Summary
Tourette syndrome (TS) is a neurodevelopmental disorder characterized by multiple tics, which can require active intervention. It is recognized that behavioral techniques, especially habit reversal therapy (HRT), can offer an effective alternative or complement to pharmacotherapy in this setting. We conducted a systematic literature review to evaluate the efficacy of HRT in TS and other chronic tic disorders (CTDs). Our search was restricted to randomized controlled trials that used standardized diagnostic and outcome measures to compare the efficacy of HRT against a control treatment. We identified five relevant studies, which included 353 patients. Significant post-treatment reductions in tic severity scores (range: 18.3%–37.5%) were seen in the HRT groups across all studies. Current evidence suggests that HRT can significantly reduce tic severity in both adults and children with TS and other CTDs. Further head-to-head studies are needed to compare the efficacy of HRT with other behavioral interventions for tic management.
Keywords: behavioral therapy , habit reversal , tics , Tourette syndrome , treatment
Introduction
Tourette syndrome (TS) is a neurodevelopmental disorder characterized by the presence, for over a year, of multiple motor tics and at least one vocal or phonic tic ( Cavanna et al., 2009). Tics are defined as repetitive, involuntary, non-rhythmic, sudden movements or vocalizations that can involve discrete muscle groups and often present between the ages of four and six years ( Woods et al., 2007 ; Robertson and Cavanna, 2008), with a male:female ratio of approximately 4:1 ( Cavanna et al., 2009). It has been shown that tics can affect health-related quality of life across the lifespan ( Hassan and Cavanna, 2012) and require active treatment intervention ( Eddy et al., 2011, Cavanna et al., 2008).
The European clinical guidelines for TS and other tic disorders state that the typical antipsychotics haloperidol and pimozide are the most effective medications for tic management ( Roessner et al., 2011). Although there is strong evidence in favor of pharmacological intervention, it is also acknowledged that there are drawbacks to this approach. For example, the currently available agents are rarely able to eradicate tics completely. Furthermore, antidopaminergic medications are commonly associated with unwanted effects, including weight gain, sedation, extrapyramidal effects and dyskinesia. A decline in the use of neuroleptics, due to patients being unable to tolerate their frequent and often severe adverse effects, was recently reported ( Roessner et al., 2011).
Psychosocial management of TS and tic disorders, in combination with pharmacological interventions ( Frank and Cavanna, 2013), has long been considered. Behavioral therapies are the psychological interventions most commonly used, with habit reversal therapy (HRT) considered one of the most efficacious strategies. HRT is also the most researched of all behavioral therapies for TS, having first been mentioned in 1973 as a method of suppressing nervous tics ( Azrin and Nunn, 1973). Since then, strong evidence has accumulated on the usefulness, in tic disorders, of HRT combined with response prevention (ERP), whilst studies on other behavioral interventions have given inconsistent findings ( Frank and Cavanna, 2013).
Habit reversal therapy consists of several components, including awareness training with self-monitoring, relaxation training and competing response training ( Azrin and Peterson, 1988). Regardless of the way in which HRT is administered (e.g. alone or as part of treatment packages such as Comprehensive Behavioral Intervention for Tics, CBIT), awareness training and competing response training are widely accepted to be the two key components of this intervention ( Azrin and Nunn, 1973; Woods and Miltenberger, 1995). Arguably, HRT offers an effective non-pharmacological method of suppressing tics, without causing unwanted effects such as those associated with pharmacotherapy.
The majority of studies on HRT have involved only small numbers of patients, and in several cases just one individual ( Woods et al., 2007 ). Only a few studies have recruited large cohorts of participants and randomized subjects to two different treatment options. The aim of this systematic literature review was to analyze these randomized studies of HRT in order to accurately evaluate its efficacy and to provide an up-to-date and reliable evidence base on the effect of HRT on tic suppression in TS and other chronic tic disorders (CTDs).
