Abstract
Study objective
We examined variability among emergency department (ED) physicians in rate of hospitalization for patients with pneumonia, and the effect of variability on clinical outcomes.
Methods
We studied 2,069 LDS Hospital ED patients with community-acquired pneumonia ≥18 years old during the years 1996-2006, identified by ICD-9 coding and compatible chest radiographs. We extracted vital signs, laboratory and radiographic results, hospitalization, and outcomes from the electronic medical record. We defined “low severity” as PaO2/FiO2 ratio ≥280 mm Hg, predicted mortality <5% by an electronic version of CURB-65 that utilizes continuous and weighted elements (eCURB), and <3 IDSA-ATS 2007 severe pneumonia minor criteria. We adjusted hospitalization decisions and outcomes for illness severity and patient demographics.
Results
Initial hospitalization rate was 58%; 10.7% of patients initially treated as outpatients were secondarily hospitalized within 7 days. Median age of admitted patients was 63 years; median eCURB predicted mortality was 2.65% (mean 6.8%), versus 46 and 0.93% for outpatients. The 18 ED physicians (average age 44.9 (7.6) years, years in practice 8.4 (6.9)) objectively calculated and documented illness severity in 2.7% of patients. Observed 30-day mortality for inpatients was 6.8% (outpatients 0.34%) and decreased over time. Individual physician admission rates ranged from 38% to 79%; variability not explained by illness severity, time of day, day of week, resident care in conjunction with an attending, or patient or physician demographics. Higher hospitalization rates were not associated with reduced mortality or fewer secondary hospital admissions.
Conclusions
We observed a twofold difference in pneumonia hospitalization rates among ED physicians, unexplained by objective data.
Introduction
Background and Importance
Community-acquired pneumonia combined with influenza is the 8th leading cause of death in the United States. (1) About 6 million cases yearly lead to an estimated 500,000 hospitalizations. (2) Treatment costs are 8.4-10 billion dollars annually in the United States, with the cost of inpatient care 25 times that of outpatient care. (3) The selection of inpatient versus outpatient care is a major decision in the management of pneumonia and is guided by estimated severity of the patient's disease and need for specific treatments. (4) Less ill patients are more satisfied with their care and return to usual activities faster if treated at home. (5,6) Eighty percent of low risk patients prefer outpatient therapy. (7) On the other hand, patients hospitalized after failed outpatient treatment have higher mortality. (8) Variability in rate of hospitalization for pneumonia has been demonstrated between hospitals, but no physician level data are available. (9,10)
The LDS Hospital Emergency Department (ED) in Salt Lake City, Utah, adopted an electronic medical record (EMR) in 1995, providing the opportunity to study care delivery using detailed patient data over an extended period. During the same year, the ED implemented a paper-based pneumonia guideline that provided an objective severity assessment system based on risk factors identified in the 1993 American Thoracic Society pneumonia guideline. (11,12) The guideline's severity assessment was changed to CURB-65 after development and international validation of the CURB-65 severity scoring system in 2003. (13) The pneumonia guideline was effective in standardizing antibiotic prescribing practices and the ordering of microbiologic studies (14).
Goals of this study
In this observational study, we identified patient characteristics associated with the decision for inpatient versus outpatient care in patients with pneumonia. We hypothesized that individual ED physicians would vary in their determination of which patients to hospitalize, after adjusting for severity of illness. We also evaluated whether hospitalization rates by individual ED physician might affect mortality or secondary hospital admissions..
Setting
The study was performed at LDS Hospital, a tertiary care, university-affiliated teaching hospital, with 520 total and 68 intensive care unit beds in Salt Lake City, Utah, USA. The ED has 24 beds, including six beds that also serve as an “observation” unit. The observation unit was not used for treatment of pneumonia patients, but for overflow and brief treatment of patients with minor intoxications or volume depletion. Internal medicine and emergency medicine residents participated in the care of ED patients, although they did not independently dictate reports until July, 2005. Mean time from ED admission to antibiotic administration for pneumonia patients was 195 minutes, median 145 minutes.
