Abstract
Purpose:
To evaluate the psychometric properties of the UK FIM + FAM.
Methods:
(a) A systematic literature review integrating the evidence for psychometric qualities of both the original and UK versions, and (b) exploratory and confirmatory factor analysis of admission/discharge data from an inpatient general neuro-rehabilitation cohort using parametric and non-parametric techniques. A prospective cohort of 459 patients with a male:female ratio of 57:43 and mean age of 44.5 (SD 14.3) years participated in this study.
Results:
Seven published articles together demonstrated acceptable utility, concurrent validity, inter-rater reliability and responsiveness of the UK FIM + FAM. Factor analysis demonstrated that all items loaded high (>0.58) on the first principal component and distinct motor and cognitive factors emerged after rotation. A four-factor solution also demonstrated four distinct, interpretable dimensions (Physical, Psychosocial, Communication and Extended Activities of Everyday Living (EADL)). Mokken analysis of the second data set confirmed these dimensions. Cronbach’s αs were 0.97 and 0.96 for the motor and cognitive domains and 0.90–0.97 for the subscales. Analysis of responsiveness demonstrated “large” effect sizes (0.86–1.29).
Conclusions:
The UK FIM + FAM, including the newer EADL module, is a valid, reliable scale of functional independence. It has high internal consistency in two domains and four subscales and is responsive to changes occurring in a general inpatient neuro-rehabilitation population.
Implications for Rehabilitation
The UK FIM + FAM is a valid, reliable scale of functional independence, which is responsive to changes occurring in a general inpatient neuro-rehabilitation population.
Physical, Psychosocial, Communication It can be used to derive a reliable, single score of overall independence and also yields specific information in two main domains and four separate subscales of independence: Physical, Psychosocial, Communication and Extended Activities of Daily Living (EADL).
The newer EADL item module provides added value, measuring functional independence for community-based activities.
Keywords: Extended activities of daily living, factor analysis, Mokken analysis, neurological rehabilitation, psychometrics, UK FIM + FAM
Introduction
Global measures of disability such as the Functional Independence Measure (FIM) [1] and Functional Assessment Measure (FIM + FAM) [2] are widely used internationally to measure outcome from inpatient rehabilitation programmes. At the individual clinical level, they provide valid and reliable information about a person’s requirements for assistance with essential tasks of daily living, and on a group level, they can be used to measure and compare outcomes across different practices and populations. Consequently, it is important to understand their metric properties in the population in which they are to be used.
The FIM is an 18-item ordinal measure of disability which includes 13 motor items and five cognitive items [3]. It was developed in the 1980s by a national task force in the United States (US) and is now one of the most commonly used generic outcome measures in rehabilitation. Its psychometric properties have been very thoroughly evaluated in the world literature [3–6]. The FAM does not stand alone (hence the abbreviation “FIM + FAM”) but adds a further 12 items to the FIM primarily addressing cognitive and psychosocial function.
The original US version of the FAM was developed in the early 1990s, for evaluating outcomes after traumatic brain injury [2,7]. Although the US FAM and original training materials are still accessible from the TBI COMBI (Centre for Outcomes Measurement in Brain Injury) website [8], the US version is no longer actively maintained or centrally collated.
The UK version of the FAM was developed in the mid-1990s by the United Kingdom FIM + FAM Users Group [9] in collaboration with the US originators, to translate it into UK-English and address the known subjectivity and inconsistency of some items. The resulting tool was shown to have improved reliability and utility in comparison with the US version [9]. It has continued to be revised and developed, with the addition of a six-item Extended activities of Daily Living (EADL) module (to extend the upper range of the instrument) and an active programme for training and accrediting users [10].
The two versions are structurally similar, so that the psychometric performance of the US version has relevance for the UK FIM + FAM. However, they are sufficiently different so that the UK version requires validation in its own right.
Although originally conceptualised for use with traumatic or diffuse brain injury, many of the FAM items are more widely applicable in other neurological conditions, including spinal cord injury and progressive neurological conditions. For this reason, the UK FIM + FAM has gained in popularity over the last decade, effectively taking over where development of the US version ceased and it is now the version that continues to be promoted and developed. It has recently been adopted as the principal outcome measure for neuro-rehabilitation in the UK national dataset for specialist rehabilitation (UK Rehabilitation Outcomes Collaborative [11,12]) and is increasingly being explored as an outcome measure for rehabilitation in other countries, including Australia, New Zealand, Europe and South America. It is therefore pertinent to examine its psychometric properties in the broader neuro-rehabilitation group in which it will be applied.
The aim of this article is to examine the extent to which the UK FIM + FAM satisfies the criteria of the Medical Outcomes Trust for a psychometrically robust measure [13]. These nine criteria include content validity, internal consistency, criterion validity, construct validity, reproducibility, responsiveness, floor/ceiling effects and interpretability.
Part 1 of this article reports a brief systematic review and assimilation of the existing literature on the psychometric properties of both the original US version and the UK FIM + FAM.
In Part 2, in order to address the identified gaps in the literature, we used a combination of parametric and non-parametric techniques to explore dimensionality, internal consistency and responsiveness of the UK FIM + FAM in a large consecutive cohort of inpatients representing the diagnostic diversity of a general neuro-rehabilitation sample.
Part 1: A Systematic review of US FIM + FAM and UK FIM + FAM studies
Methods
To identify existing studies on psychometric aspects of the US and the UK FIM + FAM, we searched the following databases using the search terms Functional Assessment Measure.mp and FIM + FAM.mp: Medline 1948 – November 2012, Embase 1980 – November 2012, PsycINFO 1806 – November 2012. Studies concerned with the psychometric properties of the FIM + FAM, as well as studies that were not primarily psychometric but might report relevant statistics (e.g. predictive validity), were identified by two investigators (L.T.S. and R.J.S.) on the basis of the title or abstract.
Results
We recovered 16 articles reporting on the psychometric qualities of the US FIM + FAM [2,7,14–27] and seven [9,10,12,28–31] on the UK FIM + FAM (six relating to the main scale and one to the EADL module). Appendix 1 summarises the existing literature and also highlights the contribution of new psychometric data presented in this article. The 16 articles on the US version reported a range of important psychometric properties including utility, reliability, validity, dimensionality (i.e. factor structure), responsiveness and floor/ceiling effects. In general, the US FIM + FAM had good psychometric properties, although several papers raised concerns about ceiling effects when it is used in outpatient or community settings.
The seven papers on the UK version reported good psychometric properties for responsiveness, utility, inter-rater reliability and concurrent validity. One raised concerns regarding ceiling effects in an outpatient setting [28]. To date, only two articles have examined responsiveness of the UK FIM + FAM [28,29], and only one has examined the psychometric properties of the newer Extended Activities of Daily Living module – reporting inter-rater and test–retest reliability [10]. We found no previously published reports on the internal consistency or the factor structure of the UK FIM + FAM.
Part 2: Scaling properties and dimensionality of the UK FIM + FAM in a mixed neuro-rehabilitation cohort
Methods
The FIM + FAM scale
The content of the US and UK FIM + FAM are shown in Table 1. The 18-item FIM component is common to both.
Table 1.
