Abstract
Objective
Following a successful2005–2012 phase with three regional practice-based research networks (PBRNs), a single, unified national network called “The National Dental PBRN” was created in 2012 in the United States to improve oral health by conducting practice-based research and serving dental professionals through education and collegiality.
Methods
Central administration is based in Alabama. Regional centres are based in Alabama, Florida, Minnesota, Oregon, New York and Texas, with a Coordinating Centre in Maryland. Ideas for studies are prioritized by the Executive Committee, comprised mostly of full-time clinicians.
Results
To date, 2736 persons have enrolled, from all six network regions; enrollment continues to expand. They represent a broad range of practitioners, practice types, and patient populations. Practitioners are actively improving every step of the research process, from idea generation, to study development, field testing, data collection, and presentation and publication.
Conclusions
Practitioners from diverse settings are partnering with fellow practitioners and academics to improve clinical practice and meet the needs of clinicians and their patients.
Clinical significance
This “nation’s network” aims to serve as a precious national resource to improve the scientific basis for clinical decision-making and foster movement of the latest evidence into routine practice.
Keywords: Practice-based research, Dentistry, Primary care, Health services research, Multi-centre studies
1. Introduction
Practice-based research networks (PBRNs) have demonstrated that they can make major and unique contributions in improving clinical practice.1–3 Their growth in number and diversity is due to the unique advantages that they offer both to research and quality improvement, to their ability to bring practice-relevant topics onto the research agenda, and to their ability to move scientific advances into routine practice quickly.4–11 Although medical PBRNs began in the 1970s, to our knowledge no dental PBRN existed in the United States before 2002. To catalyze the development of dental PBRNs, the National Institute of Dental and Craniofacial Research (NIDCR), part of the National Institutes of Health, the main funder of biomedical and health research in the United States, funded three regional dental PBRNs in 2005 for a seven-year period. By the end of their funding period in 2012, the regional PBRNs had conducted numerous studies with thousands of patients and hundreds of practitioners on a broad range of topics and study designs; demonstrated rigour, adherence to protocol, and impact on clinical practice; and proven that dental practitioners can effectively contribute to every step of the research process. Owing to the success of the regional PBRNs, NIDCR funded the PBRN initiative for an additional seven-year period, but in this new phase, as a single, unified national network, rather than regional PBRNs. In April 2012, this new network, “The National Dental PBRN”, began operation. Our objectives are to describe the purpose, structure and function of this new national network, as well as to encourage participation in it.
2. Methods
2.1. Administrative structure of the network: central offices
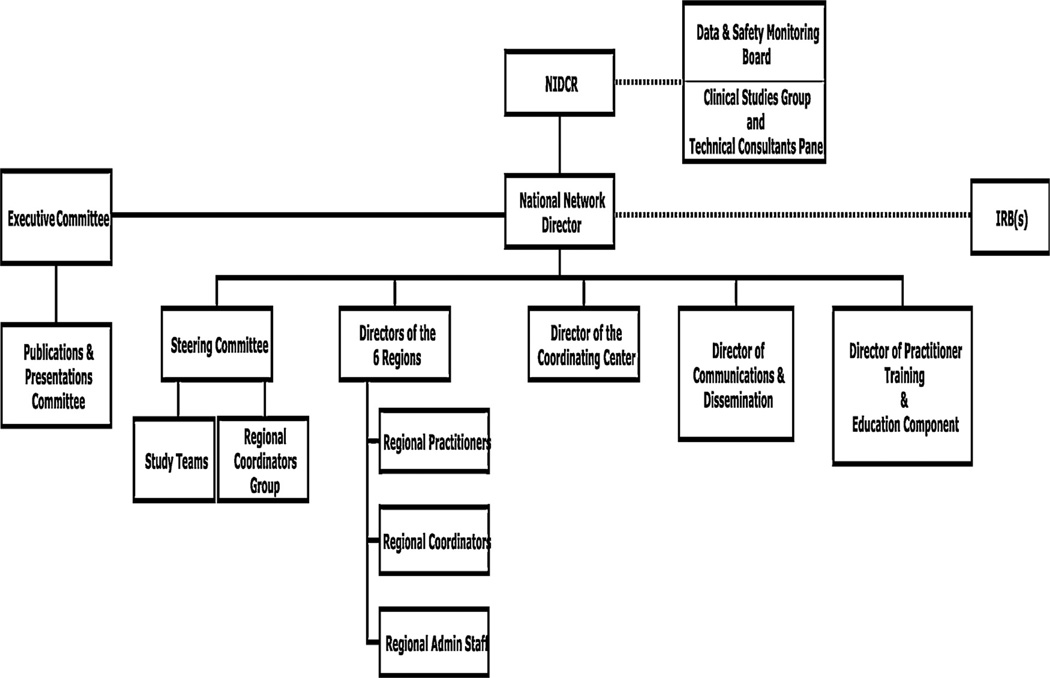
The mission of the network is “to improve oral health by conducting dental practice-based research and by serving dental professionals through education and collegiality”. It is committed to maximize the practicality of conducting research in everyday clinical practice across geographically dispersed regions and diverse practice types. Its structure is designed to focus some activities at the regional level (e.g., close interactions with practitioners), while other activities of the entire network are better managed centrally (e.g., study development and dissemination). The network’s organizational chart is shown in Fig. 1. The central administrative base is at the University of Alabama at Birmingham, with six network regions administratively based in Alabama, Florida (University of Florida), Minnesota (HealthPartners Institute for Education and Research), New York (University of Rochester), Oregon (Kaiser Permanente Centre for Health Research), and Texas (University of Texas Health Science Centre at San Antonio). All enrolled practitioners are associated with one of these regional centres.
