Abstract
Objective
The objective of this study was to evaluate the relationship between self reported cost-related nonadherence to medications and emergency department utilization among a population of Medicare beneficiaries. We hypothesized that persons who reported cost-related medication nonadherence (CRN) would have higher emergency department (ED) use.
Methods
We conducted a retrospective cohort study of continuously enrolled Medicare beneficiaries from in 2006 and 2007. We used multivariate logistic regression to evaluate the relationship between ED use and CRN. Our principal dependent variable was any emergency department visit within a 364-day period after the initial interview assessing CRN. Our principal independent variables were two variables to denote CRN: mild CRN, defined as a reduction in medication dose or delay in getting medications because of cost, and severe CRN, defined as a medication not being filled at all due to cost.
Results
Our sample consisted of 7177 Medicare Cost Beneficiary Survey (MCBS) MCBS respondents. Approximately 7.5 percent of these respondents reported mild CRN only (n=541) and another 8.2 percent reported severe CRN (n=581). Disabled Medicare beneficiaries with severe CRN were more likely to have at least one ED visit (1.53, 95% CI 1.03–2.26) as compared to both disabled Medicare beneficiaries without CRN and elderly Medicare beneficiaries in all CRN categories.
Conclusions
Our results show an association between severe CRN and emergency department use. Disabled beneficiaries under age 65 who report severe CRN were more likely to have at least one emergency department visit, even when adjusting for other factors that impact utilization.
Introduction
Background
Prescription drugs represent one of the highest out of pocket (OOP) health care costs for American consumers accounting for over $48 million dollars spent annually.1 Approximately 187 million adults currently take at least one prescription medication. Medication needs are greatest for the elderly and patients with major medical conditions. Medicare enrollees over age 65 fill an average of over six unique prescriptions each year. 2 Non-elderly Medicare disabled beneficiaries fill 40% more prescriptions and have significantly higher out of pocket spending than the average Medicare enrollee.3–5 Despite the substantial need for medications, a large percentage of older and disabled adults have inadequate drug coverage and often report high rates of nonadherence due to cost-related concerns.6 This high rate of nonadheraence in turn has been estimated to account for over 100 million dollars in spending due to avoidable hospitalizations.7
Since the implementation of Medicare Part D in 2006, significant improvements in pharmaceutical coverage for the elderly and disabled have occurred. 8–12 However, despite improvements in coverage and associated declines in out-of-pocket spending, 11% of Medicare beneficiaries continue to report skipping doses, splitting pills, or not filling medications due to cost. The prevalence of cost-related nonadherence (CRN) among adults with poor health status is about 20% even in the era of Part D.13
Importance
CRN has been linked to a decline in health status and poor health outcomes, such as a worsening of symptoms among patients with hypertension or diabetes.14,15 Patients with chronic disease who are non-compliant with essential medications have higher rates of hospitalization and mortality than those who have high levels of compliance.16–18 For example, patients who have suffered from acute myocardial infarction (MI) and who are nonadherent to recommended post-MI medication regimens have higher one year mortality rates compared with adherent patients.18,20
Less is known about how cost-related medication nonadherence specifically affects emergency department (ED) use. Emergency department visits could theoretically increase as a consequence of CRN due to complications associated with not taking medications, or when patients visit the ED to obtain prescription medications they cannot afford.
Objective of this Investigation
The objective of this study was to evaluate the relationship between cost-related medication nonadherence and subsequent emergency department utilization among a nationally representative population of Medicare beneficiaries in a period after implementation of Medicare Part D. We hypothesized that persons who reported cost-related medication nonadherence would be more likely to have at least one emergency department visit and would have a higher total mean number of emergency department visits compared with persons without CRN.
Methods
Study Design
We conducted a retrospective cohort study of continuously-enrolled Medicare beneficiaries in 2006 and 2007.
Data Collection and Processing
We merged the 2006 and 2007 Medicare Current Beneficiary Survey (MCBS) Access to Care files with Medicare inpatient and outpatient claims for survey respondents for the same years. The Medicare Current Beneficiary Survey is a longitudinal survey administered annually by the Centers for Medicare and Medicaid Services to a nationally representative sample of approximately 12,000 elderly and disabled Medicare beneficiaries. The MCBS uses a rotating sample design, with 4 panels of participants interviewed each year. The initial interview each year occurs in the fall at which time panel members are queried about demographics, health status, utilization and measures related to cost-related medication adherence.21 The survey data can be linked to Medicare fee-for-service claims files providing additional information about medical service utilization.22
We restricted our sample to non-institutionalized beneficiaries who were continuously enrolled in Medicare Parts A and B (traditional fee-for service) for 12 months after their annual fall survey date and who participated in the 2006 and 2007 waves of MCBS. We excluded Medicare Advantage enrollees because of incomplete claims data for this population, which in 2006 made up 18% of Medicare beneficiaries nationwide.23 We included health care claims up to 364 days after the date on which fall survey data, including self-reported CRN, were collected.
Outcomes
Our principal outcome of interest was any emergency department visit resulting in either discharge or hospitalization identified through the Medicare inpatient or outpatient claims file within a 364 day period after the fall interview assessing CRN. Our secondary outcome was the number of distinct ED visits during this same period. The reliability of claims-based measures of ED visits has been well documented.24,25
Our principal independent variable, cost-related medication nonadherence, was developed from previously validated measures used in a number of prior studies.26–28 Starting in 2006, CRN measures in the MCBS were more complete, particularly with respect to not filling prescriptions and delaying fills. 26,–28 In the present analyses, we included two variables to denote cost-related medication nonadherence. One was mild CRN, defined as a positive response to any of the following behaviors in the prior year: (1) “skipped doses to make the medicine last longer”; (2) “taken smaller doses of a medicine to make the medicine last longer”, and, (3) “delayed getting medicines because of cost.”
The second variable, severe cost-related nonadherence, was defined as a positive response to the following survey questions: (1) “were any medicines prescribed for you that you did not get” because “you thought it would cost too much” or (2) “decide not to fill or refill a prescription because it was too expensive.”
