hypoglycemic episodes after discharge. Total serum insulin, titer of insulin autoantibody, and level of serum C-peptide decreased gradually after 5 months (Table 2). Treatment with 131I 20 mCi was performed to address Graves' disease in the patient.
Table 1.
Results of a 75-g Oral Glucose Tolerance Test in the Two Patients
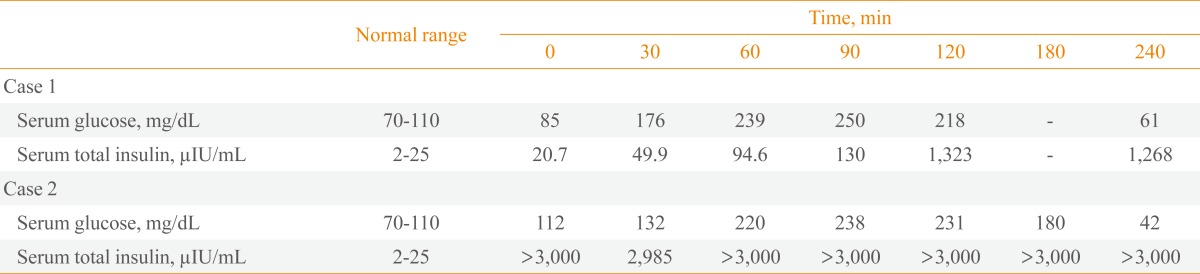
Table 2.
Serum Total Insulin, Serum C-Peptide, and Insulin Autoantibody of the Two Patients
Case 2
A 53-year-old woman visited the emergency room of our hospital complaining of headache, palpitation, and chest discomfort. She was diagnosed with Graves' disease at a different hospital 1 month prior to being admitted at our hospital and had been taking both methimazole 40 mg/day and β-blocker since her diagnosis. Prior to visiting our emergency room, she consumed breakfast and was measured with a serum glucose level of 294 mg/dL. Laboratory studies including complete blood cell count with differential, chemistry profile, and electrolytes were all within normal limits. The result of thyroid function tests were TSH <0.01 µIU/mL, free T4 2.74 ng/dL, and T3 184.8 ng/dL. The patient's symptoms were initially attributed to hyperthyroidism due to the lack of abnormal findings on neurologic exam and brain magnetic resonance imaging. However, 6 hours after discharge, the patient revisited our emergency room due to sweating and altered mental state, where it was noted that she had neither a history of diabetes mellitus nor previous exposure to insulin or oral antidiabetic agents. Furthermore, there was no family history of thyroid disease and diabetes mellitus. The patient's initial serum glucose level was 27 mg/dL, HbA1c was 5.8%, serum total insulin was 600 µIU/mL, and serum C-peptide was 15.3 ng/mL. The titer of insulin autoantibody was 84.8%, while detection of both insulin receptor antibody and islet cell antibody were negative. The percent of 125I-insulin binding was not measured. The titers of serum thyroid autoantibodies were high. Specifically, antithyroid peroxidase antibody was 2,876 U/mL (normal range, 0 to 100), antithyroglobulin antibody was 330 IU/mL (normal range, 0 to 115), and TSH receptor antibody was 2.95 IU/L (normal range, <1.22). A CT scan revealed no evidence of insulinoma or extrapancreatic neoplasm. The patient's fasting insulin level was more than 3,000 µIU/mL and C-peptide was 25.9 ng/mL on hospital day 7. A 75-g oral glucose tolerance test showed marked increase of total insulin level and subsequent hypoglycemia developed after 240 minutes (Table 1). HLA genotyping was performed by sequence based typing and the result was HLA-DRB1*0406 and *1501. Continuous intravenous glucose injection was needed due to recurrent fasting hypoglycemia. Methimazole-induced insulin autoimmune syndrome was diagnosed, and methimazole was subsequently discontinued. Hypoglycemic episodes disappeared after 1 month, with the patient consuming small frequent meals and a low carbohydrate diet. The concentration of serum total insulin, titer of insulin autoantibody, and serum C-peptide level decreased gradually after 5 months (Table 2). Radioactive iodine therapy with 131I 15 mCi was performed to address Graves' disease in the patient.