Study Design and Patient Selection
We have detailed our community-acquired pneumonia case-finding strategy previously. (15) Briefly, using a previously validated algorithm (16), we retrospectively identified all patients admitted to the LDS Hospital ED from 1996 through 2006 with International Classification of Diseases (ICD-9) codes compatible with a primary discharge diagnosis of pneumonia (480-487.1) or respiratory failure or sepsis (518.×, 038.×) with secondary diagnosis of pneumonia. Data collection began Jan 1, 1996, once the electronic medical record implemented the prior year had evolved into a stable process. We completed observation of patients at the end of 2006 because the following year, the LDS Hospital ED downsized and changed markedly with the transfer of teaching and tertiary care services to Intermountain Medical Center in Murray, Utah. An admission chest radiograph compatible with pneumonia was required for inclusion, as determined by review of radiology reports. We excluded patients residing in a skilled nursing facility, patients discharged from a hospital within 90 days, and patients receiving chronic hemodialysis as representing health care associated pneumonia. (17) We also excluded patients with significant immune suppression, and patients who expired in the ED.
Data Collection and Processing
We extracted from the EMR data elements necessary for measuring severity of illness by eCURB, an electronic version of CURB-65 utilizing continuous and weighted elements to improve correlation with 30-day all-cause mortality (15) and by the Infectious Disease Society of America/American Thoracic Society 2007 severe pneumonia minor criteria (2007 sCAP, table 1). (4) We used the first ED recorded vital signs and laboratory results for severity assessment, as our prior work determined these were more predictive of outcome than subsequent measurements. (15,18) Blood for laboratory studies was typically drawn at the time of initial nurse assessment and vital sign measurement. As only 13% of patients had arterial blood gases measured, we used the Severinghaus equation to convert SpO2 to PaO2 in patients without measured arterial blood gases. (18,19) We standardized the Severinghaus equation using temperature of 37.5 C (the mean population value) and pH of 7.40. Fraction of inspired oxygen for patients receiving supplemental oxygen by liter flow was estimated as previously. (18) As LDS hospital is located at an elevation of 1400 meters, we corrected PaO2/FIO2 cutoffs by dividing by the ratio of local (645 mm Hg) to sea level barometric pressure (0.85). Authorship of the dictated ED encounter note identified the physician responsible for the admission decision. Participation in care by residents was also identified by the dictation. We identified physicians caring for patients following hospital admission by authorship of the admission dictation. Concept-based query of dictated reports was applied to identify use of any objective severity assessment tool, and do-not-resuscitate/do-not-intubate (DNR/DNI) care directives. (20)
Table 1.
Infectious Disease Society of America/American Thoracic Society 2007 severe pneumonia minor criteria. CURB-65 is comprised of the 4 starred elements, plus age.
| *Respiratory rate ≥30 breaths/min |
| *Systolic blood pressure <90 mm Hg |
| *Confusion/disorientation |
| *Uremia (BUN ≥ 20 mg/dL) |
| PaO2/FiO2 ratio ≤250 |
| Multilobar infiltrates |
| Leukopenia (WBC count < 4000 cells/mm3) |
| Thrombocytopenia (platelet count < 100,000 cells/mm3) |
| Hypothermia (core temperature ≤ 36°C) |
BUN = blood urea nitrogen; WBC = white blood cell count.
Outcome measures
Length of stay (LOS) for admitted patients was determined from the EMR. Thirty-day all-cause mortality was determined by merging EMR data with vital status information from the Utah Population Database. (21) Cause of death in the 3 outpatients was identified by review of the EMR and death certificates from the Utah Population Database. We identified secondary admission to any Intermountain Healthcare Hospital within 7 days of the initial ED evaluation through the EMR. The time frame of 7 days was chosen because most secondary admissions occurred within that period, and later admissions were mostly attributable to diagnoses other than pneumonia. Patients not directly admitted to the hospital during their initial ED evaluation were termed “outpatients” regardless of secondary hospital admission. Inpatient mortality was defined as death from any cause prior to hospital discharge, censored at 30 days.
The study was approved by the Intermountain Healthcare Institutional Review Board, approved by the Intermountain Privacy Board (HIPPA waiver) and authorized by the Utah Population Database. Individual patient consent was not required as there was no intervention or patient contact.
