Abstract
BACKGROUND:
Locus of control (LOC) is related to the impact of headaches and chronic pain; however, literature evidence regarding LOC is not always consistent. Several authors consider this to be due, in part, to the separate interpretation of LOC factors, during which the interaction among them is ignored. In 1982, Wallston and Wallston proposed eight possible LOC health patterns depending on whether the individual scored high or low in each of three dimensions.
OBJECTIVE:
To identify these LOC patterns in patients with headaches and chronic pain, and to validate them in terms of their association with a selection of the main pain indicators.
METHODS:
A total of 228 individuals were recruited at three public centres in Seville, Spain. Participants completed a semistructured clinical interview and several questionnaires assessing psychological variables related to pain. The main statistical analyses used were two-step cluster analysis and ANCOVA.
RESULTS:
The six-cluster solution was optimal. The patterns observed coincided with: the believer in control; the yea-sayer; the pure chance; the pure internal; the pure professional; and the nay-sayer clusters. The double external or type VI clusters were not observed. Clusters could be classified from the best to the worst adjustment to chronic pain.
CONCLUSIONS:
These results support the empirical validity of the theoretical model of LOC patterns proposed in 1982 by Wallston and Wallston among a chronic pain population. The analysis of patterns provides more accurate information regarding the adjustment to pain compared with analysis of the LOC factors separately.
Keywords: Chronic pain, Headache, Locus of control, Patients’ subgroups, Psychological assessment, Two-step cluster analysis
Abstract
HISTORIQUE :
Le locus de contrôle (LdC) est lié aux répercussions des céphalées et de la douleur chronique. Cependant, les données probantes tirées des publications ne sont pas toujours compatibles. Plusieurs auteurs pensent que ce phénomène est partiellement attribuable à l’interprétation distincte des facteurs de LdC, qui néglige l’interaction entre les facteurs. En 1982, Wallston et Wallston ont proposé huit profils de santé de LdC possibles selon les résultats faibles ou élevés de l’individu dans chacune des trois dimensions.
OBJECTIF :
Déterminer les profils de LdC chez les patients souffrant de céphalées et de douleur chronique et en valider l’association avec une sélection des principaux indicateurs de douleur.
MÉTHODOLOGIE :
Au total, 228 personnes ont été recrutées dans trois centres publics de Séville, en Espagne. Les participants ont rempli une entrevue clinique semi-structurée et plusieurs questionnaires évaluant les variables psychologiques liées à la douleur. Les principales analyses statistiques utilisées étaient des analyses de grappe en deux étapes et l’analyse de covariance.
RÉSULTATS :
La solution à six grappes était optimale. Les profils observés coïncidaient avec la grappe des convaincus du contrôle, des positifs, des hasards purs, des internes purs, des professionnels purs et des négatifs. On n’a pas observé de grappes externes doubles ou de type VI. Les grappes pourraient être classées de la meilleure à la pire adaptation à la douleur chronique.
CONCLUSIONS :
Les présents résultats étayent la validité empirique du modèle théorique de profils de LdC qu’ont proposé Wallston et Wallston en 1982 au sein de la population souffrant de douleur chronique. L’analyse des profils fournit des renseignements plus précis à l’égard du soulagement de la douleur par rapport à l’analyse des facteurs distincts de LdC.
The concept of locus of control (LOC) was introduced by Rotter (1) to refer to the control-over-reinforcements attribution process. He formulated it as general and one-dimensional: internality, understood as the degree of control over reinforcements an individual perceives. Subsequent research has broadly confirmed the utility of this construction, but a few modifications have been proposed. First, a dimension for internality (I-LOC) and another for externality (E-LOC) have been created; however, the latter has also been divided. E-LOC is thus distinguished between the action of powerful others (P-LOC) and chance (C-LOC), ie, the role of luck (2). On the other hand, in terms of generality, Wallston (3) provides an in-depth examination of LOC’s conceptual evolution by proposing three levels of analysis: general, as conceived by Rotter (1), ie, stable and consistent; the intermediate level, covering the concrete domains of life such as health, work or interpersonal relations; and the specific level, which refers to a particular situation or specific behaviour.
Wallston et al (4) were among the first authors to use the LOC concept in health. Based on the research conducted by Levenson (2), they developed the Multidimensional Health Locus of Control (MHLC) (5). One of the most significant novelties in the LOC health concept was including health professionals as the ‘doctors’, an incorporation that has occurred since Form C of the MHLC scales was developed (6). There is abundant evidence that LOC is an influential variable in health. For example, according to the 1970 British Cohort Study, when LOC is measured after 10 years, it serves as an important predictor of different health indicators at 30 years of age such as obesity, excessive weight, perception of health and stress (7).
If we follow Wallston’s concept (3), the pain LOC is located at an intermediate specific level, which is somewhat more specific than the health LOC. With regard to chronic pain, the main evidence regarding LOC is centred on its connection with the impact of the disorder and the effectiveness of treatments.
With reference to the first aspect, the I-LOC has been associated with better adjustment to the disorder, less pain and lower disability levels (8,9), a better quality of life (10,11), more adaptive coping (12–15) and higher likelihood of returning to work (16,17). In contrast, C-LOC and P-LOC are usually associated with more serious pain and the interference of pain in daily life (18,19) including decreased physical activity (20) and abuse of medication (21,22). Furthermore, individuals among whom C-LOC prevails use more maladaptive coping strategies such as catastrophising (23).
With regard to the connection of LOC with treatments, low levels of I-LOC and high levels of P-LOC are in the precontemplative phases of therapeutic change (24). Once interventions are made, I-LOC provides therapeutic effectiveness, acting as a moderating variable in psychological (25) and multimodal (26) treatments as well as in physiotherapeutic (14) treatments.
In addition, I-LOC has been used as a result variable in several types of treatment such as self-hypnosis (27), physiotherapy (28) and, above all, multidisciplinary therapy (29–31).
In spite of the statements above, the evidence regarding the role of LOC in chronic pain is not always consistent (32). For example, psycho-educational interventions have increased the scores for E-LOC but not for I-LOC (33). In some studies, LOC has not been associated with disorder impact parameters (34,35) or with more adaptive coping with pain (12).
Several authors consider this to be due, in part, to the separate interpretation of LOC factors, during which the interaction among them is ignored (32,36–38). In fact, studies on LOC that comprehensively consider such factors are rare. In that respect, the theoretical proposal of Wallston and Wallston (38) broke new ground. The authors identified eight possible LOC health patterns depending on whether the individual scored high or low in each of the three dimensions (Table 1).