Content of the US and UK FIM + FAM – all items are scored on a range of 1–7.
| FIM items – 18 items (common to both instruments) | US FAM items – 12 items | UK FAM items – 18 items |
|---|---|---|
| Eating | Swallowing | Swallowing |
| Grooming | Car transfers | Car transfers |
| Bathing | Community mobility | Community mobility |
| Dressing – upper body | Reading | Reading |
| Dressing – lower body | Writing | Writing |
| Toileting | Speech intelligibility | Speech intelligibility |
| Bladder management | Emotional status | Emotional status |
| Bowel management | Adjustment to limitations | Adjustment to limitations |
| Bed, chair, wheelchair transfers | Employability | Use of leisure timea |
| Toilet transfers | Orientation | Orientation |
| Tub and shower transfers | Attention | Concentrationa |
| Walking/wheelchair locomotion | Safety judgment | Safety awarenessa |
| Stairs | ||
| Comprehension | UK EADL items | |
| Expression | Meal preparation | |
| Social interaction | Laundry | |
| Problem solving | Housework | |
| Memory | Shopping | |
| Financial management | ||
| Work/educationb |
aItems that are re-defined in the UK FIM + FAM.
bWork education has been added subsequent to the data collection for this analysis.
FIM, Functional Independence Measure; FAM, Functional Assessment Measure; EADL, Extended Activities of Daily Living.
Both US and UK versions of the FAM comprise 12 additional items which are scored on the same seven-level structure as the FIM – each item being rated on seven levels with a score ranging from 1 – “Total dependence” to 7 – “Complete independence”.
Three items in the UK FIM + FAM differ from the US version [9]: “Concentration” replaces “Attention”; “Safety awareness” replaces “Safety judgement”; and “Use of leisure time” replaces “Employability”. In addition, a module addressing extended activities of daily living has been developed to address reported ceiling effects of the UK FIM + FAM in community rehabilitation settings [10]. Five items (see Table 1) were originally included, to which a sixth item addressing “Working ability” has recently been added.
Participants and setting
Data were analysed from a tertiary specialist inpatient rehabilitation service in London (catchment population in excess of five million) for patients with complex neurological disability. In this unit, the UK FIM + FAM has been routinely collected as part of routine clinical practice since 1999, although the EADL items were introduced gradually and only collected for all patients since August 2007.
UK FIM + FAM scores are routinely rated by the multidisciplinary treating team within 10 days of admission and during the last seven days before discharge. The unit is the national training centre for the UK FIM + FAM, so that all staff receive full training and regular updates on its application. From a cohort of 764 consecutive patients admitted between January 1999 and December 2009, 459 had complete FIM + FAM data (including the EADL items) on admission and discharge. All 305 scores with missing EADL data were for admissions prior to August 2007. Between August 2007 and December 2009, data collection was complete for all admissions (n = 188). Demographic characteristics of the cohort (n = 459) are shown in Table 2.
Table 2.
Participants’ demographic characteristics (n = 459).
| Demographic | Mean (SD) | Range |
|---|---|---|
| Age | 44.5 (14.3) years | 15–82 |
| Length of stay | 101 (61) days | 12–435 |
| N | % | |
| Male:Female | 262:197 | 57:43 |
| Diagnosis: | ||
| Acquired brain injury | 384 | 84% |
| Aetiology: | ||
| Vascular | 256 | 67% |
| Traumatic | 67 | 17% |
| Inflammatory | 23 | 6% |
| Hypoxic | 21 | 5% |
| Tumour | 14 | 4% |
| Other | 3 | 1% |
| Spinal cord injury | 38 | 8% |
| Other neurological conditions: | 37 | 8% |
| Peripheral nerve disordersa | 33 | 7% |
| Progressive (e.g. multiple sclerosis) | 4 | 1% |
aPeripheral nerve disorders include Guillain--Barré Syndrome, critical illness neuropathy, etc.
Ethics approval
The data were gathered routinely in the course of clinical practice. Approval has been granted by the Harrow Research Ethics Committee (ref no. 04/Q0405/81) for reporting this centre’s clinical data retrospectively for research and audit purposes.
Analysis
As this is the first examination of factor structure within the UK FIM + FAM, our two-stage analysis included both exploratory and confirmatory components. FIM + FAM data are ordinal and often skewed, so we used a combination of parametric and non-parametric techniques. To do this, we divided the sample at random (using the PASW v.18 select cases function) into two smaller samples of 225 (parametric, exploratory factor analysis (EFA)) and 234 (non-parametric, Mokken scale analysis). For both samples, we included each participant’s admission and discharge FIM + FAM ratings, in order to maximise the range of ability sampled. This also doubled the sample size.
Stage 1 – EFA
We first applied an EFA to the pooled admission/discharge scores of the first sample (n = 450). Even though they are based on parametric assumptions, principal components and factor analysis are widely used in this context and have generally been considered appropriate for the initial stage of exploring and describing the relationships among a large set of variables, even where assumptions of normality may not strictly hold [32]. The EFA was completed using PASW-18 software (SPSS, Chicago, IL). The Kaiser--Meyer--Olkin and Bartlett’s test both indicated that the correlation matrix was suitable for factor analysis [33]. The choice of principal component analysis and Varimax rotation was made because these methods typically provide clear, interpretable solutions [34] and also to allow for direct comparison with the one previous factor analysis of the US FIM + FAM by Hawley et al. [16]. On the basis of that previous factor analysis, we rotated two components [16]. However, our principal components analysis revealed four components with eigenvalues >1 (suggesting four substantial sources of variance), so we also examined a four-factor solution.
Stage 2 – Confirmatory Mokken analysis
We used Mokken analysis in our confirmatory analysis of the second pooled dataset (n = 468), to see if the dimensions identified from the EFA could be confirmed using non-parametric methods. Mokken scaling analysis of polytomous items was undertaken using MSPWIN 5.0 software [35]. In addition to examining the full 35-item scale, we also tested the subscales based on the two-factor and four-factor solutions provided by the EFA.
Unlike parametric methods, such as confirmatory factor analysis (CFA) or Rasch [36–38], Mokken analysis makes no assumptions concerning the distribution underpinning the data. It calculates Loevinger’s H coefficient for a scale, and each of its individual items, to determine if they satisfy the requirements for a stochastic or probabilistic Guttman scale [39]. H values < 0.30 are considered to reflect a poor item and values for the scale as a whole are interpreted as follows: H values in the range 0.30–0.40 reflect a weak scale, 0.40–0.50 a medium scale and H > 0.50 reflects a strong scale. Hence, any scale that fulfils the criteria for a robust scale in Mokken terms can be considered a reliable, unidimensional, ordinal scale that is suitable for rank-ordering persons.
Interpretation and responsiveness
After completing EFA and CFA on the split dataset, internal consistency of the identified subscales was evaluated using Cronbach’s α for the entire dataset (including both admission and discharge scores). Despite the ordinal nature of FIM + FAM data, parametric and non-parametric evaluation of responsiveness in this large dataset gave very similar results. Here, we report the evaluation of responsiveness (change between admission and discharge) within the various subscales using paired t tests. Effect sizes are calculated using Cohen’s d, taking account of the correlation between the means, and interpreted according to Cohen (0.2 = Small, 0.5 = Medium, 0.8 = Large) [40]. (A non-parametric analysis of responsiveness is available from the authors on request.)
Results
Stage 1 – EFA and internal consistency
The results of the principal components analysis with two-factor Varimax rotations are presented in Table 3.
Table 3.