The two CRN categories were mutually exclusive. Although persons with severe CRN could have also skipped or delayed medicines, all of the individuals in this group reported not getting medicines or not filling prescriptions due to cost. Similarly, none of the mild CRN group reported not getting medicines or not filling prescriptions due to cost. We compared both groups to those without any reported CRN.
Statistical Analyses
We used both univariate and multivariate analyses to examine the relationship between ED visits and CRN, adjusting for demographic, health-related, SES, and ethnicity variables that have been shown to impact CRN26–29 and that could also affect utilization.29–33 These included: race/ethnicity (non-Hispanic black, Hispanic, other race, non-Hispanic white), number of comorbid medical conditions, (a count of any one of the following: coronary artery disease, congestive heart failure, diabetes, copd/asthma, cerebrovascular accident, hypertension, cancer, dementia, arthritis, mental illness, and other neurologic conditions--grouped into 0–1 comorbidities, 2–3 comorbidities and 4 or more comorbidities), self-reported health status (excellent, very good or good combined as compared to fair or poor), age category (≤64, 65–74, 75–84,≥85 years), education (less than high school as compared to high school graduate or more), income (≤$25,000 a year,>$25,000 a year), gender, identification of a usual site of care (defined as having one or more sites other than an emergency department or walk-in urgent care center where care is regularly sought versus no identifiable site), limitations in activities of daily living (0 limitations, 1–2 limitations and 3 or more limitations, constructed from a 6-item scale)32, and metropolitan versus rural residence. We also controlled for prescription drug coverage grouped in the following categories: employer based coverage including retiree coverage and Tricare, Medicaid Part D coverage, Low-Income Subsidy (LIS) Part D coverage (including partial subsidy at any level), no prescription drug coverage(including prescription drug discount cards with no other identified source of coverage) and other coverage. The other coverage group includes other Part D coverage (including private stand alone prescription drug plans), supplementary prescription drug assistance from State Pharmaceutical Assistance Programs (SPAP), Veterans Administration coverage (excluding Tricare), and all other coverage categories. The Medicaid and LIS Part D categories were combined in our multivariate analysis. All variables were self reported except for age and gender, which were taken from administrative files. The drug coverage variable was formed from a combination of self-report and administrative files. Missing values for income were imputed by CMS using data from prior rounds.34 Data were missing for less than 1.5% of all other observations and were excluded from our multivariate analysis. Missing data was not correlated with any one outcome and there was no significant difference in coefficients in our independent variables of interest using deletion versus handling missing data with other imputation methods.35
We used multivariate logistic regression analysis to evaluate the relationship between all categories of CRN and at least one ED visit. Because most individuals in the sample had no ED visits, we used multivariate Poisson regression analysis to investigate the relationship between the total number of ED visits and CRN. We examined a number of interaction terms (CRN categories interacted with age, income, and chronic disease) to examine the combined effect of CRN with demographic, socioeconomic, and clinical factors. We also explored other covariates including self reported depressive symptoms (among persons who did not report a diagnosis of depression or other mental health conditions) 36,38 and found that they did not significantly alter the coefficients of our independent variables of interest. Our threshold for inclusion in our final model was a p value of <0.05 associated with our interaction terms. Our final models included an interaction between CRN and age-based eligibility categories (age 64 and under identified disabled beneficiaries, age 65–74, 75–84 and 85 and over). Our interaction terms on the elderly’s individual age categories were insignificant and we therefore present effects on this group combined (≥age 65). The interaction between being disabled and CRN was significant; we hypothesized that this indicated that ED utilization is modulated by CRN in a different way among the disabled than among the elderly; this supports prior evidence of significant differences in utilization patterns among these two populations.39
In order to more clearly demonstrate the association of CRN with ED visits among the entire group as well as in specific sub-populations, we estimated predicted probabilities of our outcomes using our fitted models and constructed 95% confidence intervals around these probabilities40,41 The predicted probabilities allow us to estimate ED use for the average person in each category of CRN, for our total population as well as for the subpopulations of non-elderly disabled and elderly. To do this, we used the average values for our covariates and set the CRN and age coefficients to 0 or 1 depending on the predicted category. 40,41
Data were analyzed using STATA version 11 (StataCorp LP, College Station, Texas). Our analyses were weighted to reflect the general U.S. population of Medicare beneficiaries using survey weights provided with the MCBS Access to Care data. Although there have been a number of approaches used in applying weights to multi-year MCBS data, we used 2007 one year backward longitudinal survey weights (designed for analysis going one year backward over time in two consecutive years) as our data crossed 2006 and 2007.42, 43 The study was approved by the Harvard Pilgrim Health Care and George Washington University Institutional Review Boards.
Results
Characteristics of Study Subjects
Our sample consisted of 7177 MCBS respondents in both the 2006 and 2007 survey panels who were community dwelling and continuously enrolled in Medicare Parts A and B for at least 12 months following their fall 2006 interview. Approximately 7.5 percent of respondents in the study sample reported mild CRN only (n=541) and another 8.2 percent reported severe CRN (n=581). Characteristics of our sample are shown in Table 1.
Table 1.