Primary data analysis
To explore ED physician variability in the admission decision, we derived a definition of “low severity” for use as an admission rule against which we could compare physician behavior. Potential severity rules comprised disjunctive combinations of the following parameters and thresholds:
Predicted 30 day mortality risk by eCURB: 0.03, 0.04, 0.05
2007 sCAP: 2, 3, or 4 minor criteria
PaO2/FiO2 ratio: 200, 250, 260, 270, 280, 290, 300
CURB-65: 2, 3 criteria
On supplemental oxygen: Yes
For instance, one admission rule would be eCURB>=0.04, or sCAP>=4, or PaO2/FiO2<250. Another example would be eCURB>=0.03 or 2007 sCAP>=4 with no consideration of PaO2/FiO2. We tested 768 possible admission rules using these described combinations. For each potential admission rule, we determined how often the admission rule was concordant with physician behavior, both overall and for each physician individually. We ranked the candidate admission rules according to (a) the slope of the relationship between physician agreement with the admission rule and physician admission rate and (b) overall agreement between physician admission decisions and the admission rule. Specifically, we sought to achieve a maximum negative slope for the correlation between physician agreement with the admission rule and their individual rate of admission. This technique assured that low-admitting physicians were in greater agreement with the preferred admission rule than high-admitting physicians. This negative slope was weighted as twice as important as the overall agreement. We retained overall agreement in our calculations to avoid over-fitting the admission rule to the behavior of the low-admitting physicians.
Means and medians were used to describe continuous predictors based on whether the distributions were normal. Confidence intervals for proportions utilized the exact method. We used the likelihood ratio test of logistic regression models to test the hypothesis that the ED physician contributed significantly to the likelihood of admission after controlling for other factors. We included all factors present in our database that by prior literature, or by consensus of the authors, might affect the admission decision. For all agreement calculations, we utilized the simple agreement score. All statistical analyses were carried out using R v2.11.1. (22)
Results
Characteristics of study patients
The study population comprised 2,069 ED encounters (figure 1), with patient characteristics presented in table 2. Thirty-day mortality for all patients was 1.58%. Median eCURB predicted mortality for inpatients was 2.65% (mean 6.8%), versus 46 and 0.93% for outpatients. Rate of initial hospital admission was 58%. Median LOS was 3.1 days, and 10.7% of outpatients were secondarily admitted to the hospital within 7 days after outpatient care was initially chosen. Only 3 of 870 patients never admitted to LDS Hospital died within 30 days (0.34%), none within 7 days of initial ED evaluation, and none caused by pneumonia.
Figure 1. Study population.

Table 2. Study population demographics.
| Inpatient | Outpatient | |
|---|---|---|
| Study population | 1199 | 870 |
| Mean age | 63 years (SD 18) | 46 years (SD 18) |
| % Female | 48.8 % | 47.2 % |
| Outpatients admitted within 7 days | N/A | 10.7% |
| Length of Stay | 3.1 days (IQR=2-5.7) | N/A |
| eCURB predicted mortality (median) | 2.65% | 0.93% |
| Inpatient mortality | 4.92% (CI: 3.77-6.30) | N/A |
| 30-day mortality | 6.80% (CI=5.48-8.42) | 0.34%(CI= 0.07-1.00) |
Characteristics of physicians
There were 18 ED physicians who cared for at least 10 pneumonia patients during the 11-year study period. Twelve (67%) were board certified in emergency medicine, 9 (50%) certified in internal medicine, 4 (22%) certified in both specialties, and 1 (6%) had no board certification. The ED physicians in 2002 had a mean age of 44.9 (7.6) years and 2 (11%) were female. Study physicians' experience as LDS Hospital ED attendings averaged 8.4 (6.9) years as of 2002. In addition, 20 other physicians saw 43 pneumonia patients during the study years; these were treated as if seen by one aggregate physician (“other” in figure 2), and reflected ED physicians with less than 10 encounters and internal medicine physicians caring for an occasional patient in the ED. Among attending physicians caring for pneumonia patients after hospital admission, 16% were pulmonary/critical care medicine specialists, 39% were hospitalists, and 44% were family practice or internal medicine physicians other than pulmonary/critical care.