Principal components analysis with two- and four-factor varimax rotations of 30 FIM + FAM and five EADL items (n = 450)a.
| Two factors |
Four factors |
|||||||
|---|---|---|---|---|---|---|---|---|
| Item | Median (IQR)a | Single factor 1st PC |
Motor | Cognitive | Physical | Psycho-social | Com’n | EADL |
| Eating | 5 (5–7) | 0.79 | 0.52 | (0.61) | 0.57 | |||
| Swallowing | 7 (6–7) | 0.65 | (0.34) | (0.58) | 0.51 | (0.53) | ||
| Grooming | 5 (4–7) | 0.89 | 0.63 | (0.63) | 0.62 | |||
| Bathing | 4 (3–6) | 0.89 | 0.77 | 0.73 | ||||
| Dressing – upper | 5 (3–7) | 0.88 | 0.68 | (0.55) | 0.66 | |||
| Dressing – lower | 3 (2–6) | 0.87 | 0.84 | 0.76 | ||||
| Toileting | 5 (2–7) | 0.84 | 0.85 | 0.84 | ||||
| Bladder management | 6 (3–7) | 0.74 | 0.67 | 0.74 | ||||
| Bowel management | 6 (3–7) | 0.72 | 0.64 | 0.74 | ||||
| Transfers – bed/chair | 5 (3–7) | 0.85 | 0.86 | 0.86 | ||||
| Transfers – toilet | 5 (2–6) | 0.85 | 0.87 | 0.87 | ||||
| Transfers – tub/shower | 4 (1–6) | 0.80 | 0.87 | 0.81 | ||||
| Car transfer | 3 (1–5) | 0.79 | 0.85 | 0.73 | ||||
| Locomotion | 5 (1–6) | 0.79 | 0.79 | 0.75 | ||||
| Stairs | 1 (1–6) | 0.71 | 0.86 | 0.78 | ||||
| Community mobility | 1 (1–3) | 0.74 | 0.75 | 0.71 | ||||
| Comprehension | 6 (4–7) | 0.67 | 0.84 | 0.73 | ||||
| Expression | 5 (3–7) | 0.68 | 0.84 | 0.81 | ||||
| Reading | 5 (4–7) | 0.66 | 0.79 | 0.70 | ||||
| Writing | 4 (2–6) | 0.70 | 0.77 | 0.73 | ||||
| Speech intelligibility | 7 (4–7) | 0.59 | 0.65 | 0.74 | ||||
| Social interaction | 6 (5–7) | 0.71 | 0.77 | 0.75 | ||||
| Emotional status | 6 (3–7) | 0.63 | 0.61 | 0.68 | ||||
| Adjustment | 5 (3–6) | 0.76 | 0.65 | 0.69 | ||||
| Use of leisure time | 6 (3–6) | 0.81 | 0.67 | 0.51 | ||||
| Problem solving | 5 (2–6) | 0.81 | 0.78 | 0.68 | ||||
| Memory | 5 (3–7) | 0.75 | 0.77 | 0.73 | ||||
| Orientation | 7 (4–7) | 0.75 | 0.80 | 0.72 | ||||
| Concentration | 6 (4–7) | 0.75 | 0.76 | 0.74 | ||||
| Safety awareness | 4 (2–6) | 0.82 | 0.67 | 0.60 | ||||
| Meals | 2 (1–5) | 0.78 | 0.73 | 0.67 | ||||
| Laundry | 1 (1–2) | 0.60 | 0.59 | 0.78 | ||||
| Housework | 1 (1–2) | 0.61 | 0.66 | 0.77 | ||||
| Shopping | 1 (1–3) | 0.68 | 0.68 | 0.79 | ||||
| Financial management | 1 (1–3) | 0.57 | 0.55 | 0.58 | ||||
All factor loadings rounded to two decimal points. Loadings <0.50 removed for clarity.
aIQR = 25th–75th centiles; all items included the full a score range of 1–7.
PC, principal component; Com’n, communication; EADL, Extended Activities of Daily Living.
The first two components extracted accounted for 66% of the total variance in responses. All items loaded strongly on the first principal component (i.e. above 0.55). Table 3 also shows a reasonably clear two-factor structure, with the 35 items falling into a Motor and a Cognitive factor. Within the EADL module, all items loaded on the Motor factor, with the exception of Financial management which loaded on the Cognitive factor. Similarly, the results of the four-factor analysis also showed show four clear, interpretable factors corresponding to the following dimensions of independence: Physical independence, Psychosocial independence, Communication and Extended Activities of Everyday Living (EADL). In this solution, Community Mobility loaded onto the EADL factor.
A modest degree of overlap was seen for some items. The Eating, Grooming and Dressing upper body items loaded onto both Motor and Cognitive factors and Swallowing loaded onto both the Physical and the Communication factors in the four-factor solution. For pragmatic reasons (and in line with the well-established Motor and Cognitive subscales of the FIM and FIM + FAM [16]), we elected to place all four of these items within the Motor and Physical parts of the scale. This led to the identification of two principal “domains” (Motor: 20 items (range score 20–140) and Cognitive: 15 items (range score 15–105)) and four “subscales” (Physical: 15 items (range score 15–105), Psychosocial: 9 items (range score 9–63), Communication: 6 items (range score 6–42) and EADL: 5 items (range score 5–35). These were then tested in the confirmatory analysis.
Stage 2 – Confirmatory Mokken analysis
Table 4 presents Loevinger’s H coefficient for the overall scale and each individual item within each scale for the full 35-item scale and the subscales of the two- and four-factor solutions provided by the EFA. The H coefficient of the full 35-item scale was 0.64 reflecting a strong scale. For the Motor and Cognitive scales, the H coefficient was 0.82 and 0.65, respectively, once again reflecting strong scales. The H coefficient values for individual items were high across all three scales and always well above the accepted 0.30 cut-off. In the four-factor solution, once again H coefficient values for each subscale were high, ranging from 0.67 to 0.82, indicative of strong scales. Individual item H coefficient values were also all high (i.e. >0.50) and all well above the accepted cut-off (i.e. H > 0.30).
Table 4.
H coefficient values from Mokken analysis for 30 item FIM + FAM and five EADL items and for two- and four-factor based solutions (n = 468).