Baseline demographic, SES and health characteristics of study sample by self-reported cost-related nonadherence status in 2006, (n=7177)*
| Cost-related nonadherence | ||||||
|---|---|---|---|---|---|---|
| No CRN (n=6055) | Mild CRN (n=541) | Severe CRN (n=581) | ||||
| % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| Race/Ethnicity* | ||||||
| Black (n=673) | 524 | 76.3 (71.8–80.7) | 54 | 8.7 (5.7–11.6) | 95 | 15.1 (10.9–19.3) |
| Other race(excluding white) (n=314) | 262 | 82.3 (75.5–89.0) | 21 | 6.0 (2.8–9.1) | 31 | 11.7 (5.2–18.3) |
| White (n=6185)** | 5265 | 85.3 (84.3–86.3) | 465 | 7.4 (6.6–8.2) | 455 | 7.3 (6.6–8.0) |
| Ethnicity | ||||||
| Hispanic (n=393) | 334 | 83.9 (77.5–90.3) | 19 | 4.7 (1.5–8.0) | 40 | 11.3 (6.5–16.2) |
| Non-Hispanic (n=6784)** | 5721 | 84.4 (83.4–85.4) | 522 | 7.6 (6.9–8.3) | 541 | 8.0 (7.2–8.8) |
| Number of chronic conditions*** | ||||||
| 4 or more (n=1931) | 1521 | 77.8 (75.6–79.9) | 181 | 9.9 (8.4–11.4) | 229 | 12.3 (10.6–14.1) |
| 2–3 (n=3412) | 2899 | 85.3 (84.0–86.6) | 257 | 7.3 (6.2–8.4) | 256 | 7.4 (6.4–8.4) |
| 0–1 (n=1834)** | 1635 | 89.7 (88.0–91.4) | 103 | 5.2 (4.0–6.3) | 96 | 5.1 (3.9–6.4) |
| Self reported health status* | ||||||
| Fair or Poor (n=1844) | 1337 | 72.4 (69.9–74.9) | 215 | 11.8 (10.2–13.4) | 292 | 15.8 (13.9–17.7) |
| Excellent, very good or good (n=5304)** | 4693 | 88.4 (87.3–89.4) | 325 | 6.0 (5.2–6.9) | 286 | 5.6 (4.8–6.4) |
| Education* | ||||||
| Did not complete high school (n=1952) | 1607 | 81.9 (79.8–83.9) | 153 | 7.9 (6.8–8.9) | 192 | 10.3 (8.4–12.2) |
| High school or more (n=5187)** | 4415 | 85.2 (84.1–86.4) | 384 | 7.3 (6.4–8.2) | 388 | 7.5 (6.6–8.3) |
| Income | ||||||
| Annual income ≤$25K (n=4040) | 3250 | 80.4 (78.9–81.9) | 347 | 8.4 (7.3–9.4) | 443 | 11.2 (10.0–12.4) |
| Annual income >25K (n=3137)** | 2805 | 88.8 (87.4–90.3) | 194 | 6.4 (5.4–7.5) | 138 | 4.7 (3.8–5.6) |
| Gender | ||||||
| Male (n=3217) | 2733 | 85.1 (83.7–86.5) | 239 | 7.4 (6.4–8.4) | 245 | 7.5 (6.3–8.7) |
| Female (n=3960)** | 3322 | 83.8 (82.5–85.1) | 302 | 7.5 (6.4–8.6) | 336 | 8.7 (7.7–9.7) |
| Primary Care Provider | ||||||
| Presence of a regular provider (n=6762) | 5704 | 84.2 (83.1–85.2) | 519 | 7.7 (6.9–8.5) | 539 | 8.2 (7.4–8.9) |
| No regular provider identified (n=415)** | 351 | 87.5 (83.1–91.8) | 22 | 4.1 (1.9–6.3) | 42 | 8.5 (4.8–12.1) |
| Prescription Drug Coverage**** | ||||||
| Medicaid Part D (n=1476) | 1148 | 78.4 (75.2–81.7) | 143 | 9.1 (7.3–11.0) | 185 | 12.4 (10.0–14.9) |
| LIS Part D (excludes Medicaid) (n=343) | 226 | 65.4 (58.2–72.6) | 46 | 14.3 (8.6–20.1) | 71 | 20.3 (13.6–27.0) |
| No prescription drug coverage (n=1245) | 1056 | 84.2 (81.7–86.6) | 73 | 6.3 (4.7–7.9) | 116 | 9.5 (7.5–11.5) |
| Other Coverage (n=1449) | 1210 | 82.6 (80.0–85.2) | 119 | 8.2 (6.4–10.0) | 120 | 9.2 (7.3–11.2) |
| Employer Sponsored/Tricare (n=2664)** | 2415 | 90.3 (89.0–91.7) | 160 | 6.1 (4.8–7.3) | 89 | 3.6 (2.8–4.4) |
| Residence | ||||||
| Metro (n=4908) | 4231 | 86.1 (84.9–87.3) | 317 | 6.4 (5.5–7.4) | 360 | 7.5 (6.5–8.4) |
| Non-metro (n=2269)** | 1824 | 80.0 (76.9–83.1) | 224 | 10.1 (8.2–12.0) | 221 | 9.9 (8.0–11.8) |
| Restrictions in ADLs | ||||||
| 3 or more (n=671) | 510 | 74.5 (69.6–79.4) | 67 | 11.0 (7.3–14.6) | 94 | 14.6 (10.5–18.6) |
| 1–2 (n=1498) | 1184 | 78.3 (76.1–80.6) | 156 | 11.0 (9.1–12.9) | 158 | 10.6 (9.0–12.3) |
| None (n-5008)** | 4361 | 87.3 (86.2–88.4) | 318 | 6.0 (5.2–6.8) | 329 | 6.7 (5.9–7.5) |
| Age Category | ||||||
| Non-Elderly/Disabled | ||||||
| Age ≤64 (n=1349) | 905 | 64.9 (61.5–68.3) | 166 | 12.6 (10.2–14.9) | 278 | 22.6 (19.6–25.5) |
| Elderly | ||||||
| Age 65–74 (n=2489) | 2126 | 85.6 (84.2–87.0) | 188 | 7.4 (6.1–8.7) | 175 | 7.0 (6.1–7.9) |
| Age 75–84 (n=2449) | 2199 | 89.9 (88.6–91.1) | 149 | 6.0 (5.1–7.0) | 101 | 4.1(3.2–5.0) |
| Age ≥85 (n=890)** | 825 | 92.8 (90.7–94.9) | 38 | 4.1 (2.5–5.8) | 27 | 3.1 (1.8–4.4) |
Includes missing data. Data missing <1.5% of total sample. Data missing for 0.07% of race, 0.4% of self reported health status and 0.4% of education.
Reference group. Bolded values indicate significant difference at 95% confidence interval as compared to reference group in each category.
Chronic conditions include coronary artery disease, congestive heart failure, diabetes mellitus, copd,/asthma, cerebrovascular accident, hypertension, cancer, dementia, arthritis, mental illness and other neurologic diseases.
Medicaid Part D and Low Income Supplement Part D includes coverage for at least part of year. LIS Part D includes subsidies at any level (including partial) but excludes Medicaid.. Other coverage includes all other part D private stand alone prescription drug plans, excluding Medicaid Part D and LIS Part D plans, and all other categories including State Pharmaceutical Assistance Program and Veterans Assistance coverage (other than TRICARE). No coverage includes prescription drug discount cards if no other coverage source identified.