Figure 2.
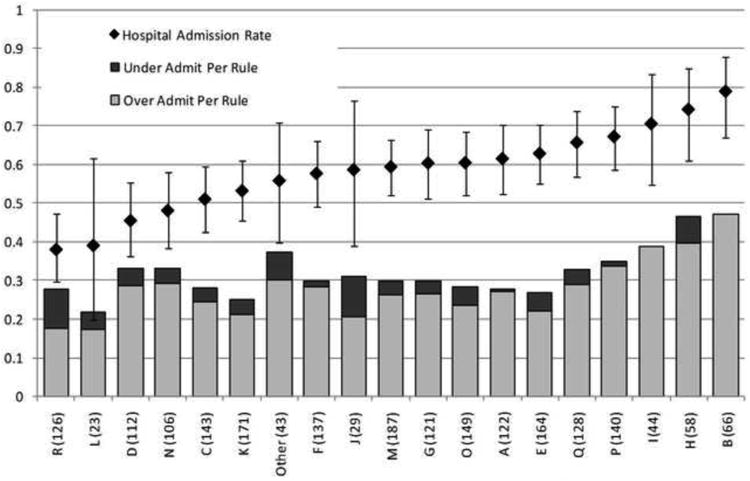
Proportion of patients admitted to the hospital (bars indicate confidence interval), and proportion of patients with discordant disposition. Discordance (stacked bar) is separated into patients admitted with “low severity” according to the rule and “non low severity” patients discharged to outpatient care. Each ED physician is signified by a letter code. The denominator for each proportion is the total number of patients per physician, indicated in parentheses.
Temporal trends over the study years
Annual ED patient volume increased gradually from 28,000 in 1996 to 39,000 in 2006. Annual number of diagnosed pneumonia cases also increased, averaging 173 cases 1996-1998 versus 222 for 2004-2006. Patients with pneumonia accounted for about 0.6% of total ED encounters. Examining the same 3-year intervals, admission rate decreased from 62.0% to 53.8%. Unadjusted 30-day mortality decreased from 6.2% 1996-1998 to 2.4% for 2004-2006. However, these decreases were not significant after adjusting for lower severity of illness (eCURB) in the later years.
Admission rates and outcomes by ED physician
Individual ED physician admission rates ranged from 38% to 79% (figure 2). The ED physician remained a highly significant predictor of admission (likelihood ratio chi-squared <0.001) in a logistic regression model adjusting for eCURB, 2007 sCAP (table 1), PaO2/FiO2 ratio, DNR/DNI directives, time of day, day of week, year patient seen, and observed mortality. There were no significant correlations between admission rate and physician age, years of ED experience, specialty board certification, or pneumonia case volume. We identified 65 cases where care was provided by a resident under an attending's supervision. There was no discernable effect of resident care on the decision for hospital admission by either univariate or multivariate logistic regression. Calculation of illness severity was documented in only 2.7% of ED patients. Dictated reports mentioned an illness severity score in an additional 1.4% of patients in the context of antibiotic selection, rather than concerning patient disposition. Among patients where severity of illness calculation was noted, 61% were admitted to the hospital, not different from the 58% admission rate observed overall.
To further explore ED physician variability in respect to the hospital admission decision in pneumonia patients, we derived a definition of “low severity” for use as an admission rule (see statistical methods). The best definition used only 3 criteria; PaO2/FiO2 ratio > 280 mm Hg, eCURB predicted mortality < 5%, and 2007 sCAP < 3 minor criteria. Compared with observed initial hospital admission, the rule was associated with a mean agreement of 69% and linear correlation of -0.71. Higher admitting physicians were more likely to be discordant in their disposition decisions compared with the admission rule (figure 2). Considerable variability between different ED physicians is evident both in admission of low severity patients, and outpatient treatment of patients who were not low severity. Physicians “I” and “B” did not disposition any non low severity patients to outpatient care, where physician “R” had the highest rate of outpatient disposition for non low severity patients. However, there was little correlation overall between rate of admission and outpatient disposition of non low severity patients, as evidenced by physicians “J” and “H”. Higher hospitalization rates were not associated with reduced mortality or fewer secondary hospital admissions.