TABLE 1.
Proposed locus of control (LOC) patterns
| Type | Description | I-LOC | P-LOC | C-LOC | Comment |
|---|---|---|---|---|---|
| I | Pure internal (PI-LOC) | + | − | − | “…depends on me” |
| II | Pure powerful others (PP-LOC) | − | + | − | “…depends on others” |
| III | Pure chance (PC-LOC) | − | − | + | “…depends on chance” |
| IV | Double external (DE-LOC) | − | + | + | “…does not depend on me” |
| V | Believer in control (BiC-LOC) | + | + | − | “…depends partly on me and partly on others” |
| VI | Type VI-LOC* | + | − | + | “…depends partly on me and partly on chance” |
| VII | Yeasayer (YS-LOC) | + | + | + | “…depends on all these three factors” |
| VIII | Naysayer (NS-LOC) | − | − | − | “…does not depend on any of these three factors” |
We only found five empirical validation studies on the proposal made by Wallston and Wallston (38), all of which used cluster analysis. They were conducted using samples of university students (39), patients with chronic pain (36), women (40), adolescents (41) and cancer patients awaiting transplants (42). The number of patterns validated by researchers varied from three (42) to four (36) to five (40) to six (39) and, in yet another study, all eight patterns of the theoretical proposal were validated (41). In general, studies with a greater number of subjects and with nonpatient samples show a higher number of clusters, with a more balanced distribution of cases among them.
Pure internal (PI)-LOC was found in all of the studies mentioned, except for that conducted among cancer patients (42). It was associated with higher educational and socioeconomic levels, a better general state of health (40), and with an active, although self-blaming, disease management style (36). Pure powerful others (PP)-LOC coincides with PI-LOC in the active coping style, but it also incorporates causal worry and stress attributions associated with the disease (39,42). Believer in control (BiC)-LOC, found in all the studies except for those conducted among cancer patients (42), is similar to PI-LOC, and is associated with active pain coping styles (36), a better general state of health (41), and the active search for treatment (40). All that is known about the pure chance (PC)-LOC is that it is associated with a worse state of health (40,41). The double external (DE)-LOC is known to be associated with depressive coping styles (42). The type VI-LOC was only found in the study on adolescents (41), who associated it with a poorer general state of health (41). The yeasayer (YS)-LOC was found in all studies, except the study that examined patients experiencing chronic pain (36), and was associated with poorer general health, low educational and socioeconomic levels, elevated neuroticism and social desirability (40). However, it was also connected to active disease coping styles (39,42). Regarding the nay-sayer (NS)-LOC, in spite of the fact that it was found in all studies except for the study that examined cancer patients (42), only the Eysenck Personality Inventory study (40) found a positive correlation between NS-LOC and social desirability. Thus, PI-LOC, PP-LOC and BiC-LOC patterns appear to be associated with a lesser impact of the disorder and a better state of health in general terms, unlike the other patterns.
In summary, evidence regarding the role of LOC patterns in health is limited to a single study in the case of chronic pain.
Based on the theoretical proposal of Wallston and Wallston (38), the purpose of the present study was to identify LOC patterns in patients with headaches and chronic pain, and to validate them in terms of their association with a selection of the main indicators of experiencing pain used in the studies investigating pain LOC. Based on the studies mentioned above, we propose two hypotheses. First, we expect to find all eight pain LOC patterns. Second, we hypothesize that individuals with the PI-LOC, PP-LOC and BiC-LOC patterns will have significantly lower scores than individuals with the other five patterns (NS-LOC, PC-LOC, YS-LOC, type VI-LOC and DE-LOC) in pain maladjustment indicators (pain intensity, pain frequency, use of medication, negative automatic thoughts, pain behaviour and maladaptive coping strategies). Similarly, we expect individuals with the PI-LOC, PP-LOC and BiC-LOC patterns to have higher scores in pain adjustment indicators (adaptive coping strategies and perceived self-efficacy).
METHODS
Participants
The study sample consisted of 228 individuals who were recruited at three public centres in Seville, Spain. Two were primary care centres, and one was a pain care unit. After a scientific-technical cooperation agreement with the health districts involved, the centres were selected to guarantee the presence of patients from urban, suburban and rural areas, as well as the two levels of medical care (primary and specialized). Patients treated at the centres mentioned above were invited to participate by their physicians and, thus, their informed consent was required. The study was presented as part of the patients’ medical care. Patients were receiving pharmacological treatment at the primary care centres (analgesics, migraine medication, antianxiety agents and/or antidepressants), and 36% attended acupuncture sessions at the pain care unit (the mean [± SD] number of sessions was 3.55±7.7). They did not receive any other type of medical care, psychological treatment or any other kind of treatment. The sampling used was incidental. To meet the requirements of another study (43), patients in the primary care centres should have had a diagnosis of headache while the patients in the pain unit should have been diagnosed with chronic pain. For this reason, almost one-half the sample consisted of patients with headaches; to distinguish them, they will be referred to here as the headache and chronic pain subsamples. One hundred per cent of the subjects of legal age invited to participate on a consecutive basis for one month were included, in the order in which they attended scheduled appointments with their physicians. Research was performed according to the ethical principles established in the Declaration of Helsinki (44) and the International Association for the Study of Pain guideline for pain research in humans (45), and was approved by the ethics committees of both the South Seville Primary Care Health District and the University of Seville. Sociodemographic information of the sample is shown in Table 2.
TABLE 2.
Sociodemographic data of the sample
| Entire sample n=228 (100%) | Headaches n=118 (52%) | Chronic pain n=100 (48%) | |
|---|---|---|---|
| Sex | |||
| Female | 86.3 | 85.6 | 81.8 |
| Male | 14.7 | 14.4 | 18.2 |
| Age, years, mean ± SD | 41±9.7 | 39±9.9 | 44±8.7 |
| Academic level | |||
| None | 22 | 21 | 23 |
| Primary | 46 | 44 | 47 |
| Secondary | 22 | 24 | 20 |
| University | 10 | 11 | 10 |
| Marital status | |||
| Single | 11 | 16 | 5 |
| Married/cohabitating | 83 | 82 | 84 |
| Other | 6 | 2 | 11 |
| Job status | |||
| Housewives | 44 | 56 | 32 |
| Working | 27 | 26 | 28 |
| Disabled | 18 | 3 | 34 |
| Students | 6 | 9 | 3 |
| Unemployed | 5 | 6 | 4 |
| Per capita income per year, €, mean ± SD | 3,964±4,737 | 3,495±2,921 | 4,466±6,089 |
Data presented as % unless otherwise indicated
Measures
To assess the clinical pain parameters (and also the sociodemographic variables) a semistructured clinical interview was used to determine: diagnosis; chronicity (duration of the condition in years); intensity of pain (11-point numerical scale); frequency of pain (in crises/episodes per month); duration of the crises/episodes of pain (in h/day); interference of pain (mild/moderate/severe); medication (per day); and the number of acupuncture sessions in the past year.