| Two factors |
Four factors |
|||||||
|---|---|---|---|---|---|---|---|---|
| Median (IQR)a | Single factor Total scale |
Motor | Cognitive | Physical | Psycho-social | Com’n | EADL | |
| Eating | 5 (5–7) | 0.70 | 0.82 | 0.82 | ||||
| Swallowing | 7 (6–7) | 0.73 | 0.78 | 0.78 | ||||
| Grooming | 5 (4–7) | 0.69 | 0.80 | 0.80 | ||||
| Bathing | 4 (3–6) | 0.71 | 0.85 | 0.85 | ||||
| Dressing – upper | 5 (3–7) | 0.69 | 0.81 | 0.81 | ||||
| Dressing – lower | 4 (2–6) | 0.69 | 0.85 | 0.86 | ||||
| Toileting | 5 (1–7) | 0.68 | 0.86 | 0.86 | ||||
| Bladder management | 6 (3–7) | 0.65 | 0.77 | 0.77 | ||||
| Bowel management | 6 (3–7) | 0.63 | 0.77 | 0.77 | ||||
| Transfers – bed/chair | 5 (2–7) | 0.69 | 0.86 | 0.86 | ||||
| Transfers – toilet | 5 (2–6) | 0.68 | 0.86 | 0.86 | ||||
| Transfers – tub/shower | 4 (1–6) | 0.66 | 0.83 | 0.83 | ||||
| Car transfer | 3 (1–6) | 0.66 | 0.82 | 0.82 | ||||
| Locomotion | 5 (1–6) | 0.66 | 0.80 | 0.80 | ||||
| Stairs | 1 (1–6) | 0.66 | 0.84 | 0.84 | ||||
| Community mobility | 2 (1–3) | 0.70 | 0.79 | 0.68 | ||||
| Comprehension | 6 (5–7) | 0.56 | 0.68 | 0.73 | ||||
| Expression | 6 (3–7) | 0.56 | 0.66 | 0.77 | ||||
| Reading | 6 (4–7) | 0.54 | 0.64 | 0.72 | ||||
| Writing | 5 (2–6) | 0.54 | 0.58 | 0.70 | ||||
| Speech intelligibility | 6 (4–7) | 0.52 | 0.58 | 0.71 | ||||
| Social interaction | 6 (4–7) | 0.57 | 0.65 | 0.71 | ||||
| Emotional status | 6 (3–7) | 0.48 | 0.53 | 0.58 | ||||
| Adjustment | 4 (2–6) | 0.60 | 0.68 | 0.76 | ||||
| Use of leisure time | 6 (3–6) | 0.66 | 0.68 | 0.72 | ||||
| Problem solving | 5 (2–6) | 0.64 | 0.72 | 0.77 | ||||
| Memory | 5 (3–7) | 0.56 | 0.67 | 0.75 | ||||
| Orientation | 7 (4–7) | 0.63 | 0.69 | 0.76 | ||||
| Concentration | 6 (4–7) | 0.59 | 0.65 | 0.73 | ||||
| Safety awareness | 4 (2–6) | 0.63 | 0.71 | 0.75 | ||||
| Meals | 2 (1–5) | 0.68 | 0.77 | 0.76 | ||||
| Laundry | 1 (1–2) | 0.69 | 0.78 | 0.67 | ||||
| Housework | 1 (1–2) | 0.69 | 0.80 | 0.68 | ||||
| Shopping | 1 (1–3) | 0.68 | 0.75 | 0.72 | ||||
| Financial management | 1 (1–3) | 0.58 | 0.71 | 0.52 | ||||
| Scale H coefficient | 0.64 | 0.82 | 0.65 | 0.82 | 0.72 | 0.72 | 0.67 | |
aIQR = 25th–75th centiles; all items included the full a score range of 1–7.
Com’n, Communication; EADL, Extended Activities of Daily Living.
Consistency
Consistency was tested for these across the whole dataset. The full-scale reliability (internal consistency) was high with Cronbach’s α = 0.98 for the full scale and item-total correlations ranging from 0.56 to 0.88. Cronbach’s α was 0.97 and 0.96, respectively, for the Motor and Cognitive domains, and 0.97, 0.95, 0.92 and 0.90, respectively, for the Physical, Psychosocial, Communication and EADL subscales.
Responsiveness
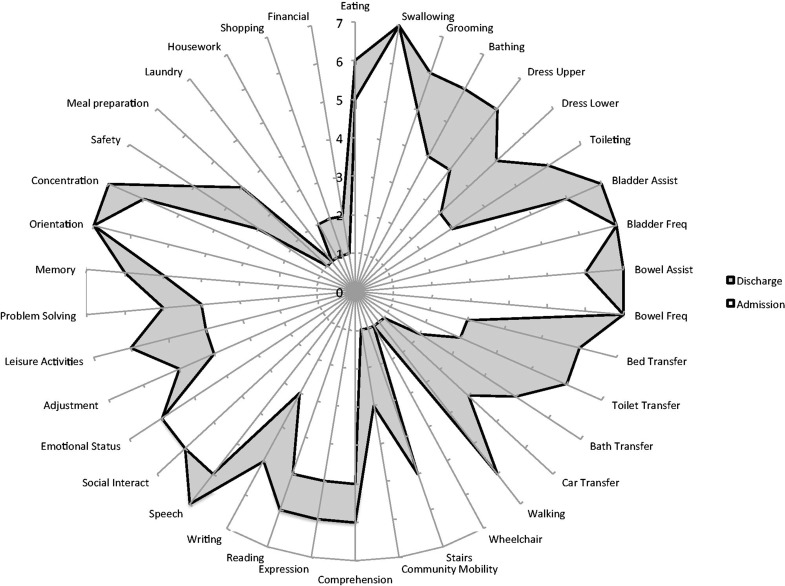
Change in domain and subscale scores between admission and discharge is shown in Table 5. Significant changes were seen in all four subscales with “large” effect sizes ranging from 0.86 to 1.29. Figure 1 shows a composite “FAM-splat” for the full sample, depicting the change in median scores at item level.
Table 5.
Scales and domain scores on admission and discharge, and change scores (n = 459).
| Admission |
Discharge |
Paired t tests |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | Mean difference | 95% CI | t | df | Effect size (Cohen’s d) | ||
| Subscales | ||||||||||
| Physical | 55.2 (26.0) | 15–105 | 77.2 (26.7) | 15–105 | 22.1 | 20.5, 23.6 | 27.6 | 457 | <0.001 | 1.29 |
| Psychosocial | 40.0 (15.9) | 9–63 | 46.9 (14.5) | 9–63 | 7.0 | 6.2, 7.7 | 18.1 | 457 | <0.001 | 0.86 |
| Communication | 22.9 (9.2) | 5–35 | 26.6 (8.1) | 5–35 | 3.7 | 3.3, 4.1 | 18.2 | 458 | <0.001 | 0.87 |
| EADL | 8.8 (5.1) | 6–41 | 16.7 (9.1) | 6–42 | 7.9 | 7.2, 8.5 | 22.7 | 458 | <0.001 | 1.21 |
| Domains | ||||||||||
| Motor | 63.9 (28.0) | 20–133 | 85.8 (30.7) | 19–132 | 22.0 | 20.3, 23.6 | 26.2 | 457 | <0.001 | 1.24 |
| Cognitive | 64.7 (24.4) | 15–105 | 76.3 (22.6) | 15–105 | 11.7 | 10.7, 12.7 | 22.0 | 457 | <0.001 | 1.05 |
EADL, Extended Activities of Daily Living; CI, confidence interval.
Figure 1.
Composite FAM-splat – a radar chart illustrating the median item scores on admission and discharge. The FAM-splat provides graphic presentation of the disability profile in a radar chart. The FIM + FAM items are arranged as “spokes” of the wheel and the levels from 1 (total dependence) to 7 (total independence) run from the centre outwards. Thus a perfect score would be demonstrated as a large circle. The shaded area represents the difference between the median scores on admission and discharge.
Discussion
The systematic review of existing literature on the psychometric properties of the UK FIM + FAM supported the psychometric robustness of the UK FIM + FAM, although as with the US version, ceiling effects can be a problem with outpatient samples. The analysis of new data from a large, mixed neuro-rehabilitation cohort demonstrated that the UK FIM + FAM has a highly acceptable level of internal consistency or reliability. Moreover, the internal consistency was high not simply for the full 35-item scale, but also for the two Motor and Cognitive domains and the four subscales (physical, psychosocial, communication and EADL) similarly identified by factor analysis. This suggests that the FIM + FAM is particularly useful measure as it can be used to derive a reliable, single score of overall independence and also yields specific information on four separate dimensions of independence. Mokken analysis confirmed that each of these constituted a reliable, unidimensional ordinal scale appropriate for rank-ordering persons.