Fig. 1.
Network organizational chart.
2.2. National Network Director
The National Network Director is responsible for overall scientific and administrative leadership, operations and fiscal management, and chairing the Executive Committee and Steering Committee. The office of the National Network Director also has a faculty-level Director of Communications and Dissemination (also located at the University of Alabama at Birmingham), who directs the network’s web site, email and postal communications, webinars, and plans network communications and dissemination activities. A Director of Practitioner Training and Education Component (located at the University of Florida) also reports to the National Network Director, directing practitioner enrollment, training and education activities, such as the Enrollment Questionnaire, network orientation, training and certification in human subjects research and financial conflict of interest.
2.3. Coordinating Centre
The Coordinating Centre, based at Westat in Rockville, MD, provides expertise in study design and statistical support, develops and maintains databases and information systems, conducts data analyses, and participates in publications, among other duties. It contains doctoral-level biostatisticians plus staff with expertise in data management and analysis, study design, and informatics.
2.4. Recruitment
Recruitment of practitioners into the network includes general dentists, dental specialists, and dental hygienists. Practitioners may receive a postal or electronic mailing that describes the network and invites their participation. They also may be recruited at dental meetings, at annual meetings of existing network practitioners, by other network practitioners, by announcements from dental organizations, or via the network’s internet site. Enrollment consists of completing an online Enrollment Questionnaire that describes practitioner and practice characteristics.12 Enrollees choose one of three participation levels: (1) information only (join the network’s mailing list to receive regular news and study updates); (2) limited participation (mailing list, plus participate in network surveys); (3) full participation (includes participation in in-office studies). Practitioners who wish to be full participants are required to attend a network annual meeting or orientation session (or electronic version of it, for which they receive continuing education credit; complete an online course in human participants research (also receive continuing education credit); and complete documents that affiliate them with an Institutional Review Board (ethics committee).
Once full-participant practitioners have completed these requirements, they are eligible for recruitment to specific clinical studies. Practitioners can participate in as few or as many studies as they wish, depending on any network requirements for specific studies. Study-specific requirements may comprise seeing a sufficient number of patients of a particular type, or doing a certain treatment procedure on a regular basis. From this given study-specific pool of eligible practitioners, recruitment is typically made by emailing descriptions of the study and asking if the practitioner is interested in such a study. Recruitment goals usually require region-specific quotas so as to disperse participation nationally.
General dentists, dental specialists, and dental hygienists can enrol. Additionally, non-practitioners can enrol in the information-only participation level. The network defines a non-practitioner as anyone who does not meet both of these criteria: (1) currently licensed to practice dentistry or dental hygiene; and (2) currently treats patients on a regular basis. This means that dental students and dental residents can enrol, as can retire dentists, dental faculty who do not currently treat patients, and non-dental care providers. Non-practitioners are encouraged to enrol because they can serve as additional means to disseminate information, provide expertise for studies, and encourage practitioners to enrol.
2.5. Administrative structure of the network: committees
Much of the work of the network is handled by the following four committees. Additional details about the network’s administrative structure are publicly available.13
2.5.1. Executive Committee
This committee is the key decision-making body of the network and is structured to make the network practitioner-driven. By design, majority voting authority resides with its six practitioner-investigator representatives. One vote is also given to the National Network Director and the Director of the Coordinating Centre, and a NIDCR representative serves on the committee as an ex officio, non-voting member. The most important role of the committee is to render judgement about proposed study ideas and study protocols. All accepted studies must be deemed suitable for the PBRN research context, feasible, of interest to network practitioners, and able to significantly impact routine clinical practice and/or public oral health after their completion. This committee also renders judgement about the amount of compensation that will be paid to practitioners for each study. Additionally, it makes decisions about certain operational issues, especially those that most directly impact practitioners. The committee usually meets monthly. Most meetings are held by telephone conference, with one meeting held face-to-face each year.
2.5.2. Steering Committee
This committee’s voting members comprise the National Network Director, the Director of the Coordinating Centre, and the Directors of the network’s six regions. Its purpose is to determine how best to implement decisions made by the Executive Committee; assist investigators with developing study applications into a more-final form before they are sent to the Executive Committee; and maximize coordination of tasks across regions, in conjunction with the Regional Coordination Committee. The committee meets monthly by telephone conference and annually face-to-face.
