Abstract
Posttraumatic growth (PTG) after cancer can minimize the emotional impact of disease and treatment; however, the facilitators of PTG, including support-seeking, are unclear. We examined the role of support-seeking on PTG among 604 breast cancer survivors ages 40–64 from the Health Eating, Activity, and Lifestyle (HEAL) Study. Multivariable linear regression was used to examine predictors of support-seeking (participation in support groups and confiding in healthcare providers) as well as the the relationship between support-seeking and PTG. Support program participation was moderate (61.1%) compared to the high rates of confiding in health professionals (88.6%), and African Americans (AA) were less likely to report participating than Non-Hispanic Whites (NHWs) (Odds Ratio: 0.14 (0.08, 0.23)). The mean (SD) PTG score was 48.8 (27.4) (range 0–105). Support program participation (β=10.4) and confiding in healthcare providers (β=12.9) were associated (p<0.001) with higher PTG. In analyses stratified by race/ethnicity, PTG was significantly higher in both NHW and AA support program participants (p<0.01), but not significantly higher in Hispanics/Latinas. Confiding in a healthcare provider was only associated with PTG for NHWs (p= 0.02). Support program experiences and patient-provider encounters should be examined to determine which attributes facilitate PTG in diverse populations.
Keywords: breast cancer, cancer survivor, support group, patient-provider support, posttraumatic growth
Introduction
Social support is associated with improved quality of life (QOL) (Sammarco & Konecny, 2008) and health-related quality of life (HRQOL) (Montazeri, 2008), and in some cases, increased survival time (Kroenke, Kubzansky, Schernhammer, Holmes, & Kawachi, 2006) and lower overall mortality (Beasley et al., 2010) among women with breast cancer. In addition to support from traditional social resources, cancer survivors may seek some degree of support from their healthcare providers directly during the clinical encounter or by requesting referrals to organized support groups (Hewitt, Breen, & Devesa, 1999). Organized support groups function as supportive social networks and are cost-effective interventions that may improve patient QOL (Zabalegui, Sanchez, Sanchez, & Juando, 2005). Previous research indicates that cancer support group participants are more likely to be female, single, have higher educational attainment, and report more social support than non-participants (Grande, Myers, & Sutton, 2006). In addition, breast cancer survivors are among the highest users of cancer support groups (Owen, Goldstein, Lee, Breen, & Rowland, 2007), and these groups often fill important gaps in socialization needs among cancer survivors (Galvan, Buki, & Garces, 2009). Support programs can provide a space for participants to gain both enhanced behavioral capacity and increased self-efficacy as well as provide an opportunity for observational learning and reinforcement (Simoni, Franks, Lehavot, & Yard, 2011).
Although satisfaction and improvements in health-related quality of life (HRQOL) may be high among cancer survivors (Grassi, Sabato, Rossi, Marmai, & Biancosino, 2010; Leadbeater, 2004; Schou, Ekeberg, Karesen, & Sorensen, 2008; Till, 2003), the psychological processes that lead to this improvement remain unclear. One such process may be posttraumatic growth (PTG), which is a concept encompassing positive changes in self-perception, interpersonal relationships, and/or life philosophy following a traumatic life event (Tedeschi & Calhoun, 1996). Posttraumatic growth may buffer the negative impacts of cancer on psychological and social quality of life (Silva, Moreira, & Canavarro, 2011). Thus, understanding potentially modifiable factors that faciliate PTG, including support-seeking throughout the cancer survivorship continuum, has the potential to reduce the emotional toll of cancer. Although most research examining PTG among cancer survivors has focused on personal or clinical characteristics, some studies have investigated the role of social support for benefit finding and adjustment to cancer (Helgeson & Cohen, 1996; Kinsinger et al., 2006; Schroevers, Helgeson, Sanderman, & Ranchor, 2010; Schwarzer, Luszczynska, Boehmer, Taubert, & Knoll, 2006; Scrignaro, Barni, & Magrin, 2011; Silva, Crespo, & Canavarro, 2012). Schroevers and colleagues (2010) found that support provision, particularly during the time following diagnosis, was critically important for the endurance of PTG; this finding was recently replicated in a longitudinal study that demonstrated that PTG mediated the relationship between coping during breast surgery to quality of life and depression posttreatment, approximately one year later (Silva, et al., 2012).
The scant research on PTG in Non-White female cancer survivors has shown that both African American (Bellizzi et al., 2010) and Hispanic (Smith, Dalen, Bernard, & Baumgartner, 2008) cancer survivors report higher levels of PTG than Whites. These findings have been partially explained by higher reported levels of religiosity or spirituality among African American and Hispanic/Latinas (Schaefer, Blazer, & Koenig, 2008). Given the extensive literature documenting persistent cancer health disparities (Masi & Olopade, 2005) and differences in perceptions of breast cancer treatment (Masi & Gehlert, 2009) for racial and ethnic minorities, it seems likely that other cultural or healthcare system factors (including support service seeking) may be related to differential PTG across racial and ethnic groups. Support program seeking has been shown to be lower among racial/ethnic minority patients (Owen, et al., 2007), for reasons including concerns about racism, language barriers, logistical difficulties such as inadequate transportation and competing familial demands, and cultural differences in attitudes toward the introspection assumed to be part of participating in support groups (Avis et al., 2008; Coward, 2005).