In this analysis, we used a combination of parametric and non-parametric approaches for exploratory and confirmatory analysis, which to our knowledge is novel. We considered Mokken analysis uniquely suited for confirmatory analysis, given that it makes no assumptions about the nature of the distribution of responses on the item response scales and at the same time provides a robust index of unidimensionality. Whilst some might challenge this approach, we consider that it is helpful. If a plurality of approaches yields the same conclusions, it increases the likelihood that the findings are robust. This approach may also have application in other areas of rehabilitation measurement, where clinical data are typically ordinal and often are not normally distributed.
Our results are consistent with those of Hawley et al. [16] who reported a two-factor analysis of the US FIM + FAM with a large sample of patients with traumatic brain injury from 11 UK programmes. They also found a strong first principal component and two specific factors representing the motor and cognitive scales. However, they did not examine any alternative solutions such as the four-factor solution examined in the present study. Theirs is the only other factor analysis of the FIM + FAM that we are aware of, although other authors have examined dimensionality of the US FIM + FAM using Rasch analysis [14,15].
Limitations of the present research
The authors recognise a number of limitations to this study:
First, all the analyses were completed on patients from a single tertiary rehabilitation service. Even though they were drawn from a very large catchment area (in excess of five million), the results require replication in an independent population.
We used both admission and discharge scores, which were then randomised to the split samples used for exploratory and confirmatory analysis. This approach was used to ensure representation across the full score range for all items in both samples, which was achieved. However, as admission and discharge scores are expected to correlate, this may have inflated the degree of internal consistency giving an enhanced impression of homogeneity.
We were not able to test the more recently added “Work” item in the EADL, as there was insufficient representation in this dataset. This will require evaluation in future analyses.
Conclusion
Notwithstanding the above limitations, the findings demonstrate that the UK FIM + FAM is a reliable measure of independent functioning suitable for use in mixed inpatient neuro-rehabilitation settings. Our findings suggest that it may be acceptable to sum item scores into a single total figure, but that the instrument also provides meaningful scores on two and four sub-dimensions. In this study, all four subscales were responsive to change occurring during inpatient rehabilitation, with effect sizes ranging from 0.86 to 1.29. The data reported may inform power calculations for future studies that use the UK FIM + FAM as a primary outcome measure.
This study also provides the first examination of the relationship between the 30 FIM + FAM items and the five additional EADL items. The results suggested that these five items provide useful information on these more extended activities of everyday living and that they combined well with the existing 30 FIM + FAM items. In future publications, we plan to report the results of Rasch analysis to further explore the scaling properties of the UK FIM + FAM, as well as differential item functioning, across different groups of patients, according to impairment and localisation of neurological injury.
Acknowledgements
The authors are grateful to all the patients on the Regional Rehabilitation Unit, Northwick Park Hospital, who allowed their data to be used and the staff who performed the assessments. The authors are especially grateful to Heather Williams for managing the dataset.
Appendix 1
Clinimetric evaluation of the US FIM + FAM and UK FIM + FAM according to the Medical Outcomes Trust framework
| Attribute | Criteria | Evaluation – US version | Evaluation – UK version |
|---|---|---|---|
| Conceptual and measurement model | The rationale for and description of the concept and the populations that the measure is intended to assess | ||
| Clinical content and design | • A global measure of disability, designed primarily for use in patients with acquired brain injury. • FIM + FAM is a 30-item ordinal scale which extends the scope of the 18-item FIM, by adding 12 items primarily addressing psychosocial and cognitive aspects of function (which are often the principal factors limiting independent function in this group) [1]. • Items are scored on a seven-point scale ranging from 1 (total dependence) to 7 (complete independence). • Persons are rated by a multidisciplinary team of clinicians on the basis of observed performance not potential or capability, except for “Employability” which is rated on the basis of presumed capability. |
• The UK version retains the same overall structure as the US version – 12 FAM items added to the 18 FIM items are scored on the seven-point scale structure, and rated similarly by a multidisciplinary team on the basis of observed performance [2]. • Intended for a similar group of patients, the UK version was designed by a multicentre Development Group, in collaboration with the FAM originators, to address the subjective nature of some of the items. Ten “troublesome” items were identified and adjusted [2]. • The FIM items remain consistent across the two versions. • Item level definitions differ slightly for the UK FAM items (see “Content” below) • A five-item module addressing extended activity of daily living (EADL) was also developed [3]. |
|
| Dimensionality | Data from two studies of patients with TBI: n = 60 [4], n = 965 [5]; and one of stroke patients n = 376 [6]: • Two distinct principal components representing Motor and Cognitive functioning [5]. • Three Rasch studies reported a number of misfitting items for full 30 items and for Motor and Cognitive subscales analysed separately. Indicates neither the full scale nor two subscales are entirely unidimensional [4–6] |
Data from present study (n = 459) mixed neuro-rehabilitation inpatients:
• A strong principal component with all 35 items loading >0.55 on it. On rotation clear two-factor (Motor and Cognitive functioning) and four-factor solutions (Physical, Psychosocial, Communication and EADL) • Mokken scaling H coefficient values of 0.64, 0.82 and 0.65 for Full Scale, Motor and Cognitive scales, respectively (H > 0.50 indicates a “strong” scale). • H coefficients for four subscales Physical (H = 0.82), Psychosocial (H = 0.72), Communication (H = 0.72), EADL (H = 0.67). |
|
| Reliability | The degree to which the instrument is free from random error | ||
| Internal consistency | Data from two studies of patients with TBI: n = 965 [5], n = 60 [4]; and one of mixed neuro-rehabilitation, n = 149 [7] • Cronbach’s α for full scale FIM + FAM = 0.96, Motor subscale = 0.99, Cognitive subscale = 0.98 [5,7] • Rasch person and item consistency high at 0.91 and 0.93, respectively [4] |
Data from present study (n = 459) mixed neuro-rehabilitation inpatient sample:
• Cronbach’s α for Full Scale = 0.98, Motor subscale = 0.97 and Cognitive subscale = 0.96. • Cronbach’s α for Physical (0.97), Psychosocial (0.95), Communication (0.92) and EADL (0.90) subscales • Rasch analysis is currently underway – not yet published. |
|