Methods
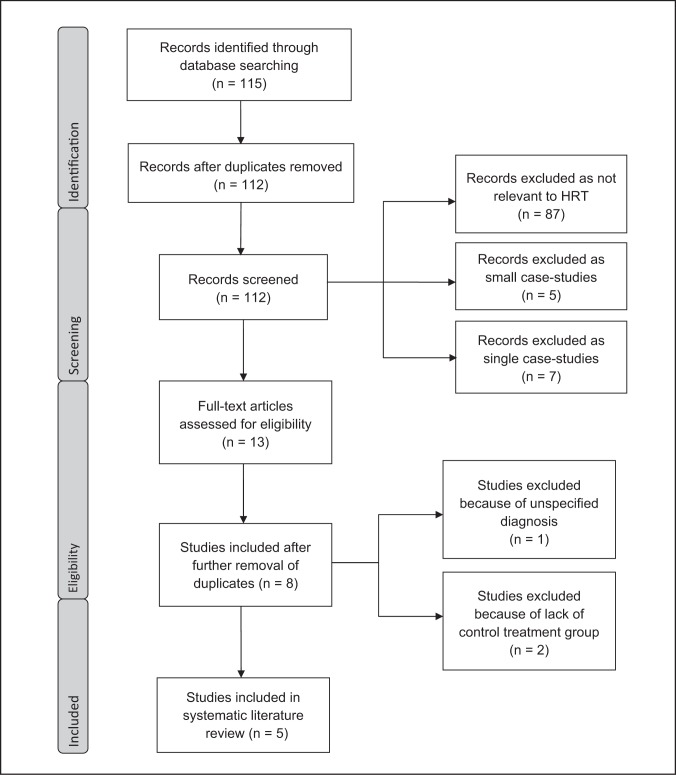
For this systematic literature review, the healthcare databases PubMed and PsycINFO were searched following the methodology outlined in the Prisma guidelines ( Moher et al., 2009) ( Fig. 1 ). First, using PubMed, relevant search terms were entered (“Tourette*”, “tic*”) using the “Map to Thesaurus” tool. The subject headings “Tourette syndrome” OR “Tics” OR “Tic disorders” AND “habit revers*” OR “comprehensive behav*” were entered, screening titles and abstracts of papers written in English. This search produced a list of 36 papers. The process was then repeated for the PsycINFO database, and this second search yielded 79 results. The results of the two literature searches were analyzed and duplicates were removed. This left 112 results, which were then screened for inclusion in the present systematic literature review. Only original studies looking at the effectiveness of HRT in the treatment of TS and other CTDs, in children or adults, could be included. With regard to study paradigms, we focused on the best level of evidence, i.e. randomized controlled trials involving HRT. The majority of the papers mentioning HRT did not describe studies specifically focusing on this technique (n=87) and were therefore excluded; others were excluded because they reported small case studies carried out on fewer than thirty patients (n=5), or presented single case studies (n=7). Judging by their abstracts, thirteen papers appeared to meet the search criteria detailed above. After eliminating results which had escaped the initial removal of duplicates, eight studies remained which were then assessed more closely for their eligibility to be included in the present review. Only studies that used a standardized method for the diagnosis of tic disorders, such as the DSM-IV-TR criteria, could be included. Eligible studies also used a standardized outcome measure to quantify the efficacy of treatment, with the Yale Global Tic Severity Scale (YGTSS) being the preferred choice. Ideally, studies included would be blinded to those rating the effectiveness of treatment and an intention-to-treat (ITT) analysis would be implemented, however these were not strict criteria for inclusion.
Figure 1 .
PRISMA flow diagram for the inclusion and exclusion of studies
A further three studies were eventually excluded: an early study by Azrin et al. (1980) because the patients were not selected according to specific criteria for the diagnosis of TS or other tic disorders, and two others ( Azrin and Peterson, 1990; O’Connor et al., 2001) because they did not compare HRT with a control treatment option, instead using a waiting list as the control group. This left five studies which met all the criteria for inclusion in our systematic literature review.
Results
Table I sets out the main findings of the five relevant studies identified by our search.
Table I .