Support programs can provide a place for social comparison, either upward (identifying with survivors who are doing well), downward (contrasting to other survivors who are doing worse), or parallel (Bellizzi, Blank, & Oakes, 2006). Upward social comparison has been linked to increased posttraumatic growth (Morris, Chambers, Campbell, Dwyer, & Dunn, 2011), indicating a mechanism by which peer-support may be linked to more positive assessment of cancer. Support-seeking from other cancer survivors and from healthcare providers may influence PTG, and interventions that facilitate PTG have the potential to improve quality of life and reduce the emotional toll of cancer for some people. Given the potential for interventions to build on support-seeking, we expand on a previous analysis by the study team of individual predictors of PTG (i.e. age, employment status, race, religiosity, and stage of disease), which found that African American survivors reported higher levels of PTG than White women, and that religiosity mediated this relationship (Bellizzi, et al., 2010). The current study seeks to understand relationships between support-seeking (i.e. participation in support programs and confiding in healthcare providers) and PTG in a diverse population of breast cancer survivors. We hypothesize that support-seeking is positively related to PTG. To inform future interventions that facilitate PTG in diverse populations, we explore how these relationships differ between race/ethnicity and expect different patterns among survivors of different race/ethnicities, although given a paucity of research in this area, we do not hypothesize a direction of difference. We also describe those survivors who participate in support programs and confide in healthcare providers in order to understand who utilizes these resources.
Methods
The current inquiry analyzed data from the Health, Eating, Activity, and Lifestyle (HEAL) Study, a multi-center prospective study of female breast cancer patients diagnosed with in situ or Stages I – IIIA disease (Irwin et al., 2003). Women diagnosed with their first primary breast cancer were recruited from three Surveillance Epidemiology and End Results (SEER) registries (New Mexico, Western Washington, and Los Angeles County, California). Recruitment criteria for the HEAL study varied slightly across the three sites. In New Mexico, 399 women aged 29–64 years, diagnosed between 1996–1999, and living in Bernalillo, Santa Fe, Sandoval, Valencia, or Taos counties were recruited. In Washington, 202 women aged 40–64 years, diagnosed between 1997–1998, and living in King, Pierce, or Snohomish counties were recruited. In Los Angeles, 366 Black/African American women, diagnosed between 1995–1998, aged 35–64 years at diagnosis, and who participated in the Women’s Contraceptive and Reproductive Experiences Study or a parallel case-control study were recruited. The study was performed with the approval of the institutional review boards of the participating centers, in accord with an assurance filed with and approved by the US Department of Health and Human Services.
Data for the current study included three assessement points: the baseline interview (range of 2–12 months after diagnosis) and two follow-up assessments approximately 30 months after diagnosis (range 24–41) and 39 months after diagnosis (range 24–59). The first two assessments collected information on demographic, lifestyle and clinical variables. The 39-month follow-up questionnaire assessed health-related quality of life (HRQOL) including PTG and support-seeking behavior. In order to achieve consistency in the age ranges and race/ethnicities across study sites and race/ethnicities consistent, only women between the ages of 40 and 64 were included in the current anaylsis. A total of 669 women aged 40–64 at diagnosis completed the HRQOL assessment. Women diagnosed with a new primary breast cancer or recurrence between the time of enrollment and receipt of the HRQOL questionnaire (n = 48) or individuals for whom there was missing data on marital status (n = 12), religiosity (n = 3), or PTG (n=2) were excluded from the final analyses, leaving a final sample size of 604 women.
Measures
Respondents were asked in the HRQOL questionnaire about cancer-related support programs that they participated in around the time of diagnosis: support groups with other cancer survivors, one-on-one interactions to receive support or information from other breast cancer survivors, groups to provide medical information about breast cancer and/or recovery, and groups to help change exercise or eating habits, or other types of support groups. Participants were also asked to rate their level of satisfaction with the their support activity as “very satisfied,” “satisfied,” “unsatisfied,” or “very unsatisfied.” In addition to support program participation, support-seeking was also assessed by asking participants about how much (not at all, some, a lot, not applicable) they could confide in certain persons (family: spouse, children, other relatives; friends and neighbors; and healthcare providers: nurses, treating physicians, psychiatrist, psychologist) around the time of diagnosis. Responses were dichotomized into no and yes.
Covariates abstracted from SEER registry records and medical records included age at diagnosis, stage at diagnosis and treatment regimen (chemotherapy and/or radiation in addition to surgery). Participants provided information on race/ethnicity, education, current employment and marital status at time of interview, and comorbidities. Religiosity was measured using the Duke Religion Index, a five-item scale that measures importance of religion and spirituality, with higher scores indicating higher levels of religiosity (Bellizzi, et al., 2010; Koenig, Parkerson, & Meador, 1997; Storch et al., 2004). Cronbach’s alpha for the religiosity scale in our sample was 0.65. Income was excluded as a predictor due to extensive missing data (n = 32) and its moderate correlation with education (r = 0.35, p < 0.001).
To measure PTG, the Posttraumatic Growth Inventory (PTGI) was employed. The PTGI is a 21-item scale that measures perceived postitive outcomes following a negative life event (Tedeschi & Calhoun, 1996). Domains include items on relationships with others, new possibilities, appreciation of life, spirituality, and personal strength. The range for the entire 21-item scale is 0–105, with high scores indicating high levels of growth. A previous confirmatory factor analysis indicated that a one-factor PTGI model explained the majority of the variance in the HEAL study population (Bellizzi, et al., 2010); therefore the PTGI was analyzed as a unidimensional factor. Cronbach’s alpha for the scale in our sample was 0.96.