DISCUSSION
The main causes of hypoglycemia combined with hyperinsulinemia are insulinoma, inappropriate use of antidiabetic agents, and autoimmune hypoglycemia. Hirata et al. [1] first described the possibility of spontaneous production of insulin antibodies after observing a case of hypoglycemia associated with insulin-binding antibodies in a patient with no history of exposure to exogenous insulin. The prevalence of insulin autoimmune syndrome is particularly high in Japan. As of 2007, there have been 330 reported cases of insulin autoimmune syndrome in Japan, 20 of which were attributed to East Asians excluding Japanese individuals, and 47 cases in Caucasians [5]. Approximately 80% of insulin autoimmune syndromes are capable of coexisting with other autoimmune diseases, namely, 25% of patients with Graves' disease as well as others with systemic lupus erythematosus, rheumatoid arthritis, and chronic hepatitis, etc.
Graves' disease per se is not a risk factor for insulin autoimmune syndrome. Takei [12] compared the prevalence of insulin autoantibodies in patients with Graves' disease treated with methimazole (n=206) or propylthiouracil (n=118) as well as patients with untreated hyperthyroidism (n=160), identifying 13 cases (6.3%) with insulin autoantibodies only among patients treated with methimazole. The molecular mechanism of methimazole induced insulin autoimmune syndrome is thought to be related to the sulfhydryl group of methimazole. Specifically, the disulfide bond of insulin molecules can be cleaved via the reducing power of the sulfhydryl group present in methimazole. Further, insulin-derived peptides produced via disruption of the native structure of insulin continue to be recognized by antigens presenting cells as self-antigens, resulting in stimulation of T cell mediated immunity [3]. Indeed, up to one half of patients with insulin autoimmune syndrome presented with a history of using drugs containing a sulfhydryl group, which include methimazole, α-mercaptopropionyl glycine, and glutathione within the previous year [13]. More recently, cases of insulin autoimmune syndrome caused by α-lipoic acid have been increasing, which has been attributed to the two sulfur atoms connected by a disulfide bond of α-lipoic acid, which generates a strong reducing power [14]. Based on these observations, insulin autoimmune syndrome is attributed to either methimazole or carbimazole, which is converted to methimazole in the body, in patients with Graves' disease.
The prevalence of methimazole-induced autoimmune syndrome is high in Japan. Indeed, there have been 64 reported cases of methimazole-induced insulin autoimmune syndrome in Japan as well as 16 cases in East Asians (excluding Japanese) and two cases in Caucasians; only three of these cases were reported in Korea. We experienced two cases of insulin autoimmune syndrome in female patients with Graves' disease who presented with an altered mental state due to fasting hypoglycemia after 4-week treatment with methimazole. The two patients had hyperinsulinemia and insulin autoantibodies without previous insulin administration or evidence of insulinoma.
To the best of our knowledge, this is the first report in Korea to identify HLA-DRB1*0406 in a case of methimazole-induced autoimmune syndrome. HLA genotypes are considered to have strong association with insulin autoimmune syndrome in Japan. Polyclonal insulin antibodies, which are observed in most cases of insulin autoimmune syndrome, were strongly associated with HLA-DRB1*0406, DQB1*0302, and DQA1*0301 [6]. These are frequent HLA alleles in Japanese and are considered to be related with a higher prevalence of insulin autoimmune syndrome compared with the general population [7]. The relationship of specific HLA genes with methimazole-induced autoimmune syndrome has only been described in Japan. Thus, patients with Graves' disease are thought to develop insulin autoimmune syndrome when they have a specific HLA allelic combination of Bw62/Cw4/DR4 including DRB1*0406 [8]. Likewise, it has been suggested that the HLA class II beta chain, which is encoded by HLA-DRB1 gene, binds with insulin-derived peptides and is cleaved by reducing compounds such as methimazole, resulting in insulin-specific proliferation of T cells [15]. Indeed, the majority of frequent HLA-DR alleles in Koreans, in decreasing order of frequency, are DR4, DR15, DR13, and DR8 [16] with HLA-DRB1*0803 and *1602 alleles conferring susceptibility to Graves' disease in Koreans [17]. Because the frequency of HLA-DRB1*0406 was 9.1% in Korean patients with Graves' disease [17], Koreans might have a high risk of methimazole-induced autoimmune syndrome, a topic that warrants further case studies and clinical evaluation.