| Reproducibility | Data from two studies of patients with neurological injury – mainly ABI n = 30 [8]; and severe TBI n = 53 [9]: • Kappa ranged from 0.35 to 0.95 for 29/30 items [8] • ICCs ranged from good (0.60–0.74) to excellent (0.75–1.0) for 29/30 items [9] |
Data from one vignette-based study of 28 clinician raters scoring individually and then in teams [2]: • Modest improvement in scoring accuracy of UK FIM + FAM in comparison with US version. Accuracy for individual item ratings improved from 75% (US) to 77% (UK) for and team accuracy from 84% to 86% [2] • Kappa ranged from 0.57 to 0.85 (for individual raters) and from 0.60 to 0.94 (for team ratings) across the 30 items. For EADL module, one vignette-based study: 50 vignettes and 12 clinician raters [3]: • Agreement with “gold standard scores” was high. Kappa ranging from 0.88 to 0.97 (individual ratings) and 0.93–1.0 (team ratings) [3]. • Inter-rater agreement ranged from Kappa 0.68 to 0.92 (individuals) and from 0.74 to 1.0 (teams). • Test–retest agreement Kappa values ranged from 0.92 to 1.0 (individuals) and 0.89–0.99 (teams) [3]: |
|
| Validity | The degree to which the instrument measures what it purports to measure | ||
| Content | • 30 items tap different aspects of six important aspects of independence: self-care, bowel and bladder management, mobility, communication, psychosocial function and cognition | • Covers the same range of function as the FAM, with the exception of employability • Three items are significantly altered: ○ “Use of Leisure time” replaces “Employability”; ○ “Concentration” replaces “Attention”: ○ “Safety Awareness” replaced “Safety Judgement”. • The five-item EADL module covered community-based activities: Meal preparation, Shopping, Laundry, Housework, Financial management [3]: • A sixth item (Work) has recently been added, but has not yet been fully tested. |
|
| Criterion-related | Not testable – no accepted gold standard currently exists | As for the US version – not testable | |
| Concurrent | Data from five studies of patients with TBI: n = 48 [10], n = 332 [1], n = 612 [11], n = 167 [12], n = 54 [13]; acquired brain injury n = 52 [14]; and inpatient neuro-rehabilitation (n = 149) [7]. • Positive Spearman correlations between five FIM + FAM dimensions (comprehension, problem-solving, memory, orientation, attention) and seven standard neuropsychological tests – 29/40 correlations significant [14]. • Correlation with the OPCS (rho 0.82) [13] • Correlations with the DRS were FIM + FAM motor 0.68, FIM + FAM cognitive 0.75 [1] • FAM employment item correlated −0.86 and −0.96 with DRS level of function and DRS employability items, respectively [10] • FAM items displayed modest advantage over the FIM in predicting employment and community integration at 24 months post-TBI [12]. • High correlations between FIM, FIM + FAM Total, BI, FIM motor, FIM Cognitive, FIM + FAM Motor, FIM + FAM Cognitive – Pearson’s r = 0.96–0.99 [7] • Direction, magnitude and pattern of FIM + FAM correlations with six measures of similar and different constructs were as predicted supporting its convergent and discriminant validity |
Data from one study of patients with acquired brain injuries (all causes) n = 164 [15]; and a mixed neuro-rehabilitation inpatient sample, n = 569 [16]. • Strong positive correlations between the FIM + FAM and the Barthel Index (rho = 0.84); moderate correlation (rho = 0.38) with personal goal attaiment scores [15] Strong positive correlation between UK FIM + FAM Motor scores and nursing dependency (NPDS) (rho 0.82–0.85) and between UK FIM + FAM Cognitive scores and NPDS Cognitive items (rho 0.76–0.77) [16] |
|
| Responsiveness | Ability to detect change over time where real changes occur | ||
| Change: admission to discharge | Data from two studies of patients with TBI n = 94 [17] and n = 105 [18]; and one inpatient neuro-rehabilitation, n = 149 [7]. • Standardised response means (n = 139) for FIM and FIM + FAM were 0.48 and 0.42, respectively [7]. • Difference between Outreach (n = 48) and Information (n = 46) groups on change scores not significant for total score and all five subscales due to ceiling effects at intake [17]. • Paired t tests showed only two items (bowel management and bladder management) did not show significant improvement (n = 105). Clinically meaningful improvements detected by 20/30 items in ≥60% of patients. • FIM + FAM Motor score below the ceiling predicted referral for on-going therapy services with a sensitivity of 0.88 and specificity of 0.65 [18]. |
Data from one study of n = 65 neuro-rehabilitation outpatients [19]; and n = 164 inpatients with acquired brain injury [15]; in addition to data from this study (n = 459)
• Neuro-rehabilitation outpatient programme. Mean admission–discharge change scores for Motor (12.0), Cognitive (7.3) and FIM + FAM total score (19.3) all clinically significant [19]. • Neuro-rehabilitation inpatient programme: Median admission–discharge change scores for Motor, Cognitive and FIM + FAM total score all clinically significant [15]. Data from this study confirm that significant changes were seen during inpatient rehabilitation across both FIM + FAM motor and cognitive domains (effect size 1.24 and 1.05, respectively) and across the four subscales (Effect sizes 0.86–1.29) |
|
| Floor/Ceiling effects | No. respondents with highest or lowest possible score | Data from five community-based TBI programmes (total N = 919) and one inpatient stroke study (n = 376) [6]: • Ceiling effects reported for community resident TBI survivors [4,10,11,17,18] and inpatient stroke rehabilitation [6] |
Data from one neuro-rehabilitation outpatient study, n = 65 [19]: • Ceiling effects on individual items at the start of programme ranged from 4.6% to 90.8% and at discharge from 18.5% to 93.8% [19] |
| Interpretability | The degree to which easily understood meaning can be assigned to the quantitative scores | ||
| Clinical meaning | • FIM + FAM provides two scores, one for motor independence and one for cognitive/behavioural independence, both of which are readily understood by clinicians • The cognitive items are noted to be more subjective and less “imageable” than the motor items, and so harder to rate reliably [20] |
• As for the US version, the UK FIM + FAM divides into Motor and Cognitive domains.
• The UK FIM + FAM software generates a “FAM-splat” providing an “at-a-glance” summary of change in the individual items of the FIM + FAM [21] |
|
| Burden | The time, effort or other demands of administering the instrument | ||
| Time to administer | • Approximately 35 min | • Approximately 30 min | |
| Alternative modes of administration | • Manual includes item level definitions and decision trees as for the FIM | • Manual includes item level definitions and decision trees as for the FIM | |
| Cultural and language adaptations | • UK FIM + FAM [2] • German adaptation and translation [22]. ICCs for single FAM items ranged from 0.08 to 0.87 for inter-rater and from 0.50 to 0.99 for intra-rater reliability. |
• Brazilian version [23] in Brazilian Portuguese. Intra-rater ICCs for 12 FAM items ranged from 0.60 to 0.94. ICCs for inter-rater reliability ranged from 0.51 to 0.90 across 12 items. | |
Data from this study are given in bold.
BI, Barthel Index; FIM, Functional Independence Measure; FAM, Functional Assessment Measure; FIM + FAM, Functional Independence Measure plus Functional Assessment Measure; ICC, Intra-Class Correlation.