Statistical Analysis
Multiple logistic regression models examined the relationships between support program participation and confiding in healthcare providers and the following variables: age at diagnosis (continuous), race/ethnicity (Non-Hispanic White, Black/African-American, Hispanic/Latina, or other), educational attainment (high school or less, some college or technical school, college graduate, or other), current employment status (employed, not employed/retired), current marital status (married/living as married, never married, widowed/divorced/separated), stage at diagnosis (in situ, localized, regional), number of comorbidities that limit activity (0, 1, or ≥ 2), summary of cancer treatment (surgery only, surgery and chemotherapy, surgery and radiation, all three), religiosity (continuous), and confiding in family and friends (yes or no).
Posttraumatic growth was regressed on support program participation and confiding, adjusting for the sociodemographic and clinical factors mentioned previously. All associations were considered statistically significant at p<0.05. Posttraumatic growth was modeled overall and then stratified by race/ethnicity (Non-Hispanic White, African American, and Hispanic/Latina) to explore differences in parameter estimates across racial and ethnic groups. Analyses were conducted in SAS version 9.2 (SAS Institute Inc., Cary, NC). To assess the clinical significance of differences in PTG by support-seeking characteristics, we calculated effect sizes for differences in PTG between groups using Cohen’s d. Effect sizes of 0.20–0.49 are considered small, 0.50–0.79 moderate, and ≥ 0.80 considered large (Cohen, 1977).
Results
Support Program Participation
A total of 394 (60.4%) women indicated that they had participated in at least one support program since their diagnosis. One-on-one support interactions had the highest attendance (n = 304), followed by support groups with other cancer survivors (n = 147), groups that provided medical information (n = 125), health promotion groups (n = 77), and other groups (n = 71). The most common type of “other” group that participants reported was family and friends (n = 29), followed by church or other type of religious groups (n = 10). Support program satisfaction was high and did not vary significantly by race/ethnicity (all p values > 0.12); 86.7% of women reported being satisfied or very satisfied with the support programs they attended.
The proportion of women who participated in support progams was significantly lower in African Americans (AA) (30.6%, adj OR = 0.14 (0.08, 0.23) than in Non-Hispanic Whites (NHW) (75.5%). Support program participation increased with higher levels of educational attainment. Women with at least some college or technical school education and those with graduate school experience were more likely to report support program participation than those with a high school degree or less educational experience (p<0.05). Support program participation did not significantly differ by age at diagnosis, employment status, marital status, treatment history, stage at diagnosis, or presence of limiting comorbidities.
Although income was moderately correlated with education (ρ 0.35, p<0.001) and thus not included in the multivariable regression for support program participation, women reporting lower annual household income levels also reported significantly lower support program participation: ≤ $20,000: 45.5%; $20,000–70,000: 64.8%; >$70,000: 63.4% (χ2 = 12.7, p=0.005).
Confiding in healthcare providers
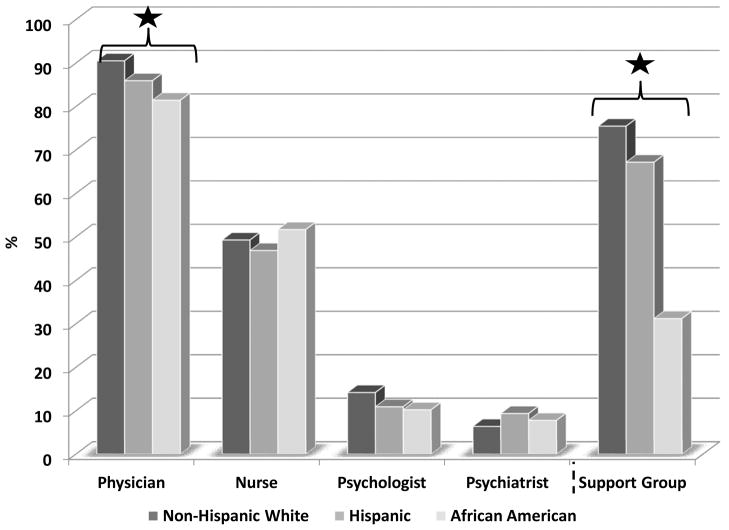
Individuals who confided in friends and neighbors (adj OR: 3.37 (1.34, 8.52) and those reporting participation in a support program (adj OR: 1.85 (1.02, 3.36) were significantly more likely to confide in healthcare providers. No other variables were associated with confiding in healthcare providers. Figure 1 shows the percentages of survivors within specific racial/ethnic groups who confided in specific types of healthcare providers (physicians, nurses, psychologists, and psychiatrists) and the percentage of those who participated in support programs. Confiding in physicians was high in all racial/ethnic groups (81–91%), intermediate for nurses (46–52%) and very low (6–14%) for psychologists and psychiatrists. Both African American (AA) and Hispanic/Latinas (HL) were less likely to confide in physicians and participate in support programs than NHW (p<0.01).
Figure 1.
Percentage of survivors who confided in healthcare providers (physician, nurse, psychologist, or psychiatrist) and participated in support programs. Stars indicate significant (p<0.01) variability across race/ethnicity.