Taking into consideration that one-half of the sample consisted of patients with headaches, the Spanish language adaptation of the Headache Specific-Locus of Control (HSCL) scale was used to measure the pain LOC (46). The HSLC scale is a measure derived from the MHLC scales (47) and consists of 33 scorable items on a 5-point Likert-type scale, which provide three factors: internal, health care professionals and chance. It has sufficient internal consistency (Cronbach α coefficients between 0.84 and 0.88) and validity (46,48). An adaptation of the complete scale was used with the sample of the present study, eliminating the term ‘head’ when the patient was not experiencing headaches (43). In this adaptation, the factor analysis revealed a structure identical to that obtained by Martin et al (46), and VandeCreek and O’Donnell (48), except for items 27 (“When my doctor makes a mistake I end up having a pain episode”) and 12 (“My pain is alleviated just by going to the doctor’s”), which had a factorial weight lower than 0.30 and were eliminated. Internal consistency was high, with Cronbach α coefficients of 0.82 and 0.86.
Other instruments used for the assessment of variables involved in stress and pain coping processes were the Inventory of Negative Thoughts in Response to Pain (49) in its Spanish-language adaptation (50), which has an internal consistency of 0.91; a Spanish-language adaptation of the Coping Strategies Questionnaire (51,52), with internal consistency coefficients between 0.68 and 0.89; a Spanish-language adaptation of the Pain Behaviour Questionnaire (53,54) with internal consistency coefficients between 0.70 and 0.89; and the Headache Self-Efficacy Scale (55), a Spanish-language adaptation with modifications similar to those of the HSLC (43), with an internal consistency of 0.94. The Inventory of Negative Thoughts in Response to Pain measures negative automatic thoughts; the Coping Strategies Questionnaire assesses coping strategies, both maladaptive (catastrophizing, and faith and prayer) and adaptive (distracting behaviours, ignoring pain, reinterpreting pain, coping self-statements, hope and cognitive distraction); the Pain Behaviour Questionnaire assesses pain behaviours (nonverbal complaints, verbal complaints, stimuli avoiding and activities avoiding); and the Headache Self-Efficacy Scale measures expectations of perceived self-efficacy. All of the variables mentioned in this paragraph were considered as criteria of adjustment to chronic pain based on the scientific evidence mentioned in the introduction. Thus, low scores on negative automatic thoughts, maladaptive coping strategies and pain behaviour, and/or high scores on adaptive coping strategies and perceived self-efficacy would indicate good psychological adjustment to chronic pain. If the opposite occurred (high scores on the former and low scores on the latter), this would suggest poor adjustment to chronic pain. For the purposes of description, the degree of adjustment to chronic pain was assessed based on the quantity of criteria listed above that have been met. The structured interview and the other instruments were administered by the first author.
Statistical analysis
To present the sample percentages, means and SDs were used. To obtain the LOC patterns, two-step cluster analysis was used based on the HSLC scores. This procedure is an exploratory tool designed to reveal natural groupings (or clusters) within a data set that would otherwise not be apparent. The algorithm used in this procedure has several desirable features that differentiate it from traditional clustering techniques such as the automatic selection of the number of clusters. The log-likelihood distance measurement and the Akaike Information Criterion as the clustering criterion were used. A series of ANCOVA analyses with Bonferroni multiple comparisons was used to validate the clusters, as well as χ2 analyses in the case of nominal variables. A significance level of P<0.05 was established. All data were processed using PASW version 18 (IBM Corporation, USA). The unique nature of the sample, which contains almost one-half of the headache cases, was taken into consideration in all of the statistical analyses mentioned above.
RESULTS
Table 3 shows the main descriptive statistics for both the overall sample and for the headache and chronic pain subsamples corresponding to clinical data and outcome variables.
TABLE 3.
Descriptive statistics of the sample
| Clinical data | Entire sample, n=228 (100%) | Headaches, n=118 (52%) | Chronic pain, n=100 (48%) | |
|---|---|---|---|---|
| Specific diagnosis | Migraine, 33%; chronic tension-type headache, 19%; fibromyalgia, 16%; chronic low back pain, 7%; neck pain, 4%; arthritis, 3%; arthrosis, 3%; other, 15% | Migraine, 63%; chronic tension-type headache, 37% | Fibromyalgia, 34%; chronic low back pain, 16%; neck pain, 9%; arthritis, 8%; arthrosis, 6%; postsurgical pain, 5%; ankylosing spondylitis, 4%; atypical facial pain, 3%; carpal tunnel syndrome, 3%; herniated disc, 3%; tendinitis, 2%; chest pain, 2%; other, 5% | |