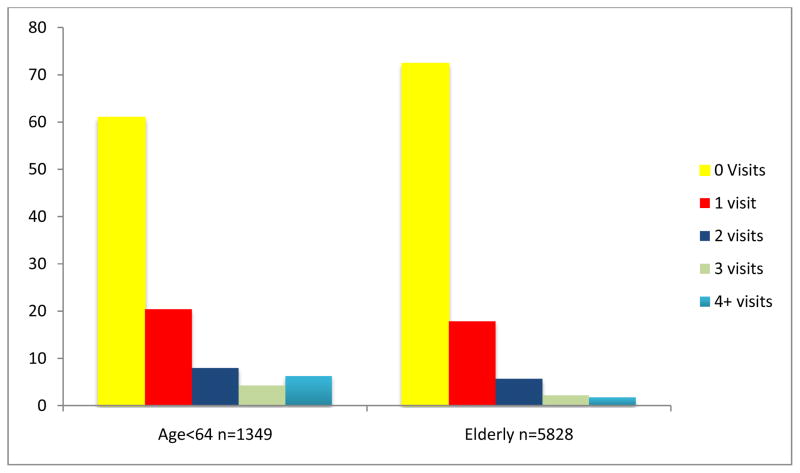
As expected, Blacks, persons with 4 or more comorbid medical conditions, fair/poor self-reported health status, lower education levels, lower incomes, one or more restrictions in ADLs, individuals who were in the age 64 and under disabled eligibility category and individuals aged 65 to 74 were more likely to report severe CRN. Persons with Medicaid Part D, LIS Part D, no prescription drug or other coverage were also more likely to have severe CRN than persons with employer sponsored coverage or Tricare. (All values significant at the 95% confidence level). Figure 1 shows the number of ED visits by age category. Thirty nine percent of disabled individuals and just under 27% of elderly individuals had at least one visit during the 364 day period after the interview. The number of visits were largely skewed towards 1, with 20% of disabled and 18% of elderly respondents reporting one visit. In contrast, just seven percent of disabled individuals had 4 or more visits as compared to less than 2% of non-elderly individuals.
Figure 1. Percentage of persons with 0, 1, 2, 3, and 4 or more visits, by age and eligibility categories*.
* Weighted to National Medicare Population, includes missing observations.
Main Results
Medicare beneficiaries reporting severe CRN in 2006 were more likely than those without CRN to have at least one emergency department visit and they also had a higher average number of ED visits within the 364 day time period following the interview (unadjusted). Approximately 39.3% (95% CI 32.5%–46.2%) of individuals with severe CRN had at least one emergency department visit as compared to only 28.7% (95%CI 27.4%–29.9%) of persons with no CRN; this group had an average of 0.84 ED visits (95%CI 0.64–1.05) as compared to 0.50 ED visits (95%CI 0.47–0.54) among the no CRN group. The percentage of people (28.0%, 95%CI 23.2%– 32.9%) with mild CRN who had at least one ED visit was not statistically different from those with no CRN, nor was the mean number of visits (0.52, 95%CI 0.38–0.67).
Table 2 shows the relationship between utilization and CRN adjusting for race, number of comorbid medical conditions, self-reported health status, education, income, gender, identification of a usual site of care, limitations in activities of daily living, metropolitan residence, prescription drug coverage and age (n=7105, excludes missing observations). Although our final model includes all age categories and interaction terms, we also show both the odds ratios (OR), derived from the logistic regression analyses, and the incidence rate ratios (IRR), from the Poisson regression analyses, separately for the disabled and the elderly. As compared to the disabled without CRN, disabled individuals with severe CRN had a 1.53 greater odds of any ED visit (95% CI 1.03–2.26). Other covariates significantly associated with having any ED visit in our adjusted analysis included having 2–3 comorbidities or 4 or more comorbidities, fair or poor self reported health status, annual Medicaid Part D or LIS Part D coverage and 3 or more restrictions in ADLs (see Table 2).
Table 2.
Adjusted Odds Ratios and Incident Rate Ratios: Any ED visit and average number of ED visits*, (n=7105)
| Any ED visit: Odds Ratio (95% C.I.) | Number of ED visits: Incidence Rate Ratio (95% C.I.) | |
|---|---|---|
| Cost-related Nonadherence | ||
| Non-Elderly/Disabled, (n=1328) | ||
| Mild CRN only | 0.61 (0.37–1.01) | 0.85 (0.51–1.42) |
| Severe CRN | 1.53 (1.03–2.26) | 1.23 (0.90–1.66) |
| No CRN | reference | reference |
| Elderly (n=5777) | ||
| Mild CRN only | 0.82 (0.63–1.06) | 0.77 (0.61–0.98) |
| Severe CRN | 0.91(0.66–1.25) | 0.92 (0.70–1.20) |
| No CRN | reference | reference |
| Other Covariates | ||
| Race | ||
| Black | 1.06 (0.84–1.34) | 0.99 (0.82–1.19) |
| White/other race | Reference | Reference |
| Ethnicity | ||
| Hispanic | 0.91 (0.79–1.05) | 1.00 (0.88–1.15) |
| Non-Hispanic | Reference | Reference |
| Number of chronic conditions* | ||
| 4 or more | 2.29 (1.83–2.87) | 2.18 (1.77–2.69) |
| 2–3 | 1.45 (1.21–1.73) | 1.47 (1.22–1.78) |
| 0 | Reference | Reference |
| Self reported health status | ||
| Fair or Poor | 1.34 (1.17–1.53) | 1.32 (1.14–1.53) |
| Excellent- very good or good | Reference | Reference |
| Education | ||
| Did not complete high school | 1.03 (0.90–1.18) | 0.89 (0.80– 1.00) |
| High school or more | Reference | Reference |
| Income | ||
| Annual income ≤$25K | 1.06 (0.94–1.20) | 1.28 (1.14–1.45) |
| Annual income >25K | Reference | Reference |
| Gender | ||
| Male | 0.98 (0.88–1.09) | 1.04 (0.94–1.16) |
| Female | Reference | Reference |
| Primary Care Provider | ||
| Presence of a regular provider | 0.95 (0.71–1.29) | 0.96 (0.78–1.20) |
| None regular provider identified | Reference | Reference |
| Prescription Drug Coverage** | ||
| Medicaid/LIS Part D | 1.30 (1.09–1.55) | 1.39 (1.16– 1.68) |
| No prescription drug coverage | 0.87 (0.75–1.02) | 0.84 (0.71– 0.99) |
| Other Prescription Drug Coverage | 0.97 (0.84–1.12) | 0.96 (0.84– 1.10) |
| Employer Sponsored/Tricare | Reference | Reference |
| Residence | ||
| Metro | 0.92 (0.80–1.07) | 0.96(0.84–1.09) |
| Non-metro | Reference | Reference |
| Restrictions in ADLs | ||
| 3 or more | 1.28 (1.01– 1.64) | 1.11 (0.93–1.34) |
| 1–2 | 1.16 (0.99– 1.35) | 1.04 (0.90–1.20) |
| None | Reference | Reference |
Disabled individuals with CRN also had a 1.23 higher incidence rate ratio (IRR) of number of ED visits as compared to the disabled without CRN, though not statistically significant (95% CI 0.90–1.66). In contrast, the elderly with mild CRN had a lower IRR of number of ED visits than the elderly with no CRN (0.77, 95% CI 0.61–0.98). No significant difference in the IRR of number of ED visits was seen among the elderly with severe CRN as compared to the elderly without CRN. Covariates significantly associated with having a higher IRR of number of ED visits included having 2–3 comorbidities or 4 or more comorbidities, fair or poor self reported health status, annual income ≤ 25K a year, Medicaid Part D coverage or LIS Part D coverage. Having less than a high school education was associated with having a lower IRR of number of ED visits (see Table 2).