Posttraumatic Growth
Posttraumatic growth scores ranged from 0 to 105 with a mean (SD) of 48.8 (27.4). Mean PTG scores by race/ethnicity were as follows: NHW: 47.3 (25.4) AA: 49.8 (30.5) HL: 53.2 (27.7). The overall model predicting PTG was significant (F(21, 575)) = 5.29, p<0.0001), accounting for 13% of the variance (adjusted r2). Table 2 gives multivariable linear regression estimates of PTG. In addition to support program participation and confiding in a healthcare provider, race/ethnicity, age, stage at diagnosis, and religiosity were all significantly associated with PTG. African American women reported significantly higher adjusted PTG scores than NHW, and PTG significantly decreased with age. Women with localized or regional stage at diagnosis had higher PTG, and women with higher levels of religiosity reported lower PTG.
Table 2.
Multivariable model examining factors associated with posttraumatic growth
| Adjusted r² = 0.17 | |||
|---|---|---|---|
| Parameter | B (SE) | β | p |
| Race/ethnicity | |||
| Non-Hispanic White | Ref | Ref | 0.04 |
| Black/African-American | 7.1 (3.1) | 0.12 | 0.02 |
| Hispanic/Latina | 5.8 (3.8) | 0.06 | 0.13 |
| Other | 9.3 (5.7) | 0.06 | 0.10 |
| Age at diagnosis | −0.5 (0.2) | −0.12 | 0.01 |
| Unemployed/retired vs. employed | −5.1 (2.6) | −0.08 | 0.05 |
| Staging | |||
| In situ | Ref | Ref | 0.047 |
| Localized | 8.2 (2.6) | 0.15 | 0.002 |
| Regional | 14.8 (3.1) | 0.22 | <0.0001 |
| Religiosity | −0.7 (0.2) | −0.12 | 0.002 |
| Confided in healthcare providers | 12.9 (3.5) | 0.15 | 0.0002 |
| Participated in a support program | 10.4 (2.4) | 0.19 | <0.0001 |
Parameter estimates adjusted for all other variables present in the model as well as time since diagnosis, summary of treatment (surgery only, surgery/chemotherapy, surgery/radiation, or surgery/chemotherapy/radiation), number of limiting comorbidities, education, marital status, and confiding in family, friends, and neighbors.
Bolded numbers represent estimates statistically significant at p<0.05.
Support program participants reported higher adjusted mean PTG scores (mean (SE) = 46.8 (4.6), p<0.0001) than non-participants (mean (SE) = 37.1 (4.2), Cohen’s d = 0.36). Survivors who reported confiding in any healthcare providers (mean (SE) = 48.4 (4.1)), also had significantly higher PTG than those who did not (mean (SE) = 35.6 (4.1), Cohen’s d=0.48, p<0.0001). Figure 2 shows adjusted PTG mean scores for survivors who did or did not confide in healthcare providers by support program participation; no evidence of interaction between these two variables on PTG was apparent and an interaction term was not significant in regression modeling (p=0.86).
Figure 2.
Adjusted means (SE) for posttraumatic growth for support program participants (confided in a healthcare provider at diagnosis: 52.5 (6.7); did not: 39.0. (7.7), p=0.005) and non-participants (confided in a healthcare provider at diagnosis: 44.4 (6.7); did not: 31.9 (7.3), p=0.02). Interaction was not significant (p=0.86). Means adjusted for age, race/ethnicity, educational attainment, employment status, marital status, treatment summary, stage at diagnosis, number of limiting comorbidities, time since diagnosis, religiosity, and confiding in family and friends/neighbors.
Posttraumatic Growth by Race/Ethnicity
In the stratified analyses, the highest predictor of PTG among NHW was stage at diagnosis; survivors with either localized or regional disease reported significantly higher growth than survivors with in situ disease. Among AA, age at diagnosis was the strongest predictor. With each increasing year of age among AA, PTG decreased on average by 1.0 point. The model did not fit the data well for HL, probably due to the smaller sample size.
Support program participation predicted PTG in both NHW (Cohen’s d=0.60) and AA (Cohen’s d=0.43), with AA demonstrating higher scores than NHW (13.0 (4.9) vs. 10.4 (3.2) points). An inverse relationship between support program participation and PTG was observed for Hispanics although the association was not statistically significant. Confiding in a healthcare provider was significantly associated with PTG only for NHW (Cohen’s d=0.59), and confiders reported, on average, a 11.7 point increase in growth (5.1) after adjustment for other factors.
Discussion
The current study expands previous work on the correlates of PTG in breast cancer survivors to include support seeking from programs and from healthcare providers. Posttraumatic growth scores were slightly lower than have been reported in other recent studies of cancer survivors (Nenova, Duhamel, Zemon, Rini, & Redd, 2011; Silva, et al., 2011), although they were comparable to PTG reported by women with benign gynecologic disease (Posluszny, Baum, Edwards, & Dew, 2011). Our findings were also consistent with previous work linking use of emotional support to higher PTG in head and neck cancer patients (Llewellyn et al., 2011).
Participating in support programs and confiding in healthcare providers appear to be positively associated with PTG among African American and Non-Hispanic White breast cancer survivors, and both of these variables have small to moderate effect sizes. Given that AA reported significantly lower support program participation than NHW, it is possible that there is either disparate access to a resource with promising mental health benefits or alternatively, that more African Americans choose not to use these resources. Furthermore, although confiding in healthcare providers was associated with higher PTG, this effect was limited to NHW. Lower participation in cancer support groups for minority survivors has been associated with recruitment challenges related to mistrust due to historical mistreatment in research, competing demands of other life stressors, and general misgivings about healthcare professionals extending to group facilitators (Avis, et al., 2008; Coward, 2005). In addition, AA women may be seeking support from sources other than traditional support programs, such as church or community groups, and the ways in which the current and most other studies on this topic assess support program participation may be too narrowly defined and not reflective of these mechanisms of support (Michalec, Van Willigen, Wilson, Schreier, & Williams, 2004).