2.5.3. Regional Coordination Committee
This committee comprises the Regional Coordinators in the network, the National Network Director, National Network Director staff, and certain Coordinating Centre staff. The committee Chair is one of the Regional Coordinators whose responsibility rotates across regions on an annual basis. The main duties of the committee are to determine optimal practices for interacting with practitioners; to advise the Steering Committee, Directors, and study investigators regarding best practices; and to standardize and monitor certain study procedures among practitioners participating across all regions.
2.5.4. Publications and Presentations Committee
Its purpose is to review and render judgement about all network publications, abstracts, and presentations; encourage publications and presentations; and ensure compliance with the Publications and Presentations Policy. The committee comprises a practitioner-investigator, representatives from two network regions and the Office of the National Network Director and Coordinating Centre.
2.6. The study development process
A key operating principle for the network is that most research questions or study topics originate from practitioners, and that the answers to these questions have the potential to immediately improve clinical practice. Furthermore, the research itself is done within the practices of the network members. This situation creates a healthy tension between the needs of a sound study and the need not to be overly disruptive of routine clinical practice. The process begins with the proposed Study Principal Investigator using a network-provided Study Concept Template, which provides a 2–7 page overview of the study. Following initial review by a Regional Director or the National Network Director, the next step is review by the Executive Committee, usually during a meeting with the Study Principal Investigator present via teleconference. If the Executive Committee approves the study concept, it is forwarded to the NIDCR Clinical Studies Group to determine whether it overlaps with a study already funded by NIDCR, and to assess scientific rigour and appropriateness to the PBRN context.
2.6.1. NIDCR Clinical Studies Group
The Clinical Studies Group formalizes the process for NIDCR evaluation and approval of network projects. It is composed of NIDCR Programme Officials, the NIDCR Office of Clinical Trials Operations & Management, and others from the Institute. The Clinical Studies Group comprises experts in study methodology, scientific content, and programme knowledge. The Clinical Studies Group can approve with or without recommendations, or disapprove the concept. If disapproved by the Clinical Studies Group, no further study development occurs. If the concept is approved by the Clinical Studies Group, then a Complete Protocol is developed and if approved by the Executive Committee, the Clinical Studies Group then evaluates the Complete Protocol and provides feedback as needed during an iterative process with an eye towards eventual approval as the final Complete Protocol is agreed upon. An NIDCR Technical Consultants Panel also may be formed. This is a panel of study-specific subject experts recommended by NIDCR to guide specific aspects of protocol development.
2.6.2. Study Team
If the study concept is approved by the Clinical Studies Group, the proposed Study Principal Investigator is asked to form a Study Team. The Study Team can comprise personnel already in the network or if advisable, draw on national or international scientists with applicable expertise. The composition of the Study Team is reviewed by the Clinical Studies Group. If approved, the Study Team is asked to develop a Complete Protocol. The Complete Protocol is reviewed by the Executive Committee and if approved, undergoes review by the Clinical Studies Group. If the Complete Protocol receives Clinical Studies Group approval, the Study Team proposes a budget, and if this is approved by the Clinical Studies Group, application(s) are submitted to each region’s respective Institutional Review Board. All federally-funded human participants research conducted in the United States must be approved by an Institutional Review Board. Institutional Review Boards take responsibility for ensuring that the rights of human participants are protected and that studies include proper procedures to ensure the privacy of information that participants provide.
The Study Team administers the study from protocol development, to feasibility and pilot testing, to data collection, to data analysis, to study closure, to presentations, manuscript preparation, and other dissemination activities. The team includes subject experts and is protocol-specific. It is constituted by the National Network Director in concert with the proposed Study Principal Investigator and the NIDCR Clinical Studies Group. While forming the Study Team, the network may call on expertise nationally or internationally if needed, or only use expertise already available in the network, depending on the study topic and study design. The composition of the team varies with the stage of the study. The study is typically managed via monthly conference calls in which the only agenda items have to do with that study. During protocol development, the minimum composition is the Study Principal Investigator, the subject expert(s), the National Network Director, a Regional Coordinator, a Coordinating Centre representative, and a practitioner-investigator. At a later stage, representatives from each region join the monthly Study Team conference calls during data forms development, feasibility testing, pilot testing, and data collection phases. After Institutional Review Board approval is obtained, the study is launched directly, or more often, the Study Principal Investigator is asked to lead feasibility and/or pilot testing before a network-wide full launch. Approved versions of data collection forms for each study are pilot tested with practitioners on the Executive Committee and selected practitioners across the network. Pilot testing often leads to changes in these forms to optimize their use in a diverse range of practice settings. Once final versions of all forms have been completed, a study is implemented in all regions. After data collection for the study has ended and its data set(s) are locked, the Study Team typically dissolves and at that point the Study Principal Investigator takes responsibility for leading data analyses and manuscript preparations, a process which itself may involve conference calls of personnel involved in manuscript preparation from the study.
2.6.3. Data and Safety Monitoring Board
The Data and Safety Monitoring Board is an independent group of experts that advises NIDCR and study investigators on clinical studies, especially those that involve an intervention. Its responsibilities include monitoring human subject safety, evaluating the accumulated study data; reviewing study conduct and progress; and making recommendations to NIDCR concerning the continuation, modification, or termination of the study. Study-specific data as well as relevant background information about the disease, patient population, procedures and progress of the study are also considered.