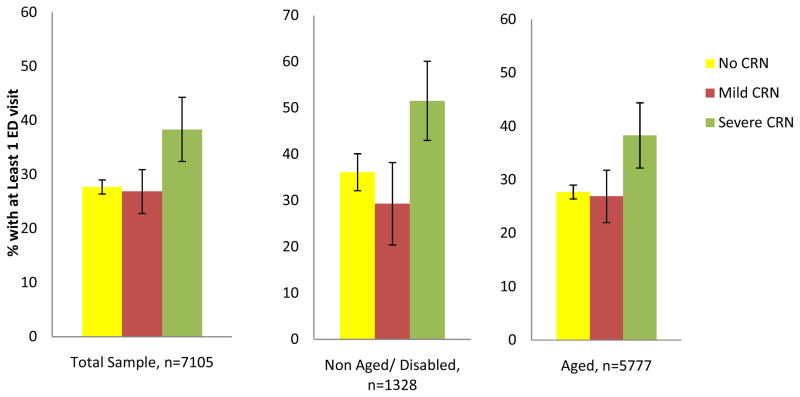
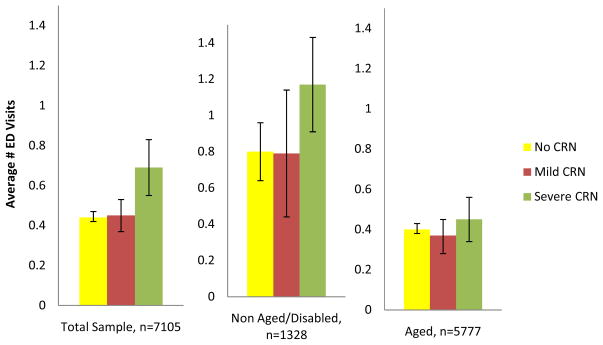
Figure 2 shows the adjusted predicted probabilities of having at least one ED visit (error bars represent the 95% CI around the predicted probabilities). Among our entire sample (and adjusting for demographic, socioeconomic, health, race/ethnicity and co-insurance characteristics) beneficiaries with severe CRN were more likely to have at least one ED visit as compared to those without severe CRN (p<0.05). Adjusting for other factors, 38.3% (95% CI 32.4–44.3%) of Medicare beneficiaries reporting severe CRN had at least one ED visit, as compared to 26.9% of people with mild CRN (95% CI 22.8–30.9%) and 27.5% of beneficiaries with no CRN (95% CI 26.4–29.0%). These results were mainly driven by findings for disabled Medicare beneficiaries; in this group, those with severe CRN were also more likely to have at least one ED visit (51.5%, 95% CI 43.0–60.1%) as compared to disabled Medicare beneficiaries without CRN (36.1%, 95% CI 32.1–40.1%), disabled Medicare beneficiaries with mild CRN (29.3%, 95% CI 20.4–38.3%), and elderly Medicare beneficiaries in all CRN categories, Figure 3 shows the adjusted predicted number of ED visits from our Poisson model by CRN and eligibility categories. Persons with severe CRN had an average of 0.69 ED visits (95% CI 0.55– 0.83) during the year as compared to persons without CRN who had 0.44 visits (95% CI 0.41–0.47). The disabled with severe CRN had an average of 1.17 visits (95% CI 0.91–1.43) as compared to 0.80 visits among the disabled without CRN (95% CI 0.64–0.96).
Figure 2. Adjusted Predicted Percentages, Any ED Visit, by CRN and eligibility categories*.
* Predicted probabilities of percentages of persons with at least one ED visit from multivariate logistic regression, weighted to national Medicare population. Excludes missing observations. Error Bars Represent 95% CI (Predicted from multivariate logistic regression analysis controlling for variables in Table 2.)
Figure 3. Adjusted predicted average number of ED visits, by CRN and eligibility categories*.
* Predicted probabilities of average number of ED visits from multivariate Poisson regression, Excludes missing observations. Weighted to National Medicare Population. Error Bars Represent 95% CI34,35 (Predicted from multivariate Poisson regression analysis controlling for variables identified in Table 3.)