Although neither confiding in family nor in friends was significantly related to support group participation, some studies have found higher participation among women with larger social networks and increased social support (Grande, et al., 2006; Stevens & Duttlinger, 1998), whereas others have indicated that women with high levels of social support may not seek or choose to participate in a support group (Napoles-Springer, Ortiz, O’Brien, Diaz-Mendez, & Perez-Stable, 2007). Confiding in healthcare providers and participating in support programs offer opportunities for breast cancer survivors to use healthcare system resources to fulfill psychosocial needs. Survivors who are willing and able to open up to providers may also be more willing to join and share in a support programs which may lead to higher posttraumatic growth associated with the cancer experience. Support programs in turn may equip survivors with tools they need to discuss their cancer experiences more openly with their providers. Alternatively, physicians and other providers may have influence over survivors coping processes simply by listening to them and directing them to services and other peer support to foster coping, benefit-finding, and growth.
Very few cancer survivors report that their physicians recommend use of support programs. In a population-based survey of 1844 cancer survivors, 78.4% reported that a support group had been beneficial and 71.8% reported having told their physician about the support group, but only 10.2% had physicians who recommend participation (Owen, et al., 2007). Satisfaction with support groups has been associated with higher perceived clinician support (Steginga, Pinnock, Gardner, Gardiner, & Dunn, 2005). Survivors’ interactions with providers and peers may provide opportunities for enhancing coping experiences. Trust in healthcare providers, particularly when established from illness onset, has been shown to predict higher quality of life and reduced depression (Vogel, Leonhart, & Helmes, 2009). Only NHW women appeared to experience positive PTG associated with confiding in healthcare providers, however, this may be partially due to differences in actual and perceived care experiences among racial and ethnic groups. Siminoff and colleagues (2006) analyzed data from patient-physician encounters with women newly diagnosed with breast cancer and found that the time physicians spent engaged in communication with their patients varied by patient demographics, predominantly by race/ethnicity, such that physicians spent more time relationship-building with White vs. Non-White patients. Unfortunately physician’s race/ethnicity could not be examined in this study due to the low numbers of Non-White physicians (Siminoff, Graham, & Gordon, 2006). Relationship-building may encourage women to seek other support sources and begin to view their cancer experience more positively. Finding this association only in NHW may in part reflect a lower level of closeness or trust with physicians or lack of access to healthcare providers among AA and HL.
A few other findings warrant discussion. The higher PTG scores reported among women with tumors of more advanced stage at diagnosis has been demonstrated in breast cancer survivors (Bellizzi & Blank, 2006; Tomich & Helgeson, 2004), but an association between lower stage at diagnosis and higher PTG has also been documented (Mols, Vingerhoets, Coebergh, & van de Poll-Franse, 2009). Our study did not include women with invasive cancer, which may in part explain the positive association between higher stage at diagnosis and PTG. The inverse association between higher religiosity scores and lower PTG contradicts previous findings in the literature (Ai, Hall, Pargament, & Tice, 2012; Rand et al., 2011) and suggests a few possible interpretations. It may be that survivors with high religious orientation are less likely to view their cancer experience as traumatic, and thus do not exhibit high levels of growth following the experience. Alternatively, for some individuals, perhaps high religiosity interferes and dampens the effect of the original trauma over time (Schaefer, et al., 2008). Future studies using longitudinal designs should help clarify this relationship.
Strengths and Limitations
The current study is limited by its cross-sectional design, which makes it difficult to assess pathways by which support-seeking may influence PTG. Growth was measured at one time point but is likely a dynamic process which could reflect variability if assessed over time. Moreover, PTG is a construct that represents perceived growth, rather than a measure of actual psychological growth objectivel measured. The religiosity scale included has a moderate, rather than high value of Cronbach’s α, which may have contributed to the inverse association we found between religiosity and PTG. In addition, participants were asked to recall how much they confided in their social support networks near the time of diagnosis, a recall time of approximately three to four years, which could lead to some degree of under-reporting, if, for example, some who did participate in support programs did not recall their experience. In addition, the composition of study participants by race/ethnicity was confounded by with the fact that only AA women were recruited in Los Angeles County and nearly all of the HL women were recruited in New Mexico (N=60). Thus, it is impossible to determine whether the lower support group participation rates among AA women is attributable to racial or geographic factors. This study only includes women diagnosed with breast cancer between the ages of 40 and 64 and may not generalize to survivors older or younger at diagnosis. We do not have information about actual or perceived availability and access to support programs among the survivors surveyed. A natural next step is to explore barriers to support program participation in populations with low participation. We also lack data on physician characteristics, including their race or ethnicity. However, at present the majority of research on the relationship between patients’ race/ethnicity and the nature of their interactions with their physicians is based on studies that predominantly involve White physicians.
Despite these limitations, however, the current study advances knowledge by identifying potential contributors to PTG. The HEAL study population is a large and diverse cohort of breast cancer survivors that allows for the exploration of factors related to growth across different sub-populations. The large numbers of African Americans and Hispanics participating allowed us to draw some generalizable conclusions about these groups, which have been largely omitted from previous PTG research. We expand on previous analyses of factors related to PTG to include support seeking and suggest that work evaluating both support group experiences and patient-provider interactions could have considerable impact on benefit-finding after cancer.