The mechanism of hyperinsulinemia in insulin autoimmune syndrome is a relative insulin deficit caused by binding of insulin autoantibodies to insulin released from β-cells, resulting in inappropriate insulin secretion and delayed clearance [3]. Spontaneous hypoglycemia in insulin autoimmune syndrome is caused by an excess of free insulin released from insulin autoantibody complexes, irrespective of serum glucose concentration [3]. Indeed, hypoglycemia can occur at both fasting and postprandial states but there is a tendency of reactive hypoglycemia after several hours of food intake [18]. Hyperglycemia is also frequent right after meal because insulin released from β-cells binds to insulin autoantibodies and blood glucose cannot be utilized properly. The two patients in this report showed rather lower glucose level before a glucose load and rapid increase in glucose level of more than 200 mg/dL after 1 or 2 hours of 75-g oral glucose challenge. The elevated level of serum glucose decreased rapidly and hypoglycemia occurred after 3 or 4 hours of glucose load.
Approximately 80% of patients with insulin autoimmune syndrome had spontaneous remission of hypoglycemia after less than 3 months with no special treatment except avoiding drug exposure, although persistent hypoglycemia also has been observed in a few patients [13]. Discontinuation of the offending drug, consumption of six or more small meals per day and a low carbohydrate diet is the currently recommended treatment for methimazole-induced hypoglycemia [5]. For hypoglycemia, α-glucosidase inhibitors can be helpful by decreasing glucose uptake in the intestines and preventing over-secretion of insulin by β-cells. If hypoglycemia persists, both immunosuppressive therapy with prednisolone 30 to 60 mg/day and azathioprine or 6-mercaptopurine with plasmapheresis should be considered [19]. Further, rituximab, an anti-CD20 monoclonal antibody, has been shown to be remarkably effective in blocking de novo antibody responses and is known to suppress insulin autoantibodies [20]. Thus, this approach may be helpful by decreasing insulin autoantibodies in persistent hypoglycemia in methimazole-induced insulin autoimmune syndrome. In our two cases, hypoglycemic episodes subsided within 1 month after discontinuation of methimazole and the titers of serum total insulin, C-peptide, and insulin autoantibodies normalized gradually within 5 months.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Hirata Y, Ishizu H, Ouchi N, Motomura S, Abe M, Hara Y, Wakasugi H, Takahashi I, Sakano H, Tanaka M. Insulin autoimmunity in a case with spontaneous hypoglycemia. J Jpn Diabetes Soc. 1970;13:312–320. [Google Scholar]
- 2.Hirata Y, Tominaga M, Ito JI, Noguchi A. Spontaneous hypoglycemia with insulin autoimmunity in Graves' disease. Ann Intern Med. 1974;81:214–218. doi: 10.7326/0003-4819-81-2-214. [DOI] [PubMed] [Google Scholar]
- 3.Ichihara K, Shima K, Saito Y, Nonaka K, Tarui S. Mechanism of hypoglycemia observed in a patient with insulin autoimmune syndrome. Diabetes. 1977;26:500–506. doi: 10.2337/diab.26.5.500. [DOI] [PubMed] [Google Scholar]
- 4.Hirata Y. Methimazole and insulin autoimmune syndrome with hypoglycemia. Lancet. 1983;2:1037–1038. doi: 10.1016/s0140-6736(83)91031-0. [DOI] [PubMed] [Google Scholar]
- 5.Eisenbarth GS. Immunoendocrinology: scientific and clinical aspects. Totowa: Springer Science+Business Media; 2011. Chapter 21. Insulin autoimmune syndrome (Hirata disease) pp. 343–367. [Google Scholar]