3. Results
3.1. Characteristics of enrolled practitioners
As of March 31, 2013, 2539 practicing dentists and hygienists enrolled, defined as completing an Enrollment Questionnaire. This questionnaire comprises items about practitioner, practice, and patient characteristics, and is publicly available.12 Key characteristics of the enrolled practitioners and their practices are also shown in Table 1 (an unabridged version is publicly available),13 stratified by whether they are dentists or dental hygienists Dentists are further stratified by private vs. non-private practice and by generalist vs. specialist. Characteristics of an additional 224 enrolled non-practitioners are also publicly available.13
Table 1.
Characteristics of enrolled practitioners, by practice type (abridged version; as of March 31, 2013).
| Dentists |
Hygienists | |||||
|---|---|---|---|---|---|---|
| Private vs. non-privatea |
General vs. specialistb |
|||||
| Characteristic | All | Private practice |
Non-private | General practitioner |
Specialist | All |
| Overall | 1974 | 1704 | 259 | 1567 | 398 | 565 |
| Number of different locations at which you see patients | ||||||
| 1 | 1599 (81.1%) | 1403 (82.3%) | 187 (72.2%) | 1342 (85.6%) | 250 (62.8%) | 397 (70.3%) |
| 2 | 273 (13.8%) | 221 (13.0%) | 52 (20.1%) | 177 (11.3%) | 96 (24.1%) | 108 (19.1%) |
| 3 | 57 (2.9%) | 49 (2.9%) | 8 (3.1%) | 29 (1.9%) | 28 (7.0%) | 21 (3.7%) |
| More than 3 | 43 (2.2%) | 31 (1.8%) | 12 (4.6%) | 19 (1.2%) | 24 (6.0%) | 39 (6.9%) |
| Total | 1972 (100.0%) | 1704 (100.0%) | 259 (100.0%) | 1567 (100.0%) | 398 (100.0%) | 565 (100.0%) |
| Missing/blank | 2 | 0 | 0 | 0 | 0 | 0 |
| Gender | ||||||
| Male | 1438 (73.5%) | 1272 (75.2%) | 159 (62.1%) | 1133 (72.8%) | 304 (77.4%) | 15 (2.7%) |
| Female | 519 (26.5%) | 419 (24.8%) | 97 (37.9%) | 424 (27.2%) | 89 (22.6%) | 549 (97.3%) |
| Total | 1957 (100.0%) | 1691 (100.0%) | 256 (100.0%) | 1557 (100.0%) | 393 (100.0%) | 564 (100.0%) |
| Missing/blank | 17 | 13 | 3 | 10 | 5 | 1 |
| Age | ||||||
| Mean (S.D.) | 49.9 (11.8) | 51.1 (11.7) | 49.7 (12.9) | 50.6 (11.9) | 52.0 (11.4) | 44.2 (11.0) |
| Missing/blank | 17 | 12 | 4 | 10 | 5 | 2 |
| Hispanic/Latino | ||||||
| Yes | 117 (6.0%) | 88 (5.2%) | 27 (10.6%) | 80 (5.2%) | 35 (8.9%) | 60 (10.7%) |
| No | 1832 (94.0%) | 1596 (94.8%) | 228 (89.4%) | 1470 (94.8%) | 357 (91.1%) | 500 (89.3%) |
| Total | 1949 (100.0%) | 1684 (100.0%) | 255 (100.0%) | 1550 (100.0%) | 392 (100.0%) | 560 (100.0%) |
| Missing/blank | 25 | 20 | 4 | 17 | 6 | 5 |
| Race | ||||||
| White/Caucasian | 1625 (83.4%) | 1425 (84.5%) | 193 (76.6%) | 1287 (83.2%) | 333 (84.5%) | 499 (88.9%) |
| Black/African-American | 87 (4.5%) | 67 (4.0%) | 18 (7.1%) | 73 (4.7%) | 14 (3.6%) | 23 (4.1%) |
| American Indian/Alaska Native | 6 (0.3%) | 6 (0.4%) | 0 (0.0%) | 6 (0.4%) | 0 (0.0%) | 4 (0.7%) |
| Asian | 172 (8.8%) | 137 (8.1%) | 35 (13.9%) | 133 (8.6%) | 38 (9.6%) | 17 (3.0%) |
| Native Hawaiian/Pacific Islander | 3 (0.2%) | 2 (0.1%) | 1 (0.4%) | 2 (0.1%) | 1 (0.3%) | 2 (0.4%) |
| Other | 55 (2.8%) | 49 (2.9%) | 5 (2.0%) | 46 (3.0%) | 8 (2.0%) | 16 (2.9%) |
| Total | 1948 (100.0%) | 1686 (100.0%) | 252 (100.0%) | 1547 (100.0%) | 394 (100.0%) | 561 (100.0%) |
| Missing/blank | 26 | 18 | 7 | 20 | 4 | 4 |
| Practice location | ||||||
| Inner city of urban area | 260 (13.2%) | 172 (10.1%) | 85 (33.1%) | 193 (12.3%) | 65 (16.5%) | 119 (21.2%) |
| Urban (not inner city) | 582 (29.6%) | 490 (28.8%) | 91 (35.4%) | 443 (28.3%) | 136 (34.4%) | 135 (24.0%) |
| Suburban | 849 (43.2%) | 813 (47.9%) | 33 (12.8%) | 675 (43.2%) | 174 (44.1%) | 237 (42.2%) |