Clinical Implications
In conclusion, support-seeking among breast cancer survivors is associated with PTG. Survivors who participated in support programs and confided in healthcare providers around the time of diagnosis reported the highest levels of PTG approximately 2–4 years post diagnosis. Differences in the relationship between support-seeking and PTG were evident across racial/ethnic groups, even after adjustment for religiosity. Although the association between support program participation and PTG was significant for both AA and NHW survivors, support program participation was significantly lower in AA survivors indicating that some individuals may be missing out on the benefits of this intervention. The relationship between confiding in healthcare providers and PTG was limited to NHWs. Given previous equivocal research on the complex relationships between PTG and health-related quality of life (Bellizzi, et al., 2010; Lelorain, Bonnaud-Antignac, & Florin, 2010), future work should examine the elements of emotional support provided by healthcare providers to survivors and how those might facilitate both PTG and quality of life. Efforts to recruit and retain African Amerian and other minority cancer survivors to support groups should consider working with local community leaders to build credibility, increase awareness and trust, and incorporate a comprehensive needs assessment to identify and alleviate barriers to participation (Coward, 2005). In addition, support group leaders should consider the needs of their individual members, perhaps by discussing preferences at the onset of membership to identify concerns (eg. socioeconomic factors, immigration/documentation concerns, and racism) and prioritize them according to the preferences of their participants(Greene, 1996).
Understanding the factors that facilitate PTG after cancer across diverse groups of cancer survivors has the potential to provide insights for the development of interventions that may lessen the negative emotional impact of cancer. Interventions to bolster growth among cancer survivors should consider social support provision tailored to diverse groups of cancer survivors.
Table 1.
Sample description and variables examined for association with social support-seeking among breast cancer survivors, N = 604
| Total | Support program participation adjusted OR (95% | Confiding in a healthcare provider adjusted OR (95% | |||
|---|---|---|---|---|---|
| N (%) | N (%) | CI) | N (%) | CI) | |
| Race/ethnicity | |||||
| Non-Hispanic White | 343 (56.8) | 259 (75.5) | Ref | 317 (92.4) | Ref |
| African-American | 180 (29.8) | 55 (30.6) | 0.14 (0.08, 0.23) | 149 (82.8) | 0.65 (0.31, 1.36) |
| Hispanic/Latina | 58 (9.6) | 39 (67.2) | 0.75 (0.39, 1.44) | 51 (87.9) | 0.66 (0.25, 1.74) |
| Other | 23 (3.8) | 16 (69.6) | 1.13 (0.42, 3.06) | 18 (78.3) | 0.33 (0.11, 1.05) |
| Age at diagnosis | |||||
| 40–49 | 197 (32.6) | 115 (58.4) | Ref | 176 (89.3) | Ref |
| 50–59 | 295 (48.8) | 195 (66.1) | 1.36 (0.88, 2.11) | 259 (87.8) | 0.88 (0.47, 1.65) |
| 60–64 | 112 (18.5) | 59 (52.7) | 0.99 (0.53, 1.85) | 100 (89.3) | 0.88 (0.35, 2.21) |
| Education | |||||
| High school or less | 149 (24.7) | 62 (41.6) | Ref | 125 (83.9) | Ref |
| Some college/technical school | 212 (35.1) | 136 (64.2) | 2.28 (1.39, 3.76) | 189 (89.2) | 0.98 (0.49, 1.98) |
| College graduate | 117 (19.4) | 76 (65) | 1.58 (0.89, 2.83) | 106 (90.6) | 1.34 (0.56, 3.22) |
| Graduate school | 126 (20.9) | 95 (75.4) | 2.44 (1.34, 4.44) | 115 (91.3) | 1.15 (0.47, 2.77) |
| Current employment status | |||||
| Employed | 399 (66.1) | 260 (65.2) | Ref | 352 (88.2) | Ref |
| Not employed/retired | 176 (29.1) | 102 (58) | 0.77 (0.48, 1.24) | 159 (90.3) | 1.42 (0.70, 2.89) |
| Other or missing | 29 (4.8) | 7 (24.1) | 0.79 (0.27, 2.26) | 24 (82.8) | 1.57 (0.41, 5.93) |