Large randomized controlled trials of habit reversal therapy for tic disorders.
| Study | No. of patients | No. (%) of males | Diagnosis | Adults/Children | Mean age (SD) years | Comparator group | Outcome measure |
|---|---|---|---|---|---|---|---|
| Wilhelm et al. 2003 | 32 | 16 (50.0%) | TS | Adults | 36.2 (12.7) | SP | YGTSS |
| Verdellen et al. 2004 | 43 | 34 (79.1%) | TS | Both | 20.6 (12.1) | ERP | YGTSS |
| Deckersbach et al. 2006 | 30 | 17 (56.7%) | TS | Adults | 35.1 (12.2) | SP | YGTSS |
| Piacentini et al. 2010 | 126 | 99 (78.6%) | TS/CTD | Children | 11.7 (2.3) | SP | YGTSS |
| Wilhelm et al. 2012 | 122 | 78 (63.9%) | TS/CTD | Both | 31.6 (13.7) | SP | YGTSS |
Abbreviations: TS=Tourette syndrome; CTD=chronic tic disorder; SP=supportive psychotherapy; ERP=exposure with response prevention; YGTSS=Yale Global Tic Severity Scale
Three of these studies ( Wilhelm et al., 2003; Deckersbach et al., 2006; Wilhelm et al., 2012) only included adults (aged 18 years or older), while one study ( Piacentini et al., 2010) focused solely on the effect of HRT in children (under 18 years). All of the studies included both males and females. A total of 353 patients were included in this review, of whom 326 met formal diagnostic criteria for TS (92.4%) and 244 were males (69.1%). The number of patients included in each study ranged from 30 to 126, with a mean of 70.6 participants per study. Three studies included patients with a specific diagnosis of TS only, whereas the largest two studies included patients with both TS and other CTDs. Four studies compared the efficacy of HRT with that of supportive psychotherapy, and one compared HRT with ERP. The YGTSS was used to measure tic severity in all of the included studies.
The specific elements of the HRT intervention varied across the five studies ( Table II ): Verdellen et al. (2004) focused on competing response and awareness training only, whilst Piacentini et al. (2010) and Wilhelm et al. (2012) implemented the most comprehensive treatment protocols.
Table II .
Components of habit reversal therapy used in the randomized controlled trials.
| Study | Competing response training | Awareness training | Relaxation training | Function-based interventions |
|---|---|---|---|---|
| Wilhelm et al. 2003 | ✓ | ✓ | ✓ | ✓ |
| Verdellen et al. 2004 | ✓ | ✓ | ||
| Deckersbach et al. 2006 | ✓ | ✓ | ✓ | ✓ |
| Piacentini et al. 2010 | ✓ | ✓ | ✓ | ✓ |
| Wilhelm et al. 2012 | ✓ | ✓ | ✓ | ✓ |
Table III (over) highlights the key findings of the studies included in this review. In all five studies, HRT was shown to substantially reduce tic severity.
Table III .
Difference in tic severity before and after habit reversal therapy and control treatment in the randomized controlled trials.
| Study | Treatment group |
YGTSS
|
||
|---|---|---|---|---|
| Pre-treatment | Post-treatment | % change | ||
| Wilhelm et al. 2003 | Habit reversal | 30.5 | 19.8 | −35.1 |
| Supportive psychotherapy | 26.6 | 26.9 | 1.1 | |
| Verdellen et al. 2004 | Habit reversal | 24.1 | 19.7 | −18.3 |
| Exposure with response prevention | 26.2 | 17.6 | −32.8 | |
| Deckersbach et al. 2006 | Habit reversal | 29.3 | 18.3 | −37.5 |
| Supportive psychotherapy | 27.7 | 26.8 | −3.2 | |
| Piacentini et al. 2010 | Habit reversal | 24.7 | 17.1 | −30.8 |
| Supportive psychotherapy | 24.6 | 21.1 | −14.2 | |
| Wilhelm et al. 2012 | Habit reversal | 24.0 | 17.8 | −25.8 |
| Supportive psychotherapy | 21.8 | 19.3 | −11.5 | |
Abbreviations: YGTSS=Yale Global Tic Severity Scale.