| Rural | 273 (13.9%) | 224 (13.2%) | 48 (18.7%) | 253 (16.2%) | 20 (5.1%) | 71 (12.6%) |
| Total | 1964 (100.0%) | 1699 (100.0%) | 257 (100.0%) | 1564 (100.0%) | 395 (100.0%) | 562 (100.0%) |
| Missing/blank | 10 | 5 | 2 | 3 | 3 | 3 |
| Hours in practice | ||||||
| 32 or more hours | 1596 (81.8%) | 1447 (85.7%) | 142 (56.1%) | 1298 (83.6%) | 295 (75.1%) | 355 (63.3%) |
| Less than 32 h | 354 (18.2%) | 242 (14.3%) | 111 (43.9%) | 254 (16.4%) | 98 (24.9%) | 206 (36.7%) |
| Total | 1950 (100.0%) | 1689 (100.0%) | 253 (100.0%) | 1552 (100.0%) | 393 (100.0%) | 561 (100.0%) |
| Missing/blank | 24 | 15 | 6 | 15 | 5 | 4 |
| Percentage of patients who are [mean (S.D.)] | ||||||
| Covered by a private insurance programme |
59.0 (25.5) | 63.1 (21.4) | 31.2 (32.3) | 59.4 (25.2) | 57.2 (26.5) | 58.6 (29.1) |
| Covered by a public programme | 14.9 (23.7) | 11.4 (18.8) | 38.8 (36.3) | 14.4 (23.6) | 16.7 (23.9) | 14.7 (25.1) |
| Not covered by any third party and pays out of pocket |
22.2 (18.0) | 23.1 (17.4) | 16.3 (21.1) | 22.2 (17.6) | 22.5 (19.6) | 20.3 (19.5) |
| Receiving free care or substantially reduced fees courtesy of this practice |
3.7 (10.8) | 2.3 (4.4) | 13.2 (25.5) | 3.8 (11.0) | 3.4 (10.0) | 6.1 (17.4) |
| Missing/blank | 42 | 25 | 13 | 23 | 13 | 18 |
| Type of main practice | ||||||
| Owner of private practice | 1304 (66.4%) | 1304 (76.5%) | 0 (0.0%) | 1064 (68.2%) | 239 (60.2%) | |
| Associate or employee of a private practice |
265 (13.5%) | 265 (15.6%) | 0 (0.0%) | 212 (13.6%) | 53 (13.4%) | |
| HealthPartners Dental Group | 60 (3.1%) | 60 (3.5%) | 0 (0.0%) | 50 (3.2%) | 9 (2.3%) | |
| Permanente Dental Associates | 59 (3.0%) | 59 (3.5%) | 0 (0.0%) | 55 (3.5%) | 3 (0.8%) | |
| Other managed care or preferred provider organization |
16 (0.8%) | 16 (0.9%) | 0 (0.0%) | 15 (1.0%) | 1 (0.3%) | |
| Public health practice, community health centre, or publicly-funded clinic |
79 (4.0%) | 0 (0.0%) | 79 (30.5%) | 78 (5.0%) | 1 (0.3%) | |
| Federal Government Facility (VA, DoD, Public Health Service) |
35 (1.8%) | 0 (0.0%) | 35 (13.5%) | 27 (1.7%) | 8 (2.0%) | |
| Dental school, academic institution, or facility staffed by dental school |
145 (7.4%) | 0 (0.0%) | 145 (56.0%) | 60 (3.8%) | 83 (20.9%) | |
| Total | 1963 (100.0%) | 1704 (100.0%) | 259 (100.0%) | 1561 (100.0%) | 397 (100.0%) | |
| Missing/blank | 11 | 0 | 0 | 6 | 1 | |
| Year of graduation from dental school | ||||||
| Graduation year [Mean (S.D.)] | 1990 (12.2) | 1989 (12.1) | 1991 (12.8) | 1990 (12.4) | 1988 (11.5) | |
| Missing/blank | 8 | 2 | 1 | 1 | 1 | |
| Type of dentist | ||||||
| General dentist | 1567 (79.7%) | 1396 (82.1%) | 165 (64.2%) | 1567 (100%) | 0 (0.0%) | |
| Specialist | 398 (20.3%) | 305 (17.9%) | 92 (35.8%) | 0 (0.0%) | 398 (100%) | |
| 1965 (100.0%) | 1701 (100.0%) | 257 (100.0%) | 1567 (100.0%) | 398 (100.0%) | ||
| Missing/blank | 9 | 3 | 2 | 0 | 0 | |
| Member of | ||||||
| American Dental Association | 1562 (79.1%) | 1370 (80.4%) | 187 (72.2%) | 1217 (77.7%) | 343 (86.2%) | |
| Academy of General Dentistry | 631 (32.0%) | 582 (34.2%) | 48 (18.5%) | 616 (39.3%) | 15 (3.8%) | |
| Educational setting for your dental hygiene training | ||||||
| Technical or community college | 280 (50.2%) | |||||
| Four-year college | 207 (37.1%) | |||||
| Alabama Dental Hygiene Programme | 28 (5.0%) | |||||
| Other | 43 (7.7%) | |||||
| Total | 558 (100.0%) | |||||
| Missing/blank | 7 | |||||
| Became licensed as a dental hygienist | ||||||
| Year licensed | 1994 (12.4) | |||||
| Missing/blank | 14 | |||||
11 dentists are missing: Private vs. non-private information.