| Current marital status | |||||
| Married/living as married | 360 (59.6) | 233 (64.7) | Ref | 329 (91.4) | Ref |
| Never married | 44 (7.3) | 20 (45.5) | 0.59 (0.28, 1.21) | 39 (88.6) | 1.00 (0.35, 2.87) |
| Widowed/divorced/separated | 200 (33.1) | 116 (58) | 1.53 (0.96, 2.42) | 167 (83.5) | 0.62 (0.34, 1.14) |
| Treatment | |||||
| Surgery only | 184 (30.5) | 105 (57.1) | Ref | 159 (86.4) | Ref |
| Surgery and chemotherapy | 61 (10.1) | 40 (65.6) | 1.73 (0.78, 3.8) | 56 (91.8) | 2.03 (0.6, 6.84) |
| Surgery and radiation | 215 (35.6) | 130 (60.5) | 0.77 (0.48, 1.23) | 190 (88.4) | 0.91 (0.47, 1.76) |
| Surgery, chemotherapy, and radiation | 144 (23.8) | 94 (65.3) | 1.22 (0.64, 2.33) | 130 (90.3) | 1.13 (0.43, 2.93) |
| Staging | |||||
| In situ | 146 (24.2) | 84 (57.5) | Ref | 124 (84.9) | Ref |
| Localized | 324 (53.6) | 209 (64.5) | 1.33 (0.82, 2.17) | 294 (90.7) | 1.70 (0.87, 3.34) |
| Regional | 134 (22.2) | 76 (56.7) | 0.97 (0.47, 1.99) | 117 (87.3) | 1.15 (0.42, 3.13) |
| Limiting comorbidities | |||||
| 0 limiting comorbidities | 459 (76) | 290 (63.2) | Ref | 407 (88.7) | Ref |
| 1 limiting comorbidity | 99 (16.4) | 58 (58.6) | 0.96 (0.57, 1.62) | 89 (89.9) | 1.22 (0.56, 2.64) |
| 2+ limiting comorbidities | 46 (7.6) | 21 (45.7) | 0.7 (0.32, 1.56) | 39 (84.8) | 1.26 (0.42, 3.78) |
| Confiding in family members | 581 (96.2) | 362 (62.3) | 1.69 (0.57, 5.04) | 522 (89.9) | 2.86 (1.00, 8.12) |
| Confiding in friends and neighbors | 570 (94.4) | 356 (62.5) | 1.07 (0.44, 2.62) | 514 (90.2) | 3.37 (1.34, 8.52) |
| Confiding in healthcare providers | 535 (88.6) | 340 (63.6) | 1.89 (1.04, 3.46) | - | - |
| Support program participation | 369 (61.1) | - | - | 340 (92.1) | 1.85 (1.02, 3.36) |
| Religiosity (Mean(SD)) | 15.3 (4.6) | - | 0.98 (0.94, 1.02) | - | 0.97 (0.91, 1.03) |
Bolded numbers represent estimates statistically significant at p<0.05.
Table 3.
Multivariable model examining factors associated with posttraumatic growth, stratified by race/ethnicity.
| Non-Hispanic White (adjusted r² = 0.14) N = 343 | Black/African American (adjusted r² = 0.20) N = 180 | Hispanic/Latina (adjusted r² = 0.03) N = 58 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | β | p | B (SE) | β | p | B (SE) | β | p | |
| Age at interview | −0.4 (0.2) | −0.10 | 0.10 | −1.0 (0.4) | −0.23 | 0.008 | 0.3 (0.7) | 0.08 | 0.68 |
| Unemployed/retired vs. employed | −1.8 (3.3) | −0.03 | 0.58 | −13.3 (5.7) | −0.19 | 0.02 | 4.6 (9.2) | 0.08 | 0.62 |
| Staging | |||||||||
| In situ | Ref | Ref | 0.03 | Ref | Ref | 0.86 | Ref | Ref | 0.45 |
| Localized | 8.8 (3.4) | 0.17 | 0.01 | 2.1 (6) | 0.03 | 0.73 | 1.3 (11.1) | 0.02 | 0.91 |
| Regional | 11.6 (5.3) | 0.18 | 0.03 | 4.4 (7.6) | 0.07 | 0.56 | −18.3 (20.2) | −0.26 | 0.37 |
| Religiosity | −0.7 (0.3) | −0.15 | 0.004 | −1.3 (0.8) | −0.12 | 0.10 | 1.5 (1.1) | 0.20 | 0.19 |
| Confided in healthcare providers | 11.7 (5.1) | 0.12 | 0.02 | 4.5 (6.0) | 0.06 | 0.45 | 2.8 (14.9) | 0.03 | 0.85 |
| Participated in a support program | 10.4 (3.2) | 0.18 | 0.001 | 13.0 (4.9) | 0.20 | 0.009 | −4.1 (9.9) | −0.07 | 0.68 |
Parameter estimates adjusted for all other variables present in the model as well as time since diagnosis, treatment summary, number of limiting comorbidities, education, marital status, and confiding in family, friends, and neighbors.
Bolded numbers represent estimates statistically significant at p<0.05.
Acknowledgments
Funding: Supported by contracts from the National Cancer Institute: N01-CN-75036-20, N01- CN-05228, N01-PC-67010.
The authors would like to thank Drs. Carly Parry and Julia Rowland for their review and insightful comments on earlier versions of the manuscript.
Footnotes
Disclosures: There are no financial disclosures or conflicts of interest to report.