Table 3 compares clinical outcomes in patients whose disposition was concordant with the admission rule to patients whose disposition was discordant. Outpatients who were not low severity had higher rates of secondary admission and mortality compared with low severity outpatients. Low severity admitted patients had shorter hospital length of stay and lower mortality than patients who were not low severity admitted to the hospital.
Table 3.
Patients whose disposition was concordant with the admission rule are compared to patients whose disposition was discordant.
| Concordant Triage | Discordant Triage | |||
|---|---|---|---|---|
| Admit | Outpatient | Admit/Rule Outpatient | Outpatient/Rule Admit | |
| n | 641 | 789 | 558 | 81 |
| Age | 73 | 43 | 58 | 53 |
| % Female | 49.0% | 47.8% | 48.6% | 42.0% |
| eCURB | 5.9% | 0.9% | 1.5% | 1.7% |
| LOS | 3.77 | 2.62 | ||
| Readmit 7 | 9.4% | 22.2% | ||
| Death IP | 8.7% | 0.5% | ||
| Death 30 | 11.9% | 0.3% | 1.1% | 1.2% |
Limitations
Limitations of this study include the retrospective case identification strategy based on ICD-9 coding, although reasonable sensitivity and excellent specificity of this approach have been documented at LDS Hospital (16). The requirement of radiographic confirmation of pneumonia strengthened case identification. The study design minimized the need for subjective information or data not routinely obtained; missing data were rare. It is possible that some deaths within 30 days occurred out of state in non-Utah residents, and therefore were not detected. In addition, a secondary admission to a non-Intermountain hospital would not be detected using our methods. As well, our observations were limited to a single hospital. On the other hand, the LDS Hospital EMR provides a rich source of longitudinal data recorded for clinical purposes at the time of patient encounter. This enabled observation over more than a decade, providing a sufficient number of patient encounters for statistical analysis of individual physicians.
Our methodology does not allow study of other factors that appropriately contribute to an admission decision such as co-morbid illness and patient preference. However, we think it is unlikely that those patient factors were unevenly distributed among ED physicians, therefore explaining the range of hospitalization rates. The use of objective scoring systems may be underestimated in this study. For example, CURB-65 was published in 2003, but its calculation and the practice of including it in a dictated note might have taken time to occur. Since observed admission rate significantly exceeded that recommended by CURB-65, it is unlikely that routine use of a risk stratification system went undetected.
Discussion
We observed a twofold difference in initial hospital admission rate for pneumonia patients depending on which individual physician made the decision, in an urban ED with a single group of emergency physicians. This difference was not explained by objective patient or physician characteristics. Utilization of available severity scoring systems was rarely documented, and physicians appeared to rely on their own clinical judgment to estimate illness severity. Agreement of disposition with objective severity criteria (eCURB, 2007 sCAP minor criteria, and PaO2/FiO2)) was only 69%, with higher admitting physicians having less agreement. The highest admitting physician agreed in their disposition decision in only 52% of patients seen. We conclude that observed variability in the admission decision is likely related to personality and practice style differences among ED physicians, and perhaps with less accurate estimation of illness severity.
Based on the observed variability, some patients likely incurred unnecessary hospitalization costs, complications, and delayed return to their usual activities. On the other hand, some patients selected for outpatient treatment might have benefitted from initial hospitalization. Patients admitted to the hospital or treated as outpatients discordant with the low severity rule had worse outcomes than concordant patients. The discordant disposition rate in this study is similar to hospitalization rates observed among low risk patients in trials utilizing the Pneumonia Severity Index. (23,24,25,26,27)
Beyond objective measurements of illness severity, co-morbid illness, social factors, patient preference, and subjective impressions are part of the complex admission decision. (28) Yet the availability of equivalent antibiotic regimens, home oxygen therapy, and attentive friends or family in the home environment allows many patients with pneumonia to be safely treated outside the hospital. Prior interventional studies have demonstrated decreased rate of admission with use of objective severity scoring tools. (23,24,25,26,27) However, this has been difficult to achieve outside of research settings. (29,30) Pneumonia was an uncommon ED diagnosis, and physicians rarely used time-consuming, paper-based severity scoring tools located in a file drawer.