Most of the studies included follow-up data ranging from 3 to 10 months in order to assess whether the findings were maintained over time. Table IV (over) shows the YGTSS scores recorded at follow-up in the reviewed studies. As shown by all the studies that provided long-term data, patients followed up after undergoing HRT appeared to experience continued reduction of tic severity.
Table IV .
Tic severity at follow-up after habit reversal therapy or control treatment in the randomized controlled trials.
| Study | Treatment group (no. of patients) | YGTSS score | Follow-up (no. of patients) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Pre-Tx | Post-Tx | 3 months | 6 months | 10 months | % change since pre-Tx | ||
| Wilhelm et al. 2003 | HR (16) | 30.5 | 19.8 | 21 (10) | −31.1 | ||
| SP (13) | 26.6 | 26.9 | 23.8 (11) | −10.5 | |||
| Verdellen et al. 2004 | HR (22) | 24.1 | 19.7 | 13.5 (13) | −44.0 | ||
| ERP (21) | 26.2 | 17.6 | 14 (12) | −46.6 | |||
| Deckersbach et al. 2006 | HR (15) | 29.3 | 18.3 | 18.4 (8) | −37.2 | ||
| SP (15) | 27.7 | 26.8 | 26.6 (10) | −4.0 | |||
| Piacentini et al. 2010 | HR (61) | 24.7 | 17.1 | 13.9 (28) | 13.3 (23) | −46.2 | |
| SP (65) | 24.6 | 21.1 | 9.9 (12) | 10.4 (8) | −57.7 | ||
| Wilhelm et al. 2012 | HR (63) | 24.0 | 17.8 | ||||
| SP (59) | 21.8 | 19.3 | |||||
Abbreviations: YGTSS=Yale Global Tic Severity Scale; Pre-Tx=pre-treatment; Post-Tx=post-treatment; HR=habit reversal; SP=supportive psychotherapy; ERP=exposure with response prevention.
Discussion
The aim of this literature review was to provide an up-to-date source of evidence-based information on the efficacy of HRT in the treatment of TS and other CTDs, considering the results of suitable randomized controlled trials. Our main finding was that HRT can significantly reduce tic severity in both adults and children with TS and other CTDs, which is in line with the results of the first randomized trial of HRT in the treatment of tic disorders ( Azrin et al., 1980) and of subsequent small case studies ( Woods et al., 2007).
The male:female ratio of the patients identified in this review supports previous evidence that TS is about four times more common in males than in females ( Azrin and Nunn, 1973). The studies by Wilhelm et al. ( 2003 , 2012 ), Deckersbach et al. (2006), and Piacentini et al. (2010) all compared HRT with supportive psychotherapy. Each of these studies found that HRT was much more effective at reducing tic severity, producing a mean reduction of 32.3% (range −25.8% to −37.5%). This contrasts with the absent or limited reduction in symptoms observed with supportive psychotherapy, which averaged 7.0% (range +1.1% to −14.2%). The study by Verdellen et al. (2004) compared HRT with ERP and found that both therapies significantly improved symptoms in patients with TS.
However, in this study ( Verdellen et al., 2004), HRT did not appear to reduce tic severity to the same extent as in the other four studies reviewed in the present article. In addition, the proportion of patients who showed a >30% reduction in tic severity was 58% in the ERP group, which was substantially greater than the 28% found by Wilhelm et al. (2003) in the HRT group.