| Chronicity, years | 12±10 | 14±11 | 9±8 | |
| Clinical outcome variables | ||||
|
| ||||
| Pain intensity, 0–10 | 6.7±1.9 | 6.7±2 | 6.8±1.7 | |
| Pain frequency, days/month | 19±12 | 11.5±11 | 27.6±6.1 | |
| Pain duration, h | 24±16 | 27.7±18.6 | 18.9±9.8 | |
| Pain interference, % | ||||
| Mild | 8 | 9 | 5 | |
| Moderate | 65 | 67 | 64 | |
| Severe | 27 | 24 | 31 | |
| Daily medication | 1.26±0.73 | 1.34±0.66 | 1.18±0.8 | |
| Psychological outcome variables | Range | |||
|
| ||||
| Negative automatic thoughts (INTRP) | 0–84 | 21.83±16.4 | 18.8±15.5 | 25.1±16.7 |
| Perceived self-efficacy (HSES) | 1–5 | 2.38±0.93 | 2.4±0.85 | 2.36±1 |
| Adaptive coping (CSQ) | 0–180 | 65.4±31.2 | 62.24±29.9 | 68.9±32.4 |
| Maladaptive coping (CSQ) | 0–54 | 20.6±13.6 | 20.21±14 | 21±13.1 |
| Pain behaviors (PBQ) | 0–64 | 28.85±13.1 | 29.84±13.37 | 27.8±12.9 |
| Clustering variables | ||||
|
| ||||
| Internal locus of control (HSLC) | 0–44 | 36.9±8.5 | 37.1±7.8 | 36.8±9.3 |
| Chance locus of control (HSLC) | 0–44 | 34.5±7.9 | 33.7±7.95 | 35.4±7.8 |
| Health care professionals locus of control (HSLC) | 0–36 | 30.3±6.6 | 29.7±6.3 | 30.9±6.9 |
Data presented as mean ± SD unless otherwise indicated. CSQ Coping Strategies Questionnaire; INTRP Inventory of Negative Thoughts in Response to Pain; HSES Headache Self-Efficacy Scale; HSLC Headache Specific-Locus of Control; PBQ Pain Behaviour Questionnaire
Classification of patients according to LOC scores
The procedure classified 223 of the 228 cases correctly (five were excluded from the analysis due to missing values for one or more of the variables). The six-cluster solution was optimal because of the significant decline in the Akaike Information Criterion value (297.13) and the high ratio of distance measures (1.54). In the taxonomy of Wallston and Wallston (38), the highest to lowest number of subjects in each cluster coincided with the BiC-LOC (n=70; 31%); the YS-LOC (n=42; 19%); the PC-LOC (n=40; 18%); the PI-LOC (n=25; 11%); the PP-LOC (n=25; 11%); and the NS-LOC (n=21; 10%). The clusters DE-LOC or type VI-LOC were not observed. There were no statistically significant differences in the number of cases of headaches versus chronic pain included in each cluster (χ2=5.63; P=0.34). Of all cases included in each cluster, headache versus chronic pain distribution was 51% versus 49% in BiC-LOC, 43% versus 57% in YS-LOC, 50% versus 50% in PC-LOC, 72% versus 28% in PI-LOC, 48% versus 52% in PP-LOC and 52% versus 48% in NS-LOC. Therefore, the cluster analysis was not replicated for both subsamples separately, and it was determined that it was unnecessary to control this variable in the subsequent ANCOVAs.
The standardized means are presented in Figure 1. Individuals in the BiC-LOC cluster were characterized by high scores on I-LOC and P-LOC and low scores on C-LOC. Individuals in the YS-LOC cluster exhibited high scores on all the three LOC. Individuals in the PC-LOC cluster were characterized by high scores on C-LOC and low scores on I-LOC and P-LOC, while individuals in the PI-LOC cluster had high scores on I-LOC and low scores on C-LOC and P-LOC. Individuals in the PP-LOC cluster were characterized by high scores on P-LOC and low scores on I-LOC and C-LOC. Finally, those in the NS-LOC cluster were characterized by low scores on all three of the LOC.
Figure 1).
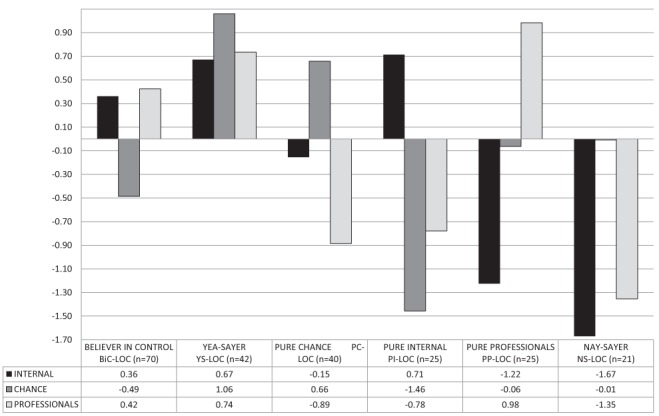
Standardized means in locus of control clusters
Clinical and psychological correlates of LOC patterns
Whether sociodemographic variables influenced the LOC patterns was also examined. No statistically significant differences were found in the LOC patterns in terms of sex (χ2=2.03; P=0.84), marital status (χ2=9.09; P=0.52) or job status (χ2=21.78; P=0.35). However, differences were found in age (F=3.94; P<0.01), per capita income (F=3.68; P<0.01) and academic level (χ2= 69.76; P<0.001). The mean (± SD) age of individuals in YS-LOC (45.17±9.05 years) and PP-LOC (45±7.56 years) was significantly higher than that of NS-LOC (41.29±9.49 years), PC-LOC (38.7±10.66 years), BiC-LOC (40.33±9.33 years) and PI-LOC (37.8±9.84 years). Individuals with PI-LOC (6.94±4.41) reported per capita income significantly higher than the other five profiles: NS-LOC (3.58±2.12); PC-LOC (3.06±2.47); BiC-LOC (4.8±7.18); YS-LOC (2.78±2.62); and PP-LOC (2.82±2.12). Similarly, 48% of PI-LOC had a university education level, while 83% of those classified as YS-LOC and 80% of PC-LOC had received no education or only primary education. The distribution of the other clusters was much more balanced. Thus, age, per capita income and academic level were included in the ANCOVA analysis as covariates.
Table 4 shows the associations between the different LOC patterns and the clinical and psychological outcome variables. With regard to the former, only the difference in the frequency of pain was statistically significant; in the case of the latter, all were statistically significant except adaptive coping. If pairwise comparisons are used, clusters can be classified from the best to the worst adjustment: PI-LOC, PP-LOC, BiC-LOC, NS-LOC, PC-LOC and YS-LOC.
TABLE 4.