We derived our definition of “low severity” through observation of clinical outcomes in a large ED database. The eCURB threshold of 5% predicted mortality is midway between a CURB-65 score of 1 (predicted mortality 2%, admission not advised), and a score of 2 (predicted mortality 8%, admission advised). (15) The 2007 sCAP criteria were important predictors among individuals where eCURB predicted mortality and PaO2/FiO2 were insufficient to identify need for hospitalization. This represents a novel use of these criteria, which were developed to identify patients with severe pneumonia needing ICU admission, rather than as hospital admission criteria.
Conclusions
Treatment of pneumonia patients in the LDS Hospital ED was associated with a low mortality rate that improved over time. However, unexplained variability in admission decisions by physicians suggests that further improvement in pneumonia care is possible, as this variability is not likely associated with best care. We plan to test our admission rule in a prospective, controlled implementation of a real time, electronic decision support tool.
Acknowledgments
We are grateful to Al Jephson for data extraction. We thank the LDS Hospital ED physicians for their dedication to patient care and interest in quality improvement.
This work has been presented in abstract form at the American Thoracic Society International Conference May 2010, New Orleans, LA, USA, and the Society of Academic Emergency Medicine Conference June 2010 Phoenix, AZ, USA.
This work was supported by a grant from the Deseret Foundation, Salt Lake City, UT, USA.
Footnotes
No author has a confict of interest relevant to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Center for Health Statistics. [Accessed June 7, 2010];Health, United States, April 24 2008. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr5610.pdf.
- 2.Marston BJ, Plouffe JF, File TM, et al. Incidence of community-acquired pneumonia requiring hospitalization. Results of a population-based active surveillance study in Ohio. The community-based Pneumonia Incidence Study Group. Arch Intern Med. 157(15):1709–18. [PubMed] [Google Scholar]
- 3.Niederman MS, McCombs JS, Unger AN, et al. The cost of treating community- acquired pneumonia. Clin Ther. 1998;20:820–37. doi: 10.1016/s0149-2918(98)80144-6. [DOI] [PubMed] [Google Scholar]
- 4.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(2):S27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Labarere J, Stone RA, Obrosky DS, et al. Comparison of outcomes for low-risk outpatients and inpatients with pneumonia: A propensity-adjusted analysis. Chest. 2007;131(2):480–488. doi: 10.1378/chest.06-1393. [DOI] [PubMed] [Google Scholar]
- 6.Carratalà J, Fernández-Sabé N, Ortega L, et al. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients. Ann Intern Med. 2005 Feb 1;142(3):165–72. doi: 10.7326/0003-4819-142-3-200502010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Coley CM, Li YH, Medsger AR, et al. Preferences for home vs hospital care among low-risk patients with community-acquired pneumonia. Arch Intern Med. 1996 Jul 22;156(14):1565–71. [PubMed] [Google Scholar]
- 8.Minogue MF, Coley CM, Fine MJ, et al. Patients hospitalized after initial outpatient treatment for community-acquired pneumonia. Ann Emerg Med. 1998 Mar;31(3):376–80. doi: 10.1016/s0196-0644(98)70350-6. [DOI] [PubMed] [Google Scholar]
- 9.McMahon LF, Jr, Wolfe RA, Tedeschi PJ. Variation in hospital admissions among small areas: a comparison of Maine and Michigan. Med Care. 1989;27:623–31. doi: 10.1097/00005650-198906000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Rosenthal GE, Harper DL, Shah A, et al. A regional evaluation of variation in low-severity hospital admissions. J Gen Intern Med. 1997 Jul;12(7):416–22. doi: 10.1046/j.1525-1497.1997.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Thoracic Society. Guidelines for the initial management of adults with community acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am Rev Respir Dis. 1993;148:1418–1426. doi: 10.1164/ajrccm/148.5.1418. [DOI] [PubMed] [Google Scholar]