Limitations
There are a number of limitations to our study. Our main outcome was any type of emergency department visit. Given our small sample size and the lack of information on prescription drug use and specifically what prescriptions were affected by CRN, we could not identify emergency department visits directly associated with cost-related medication nonadherence. There is some evidence that cost-related nonadherence is more likely to occur for certain type of medications, such as those used to relieve acute symptoms versus those taken for preventive purposes.43 We also do not have detailed data about out of pocket costs in the Access to Care file and therefore cannot directly calculate total costs associated with nonadherance in our study. In addition, beneficiaries with severe CRN were more likely to be under age 64, have poor self-reported health status, and have more comorbidities. While we adjusted for these important factors, there may be other unmeasured variables associated with CRN in these subgroups that could have impacted our results with respect to ED use.
While we did include prescription drug coverage as a covariate in our analysis, we did not have adequate sample size in smaller eligibility subgroups to examine utilization related to specific coverage in more detail. Although persons with Medicaid Part D and LIS Part D prescription drug coverage were more likely to have any ED visit as well as a higher mean number of visits as compared to persons with employer based coverage, these may have been proxies of overall higher rates of utilization and greater severity of illness among the Medicaid and LIS population rather than reflecting adequacy of coverage. Further study is needed to examine the relationship between drug coverage and utilization as well as the interaction between CRN and coverage in more detail.
Because our dataset only contains Medicare beneficiaries, we are not able to determine the relationship between CRN and the general population of non-Medicare beneficiaries. Finally, because the survey predates many of the economic changes that have occurred in recent years, we may have potentially underestimated the prevalence of CRN that occurred in 2007 when ER claims were generated after initial survey responses were collected.
Discussion
Our results show an association between severe CRN and a statistically significant increased risk of emergency department use. Disabled Medicare beneficiaries (younger than 65) who report severe cost-related medication nonadherence were more likely to have at least one emergency department visit in the following year, even when adjusting for other factors that impact utilization, such as demographic, health, SES and race/ethnicity variables. The average disabled person with severe CRN in our sample had a higher adjusted predicted probability of having at least one ED visit. They also had a trend towards having a higher mean number of annual visits as compared to the average disabled person without any CRN, although not statistically significant at p<0.05.
There are a number of possible explanations for our findings. Disabled beneficiaries represent a population with poor access and high medical needs. They have higher rates of poverty and tend to have multiple chronic conditions.36.41 There is also evidence that this population has a higher rate of emergency department use and more difficulty in accessing outpatient health care services than non-disabled Medicare beneficiaries.36,42 Our findings suggest that cost-related nonadherence may be an additional factor contributing to increased rates of ED use previously demonstrated in this vulnerable population. 39,45
Disabled beneficiaries also tend to have higher prescription drug needs and higher out-of-pocket costs compared with elderly Medicare beneficiaries.6,46 While a number of studies have shown that Part D resulted in a decrease in both CRN and out-of-pocket costs among the elderly population, these effects have been less dramatic among the disabled. 11,12, 25,47,48 The disabled are more likely than the elderly to report not being able to get a prescription medication due to cost restrictions, even when covered by Part D. 39
There was no statistically significant difference in utilization between groups in the entire sample and in the disabled with mild CRN and no CRN. Among the elderly, average number of ED visits are slightly lower among those with mild CRN as compared to no CRN. It is possible that there is a threshold effect in which ED utilization is not associated with occasionally skipping or splitting doses, but rather rates of ED visits increase with more extreme lapses in medication use that can occur when prescriptions are not obtained at all due to cost (severe CRN).
CRN is a frequent occurrence among Medicare beneficiaries and also impacts their ED use. Prior work has shown that CRN is common among the general population of emergency department users. In one study, 25% of emergency department patients reported cost-related barriers or concerns related to obtaining medications, but that study did not examine the relationship between CRN and ED visits, as we do in this study.48
Our results show that even after implementation of Part D, CRN remains a problem for a significant segment of the Medicare population. It is unclear what additional impact certain components of the Patient Protection and Affordable Care Act (ACA) will have on CRN and utilization. For example, under the ACA, in 2011 Part D enrollees received a 50 percent discount on brand-name drug spending within the doughnut hole. The law gradually reduces the ceiling of catastrophic coverage starting 2015, phasing out the doughnut hole entirely by 2020. It is also unclear what the impact of additional subsidies such as Veterans Administration (VA) drug assistance programs, State Pharmaceutical Assistance Programs or variations in LIS coverage have on CRN and on utilization. Although we did have some limited information in our dataset about participation in these programs, our sample sizes for the VA and SPAP subgroups were too small to be able to examine these effects independently. In addition, the LIS program offers assistance with premiums and lower co-pays for individuals at varying levels based on income and assets; we had insufficient sample size to examine LIS coverage at varying levels of subsidy support or by state. There is some evidence that these subsidy programs are significantly underutilized. For example, although some individuals are automatically enrolled in the LIS Part D program (including dual eligibles, persons in Medicare Savings Programs and Social Security Income recipients), an estimated 2 million individuals do not receive this benefit despite being eligible, mainly due to lack of awareness of eligibility and enrollment procedures.49 Other seniors may qualify for SPAP, which is also means tested and offers premium and copayment assistance for Part D plan participation in a number of states. 50 Finally, as we do not have charges or costs associated with each visit in our dataset, it is unclear how our findings translate into additional costs for the ED population.
Specific policies that aim to decrease CRN are likely needed for disabled Medicare beneficiaries, who represent a high risk, high use population. In the meantime, further research is warranted to better understand the factors that may contribute to the increased rate of CRN and emergency department utilization by disabled Medicare beneficiaries. CRN is not only a high risk behavior that should be identified among ED users, but it may also be a marker for other serious unmet social needs in such vulnerable populations. For example, persons with CRN have also been shown to spend less on basic needs, such as food and heat, in order to afford their medications; this may be a potential confounder in our analysis contributing to our results.25 Such social needs have been associated with an increased risk of both ED use and hospitalizations.51–55 The ED may serve as an access point in which CRN as well as other unmet needs can be addressed to prevent morbidity and improve overall health status.56 At the very minimum, health professionals working in the ED need to cultivate a greater awareness of the cost-related barriers to care that face disabled and elderly patients presenting to the ED, and also to adopt strategies to reduce such cost-related barriers, including prescribing lower cost or generic prescription medications when possible and advising patients about eligibility for potential federal and state supplemental coverage programs.