Clinical and psychological correlates of locus of control (LOC) patterns controlling age, per capita income and academic level (ANCOVA)
| Variable | Range | F | P | Partial η2 | Bic-LOC (n=70) | YS-LOC (n=42) | PC-LOC (n=40) | PI-LOC (n=25) | PP-LOC (n=25) | NS-LOC (n=21) |
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | ||||||||||
| Pain intensity | 0–10 | 1.88 | 0.09 | 0.05 | 6.32±0.23 | 7.36±0.31 | 7.09±0.30 | 6.24±0.40 | 6.87±0.38 | 6.86±0.41 |
| Pain frequency | Days/month | 3.18 | <0.01 | 0.07 | 18.03±1.38 | 21.19±1.85 | 24.49±1.83 | 14.07±2.44 | 19.16±2.32 | 15.25±2.5 |
| Pain duration | h | 0.79 | 0.56 | 0.02 | 22.30±1.87 | 22.07±2.57 | 23.14±2.49 | 24±3.32 | 24.14±3.15 | 29.51±3.39 |
| Pain interference | 1–3 | 2.15 | 0.06 | 0.05 | 2.06±0.07 | 2.39±0.09 | 2.31±0.09 | 2.07±0.12 | 2.26±0.11 | 2.19±0.12 |
| Medication | Daily | 1.74 | 0.13 | 0.02 | 1.37±0.09 | 1.40±0.12 | 1.08±0.11 | 1.19±0.15 | 1.06±0.14 | 1.13±0.16 |
| Psychological | ||||||||||
| Negative automatic thoughts (INTRP) | 0–84 | 11.89 | <0.001 | 0.22 | 16.05±1.72 | 36.21±2.35 | 26.88±2.31 | 14.66±3.05 | 18.95±2.89 | 15.33±3.11 |
| Perceived self-efficacy (HSES) | 1–5 | 5.34 | <0.001 | 0.12 | 2.43±0.11 | 2.04±0.14 | 2.1±0.14 | 2.87±0.19 | 3±0.2 | 2.28±0.2 |
| Adaptive coping (CSQ) | 0–180 | 2.2 | 0.06 | 0.05 | 69.15±3.8 | 61±5.09 | 57.14±4.98 | 81.24±6.73 | 65±6.41 | 55.55±6.79 |
| Maladaptive coping (CSQ) | 0–54 | 9.52 | <0.001 | 0.18 | 18.24±1.46 | 30.67±1.96 | 23.49±1.96 | 8.96±2.58 | 19.33±2.44 | 17.4±2.63 |
| Pain behaviours (PBQ) | 0–64 | 6.86 | <0.001 | 0.14 | 27.85±1.47 | 38.59±1.98 | 27.39±1.96 | 20.46±2.61 | 26.62±2.52 | 26.84±2.67 |
Data presented as mean ± SEM unless otherwise indicated. All pairwise comparisons are explained in the text. BiC LOC Believer in control pattern; CSQ Coping Strategies Questionnaire; HSES Headache Self-Efficacy Scale; INTRP Inventory of Negative Thoughts in Response to Pain; NS-LOC Nay-sayer locus of control pattern; PBQ Pain Behaviour Questionnaire; PC-LOC Pure chance locus of control pattern; PI-LOC Pure internal locus of control pattern; PP-LOC Pure professional locus of control pattern; YS-LOC Yea-sayer locus of control pattern
The PI-LOC pattern displayed lower scores on pain frequency and on negative automatic thoughts than the YS-LOC and the PC-LOC profiles; lower scores on pain behaviours than the BiC-LOC, the YS-LOC and the PC-LOC profiles; lower scores on maladaptive coping than all the other profiles; and higher scores on perceived self-efficacy than all other profiles except the PP-LOC.
The PP-LOC pattern showed lower scores on negative automatic thoughts than the YS-LOC and the PC-LOC profiles; lower scores on pain behaviours and maladaptive coping than the YS-LOC profile (although higher scores on maladaptive coping than the PI-LOC profile were observed); and higher scores on perceived self-efficacy than all other profiles except the PI-LOC.
The BiC-LOC pattern showed lower scores on pain frequency than the PC-LOC; lower scores on negative automatic thoughts than the YS-LOC and the PC-LOC profiles; lower scores on pain behaviours and on maladaptive coping than the YS-LOC profile, although higher scores on both than the PI-LOC profile; and higher scores on perceived self-efficacy than the YS-LOC profile, but also lower scores than the PI-LOC profile.
The NS-LOC pattern had lower scores on negative automatic thoughts than the YS-LOC and the PC-LOC profiles; lower scores on pain behaviours and on maladaptive coping than the YS-LOC profile, although higher scores on maladaptive coping than the PI-LOC profile; and lower scores on perceived self-efficacy than the PI-LOC and the PP-LOC profiles.
The PC-LOC pattern showed lower scores on pain frequency than the PI-LOC, the BiC-LOC and the NS-LOC; higher scores on negative automatic thoughts than all the other profiles; higher scores on mal-adaptive coping and on pain behaviours than the PI-LOC, although lower scores on pain behaviours than the YS-LOC; and lower scores on perceived self-efficacy than the PI-LOC and PP-LOC profiles.
The YS-LOC pattern showed higher scores on pain frequency than the PI-LOC profiles; higher scores on negative automatic thoughts, pain behaviours and maladaptive coping than all the other profiles; and lower scores on perceived self-efficacy than the PI-LOC, PP-LOC and BiC-LOC profiles.
DISCUSSION
The goal of the present study was to identify and validate the LOC patterns proposed by Wallston and Wallston (38) in a sample of patients experiencing headaches and chronic pain.
Regarding the first goal, we were forced to abandon our original hypothesis of finding all eight patterns of the LOC. We only identified six: the BiC-LOC, YS-LOC, PC-LOC, PI-LOC, PP-LOC and NS-LOC. The number of patterns found is similar to that reported for students (39); higher than that reported for chronic pain patients (36), cancer patients (42) and mothers (40), and lower than that reported for adolescents (41). When our results are compared with all similar studies, it appears that there is a positive association between the size of the sample and the number of clusters found.
As for the type of patterns found and the resulting distribution of the cases, the best match occurs in the study of mothers (40). Type VI-LOC and DE-LOC were the two patterns not found in our study. Wallston and Wallston (38) predicted that pattern type VI-LOC would be rare and infrequent; in fact, it only appeared in the study involving adolescents (41). As these authors argued, type VI-LOC may be theoretically inconsistent or may result from the understanding that certain aspects of health depend on the patient while others are totally unpredictable. In any case, in patient samples such as ours, this pattern type could represent patients who reject health care professionals and, therefore, such patients would likely not be recruited at health centres.
In some cases, the DE-LOC pattern has been found in the other studies, but the number of cases is small. For example, in the sample of chronic pain patients (36) most similar to our study, only 3% of individuals fit the DE-LOC pattern. However, 55% of cancer patients were DE-LOC in the study by Frick et al (42). This would appear to confirm the conclusion drawn by all of the studies: the type of obtained clusters and the case distribution depend on the patient’s health status. Unlike the study by Frick et al (42), our sample consisted of patients experiencing headaches and chronic pain; therefore, the I-LOC is more likely. This may also explain the significant number of patients with BiC-LOC in our sample (31%), the highest percentage in all of the baseline studies.