- 6.Uchigata Y, Kuwata S, Tokunaga K, Eguchi Y, Takayama-Hasumi S, Miyamoto M, Omori Y, Juji T, Hirata Y. Strong association of insulin autoimmune syndrome with HLA-DR4. Lancet. 1992;339:393–394. doi: 10.1016/0140-6736(92)90080-m. [DOI] [PubMed] [Google Scholar]
- 7.Uchigata Y, Hirata Y, Omori Y, Iwamoto Y, Tokunaga K. Worldwide differences in the incidence of insulin autoimmune syndrome (Hirata disease) with respect to the evolution of HLA-DR4 alleles. Hum Immunol. 2000;61:154–157. doi: 10.1016/s0198-8859(99)00144-5. [DOI] [PubMed] [Google Scholar]
- 8.Uchigata Y, Kuwata S, Tsushima T, Tokunaga K, Miyamoto M, Tsuchikawa K, Hirata Y, Juji T, Omori Y. Patients with Graves' disease who developed insulin autoimmune syndrome (Hirata disease) possess HLA-Bw62/Cw4/DR4 carrying DRB1*0406. J Clin Endocrinol Metab. 1993;77:249–254. doi: 10.1210/jcem.77.1.8325948. [DOI] [PubMed] [Google Scholar]
- 9.Cho BY, Lee HK, Koh CS, Min HK. Spontaneous hypoglycemia and insulin autoantibodies in a patient with Graves' disease. Diabetes Res Clin Pract. 1987;3:119–124. doi: 10.1016/s0168-8227(87)80017-7. [DOI] [PubMed] [Google Scholar]
- 10.Lee KS, Kim JH, Choi WH, Kim TW, Kim MH. A case report of insulin autoimmune syndrome in Graves' disease. J Korean Soc Endocrinol. 1993;8:451–455. [Google Scholar]
- 11.Lim JK, Woo YA, Kang SJ, Yoo SS, Hong KY, Kim SH. Ensulin autoimmune syndrome in a patient with methimazole-treated Graves' disease: a case report. J Korean Soc Endocrinol. 1998;13:612–616. [Google Scholar]
- 12.Takei M. Insulin autoantibodies produced by methimazole treatment in patients with Graves' disease. J Tokyo Women Med Coll. 1980;50:54–68. [Google Scholar]
- 13.Uchigata Y, Eguchi Y, Takayama-Hasumi S, Omori Y. Insulin autoimmune syndrome (Hirata disease): clinical features and epidemiology in Japan. Diabetes Res Clin Pract. 1994;22:89–94. doi: 10.1016/0168-8227(94)90040-x. [DOI] [PubMed] [Google Scholar]
- 14.Takeuchi Y, Miyamoto T, Kakizawa T, Shigematsu S, Hashizume K. Insulin autoimmune syndrome possibly caused by alpha lipoic acid. Intern Med. 2007;46:237–239. doi: 10.2169/internalmedicine.46.1893. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Nieda M, Uchigata Y, Nishimura M, Tokunaga K, Kuwata S, Obata F, Tadokoro K, Hirata Y, Omori Y, et al. Recognition of human insulin in the context of HLA-DRB1* 0406 products by T cells of insulin autoimmune syndrome patients and healthy donors. J Immunol. 1993;151:5770–5776. [PubMed] [Google Scholar]
- 16.Roh EY, Kim HS, Kim SM, Lim YM, Han BY, Park MH. HLA-A, -B, -DR allele frequencies and haplotypic associations in Koreans defined by generic-level DNA typing. Korean J Lab Med. 2003;23:420–430. [Google Scholar]
- 17.Park MH, Park YJ, Song EY, Park H, Kim TY, Park DJ, Park KS, Cho BY. Association of HLA-DR and -DQ genes with Graves disease in Koreans. Hum Immunol. 2005;66:741–747. doi: 10.1016/j.humimm.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Eguchi Y, Uchigata Y, Yao K, Yokoyama H, Hirata Y, Omori Y. Longitudinal changes of serum insulin concentration and insulin antibody features in persistent insulin autoimmune syndrome (Hirata's disease) Autoimmunity. 1994;19:279–284. doi: 10.3109/08916939409071354. [DOI] [PubMed] [Google Scholar]
- 19.Yaturu S, DePrisco C, Lurie A. Severe autoimmune hypoglycemia with insulin antibodies necessitating plasmapheresis. Endocr Pract. 2004;10:49–54. doi: 10.4158/EP.10.1.49. [DOI] [PubMed] [Google Scholar]
- 20.Yu L, Herold K, Krause-Steinrauf H, McGee PL, Bundy B, Pugliese A, Krischer J, Eisenbarth GS Type 1 Diabetes TrialNet Anti-CD20 Study Group. Rituximab selectively suppresses specific islet antibodies. Diabetes. 2011;60:2560–2565. doi: 10.2337/db11-0674. [DOI] [PMC free article] [PubMed] [Google Scholar]