9 dentists are missing: General vs. specialist information.
3.2. Motivations of practitioners to participate
Table 2 lists the benefits of participating in the network as communicated by practitioners themselves. Some practitioners have volunteered to provide written and/or video testimonials in an effort to encourage participation by colleagues.14,15 Others have written journal articles and provided oral and poster presentations for the same reasons. The network also holds annual meetings of practitioner-investigators in each region. Practitioners regularly report that they enjoy the collegial interaction that occurs at these meetings. These meetings provide face-to-face opportunities to hear the latest results from network studies, help design future studies, network with colleagues, and obtain continuing education credit. An additional benefit is that these meetings provide a mechanism for practitioners to interact, discuss the challenges of daily clinical practice, and in still a sense of belonging to a network that is much larger than them. Annual meetings with fellow practitioner-investigators also create an acceptance of responsibility for improving one’s own daily clinical practice, by understanding what is happening in their practices and the practices of fellow practitioners, having seen study results to which they themselves contributed. We have learned that interactive meetings with fellow practitioners can be an effective means to move scientific findings into clinical practice.16,17
Table 2.
Benefits of participating as communicated by network practitioners.
| Increases the practice’s visibility and stature among dental patients |
| Distinguishes the practice from other practices, acting as a practice promoter or practice builder |
| Receive financial remuneration for the time spent doing research |
| Enhances communication with patients by showing that the practitioner cares about the scientific basis of clinical practice – practitioner is “staying current” |
| Improves quality of dental care by contributing to the scientific basis for the dental procedures that are their focus |
| Get to see what is effective in their practices in comparison to other practices – using results that are presented anonymously |
| Serves as a team builder for practice staff, and engages the entire staff in the excitement of discovery and quality improvement |
| Have a venue for collegial interactions and exchange of ideas with fellow practitioners, becoming part of a community of learning and camaraderie |
| Do research projects that are relevant and benefit their practice |
| Improves the logistics of daily clinical operations |
| Receive Continuing Education credit for attendance at National Dental PBRN annual meetings and participating in training and certification activities for specific National Dental PBRN studies |
| Present at local, state, and national dental meetings and research conferences |
| Get preliminary reports of research results as soon as they are available |
| Practitioner is the first to know of upcoming studies |
| Opportunities to attend annual meetings of practitioner- investigators |
4. Discussion
Results shown in Table 1 make it clear that network enrolees represent a substantial diversity in key practice and practitioner characteristics. This may offer the network advantages, such as being able to evaluate how practice differences affect treatment outcomes. Although there is substantial diversity, network members are not selected randomly, so another consideration is how representative these practitioners are of United States practitioners at large. Comparisons can be made to dentists who participated in the 2010 ADA Survey of Dental Practice; this survey samples both American Dental Association (ADA) members and non-ADA members, is based on a national probability sample, and provides the most comprehensive information on the characteristics of United States dentists.18 Limitations are that the sample is limited to dentists in private practice, is based on a 29% response rate, and provides results from 2009. Because ADA Survey respondents cannot be practitioners in public health clinics, federal or tribal facilities, community health centres, or dental schools (provided they do not see private patients in the dental school), comparisons to network practitioners are limited in that regard. A total of 79% of ADA survey participants were general dentists, compared to 80% of network practitioners. Gender distribution in the ADA survey was 17% female [p. 6], compared to 27% female for network practitioners. The mean age in the ADA survey was 52.8 years [p. 5]; compared to 49.9 years for network practitioners. ADA Survey practices with one dentist accounted for 78% of practices [p. 8], compared to 81% for network dentists. A total of 64% of patients had private dental insurance in the ADA Survey [p. 23], compared to 59% for network practitioners. Although comparisons to the ADA data have limitations, we conclude that network enrolees have much in common with dentists at large. This is salient because network enrolees comprise only a small proportion of all of the dentists in the United States. While it is reassuring that network dentists and United States dentists are similar for the characteristics for which ADA data are available, network dentists may be more attuned to evidence-based recommendations owing to their interest in having a research component in their practice; therefore, they may differ in characteristics that are not measured in national surveys. Having extensive Enrollment Questionnaire information for these practitioners is advantageous because it allows the network to better describe these dentists’ comparability. This information is also helpful for understanding regional variations in clinical practice.