Although all the reviewed studies met our strict inclusion criteria, we nevertheless identified a number of methodological limitations. In particular, the follow-up protocols presented problems in all the studies. Wilhelm et al. (2003) carried out follow-up assessments at 10 months, which is the longest time of all the reviewed studies. They found that a significant improvement in tic severity was still apparent in the HRT group at 10 months, although the mean YGTSS scores had risen since the treatment intervention. Conversely, mean YGTSS scores in the supportive psychotherapy group had fallen. As a result, the post-treatment difference between YGTSS scores in the HRT and supportive psychotherapy groups was no longer significant at the final follow-up. For this reason, even though this study gave promising short-term results, its long-term findings were less convincing. In the study by Verdellen et al. (2004), overall follow-up rates at three months were relatively low: only 59% of the patients from the HRT group and 57% of those from the ERP group. Of these, 12 patients (8 in the HRT group and 4 in the ERP group) did not complete the follow-up. Most importantly, due to the crossover design of the study in the post-treatment phase, 25 of the follow-up patients (68%) subsequently received the opposite treatment to the initial one they were assigned to. This made it impossible to extrapolate any information about the long-term efficacy of either treatment, and to see how they compared over this time period. In this study, as well as in the ones by Piacentini et al. (2010) and Deckersbach et al. (2006), a significant number of patients initially assessed were subsequently lost to follow-up, which introduced a bias in the evaluation of follow-up tic severity scores. Moreover, in the study by Piacentini et al. (2010), only selected patients deemed to be “positive responders” to treatment, i.e. patients who had improved significantly with the initial treatment intervention, were given booster sessions at three-month intervals. A greater proportion of patients from the HRT group were evaluated as positive responders compared with the supportive psychotherapy group, resulting in a possible bias in follow-up tic severity scores.
The study by Wilhelm et al. (2012) used a similar paradigm to that of Piacentini et al. (2010) in order to investigate the efficacy of HRT as part of a tailored comprehensive intervention (CBIT). Again, only participants showing positive results were invited for follow-up assessments. The reliability of the follow-up data was reduced by the fact that of the 24 participants invited, only 15 were available for assessment. Additionally, the authors rated clinical improvement at 6-month follow-up using the Clinical Global Impression-Improvement Scale rather than the YGTSS, thus limiting the accuracy and generalizability of the findings.
A further set of problems with the examined literature relates to the blinding procedure and ITT analysis. In the study by Wilhelm et al. (2003), the interviewers who rated the YGTSS were not blinded to which treatment group the patients were in. Moreover, although patients who dropped out before the eighth session of their treatment (two in the HRT group, one in the supportive psychotherapy group) were excluded from the analysis, those who dropped out after this point (one in the HRT group, two in the supportive psychotherapy group) were included. In the more recent study by Wilhelm et al. (2012), tic severity was assessed by a blinded independent clinician and conventional ITT analysis was performed. In the study by Deckersbach et al. (2006), the YGTSS ratings, the clinical diagnoses and the treatment interventions for the patients were all performed by the same author. Therefore, it is likely that this study was not assessor-blinded. Moreover, in this study two of the initial 32 patients dropped out. Data from these two patients were not included in the analysis. However, when the analysis was repeated using an ITT paradigm, incorporating the two drop-out patients, there was no change in the significance of the results. In contrast to these articles, the studies by Verdellen et al. (2004) and Piacentini et al. (2010) were both assessor-blinded and used an ITT analysis, thus increasing the reliability and validity of their findings.
Treatment protocols varied widely across the reviewed studies. Although all had a treatment group allocated to HRT, the specific elements incorporated into the treatment intervention and the frequency with which it was administered differed between the studies. For example, the protocols adopted by Piacentini et al. (2010) and Wilhelm et al. (2012) included eight HRT sessions, whereas the protocols of the other studies included ten ( Verdellen et al., 2004) or fourteen ( Wilhelm et al., 2003; Deckersbach et al., 2006) sessions. Likewise, although the five studies used competing response and awareness training as part of the HRT procedure, the other components of the HRT intervention were not consistent across all the studies. Finally, outcome data may have been affected by the different rates of psychiatric disorders across the studies: comorbid attention deficit and hyperactivity disorder was reported in 30.2% of patients in the study by Verdellen et al. (2004), 27.9% in the study by Wilhelm et al. (2012), and 26.2% in the study by Piacentini et al. (2010), whereas obsessive-compulsive disorder was reported in 19.0% of patients in the study by Piacentini et al. (2010), 18.0% in the study by Wilhelm et al. (2012), and 14% in the study by Verdellen et al. (2004). Deckersbach et al. (2006) reported only figures for comorbid obsessive-compulsive disorder, which was present in 30.0% of patients, whilst Wilhelm et al. (2003) did not report rates of comorbid diagnoses. This systematic review provides an up-to-date summary of the existing scientific evidence for the use of HRT in the treatment of tics in TS and other CTDs. However, there are some intrinsic limitations to our literature review strategy. For example, relevant information might have been missed by choosing to use selective inclusion criteria for the reviewed studies. Moreover, there emerged significant differences between the studies in covariate variables, such as gender and age. Although such differences are acknowledged in this review, adjustment for these variables was not performed. Furthermore, other potential confounders, such as socio-economic status, ethnic origin, etc., were not considered.