Acknowledgments
Grant: This work was supported by a Diversity Supplement to Dr. Blanchard of a grant from the National Institutes of Aging, Principal Investigator, Dr. Soumerai (RO1 AG-22362)
Footnotes
Author contributions: JB, JM, DRD, and SS conceived the study. JB, JM, DRD and SS obtained research funding. JB analyzed the data. JM, DRD and SS provided statistical advice on study design and analysis. JB drafted the manuscript and all authors contributed substantially to its revision. JB takes responsibility for the paper as a whole.
References
- 1.Centers for Medicare & Medicaid Services. [Accessed November 12, 2011];National Health Expenditure Accounts. http://www.cms.hhs.gov/NationalHealthExpendData/
- 2.Stagnitti M. Average number of total (including refills) and unique prescriptions by select person characteristics, 2006. [Accessed March 3, 2012];MEPS Statistical Brief #245. 2009 May; http://meps.ahrq.gov/mepsweb/data_files/publications/st245/stat245.pdf.
- 3.Briesacher BA, Gurwitz JH, Soumerai SB. Patients at risk for cost-related medication nonadherence: a review of the literature. JGIM. 2007;22:864–71. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White House Domestic Policy Council. [Accessed February 29, 2012];Disability, Medicare and Prescription Drugs. http://clinton4.nara.gov/WH/EOP/nec/html/ParkMedicareReport000730.html.
- 5.Foote SM, Hogan C. Disability Profile And Health Care Costs Of Medicare Beneficiaries Under Age sixty-five. Health Affairs. 2001;6:242–253. doi: 10.1377/hlthaff.20.6.242. [DOI] [PubMed] [Google Scholar]
- 6.Safran DG, Neuman P, Schoen C. Prescription drug coverage and seniors: findings from a 2003 national health survey. Health Aff. 2005;W5:152–166. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- 7.Osterberg L, Blaschke T. Adherence to medication. NEJM. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 8.Levy H, Weir D. Take-up of Medicare Part D: evidence from the health and retirement study. Jl Gerontol: B Psychol Soc Sci. 2010;65:492–501. doi: 10.1093/geronb/gbp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelhardt GV, Gruber J. Medicare Part D and the financial protection of the elderly. [Accessed February 1, 2012];NBER Working Paper No 16155. http://www.nber.org/papers/w16155.
- 10.Lichtenberg FR, Sun SX. The impact of Medicare Part D on prescription drug use by the elderly. Health Aff. 2007;26:1735–1744. doi: 10.1377/hlthaff.26.6.1735. [DOI] [PubMed] [Google Scholar]
- 11.Millett C, Everett CJ, Matheson EM, Bindman AB, Mainous AG. Impact of Medicare Part D on seniors out of pocket expenditures on medications. Arch Int Med. 2010;170:1325–1330. doi: 10.1001/archinternmed.2010.208. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Donohue JM, Lave JR, O’Donnell G, Newhouse JP. The Effect of Medicare Part D on Drug and Medical Spending. N Engl J Med. 2009;361:52–56. doi: 10.1056/NEJMsa0807998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briesacher BA, Zhao Y, Madden J, et al. Medicare part d and changes in prescription drug use and cost burden: national estimates for the Medicare population 2000 to 2007. Med Care. 2011;49:834–841. doi: 10.1097/MLR.0b013e3182162afb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetics in three systems of care. Med Care. 2004;42:102–109. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- 15.Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff. 2003;22:220–229. doi: 10.1377/hlthaff.22.4.220. [DOI] [PubMed] [Google Scholar]
- 16.Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care. 2010;48:87–94. doi: 10.1097/MLR.0b013e3181c12e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ho PM, Rumsfeld JS, Masoudi DA, et al. Effect of Medication Nonadherence on Hospitalization and Mortality Among Patients With Diabetes Mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 18.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 19.Ho PM, Spertus JA, Masoudi FA, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166:1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 20.Horwitz RI, Viscoli CM, Berkman L, et al. Treatment adherence and risk of death after a myocardial infarction. Lancet. 1990;336:542–545. doi: 10.1016/0140-6736(90)92095-y. [DOI] [PubMed] [Google Scholar]
- 21.Center for Medicaid and Medicare Services. [Accessed October 20, 2011];Technical Documentation for the Medicare Current Beneficiary Survey. http://www.cms.gov/mcbs/downloads/HHC2002appendixA.pdf.
- 22.Research Data Assistance Center. [Accessed February 1, 2012];MCBS Frequenty Asked Questions. http://www.resdac.org/MCBS/mcbsFAQ.asp.
- 23.Gold M, Jacobson G, Damico A, Neuman . Medicare advantage 2012 data spotlight: enrollment maret update. Kaiser Family Foundation; [Accessed February 2, 2013]. www.kff.org/medicare/upload/8323/pdf/ [Google Scholar]
- 24.Research Data Assistance Center. [Accessed March 9, 2012];How to identify claims based emergency room visits. http://www.resdac.org/tools/TBs/TN-003_EmergencyRoominClaims_508.pdf.