Comparisons can also be made to the 2007 Suruey of Dental Hygienists sponsored by the American Dental Hygienists’ Association (AHDA),19 derived from a random sample of currently licensed dental hygienists, which had a response rate of 44%. A total of 99% of practicing hygienists in the ADHA survey were women, compared to 97% female for network hygienists. A total of 92% of ADHA survey hygienists were non-Hispanic, compared to 89% for network hygienists. The mean age of practicing hygienists in the ADHA survey was 44.1 years, compared to 44.2 years for network hygienists. A total of 53% of practicing hygienists in the ADHA survey worked full-time, which was defined in the ADHA survey as 31 or more hours per week, compared to 63% for network practitioners when full-time was defined as 32 h or more. We conclude that hygienist network enrolees have much in common with hygienists at large.
Clinical researchers have attempted many methods designed to foster movement of scientific evidence into routine clinical practice, with varying success. PBRNs provide a practitioner-friendly venue to test these methods. Because of this, the National Dental PBRN not only conducts studies of effectiveness (i.e., what clinical treatment and diagnostic methods work, for whom, and when), but also studies to test evidence dissemination and implementation methods. The network conceptualizes this two-pronged approach as comprising two “sides of the same coin”, in which one side of the coin comprises effectiveness studies, while the other side of the coin comprises dissemination and implementation science studies. Both sides of the coin are equally important, and affect the network’s research priorities. The often-lamented research-to-practice gap refers to the delay between what research evidence suggests should be happening in routine clinical practice, and what is actually happening. This single gap is best dissected into three gaps (Dr. Sharon Levine, personal communication, 2012). There first can be a “knowledge gap”, wherein the effectiveness of a treatment is not known. This creates a need to conduct research studies to determine effectiveness in order to close that gap. Then there can be a “knowing gap”, in which the effectiveness of a treatment has been scientifically established, but practitioners are not aware of this knowledge. This “knowing gap” creates a need to more effectively disseminate that knowledge (evidence). There also can be a “knouring-to-doing gap”, in which knowledge is available and providers are aware of it, but they have not yet implemented the recommended changes. This gap is a result of inadequate implementation of evidence, due to a variety of reasons. Therefore, the National Dental PBRN seeks to do studies and other activities that close all three gaps, in an effort to close the overall research-to-practice gap.
PBRNs are based on the understanding that the experience, insight, and practical wisdom of full-time clinicians and their patients are powerful means to advance the health of the population and address challenges encountered in clinical practice. Dentistry can play an active role in these advancements, showing that knowledge transfer not only happens in the research-to-practice direction, but also in the practice-to-research direction. The National Dental PBRN seeks to become a precious and prized national resource, capitalizing on the rare opportunity provided to the dental profession by the NIDCR to add to the scientific basis of clinical decision-making and movement of this evidence into routine clinical practice. It seeks to: (1) become the preferred venue where ideas are put to the test under real-world conditions; (2) conduct studies that actually make a difference in how care is provided; (3) serve as a venue for testing methods for how best to move evidence into routine practice; (4) be a network that enhancesi professional and inter-professional collaborations; (5) be a key source for what works, when, and for whom; (6) serve as an opportunity for the profession to lead rather than to be led; and (7) be a network that patients see as contributing to their well-being and enhancing the public’s view of dentistry as being committed to research and quality improvement. The dental PBRN research context has changed the profession’s model for doing research. It has done so by bringing practitioners and patients to the discussion table. The National Dental PBRN seeks to foster a future in which research and quality improvement are done on a routine basis in everyday clinical practice – just because that is what dentists do as a profession.
Acknowledgments
This work was supported by NIH grant U19-DE-22516. An Internet site devoted to details about the nation’s network is located at http://NationalDentalPBRN.org. Persons who comprise the National Dental PBRN Collaborative Group are listed at http://NationalDentalPBRN.org/users/publications. Special acknowledgement is due to the current Executive Committee members: George J. Allen, DDS, private practice in Mobile, AL; Vanessa Burton, DDS, HealthPartners Dental Group, Minneapolis, MN; William R. Calnon, DDS, private practice, Rochester, NY; Claudia L. Cavazos, DDS, Laredo, TX; George W. Ford, DMD, private practice in Atlanta, GA; Walter R. Manning, DMD, private practice in Albany, OR; and the Deputy Regional Directors not listed as co-authors: Daniel J. Pihlstrom, DDS, Portland, OR; Donald R, Nixdorf, DDS, MS, Minneapolis, MN; Rahma Mungia, BDS, MPH, San Antonio, TX; Joseph L. Riley, III PhD, Gainesville, FL; Dorota Kopycka-Kedzierawski, DDS, MPH, Rochester, NY.