The overall results of our systematic literature review reinforce the conclusions of the recently published European clinical guidelines on behavioral and psychosocial treatments for TS and other CTDs ( Verdellen et al., 2011), which suggest that HRT is an effective treatment option for reducing tic severity in both adults and children. This supports the clinicians’ perception that HRT should be considered as a first-line behavioral treatment for obtaining tic suppression in patients of all ages ( Verdellen et al., 2011). However, currently there are only a few specialists who are trained and experienced enough to administer HRT sessions ( Piacentini et al., 2010). More teaching and training in this technique are required in order to expand its application to the treatment of tics throughout healthcare systems ( Woods et al., 2007 ). Existing evidence would justify a more widespread diffusion of HRT, which in turn would allow further research on larger and clinically diverse cohorts of patients.
This review has highlighted some potential areas for further research. Verdellen et al. (2004) noted statistically significant reductions in tic severity in patients treated with ERP. The use of this behavioral therapy is supported by relatively little research in TS populations. Future studies should investigate the efficacy of ERP in larger samples of patients with TS and other CTDs, in order to allow reliable comparisons with HRT. More research into whether behavioral therapies could represent a valid complement or alternative to pharmacological intervention for tic management is also required. Some patients in the reviewed studies were taking medication whilst undergoing the behavioral interventions, and others were not. Research comparing tic severity in patients receiving first-choice antidopaminergic medication versus those receiving HRT could shed more light on the real efficacy of HRT compared with drug therapy. Quality of life should also be taken into consideration, in addition to tic severity. By replacing pharmacotherapy with HRT, adverse effects may be reduced and quality of life improved. Even if tic severity scores remain higher in patients undergoing HRT compared with those on medications, patients who experience severe side effects from their medication may prefer this compromise. In complex conditions like TS, the choice between different treatment strategies should always take into account both subjective and objective factors, in addition the best level of evidence from the scientific literature.
Acknowledgments
The authors are grateful to the Tourette Syndrome Association-USA and Tourettes Action-UK for their continuing support.
References
- Azrin NH , Nunn RG . Habit reversal: a method of eliminating nervous habits and tics . Behav Res Ther . 1973 ; 11 : 619 – 628 . doi: 10.1016/0005-7967(73)90119-8. [DOI] [PubMed] [Google Scholar]
- Azrin NH , Nunn RG , Frantz SE . Habit reversal vs negative practice treatment of nervous tics . Behav Ther . 1980 ; 11 : 169 – 178 . doi: 10.1016/0005-7967(80)90086-8. [DOI] [PubMed] [Google Scholar]
- Azrin NH , Peterson AL . Habit reversal for the treatment of Tourette syndrome . Behav Res Ther . 1988 ; 26 : 347 – 351 . doi: 10.1016/0005-7967(88)90089-7. [DOI] [PubMed] [Google Scholar]
- Azrin NH , Peterson AL . Treatment of Tourette syndrome by habit reversal: a waiting-list control group comparison . Behav Ther . 1990 ; 21 : 305 – 318 . [Google Scholar]
- Cavanna AE , Schrag A , Morley D , et al. The Gilles de la Tourette syndrome-quality of life scale (GTS-QOL): Development and validation . Neurology . 2008 ; 71 : 1410 – 1416 . doi: 10.1212/01.wnl.0000327890.02893.61. [DOI] [PubMed] [Google Scholar]