The second aim of the present study was to validate the patterns of LOC. Our hypothesis was that three of the profiles (PI-LOC, BiC-LOC and PP-LOC) would show a better adjustment to pain than the other five (NS-LOC, YS-LOC, PC-LOC, DE-LOC and type VI-LOC). As expected based on scientific evidence (3,37,56), differences related to the sociodemographic variables were found among the LOC patterns: a younger individual with a higher education and greater per capita income was more likely to be classified as an internalist. Therefore, these variables were controlled before the analysis. Our hypothesis was partially correct: five of the 10 indicators analyzed showed statistically significant differences among the clusters. One was clinical (the frequency of pain) while the other four were psychological (automatic negative thoughts, perceived self-efficacy, maladaptive coping and pain behaviours). Three clinical indicators were almost high enough to be considered significant: pain intensity, pain interference and daily medication; in contrast, pain duration was not associated with a patient’s distribution in the clusters. The only nonsignificant psychological marker, adaptive coping, was also close to significance.
The profiles were arranged from best to worst adjustment to pain, resulting in the order PI-LOC, PP-LOC, BiC-LOC, NS-LOC, PC-LOC and YS-LOC. The first three (53%) showed a good adjustment to pain, while the last two (37%) displayed maladjustment to pain. Individuals with NS-LOC (10%) did not adjust as well as the top three, but did adjust better than the last two. To summarize, patients with PI-LOC, PP-LOC and BIC-LOC expressed less pain frequency, fewer negative automatic thoughts, less maladaptive coping, and fewer pain behaviours than patients with NS-LOC, PC-LOC and YS-LOC; in addition, they showed more adaptive coping and more perceived self-efficacy. These results are consistent with those obtained in other studies (36,39–42).
Wallston and Wallston (38) hypothesized that the BiC-LOC had the greatest adaptive potential in health, particularly among the chronically ill. Ozolins et al (41) highlighted the salutogenic properties of the BiC-LOC, which was superior to the other patterns. The results of our study with patients experiencing chronic pain did not coincide with these ideas: two pure profiles, the PI-LOC and the PP-LOC, were associated with a better adjustment to pain than the BIC-LOC. There is one possible and relatively simple explanation: when pain depends primarily on the patient or primarily on health professionals, it is easier to determine which aspects correspond to the patient and which correspond to health professionals. In fact, two other studies found that the PI-LOC presented the best adjustment to pain of all the patterns (36,40).
Wallston and Wallston (38) hypothesized that YS-LOC and NS-LOC could represent a response bias or be valid. In other words, health greatly depends on all of the factors, or does not depend on any of the factors, respectively. Our results appear to support the validity of the YS-LOC: this pattern was clearly maladaptive, as reported in other studies (40). One possible explanation for this result counters the explanation given for the PI-LOC: the complexity of the LOC can simply exceed an individual’s resources. However, in other studies, the YS-LOC was also associated with active coping styles (39,42). This may depend on the degree of perceived control, the health status or the demographic characteristics of the samples used.
A final unique feature of our results is that the PI-LOC, PP-LOC and BIC-LOC were clearly adaptive patterns, a finding that differed from that of other studies. For example, the PI-LOC has also been associated with self-blame (36), PP-LOC with worry (39,42), and BIC-LOC with depression and depressive coping (40).
In brief, our results support the empirical validity of the theoretical model of LOC patterns proposed by Wallston and Wallston (38) among a chronic pain population. On the one hand, the analysis of patterns provides more accurate information about the adjustment to pain than that of the LOC factors separately. On the other hand, the type of patterns found and the number of cases within each pattern appear to depend on the health status of the patients. The main limitation of the present study was its cross-sectional design, which makes it impossible to establish the directionality of the association between the LOC profiles and the psychological adjustment to chronic pain. Other studies have provided evidence that the LOC can act as both a predictor of long-term state of health (7), and as a moderating (14,25,26) and dependent (27–31) variable in treatments. In this respect, we believe that, in our study, the relationship between LOC profiles and psychological adjustment to chronic pain must be bidirectional in nature. However, neither our study nor any of the studies that have considered LOC profiles rather than separate scores have used a longitudinal or experimental methodology. Such a methodology could reveal how to best consider the LOC – whether as a predictor, a moderator or as the result of psychological adjustment to chronic pain. This challenge is an important one for future research in the field of chronic pain.
SUMMARY
LOC is related to the impact of headaches and chronic pain. However, the evidence is inconsistent, probably due to the interpretation of the factors (internal, chance and professional) separately. Wallston and Wallston (38) proposed eight possible patterns of health LOC by combining the scores in each of the three factors. We attempted to identify and validate these patterns in 228 Spanish patients with headaches and chronic pain, using a two-step cluster analysis and ANCOVA. We detected six of the eight proposed LOC patterns. No statistically significant differences were found in terms of sex, marital status or job status; however, factors such as age, per capita income and academic level did vary for the six patterns. Patients with PI-LOC, PP-LOC and BiC-LOC patterns claimed to have experienced lower pain frequency, fewer negative automatic thoughts, less maladaptive coping, fewer pain behaviours, more adaptive coping and more perceived self-efficacy than patients with nay-sayer, pure chance and yea-sayer patterns. Our results support the empirical validity of the theoretical model in a population of headaches and chronic pain, by improving information on adjustment to pain.
Acknowledgments
This manuscript would not have been possible without the disinterested cooperation of both health care professionals and patients treated at public health centres, which was the result of scientific and technical cooperation agreements with the University Hospital “Virgen del Rocío” and with the South District of Primary Care of Seville (Spain). The authors also acknowledge the assistance of Dr Wallston in reviewing and improving the original manuscript.
Footnotes
DISCLOSURES: The study was not funded by any grant. The authors have no conflicts of interest to declare.