References for Appendix 1
- 1.Hall KM, Hamilton BB, Gordon WA, Zasler ND. Characteristics and comparisons of functional assessment indices: disability Rating Scale, Functional Independence Measure, and Functional Assessment Measure. J Head Traum Rehabil. 1993;8:60–74. [Google Scholar]
- 2.Turner-Stokes L, Nyein K, Turner-Stokes T, Gatehouse C. The UK FIM + FAM: development and evaluation. Clin Rehabil. 1999;13:277–87. doi: 10.1191/026921599676896799. [DOI] [PubMed] [Google Scholar]
- 3.Law J, Fielding B, Jackson D, Turner-Stokes L. The UK FIM + FAM Extended Activities of Daily Living module: evaluation of scoring accuracy and reliability. Disabil Rehabil. 2009;31:825–30. doi: 10.1080/09638280802355049. [DOI] [PubMed] [Google Scholar]
- 4.Tesio L, Cantagallo A. The Functional Assessment Measure (FAM) in closed traumatic brain injury outpatients: a Rasch-based psychometric study. J Outcome Meas. 1998;2:79–96. [PubMed] [Google Scholar]
- 5.Hawley CA, Taylor R, Hellawell DJ, Pentland B. Use of the Functional Assessment Measure (FIM + FAM) in head injury rehabilitation: a psychometric analysis. J Neurol Neurosurg Psychiatr. 1999;67:749–54. doi: 10.1136/jnnp.67.6.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linn RT, Blair RS, Granger CV, et al. Does the Functional Assessment Measure (FAM) extend the functional independence measure (FIM) instrument? A Rasch analysis of stroke inpatients. J Outcome Meas. 1999;3:339–59. [PubMed] [Google Scholar]
- 7.Hobart JC, Lamping DL, Freeman JA, et al. Evidence-based measurement: which disability scale for neurologic rehabilitation? Neurology. 2001;57:639–44. doi: 10.1212/wnl.57.4.639. [DOI] [PubMed] [Google Scholar]
- 8.McPherson KM, Pentland B, Cudmore SF, Prescott RJ. An inter-rater reliability study of the Functional Assessment Measure (FIM + FAM) Disabil Rehabil. 1996;18:341–7. doi: 10.3109/09638289609165892. [DOI] [PubMed] [Google Scholar]
- 9.Donaghy S, Wass PJ. Interrater reliability of the Functional Assessment Measure in a brain injury rehabilitation program. Arch Phys Med Rehabil. 1998;79:1231–6. doi: 10.1016/s0003-9993(98)90267-2. [DOI] [PubMed] [Google Scholar]
- 10.Hall KM, Bushnik T, Lakisic-Kazazic B, et al. Assessing traumatic brain injury outcome measures for long-term follow-up of community-based individuals. Arch Phys Med Rehabil. 2001;82:367–74. doi: 10.1053/apmr.2001.21525. [DOI] [PubMed] [Google Scholar]
- 11.Hall KM, Mann N, High WMJ, et al. Functional measures after traumatic brain injury: ceiling effects of FIM, FIM + FAM, DRS, and CIQ. J Head Traum Rehabil. 1996;11:27–39. [Google Scholar]
- 12.Gurka JA, Felmingham KL, Baguley IJ, et al. Utility of the Functional Assessment Measure after discharge from inpatient rehabilitation. J Head Traum Rehabil. 1999;14:247–56. doi: 10.1097/00001199-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 13.McPherson KM, Pentland B. Disability in patients following traumatic brain injury – which measure? Int J Rehabil Res. 1997;20:1–10. doi: 10.1097/00004356-199703000-00001. [DOI] [PubMed] [Google Scholar]
- 14.McPherson K, Berry A, Pentland B. Relationships between cognitive impairments and functional performance after brain injury, as measured by the Functional Assessment Measure (FIM + FAM) Neuropsychol Rehabil. 1997;7:241–57. [Google Scholar]
- 15.Turner-Stokes L, Williams H, Johnson J. Goal Attainment Scaling: does it provide added value as a person-centred measure for evaluation outcome in neurorehabilitation following acquired brain injury? J Rehabil Med. 2009;41:528–35. doi: 10.2340/16501977-0383. [DOI] [PubMed] [Google Scholar]
- 16.Siegert RJ, Turner-Stokes L. Psychometric evaluation of the Northwick Park Dependency Scale. J Rehabil Med. 2010;42:936–43. doi: 10.2340/16501977-0602. [DOI] [PubMed] [Google Scholar]
- 17.Powell J, Heslin J, Greenwood R. Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial. J Neurol Neurosurg Psychiatr. 2002;72:193–202. doi: 10.1136/jnnp.72.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seel RT, Wright G, Wallace T, et al. The utility of the FIM + FAM for assessing traumatic brain injury day program outcomes. J Head Traum Rehabil. 2007;22:267–77. doi: 10.1097/01.HTR.0000290971.56130.c8. [DOI] [PubMed] [Google Scholar]
- 19.Wilson FC, Wheatley-Smith L, Downes C. Analysis of intensive outpatient neuro-rehabilitation outcomes using FIM + FAM(UK) NeuroRehabilitation. 2009;24:377–82. doi: 10.3233/NRE-2009-0492. [DOI] [PubMed] [Google Scholar]
- 20.Alcott D, Dixon K, Swann R. The reliability of the items of the Functional Assessment Measure (FAM): differences in abstractness between FAM items. Disabil Rehabil. 1997;19:355–8. doi: 10.3109/09638289709166551. [DOI] [PubMed] [Google Scholar]
- 21.Turner-Stokes L, Williams H, Sephton K, et al. Engaging the hearts and minds of clinicians in outcome measurement – the UK Rehabilitation Outcomes Collaborative approach. Disabil Rehabil. 2012;34:1871–9. doi: 10.3109/09638288.2012.670033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vogele B, Lehmann S, Aschlimann A. Translation, cross-cultural adaption, and reliability of the German version of the Functional Assessment Measure. Neurologie Rehabil. 2009;15:308–14. [Google Scholar]
- 23.Jorge L, Marchi G, Hara P, Battistella L. Brazilian version of the Functional Assessment Measure: cross-cultural adaptation and relaibility evaluation. Int J Rehabil Res. 2011;34:89–91. doi: 10.1097/MRR.0b013e32833ba55f. [DOI] [PubMed] [Google Scholar]
Declaration of interest
Outcome measurement is a specific research interest of our centre. The UK FIM + FAM were both developed through this department, but is disseminated free of charge to trained users. Neither of the authors has any personal financial interests in the work undertaken or the findings reported. This manuscript presents independent research commissioned by the National Institute for Health Research in England (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407-10185). The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. Financial support for the preparation of this manuscript was also provided by the Dunhill Medical Trust and the Luff Foundation.