Special acknowledgement is also due to regional and Coordinating Centre staff; in Birmingham, AL: Andrea Mathews, BS, RDH, Terri McDougald; in Gainesville, FL: Pearl Harris, BASDH, RDH, CCRP, Deborah McEdward, BS, RDH, CCRP, Brenda Thacker, RDH, AS; in Minneapolis, MN: Emily Durand, RDH, Sarah Basile, RDH, MPH, Mary Kelley, BA; in Portland, OR: Kristine Funk, MS, RD, Lisa Waiwaiole, MS; in Rockville, MD: Megan Meyer, BS; in Rochester, NY: Mary Therese Biltucci, RDH, MA, Rita Cacciato, RDH, Pat Regusa, BFA, Kathy Bohn, AAS; in San Antonio, TX: Stephanie Reyes, BA, Sara Theisen, BA.
Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
Abbreviations
- ADA
American Dental Association
- ADHA
American Dental Hygiene Association
- PBRN
practice-based research network
- NIDCR
United States National Institute of Dental and Craniofacial Research
Footnotes
Author contributions
All authors contributed to manuscript preparation and editing.
REFERENCES
- 1.Green LA, Hickner J. A short history of primary care practice-based research networks: from concept to essential research laboratories. Journal of the American Board of Family Medicine. 2006;19:1–10. doi: 10.3122/jabfm.19.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Werner JJ. Measuring the impact of practice-based research networks (PBRNs) Journal of the American Board of Family Medicine. 2012;25:557–559. doi: 10.3122/jabfm.2012.05.120176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilbert GH, Richman JS, Gordan VV, Rindal DB, Fellows JL, Benjamin PL, et al. Lessons learned during the conduct of clinical studies in the dental PBRN. Journal of Dental Education. 2011;75:453–465. [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson KA, Lipman PD, Lange CJ, Cohen RA, Durako S. Supporting better science in primary care: a description of practice-based research networks (PBRNs) in 2011. Journal of the American Board of Family Medicine. 2012;25:565–571. doi: 10.3122/jabfm.2012.05.120100. [DOI] [PubMed] [Google Scholar]
- 5.Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Annals of Family Medicine. 2005;3:S12–S20. doi: 10.1370/afm.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams RL, Rhyne RL. No longer simply a practice-based research network (PBRN): health improvement networks. Journal of the American Board of Family Medicine. 2011;24:485–488. doi: 10.3122/jabfm.2011.05.110102. [DOI] [PubMed] [Google Scholar]
- 7.Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Family Practice. 2008;25:20–24. doi: 10.1093/fampra/cmn055. [DOI] [PubMed] [Google Scholar]
- 8.D’Souza RN, Ebersole JL, Fox CH, Polverini PJ, Scannapieco FA. How practicing dentists can shape dental research: the American Association for Dental Research’s vision for the future. Journal of the American Dental Association. 2012;143:1069–1071. doi: 10.14219/jada.archive.2012.0026. [DOI] [PubMed] [Google Scholar]
- 9.Gordan VV, Riley JL, 3rd, Worley DC, Gilbert GH. DPBRN Collaborative Group Restorative material and other tooth-specific variables associated with the decision to repair or replace defective restorations: findings from The Dental PBRN. Journal of Dentistry. 2012;40:397–405. doi: 10.1016/j.jdent.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rindal DB, Gordan VV, Fellows JL, Spurlock NL, Bauer MR, Litaker MS, et al. Differences between reported and actual restored caries lesion depths: results from The Dental PBRN. Journal of Dentistry. 2012;40:248–254. doi: 10.1016/j.jdent.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rindal DB, Gordan VV, Litaker MS, Bader JD, Fellows JL, Qyist V, et al. Methods dentists use to diagnose primary caries lesions prior to restorative treatment: findings from The Dental PBRN. Journal of Dentistry. 2010;38:1027–1032. doi: 10.1016/j.jdent.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enrollment Page. [[accessed 2.4.2013]];2013 Available at: http://nationaldentalpbrn.org/enrollment.php;
- 13.Peer-reviewed Publications Page. [[accessed 2.4.2013]];Citations listing this current manuscript and appendices provided to supplement this manuscript. 2013 Available at: http://nationaldentalpbrn.org/peer-reviewed-publications.php;
- 14.Testimonials Page. [[accessed 2.4.2013]];2013 Available at: http://nationaldentalpbrn.org/testimonials.php;
- 15.Videos Page. [[accessed 2.4.2013]];2013 Available at: http://nationaldentalpbrn.org/videos.php;
- 16.Gilbert GH, Richman JS, Qyist V, Pihlstrom DJ, Foy PJ, Gordan VV, et al. Change in stated clinical practice associated with participation in the DPBRN. General Dentistry. 2010;58:520–528. [PMC free article] [PubMed] [Google Scholar]
- 17.Gilbert GH, Gordan W, Funkhouser EM, Rindal DB, Fellows JL, Qyist V, et al. Caries treatment in a dental practice-based research network: movement toward stated evidence-based treatment. Community Dentistry and Oral Epidemiology. 2013;41:143–153. doi: 10.1111/cdoe.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Dental Association, Survey Center. The 2010 survey of dental practice. Chicago: American Dental Association; 2012. [Google Scholar]
- 19.American Dental Association. Survey of dental hygienists in the United States, 2007: executive summary. Chicago: American Dental Hygienists’ Association; 2009. [Google Scholar]