REFERENCES
- 1.Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80:1–28. [PubMed] [Google Scholar]
- 2.Levenson H. Activism and powerful others: Distinctions within the concept of internal-external control. J Pers Assess. 1974;38:377–83. [Google Scholar]
- 3.Wallston KA. Conceptualization and operationalization of perceived control. In: Baum A, Revenson T, Singer JE, editors. The Handbook of Health Psychology. Mahwah: Erlbaum; 2001. pp. 49–58. [Google Scholar]
- 4.Wallston BS, Wallston KA, Kaplan GD, Maides SA. Development and validation of the Health Locus of Control (HLC) Scale. J Consult Clin Psychol. 1976;44:580–5. doi: 10.1037//0022-006x.44.4.580. [DOI] [PubMed] [Google Scholar]
- 5.Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr. 1978;6:160–70. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- 6.Wallston KA, Stein MJ, Smith CA. Form C of the MHLC scales: A condition-specific measure of locus of control. J Pers Assess. 1994;63:534–53. doi: 10.1207/s15327752jpa6303_10. [DOI] [PubMed] [Google Scholar]
- 7.Gale CR, Batty G, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: The 1970 British Cohort Study. Psychosom Med. 2008;70:397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- 8.Trafimow D, Trafimow J-H. Predicting back pain sufferers’ intentions to exercise. J Psychol. 1998;132:581–92. doi: 10.1080/00223989809599291. [DOI] [PubMed] [Google Scholar]
- 9.Conant LL. Psychological variables associated with pain perceptions among individuals with chronic spinal cord injury pain. J Clin Psychol Med Settings. 1998;5:71–90. [Google Scholar]
- 10.Zaharoff AD. The relationship between fibromyalgia and emotional expressivity and its influence on locus of control, ways of coping, and quality of life. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2005;65(8-B) [Google Scholar]
- 11.Cheng SK, Leung F. Catastrophizing, locus of control, pain, and disability in Chinese chronic low back pain patients. Psychol Health. 2000;15:721–30. [Google Scholar]
- 12.Worsham SL. The effects of perceived locus of control and dispositional optimism on chronic pain treatment outcomes. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2005;65(12-B):6639. [Google Scholar]
- 13.Melding PS. How do older people respond to chronic pain? A review of coping with pain and illness in elders. Pain Rev. 1995;2:65–75. [Google Scholar]
- 14.Harkapaa K. Relationships of psychological distress and health locus of control beliefs with the use of cognitive and behavioral coping strategies in low back pain patients. Clin J Pain. 1991;7:275–82. [PubMed] [Google Scholar]
- 15.Fisher K, Johnston M. Emotional distress and control cognitions as mediators of the impact of chronic pain on disability. Br J Health Psychol. 1998;3:225–36. [Google Scholar]
- 16.Haldorsen EM, Indahl A, Ursin H. Patients with low back pain not returning to work. A 12-month follow-up study. Spine. 1998;23:1202–7. doi: 10.1097/00007632-199806010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Selander J, Marnetoft SU, Asell M. Predictors for successful vocational rehabilitation for clients with back pain problems. Disabil Rehabil. 2007;29:215–20. doi: 10.1080/09638280600756208. [DOI] [PubMed] [Google Scholar]
- 18.Pastor MA, Salas E, Lopez S, Rodriguez J, Sanchez S, Pascual E. Patients’ beliefs about their lack of pain control in primary fibromyalgia syndrome. Br J Rheumatol. 1993;32:484–9. doi: 10.1093/rheumatology/32.6.484. [DOI] [PubMed] [Google Scholar]
- 19.Scharff L, Turk DC, Marcus DA. The relationship of locus of control and psychosocial-behavioral response in chronic headache. Headache. 1995;35:527–33. doi: 10.1111/j.1526-4610.1995.hed3509527.x. [DOI] [PubMed] [Google Scholar]
- 20.Mackenbach JP, Borsboom GJ, Nusselder WJ, Looman CW, Schrijvers CT. Determinants of levels and changes of physical functioning in chronically ill persons: Results from the GLOBE Study. J Epidemiol Community Health. 2001;55:631–8. doi: 10.1136/jech.55.9.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Primavera JP, Kaiser RS. The relationship between locus of control, amount of preadmission analgesic/ergot overuse, and length of stay for patients admitted for inpatient treatment of chronic headache. Headache. 1994;34:204–8. doi: 10.1111/j.1526-4610.1994.hed3404204.x. [DOI] [PubMed] [Google Scholar]
- 22.Roome P, Humphrey M. Personality factors in analgesic usage. Stress Med. 1992;8:237–40. [Google Scholar]
- 23.Murphy JP. Partners in pain: The relationship between spousal locus-of-control and chronic pain patients’ coping behavior. Dissertation Abstracts International Section A: Humanities and Social Sciences. 1994;55(4-A) [Google Scholar]
- 24.Hadjistavropoulos H, Shymkiw J. Predicting readiness to self-manage pain. Clin J Pain. 2007;23:259–66. doi: 10.1097/AJP.0b013e31802f67f3. [DOI] [PubMed] [Google Scholar]
- 25.Lake AE., 3rd Behavioral and nonpharmacologic treatments of headache. Med Clin North Am. 2001;85:1055–75. doi: 10.1016/s0025-7125(05)70359-x. [DOI] [PubMed] [Google Scholar]
- 26.Harkapaa K, Jarvikoski A, Estlander AM. Health optimism and control beliefs as predictors for treatment outcome of a multimodal back treatment program. Psychol Health. 1996;12:123–34. [Google Scholar]
- 27.James FR, Large RG, Beale IL. Self-hypnosis in chronic pain. A multiple baseline study of five highly hypnotisable subjects. Clin J Pain. 1989;5:161–8. doi: 10.1097/00002508-198906000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Jay GW, Brunson J, Branson SJ. The effectiveness of physical therapy in the treatment of chronic daily headaches. Headache. 1989;29:156–62. doi: 10.1111/j.1526-4610.1989.hed2903156.x. [DOI] [PubMed] [Google Scholar]
- 29.Lipchik GL, Milles K, Covington EC. The effects of multidisciplinary pain management treatment on locus of control and pain beliefs in chronic non-terminal pain. Clin J Pain. 1993;9:49–57. doi: 10.1097/00002508-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Coughlin AM, Badura AS, Fleischer TD, Guck TP. Multidisciplinary treatment of chronic pain patients: Its efficacy in changing patient locus of control. Arch Phys Med Rehabil. 2000;81:739–40. doi: 10.1016/s0003-9993(00)90103-5. [DOI] [PubMed] [Google Scholar]