References
- 1.Hamilton BB, Granger CV, Sherwin FS, et al. A uniform national data system for medical rehabilitation. In: Fuhrer JM, editor. Rehabilitation outcomes: analysis and measurement. Baltimore (MD): Brookes; 1987. pp. 137–47. [Google Scholar]
- 2.Hall KM, Hamilton BB, Gordon WA, Zasler ND. Characteristics and comparisons of functional assessment indices: Disability Rating Scale, Functional Independence Measure, and Functional Assessment Measure. J Head Traum Rehabil. 1993;8:60–74. [Google Scholar]
- 3.Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level Functional Independence Measure (FIM) Scand J Rehabil Med. 1994;26:115–19. [PubMed] [Google Scholar]
- 4.Granger CV, Hamilton BB, Linacre JM, et al. Performance profiles of the Functional Independence Measure. Am J Phys Med Rehabil. 1993;72:84–9. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Corrigan JD, Smith-Knapp K, Granger CV. Validity of the Functional Independence Measure for persons with traumatic brain injury. Arch Phys Med Rehabil. 1997;78:828–34. doi: 10.1016/s0003-9993(97)90195-7. [DOI] [PubMed] [Google Scholar]
- 6.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the Functional Independence Measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–32. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 7.Hall KM, Mann N, High WMJ, et al. Functional measures after traumatic brain injury: ceiling effects of FIM, FIM + FAM, DRS, and CIQ. J Head Traum Rehabil. 1996;11:27–39. [Google Scholar]
- 8. Wright J. The Center for Outcome Measurement in Brain Injury (COMBI). Available from: http://www.tbims.org/combi [last accessed 17 Dec 2012]
- 9.Turner-Stokes L, Nyein K, Turner-Stokes T, Gatehouse C. The UK FIM + FAM: development and evaluation. Clin Rehabil. 1999;13:277–87. doi: 10.1191/026921599676896799. [DOI] [PubMed] [Google Scholar]
- 10.Law J, Fielding B, Jackson D, Turner-Stokes L. The UK FIM + FAM Extended Activities of Daily Living module: evaluation of scoring accuracy and reliability. Disabil Rehabil. 2009;31:825–30. doi: 10.1080/09638280802355049. [DOI] [PubMed] [Google Scholar]
- 11.Turner-Stokes L, Sutch S, Dredge R. Healthcare tariffs for specialist inpatient neurorehabilitation services: rationale and development of a UK casemix and costing methodology. Clin Rehabil. 2011;26:264–79. doi: 10.1177/0269215511417467. [DOI] [PubMed] [Google Scholar]
- 12.Turner-Stokes L, Williams H, Sephton K, et al. Engaging the hearts and minds of clinicians in outcome measurement – the UK Rehabilitation Outcomes Collaborative approach. Disabil Rehabil. 2012;34:1871–9. doi: 10.3109/09638288.2012.670033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Linn RT, Blair RS, Granger CV, et al. Does the Functional Assessment Measure (FAM) extend the Functional Independence Measure (FIM) instrument? A Rasch analysis of stroke inpatients. J Outcome Meas. 1999;3:339–59. [PubMed] [Google Scholar]
- 15.Tesio L, Cantagallo A. The Functional Assessment Measure (FAM) in closed traumatic brain injury outpatients: a Rasch-based psychometric study. J Outcome Meas. 1998;2:79–96. [PubMed] [Google Scholar]
- 16.Hawley CA, Taylor R, Hellawell DJ, Pentland B. Use of the Functional Assessment Measure (FIM + FAM) in head injury rehabilitation: a psychometric analysis. J Neurol Neurosurg Psychiatr. 1999;67:749–54. doi: 10.1136/jnnp.67.6.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hobart JC, Lamping DL, Freeman JA, et al. Evidence-based measurement: which disability scale for neurologic rehabilitation? Neurology. 2001;57:639–44. doi: 10.1212/wnl.57.4.639. [DOI] [PubMed] [Google Scholar]
- 18.Donaghy S, Wass PJ. Interrater reliability of the Functional Assessment Measure in a brain injury rehabilitation program. Arch Phys Med Rehabil. 1998;79:1231–6. doi: 10.1016/s0003-9993(98)90267-2. [DOI] [PubMed] [Google Scholar]
- 19.McPherson K, Berry A, Pentland B. Relationships between cognitive impairments and functional performance after brain injury, as measured by the Functional Assessment Measure (FIM + FAM) Neuropsychol Rehabil. 1997;7:241–57. [Google Scholar]
- 20.McPherson KM, Pentland B. Disability in patients following traumatic brain injury – which measure? Int J Rehabil Res. 1997;20:1–10. doi: 10.1097/00004356-199703000-00001. [DOI] [PubMed] [Google Scholar]
- 21.McPherson KM, Pentland B, Cudmore SF, Prescott RJ. An inter-rater reliability study of the Functional Assessment Measure (FIM + FAM) Disabil Rehabil. 1996;18:341–7. doi: 10.3109/09638289609165892. [DOI] [PubMed] [Google Scholar]
- 22.Hall KM, Bushnik T, Lakisic-Kazazic B, et al. Assessing traumatic brain injury outcome measures for long-term follow-up of community-based individuals. Arch Phys Med Rehabil. 2001;82:367–74. doi: 10.1053/apmr.2001.21525. [DOI] [PubMed] [Google Scholar]
- 23.Powell J, Heslin J, Greenwood R. Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial. J Neurol Neurosurg Psychiatr. 2002;72:193–202. doi: 10.1136/jnnp.72.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seel RT, Wright G, Wallace T, et al. The utility of the FIM + FAM for assessing traumatic brain injury day program outcomes. J Head Traum Rehabil. 2007;22:267–77. doi: 10.1097/01.HTR.0000290971.56130.c8. [DOI] [PubMed] [Google Scholar]
- 25.Vogele B, Lehmann S, Aschlimann A. Translation, cross-cultural adaption, and reliability of the German version of the Functional Assessment Measure. Neurologie Rehabil. 2009;15:308–14. [Google Scholar]
- 26.Alcott D, Dixon K, Swann R. The reliability of the items of the Functional Assessment Measure (FAM): differences in abstractness between FAM items. Disabil Rehabil. 1997;19:355–8. doi: 10.3109/09638289709166551. [DOI] [PubMed] [Google Scholar]
- 27.Gurka JA, Felmingham KL, Baguley IJ, et al. Utility of the Functional Assessment Measure after discharge from inpatient rehabilitation. J Head Traum Rehabil. 1999;14:247–56. doi: 10.1097/00001199-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Wilson FC, Wheatley-Smith L, Downes C. Analysis of intensive outpatient neuro-rehabilitation outcomes using FIM + FAM(UK) NeuroRehabilitation. 2009;24:377–82. doi: 10.3233/NRE-2009-0492. [DOI] [PubMed] [Google Scholar]
- 29.Turner-Stokes L, Williams H, Johnson J. Goal attainment scaling: does it provide added value as a person-centred measure for evaluation outcome in neurorehabilitation following acquired brain injury? J Rehabil Med. 2009;41:528–35. doi: 10.2340/16501977-0383. [DOI] [PubMed] [Google Scholar]
- 30.Siegert RJ, Turner-Stokes L. Psychometric evaluation of the Northwick Park Dependency Scale. J Rehabil Med. 2010;42:936–43. doi: 10.2340/16501977-0602. [DOI] [PubMed] [Google Scholar]
- 31.Jorge L, Marchi G, Hara P, Battistella L. Brazilian version of the Functional Assessment Measure: cross-cultural adaptation and relaibility evaluation. Int J Rehabil Res. 2011;34:89–91. doi: 10.1097/MRR.0b013e32833ba55f. [DOI] [PubMed] [Google Scholar]
- 32.Tabachnick BG, Fidell LS. Using multivariate statistics. 4th. Needham Heights (MA): Allyn & Bacon; 2001. [Google Scholar]
- 33.Pett MA, Lackey NR, Sullivan JJ. Making sense of factor analysis: the use of factor analysis for instrument development in health care research. Thousand Oaks (CA): Sage Publications; 2003. [Google Scholar]
- 34.Thompson B. Exploratory and confirmatory factor analysis: understanding concepts and applications. Washington (DC): American Psychological Association; 2004. [Google Scholar]
- 35. Molenaar IW, Sijtsma K, Boer P. MSP5 for Windows: a program for Mokken scale analysis for polytomous items: (Version 5.0) User’s Manual. Groningen: iec ProGAMMA; 2000.
- 36.Mokken RJ, Lewis C. A nonparametric approach to the analysis of dichotomous items. Appl Psychol Meas. 1982;6:417–30. [Google Scholar]
- 37.Sijtsma K, Molenaar IW. Introduction to nonparametric item response theory. In: Jaeger RM, editor. Measurement methods for the social sciences 5. Thousand Oaks (CA): Sage Publications; 2002. [Google Scholar]
- 38.Van Schuur WH. Mokken scale analysis: between the Guttman scale and parametric item response theory. Polit Anal. 2003;11:139–63. [Google Scholar]
- 39.Loevinger J. The technic of homogeneous tests compared with some aspects of “scale analysis” and factor analysis. Psychol Bull. 1948;45:507–30. doi: 10.1037/h0055827. [DOI] [PubMed] [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioural sciences. 2nd. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. [Google Scholar]