- 12.Dean NC, Silver MP, Bateman KA, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med. 2001;110:451–7. doi: 10.1016/s0002-9343(00)00744-0. [DOI] [PubMed] [Google Scholar]
- 13.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–82. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dean NC, Bateman KA. Local guidelines for community-acquired pneumonia: development, implementation, and outcome studies. Infect Dis Clin North Am. 2004;18(4):975–91. doi: 10.1016/j.idc.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Jones BE, Jones J, Bewick T, et al. CURB-65 pneumonia severity assessment adapted for electronic decision support. Chest. 2011;140:156–163. doi: 10.1378/chest.10-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aronsky D, Haug PJ, Lagor C, et al. Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20(6):319–28. doi: 10.1177/1062860605280358. [DOI] [PubMed] [Google Scholar]
- 17.Niederman MS, Craven D, Bonten MJ, et al. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 18.Brown SM, Jones B, Jephson AJ, et al. Validating the ATS-IDSA 2007 Predictors of Severe Community-Acquired Pneumonia (SCAP) Crit Care Med. 2009 Dec;37(12):3010–6. doi: 10.1097/CCM.0b013e3181b030d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Severinghaus JW. Simple, accurate equations for human blood O2 dissociation computations. J Appl Physiol: Respirat Environ Exercise Physiol. 1979;46(3):599–602. doi: 10.1152/jappl.1979.46.3.599. revisions, 1999, 2002, 2007. [DOI] [PubMed] [Google Scholar]
- 20.Aronsky D, Kasworm E, Jacobson E, et al. Electronic screening of dictated reports to identify patients with do-not-resuscitate status. J Am Med Inform Assoc. 2004;11(5):403–9. doi: 10.1197/jamia.M1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skolnick M. The Utah genealogical database: a resource for genetic epidemiology. In: Cairns JL, Skolnick M, editors. Banbury Report No 4; Cancer Incidence in Defined Populations. Cold Spring Harbor Laboratory; New York: 1980. pp. 285–97. [Google Scholar]
- 22.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2010. URL http://www.R-project.org. [Google Scholar]
- 23.Atlas SJ, Benzer TI, Borowsky LH, et al. Safely increasing the proportion of patients with community-acquired pneumonia treated as outpatients: an interventional trial. Arch Intern Med. 1998;158:1350–6. doi: 10.1001/archinte.158.12.1350. [DOI] [PubMed] [Google Scholar]
- 24.Marrie TJ, Lau CY, Wheeler SL, et al. A controlled trial of a critical pathway for treatment of community- acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin. JAMA. 2000;283:749–55. doi: 10.1001/jama.283.6.749. [DOI] [PubMed] [Google Scholar]
- 25.Yealy DM, Auble TE, Stone RA, et al. Effect of increasing the intensity of implementing pneumonia guidelines: a randomized, controlled trial. Ann Intern Med. 2005;143:881–94. doi: 10.7326/0003-4819-143-12-200512200-00006. [DOI] [PubMed] [Google Scholar]
- 26.Capelastegui A, Espana PP, Quintana JM, et al. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27:151–7. doi: 10.1183/09031936.06.00062505. [DOI] [PubMed] [Google Scholar]
- 27.Dean NC, Suchyta M, Bateman K, et al. Implementation of admission decision support for community-acquired pneumonia. Chest. 2000;117:1368–1377. doi: 10.1378/chest.117.5.1368. [DOI] [PubMed] [Google Scholar]
- 28.Aujesky D, McCausland JB, Whittle J, et al. Reasons why emergency department providers do not rely on the pneumonia severity index to determine the initial site of treatment for patients with pneumonia. Clin Infect Dis. 2009;49(10):e100–8. doi: 10.1086/644741. [DOI] [PubMed] [Google Scholar]
- 29.Halm EA, Horowitz C, Silver A, et al. Limited impact of a multicenter intervention to improve the quality and efficiency of pneumonia care. Chest. 2004;126:100–7. doi: 10.1378/chest.126.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee RW, Lindstrom ST. A teaching hospital's experience applying the Pneumonia Severity Index and antibiotic guidelines in the management of community-acquired pneumonia. Respirology. 2007;12(5):754–8. doi: 10.1111/j.1440-1843.2007.01121.x. [DOI] [PubMed] [Google Scholar]