- 31.Biurrun-Unzue A, Fernandez-Cuadrado MV, Jusue-Erro G. Efectos de la aplicacion de un programa de tratamiento cognitivo-conductual en el locus de control de pacientes con dolor cronico / Effects of the application of a cognitive-behavioural treatment on locus of control in chronic pain patients. Anales de Psiquiatria. 2002;18:407–10. [Google Scholar]
- 32.Seville JL, Robinson AB. Locus of control in the patient with chronic pain. In: Gatchel RJ, Weisberg JN, editors. Personality characteristics of patients with pain. Washington: American Psychological Association; 2000. pp. 165–79. [Google Scholar]
- 33.Allen LL, Haririfar M, Cohen J, Henderson MJ. Quality of life and locus of control of migraineurs. Clin Excell Nurse Pract. 2000;4:41–9. [PubMed] [Google Scholar]
- 34.Hurwitz EL, Goldstein MS, Morgenstern H, Chiang L-M. The impact of psychosocial factors on neck pain and disability outcomes among primary care patients: Results from the UCLA Neck Pain Study. Disabil Rehabil. 2006;28:1319–29. doi: 10.1080/09638280600641509. [DOI] [PubMed] [Google Scholar]
- 35.Lampl C, Heuberger B, Haas S, Yazdi K, Buzath A, Kemetzhofer P. Relationship of locus of control in women with migraine and healthy volunteers. Headache. 2003;43:878–83. doi: 10.1046/j.1526-4610.2003.03166.x. [DOI] [PubMed] [Google Scholar]
- 36.Buckelew SP, Shutty MS, Hewett J, Landon T, Morrow K, Frank RG. Health locus of control, gender differences and adjustment to persistent pain. Pain. 1990;42:287–94. doi: 10.1016/0304-3959(90)91141-5. [DOI] [PubMed] [Google Scholar]
- 37.Fournier G, Jeanrie C. Positive psychological assessment: A handbook of models and measures. Washington: American Psychological Association; 2003. Locus of control: Back to basics; pp. 139–54. [Google Scholar]
- 38.Wallston KA, Wallston BS. Who is responsible for your health? The construct of health locus of control. In: Sanders G, Suls J, editors. Social Psychology of Health and Illness. Hillsdale: Erlbaum; 1982. pp. 65–95. [Google Scholar]
- 39.Rock DL, Meyerowitz BE, Maisto SA, Wallston KA. The derivation and validation of six Multidimensional Health Locus of Control Scale clusters. Res Nurs Health. 1987;10:185–95. doi: 10.1002/nur.4770100311. [DOI] [PubMed] [Google Scholar]
- 40.Raja SN, Williams S, McGee R. Multidimensional health locus of control beliefs and psychological health for a sample of mothers. Soc Sci Med. 1994;39:213–20. doi: 10.1016/0277-9536(94)90330-1. [DOI] [PubMed] [Google Scholar]
- 41.Ozolins AR, Stenstrom U. Validation of health locus of control patterns in Swedish adolescents. Adolescence. 2003;38:651–7. [PubMed] [Google Scholar]
- 42.Frick E, Fegg M, Tyroller M, Fischer N, Bumeder I. Patients’ health beliefs and coping prior to autologous peripheral stem cell transplantation. Eur J Cancer Care. 2007;16:156–63. doi: 10.1111/j.1365-2354.2006.00725.x. [DOI] [PubMed] [Google Scholar]
- 43.Cano-García FJ. Departamento de Personalidad, Evaluación y Tratamiento Psicológicos. Sevilla: Universidad de Sevilla; 2007. Variables psicológicas implicadas en migraña y cefalea tensional Un estudio comparativo con otros trastornos por dolor crónico. < http://fondosdigitales.us.es/tesis/tesis/602/variables-psicologicas-implicadas-en-migrana-y-cefalea-tensional-un-estudio-comparativo-con-otros-trastornos-por-dolor-cronico/> (Accessed January 10, 2013). [Google Scholar]
- 44.WMA Declaration of Helsinki. Ethical principles for medical research involving human subjects. J Indian Med Assoc. 2009;107:403–5. [PubMed] [Google Scholar]
- 45.Charlton E. Ethical guidelines for pain research in humans. Committee on Ethical Issues of the International Association for the Study of Pain. Pain. 1995;63:277–8. doi: 10.1016/0304-3959(95)90040-3. [DOI] [PubMed] [Google Scholar]
- 46.Martin NJ, Holroyd KA, Penzien DB. The Headache-Specific Locus of Control Scale: Adaptation to recurrent headaches. Headache. 1990;30:729–34. doi: 10.1111/j.1526-4610.1990.hed3011729.x. [DOI] [PubMed] [Google Scholar]
- 47.Wallston KA. Multidimensional Health Locus of Control (MHLC) Scales. 2009. < www.vanderbilt.edu/nursing/kwallston/mhlcscales.htm> (Accessed on December 15, 2009). [DOI] [PubMed]
- 48.VandeCreek L, O’Donnell F. Psychometric characteristics of the Headache-Specific Locus of Control scale. Headache. 1992;32:239–41. doi: 10.1111/j.1526-4610.1992.hed3205239.x. [DOI] [PubMed] [Google Scholar]
- 49.Gil KM, Williams DA, Keefe FJ, Beckham JC. The relationship of negative thoughts to pain and psychological distress. Behav Ther. 1990;21:349–62. [Google Scholar]
- 50.Cano García FJ, Rodríguez Franco L. Pensamientos automáticos negativos en el dolor crónico. Psiquis. 2003;24:9. [Google Scholar]
- 51.Rosenstiel AK, Keefe FJ. The use of cognitive coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 52.Rodríguez Franco L, Cano-García FJ, Blanco Picabia A. Assessment of chronic pain strategies. Actas Españolas de Psiquiatría. 2004;32:29–39. [PubMed] [Google Scholar]
- 53.Appelbaum KA, Radnitz CL, Blanchard EB, Prins A. The Pain Behavior Questionnaire (PBQ): A global report of pain behavior inchronic headache. Headache. 1988;28:53–8. doi: 10.1111/j.1365-2524.1988.hed2801053.x. [DOI] [PubMed] [Google Scholar]
- 54.Rodríguez-Franco L, Cano-García FJ, Blanco-Picabia A. Conductas de dolor y discapacidad en migrañas y cefaleas tensionales. Adaptación española del Pain Behavior Questionnaire (PBQ) y del Headache Disability Inventory (HDI) Análisis y Modificación de Conducta. 2000;26:729–62. [Google Scholar]
- 55.Martin NJ, Holroyd KA, Rokicki LA. The Headache Self-Efficacy Scale: Adaptation to recurrent headaches. Headache. 1993;33:244–8. doi: 10.1111/j.1526-4610.1993.hed3305244.x. [DOI] [PubMed] [Google Scholar]
- 56.Wallston BS, Wallston KA. Locus of control and health: A review of the literature. Health Educ Monogr. 1978;6:107–17. doi: 10.1177/109019817800600102. [DOI] [PubMed] [Google Scholar]