- 25.Government Accounting Office. Medicare physician services: utilization trends indicate sustained beneficiary access with high and growing levels of service in some areas of the nation. Aug, 2009. GAO-09-559. [Google Scholar]
- 26.Madden JM, Graves AJ, Zhang F, et al. Cost related nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA. 2008;299:1922–1928. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost related medication nonadherence among the elderly and the disabled: a national survey one year before the Medicare drug benefit. Arch Intern Med. 2006;166:1829–1835. doi: 10.1001/archinte.166.17.1829. [DOI] [PubMed] [Google Scholar]
- 28.Pierre-Jacques M, Safran DG, Zhang F, et al. Reliability of new measures of cost-related medication nonadherence. Med Care. 2008;46:444–448. doi: 10.1097/MLR.0b013e31815dc59a. [DOI] [PubMed] [Google Scholar]
- 29.Fan L, Shah MN, Veazie P, Friedman B. Factors associated with emergency department use among the rural elderly. J Rural Health. 2011;27:39–49. doi: 10.1111/j.1748-0361.2010.00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah MN, Glushak C, Karrison TG, et al. Predictors of emergency medical services utilization by elders. Acad Emerg Med. 2003;10:52–58. doi: 10.1111/j.1553-2712.2003.tb01976.x. [DOI] [PubMed] [Google Scholar]
- 31.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary. Advance Data from Vital and Health Statistics. 2007:386. [PubMed] [Google Scholar]
- 32.McCusker J, Karp I, Cardin S, Durand P, Morin J. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med. 2003;10:1362–1370. doi: 10.1111/j.1553-2712.2003.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 33.Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;51:769–774. doi: 10.1016/j.annemergmed.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Katz S. Assessing self-maintenance: activities of daily living, mobility and instrumental activities of daily living. J Am Getiatr Soc. 1983;31:721–726. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 35.Spillman BC, Black KJ. The size and characteristics of the residential care population: evidence from three national surveys. The Urban Institute; Jan 4, 2006. prepared for the US Department of Health and Human Services. [Google Scholar]
- 36.Donders AR, Van der Heijdfen J, Stijnen T, Moons K. Review: a gentle introduction to imputation of missing values. Jl Clin Epi N. 2006;59:1087–1091. doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 37.Bambauer KZ, Safran DG, Ross-Degnan D, Zhang F, Adams AS, Gurwitz J, Pierre-Jacques M, Soumerai SB. Depression and cost-related medication nonadherence in Medicare beneficiaries. Arch Gen Psychiatry. 2007 May;64(5):602–8. doi: 10.1001/archpsyc.64.5.602. [DOI] [PubMed] [Google Scholar]
- 38.Zivin K, Madden JM, Graves AJ, Zhang F, Soumerai SB. Cost-related medication nonadherence among beneficiaries with depression following Medicare Part D. Am J Geriatr Psychiatry. 2009 Dec;17(12):1068–76. doi: 10.1097/JGP.0b013e3181b972d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cubanski J, Neuman P. Medicare doesn’t work as well for younger disabled beneficiaries as it does for older enrollees. Health Aff. 2010;29:1725–1733. doi: 10.1377/hlthaff.2009.0962. [DOI] [PubMed] [Google Scholar]
- 40.UCLA: Academic Technology Services. Statistical Consulting Group; [Accessed February 10, 2012]. Introduction to SAS. from http://www.ats.ucla.edu/stat/sas/notes2/ [Google Scholar]
- 41.Statistical Software. College Station, TX: StataCorp LP; 2009. Stata Base Reference Manual. Release 11. StataCorp. Stata: Release 11. [Google Scholar]
- 42.Ferraro D, Liu H. Uses of the Medicare Current Beneficiary Survey for analysis across time. [Accessed June 17, 2012];ASA Survey Section on Research Methods. http://www.amstat.org/sections/srms/proceedings/y2005/Files/JSM2005-000828.pdf.
- 43.Briesacher B, Tjia J, Doubeni CA, Chen Y, Rao SR. Methodological issues in using multiple years of the Medicare Current Beneficiary Survey. MMRR. 2012;2:E1–E20. doi: 10.5600/mmrr.002.01.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Piette JD, Heisler M, Wagner TH. Cost-Related Medication Underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94:1782–1787. doi: 10.2105/ajph.94.10.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gold M, Stevens B. Medicare’s less visible population: disabled beneficiaries under age 65. [Accessed February 29, 2012];Mathematica. 2001 http://www.mathematica-mpr.com/PDFs/opinsights2.pdf.
- 46.Briesacher B, Stuart B, Doshi J, et al. Medicare’s disabled benefiaries: the forgotten population in the depate over drug benefits. Kaiser family foundation; Sep, 2002. [Accessed February 15, 2012]. http://www.kff.org/medicare/upload/Medicare-s-Disabled-Beneficiaries-The-Forgotten-Population-in-the-Debate-Over-Drug-Benefits-Report.pdf. [Google Scholar]
- 47.Liu FX, Alexander GC, Crawford SY, Pickard AS, Hedeker D, Walton SM. The impcct of Medicare part D on out of pocket costs for prescription drugs, medication utilization, health resource utilization and preference based health utility. HSR. 2011;46:1104–1125. doi: 10.1111/j.1475-6773.2011.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacobson G, Neuman T, Damico A, Lyons B. The role of Medicare for people dually eligible for Medicare and Medicaid. Henry J. Kaiser Family Foundation; Jan, 2011. [Accessed March 1, 2012]. Issue Brief. http://www.kff.org/medicare/upload/8138.pdf. [Google Scholar]
- 49.Mazer M, Bisgaier J, Daley E, et al. Risk for cost related nonadherence among emergency department patients. Acad Emerg Med. 2011;18:267–272. doi: 10.1111/j.1553-2712.2011.01007.x. [DOI] [PubMed] [Google Scholar]
- 50.Summer L, Hadley J, Hargrave E. The Henry J Kaiser Program. Sep, 2010. The Medicare Part D Low Income Subsidy Program. [Google Scholar]
- 51.Kaiser Family Foundation. The role of state pharmaceutical assistance programs in serving low-income Medicare beneficiaries following the implementation of Medicare Part D. Jun, 2007. Issue Brief. [Google Scholar]
- 52.Nelson K, Brown ME, Lurie N. Hunger in an adult patient population. JAMA. 1998;279:1211–1214. doi: 10.1001/jama.279.15.1211. [DOI] [PubMed] [Google Scholar]
- 53.Kersey MA, Beran MS, McGovern PG, Biros MH, Lurie N. The prevalence and effects in an emergency department patient population. Acad Emerg Med. 1999;6:1109–1114. doi: 10.1111/j.1553-2712.1999.tb00112.x. [DOI] [PubMed] [Google Scholar]
- 54.Gordon JA. The hospital emergency department as a social welfare institution. Ann Emerg Med. 1999;33:321–5. doi: 10.1016/s0196-0644(99)70369-0. [DOI] [PubMed] [Google Scholar]
- 55.Gordon JA. Social welfare in the hospital emergency department: the challenge of integrated community health care. Ann Emerg Med. 2009;53:603–4. doi: 10.1016/j.annemergmed.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 56.Rodriguez RM, Fortman J, Chee C, et al. Nonmedical needs motivating visits of the homeless to an urban emergency department. Ann Emerg Med. 2009;53:598–602. doi: 10.1016/j.annemergmed.2008.07.046. [DOI] [PubMed] [Google Scholar]