- Cavanna AE , Servo S , Monaco F , et al. The behavioural spectrum of Gilles de la Tourette syndrome . J Neuropsychiatry Clin Neurosci . 2009 ; 21 : 13 – 23 . doi: 10.1176/jnp.2009.21.1.13. [DOI] [PubMed] [Google Scholar]
- Deckersbach T , Rauch S , Buhlmann U , et al. Habit reversal versus supportive psychotherapy in Tourette’s disorder: a randomized controlled trial and predictors of treatment response . Behav Res Ther . 2006 ; 44 : 1079 – 1090 . doi: 10.1016/j.brat.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Eddy CM , Rizzo R , Gulisano M , et al. Quality of life in young people with Tourette syndrome: a controlled study . J Neurol . 2011 ; 258 : 291 – 301 . doi: 10.1007/s00415-010-5754-6. [DOI] [PubMed] [Google Scholar]
- Frank M , Cavanna AE . Behavioural treatments for Tourette syndrome: An evidence-based review . Behav Neurol . 2013 doi: 10.3233/BEN-120309. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan N , Cavanna AE . The prognosis of Tourette syndrome: implications for clinical practice . Funct Neurol . 2012 ; 27 : 23 – 27 . [PMC free article] [PubMed] [Google Scholar]
- Moher D , Liberati A , Tetzlaff J , et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement . PLoS Med . 2009 ; 6 : e1000097 . doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor KP , Brault M , Robillard S , et al. Evaluation of a cognitive-behavioural program for the management of chronic tic and habit disorders . Behav Res Ther . 2001 ; 39 : 667 – 681 . doi: 10.1016/s0005-7967(00)00048-6. [DOI] [PubMed] [Google Scholar]
- Piacentini J , Woods DW , Scahill L , et al. Behavior therapy for children with Tourette disorder: a randomized controlled trial . JAMA . 2010 ; 303 : 1929 – 1937 . doi: 10.1001/jama.2010.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson M , Cavanna A . Tourette syndrome: The facts . 2nd ed . Oxford : Oxford University Press ; 2008 . [Google Scholar]
- Roessner V , Plessen KJ , Rothenberger A , et al. European clinical guidelines for Tourette syndrome and other tic disorders. Part II: pharmacological treatment . Eur Child Adolesc Psychiatry . 2011 ; 20 : 173 – 196 . doi: 10.1007/s00787-011-0163-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdellen CW , Keijsers GP , Cath DC , et al. Exposure with response prevention versus habit reversal in Tourette’s syndrome: a controlled study . Behav Res Ther . 2004 ; 42 : 501 – 511 . doi: 10.1016/S0005-7967(03)00154-2. [DOI] [PubMed] [Google Scholar]
- Verdellen C , van de Griendt J , Hartmann A , et al. European clinical guidelines for Tourette syndrome and other tic disorders. Part III: behavioural and psychosocial interventions . Eur Child Adolesc Psychiatry . 2011 ; 20 : 197 – 207 . doi: 10.1007/s00787-011-0167-3. [DOI] [PubMed] [Google Scholar]
- Wilhelm S , Deckersbach T , Coffey BJ , et al. Habit reversal versus supportive psychotherapy for Tourette’s disorder: a randomized controlled trial . Am J Psychiatry . 2003 ; 160 : 1175 – 1177 . doi: 10.1176/appi.ajp.160.6.1175. [DOI] [PubMed] [Google Scholar]
- Wilhelm S , Peterson AL , Piacentini J , et al. Randomized trial of behavior therapy for adults with Tourette syndrome . Arch Gen Psychiatry . 2012 ; 69 : 795 – 803 . doi: 10.1001/archgenpsychiatry.2011.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods DW , Miltenberger RG . Habit reversal: a review of applications and variations . J Behav Ther Exp Psychiatry . 1995 ; 26 : 123 – 131 . doi: 10.1016/0005-7916(95)00009-o. [DOI] [PubMed] [Google Scholar]
- Woods DW , Piacentini JC , Walkup JT , editors. Treating Tourette syndrome and tic disorders: A guide for practitioners . New York : The Guilford Press ; 2007 . [Google Scholar]