References
- Ai AL, Hall D, Pargament K, Tice TN. Posttraumatic growth in patients who survived cardiac surgery: the predictive and mediating roles of faith-based factors. J Behav Med. 2012 doi: 10.1007/s10865-012-9412-6. [DOI] [PubMed] [Google Scholar]
- Avis M, Elkan R, Patel S, Walker BA, Ankti N, Bell C. Ethnicity and participation in cancer self-help groups. Psychooncology. 2008;17(9):940–947. doi: 10.1002/pon.1284. [DOI] [PubMed] [Google Scholar]
- Beasley JM, Newcomb PA, Trentham-Dietz A, Hampton JM, Ceballos RM, Titus-Ernstoff L, Holmes MD. Social networks and survival after breast cancer diagnosis. J Cancer Surviv. 2010 doi: 10.1007/s11764-010-0139-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006;25(1):47–56. doi: 10.1037/0278-6133.25.1.47. 2006-01035-007 [pii] [DOI] [PubMed] [Google Scholar]
- Bellizzi KM, Blank TO, Oakes CE. Social comparison processes in autobiographies of adult cancer survivors. J Health Psychol. 2006;11(5):777–786. doi: 10.1177/1359105306066637. 11/5/777 [pii] [DOI] [PubMed] [Google Scholar]
- Bellizzi KM, Smith AW, Reeve BB, Alfano CM, Bernstein L, Meeske K, Ballard-Barbash RR. Posttraumatic growth and health-related quality of life in a racially diverse cohort of breast cancer survivors. J Health Psychol. 2010;15(4):615–626. doi: 10.1177/1359105309356364. 15/4/615 [pii] [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for behavioral sciences. New York: Academic Press; 1977. (revised ed.) [Google Scholar]
- Coward DD. Lessons learned in developing a support intervention for African American women with breast cancer. Oncol Nurs Forum. 2005;32(2):261–266. doi: 10.1188/05.ONF.261-266. [pii] [DOI] [PubMed] [Google Scholar]
- Galvan N, Buki LP, Garces DM. Suddenly, a carriage appears: social support needs of Latina breast cancer survivors. Journal of psychosocial oncology. 2009;27(3):361–382. doi: 10.1080/07347330902979283. [DOI] [PubMed] [Google Scholar]
- Grande GE, Myers LB, Sutton SR. How do patients who participate in cancer support groups differ from those who do not? Psychooncology. 2006;15(4):321–334. doi: 10.1002/pon.956. [DOI] [PubMed] [Google Scholar]
- Grassi L, Sabato S, Rossi E, Marmai L, Biancosino B. Effects of supportive-expressive group therapy in breast cancer patients with affective disorders: a pilot study. Psychother Psychosom. 2010;79(1):39–47. doi: 10.1159/000259416. [DOI] [PubMed] [Google Scholar]
- Greene B. African-American women: considering diverse identities and societal barriers in psychotherapy. Ann N Y Acad Sci. 1996;789:191–209. doi: 10.1111/j.1749-6632.1996.tb55646.x. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15(2):135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- Hewitt M, Breen N, Devesa S. Cancer prevalence and survivorship issues: analyses of the 1992 National Health Interview Survey. J Natl Cancer Inst. 1999;91(17):1480–1486. doi: 10.1093/jnci/91.17.1480. [DOI] [PubMed] [Google Scholar]
- Irwin ML, Crumley D, McTiernan A, Bernstein L, Baumgartner R, Gilliland FD, Ballard-Barbash R. Physical activity levels before and after a diagnosis of breast carcinoma: the Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer. 2003;97(7):1746–1757. doi: 10.1002/cncr.11227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsinger DP, Penedo FJ, Antoni MH, Dahn JR, Lechner S, Schneiderman N. Psychosocial and sociodemographic correlates of benefit-finding in men treated for localized prostate cancer. Psychooncology. 2006;15(11):954–961. doi: 10.1002/pon.1028. [DOI] [PubMed] [Google Scholar]
- Koenig H, Parkerson GR, Jr, Meador KG. Religion index for psychiatric research. A J Psychiatry. 1997;154(6):885–886. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–1111. doi: 10.1200/JCO.2005.04.2846. 24/7/1105 [pii] [DOI] [PubMed] [Google Scholar]
- Leadbeater M. Evaluating use of a support group in secondary breast cancer care. Nurs Times. 2004;100(50):34–36. [PubMed] [Google Scholar]
- Lelorain S, Bonnaud-Antignac A, Florin A. Long term posttraumatic growth after breast cancer: prevalence, predictors and relationships with psychological health. J Clin Psychol Med Settings. 2010;17(1):14–22. doi: 10.1007/s10880-009-9183-6. [DOI] [PubMed] [Google Scholar]
- Llewellyn CD, Horney DJ, McGurk M, Weinman J, Herold J, Altman K, Smith HE. Assessing the psychological predictors of benefit finding in patients with head and neck cancer. Psychooncology. 2011 doi: 10.1002/pon.2065. [DOI] [PubMed] [Google Scholar]
- Masi CM, Gehlert S. Perceptions of breast cancer treatment among African-American women and men: implications for interventions. J Gen Intern Med. 2009;24(3):408–414. doi: 10.1007/s11606-008-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Olopade OI. Racial and ethnic disparities in breast cancer: a multilevel perspective. Med Clin North Am. 2005;89(4):753–770. doi: 10.1016/j.mcna.2005.02.004. S0025-7125(05)00021-0 [pii] [DOI] [PubMed] [Google Scholar]
- Michalec B, Van Willigen M, Wilson K, Schreier A, Williams S. The race gap in support group participation by breast cancer survivors: real or artifact? Eval Rev. 2004;28(2):123–143. doi: 10.1177/0193841X03260313. [DOI] [PubMed] [Google Scholar]
- Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Well-being, posttraumatic growth and benefit finding in long-term breast cancer survivors. Psychol Health. 2009;24(5):583–595. doi: 10.1080/08870440701671362. 787316430 [pii] [DOI] [PubMed] [Google Scholar]
- Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res. 2008;27:32. doi: 10.1186/1756-9966-27-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris BA, Chambers SK, Campbell M, Dwyer M, Dunn J. Motorcycles and breast cancer: The influence of peer support and challenge on distress and posttraumatic growth. Support Care Cancer. 2011 doi: 10.1007/s00520-011-1287-5. [DOI] [PubMed] [Google Scholar]
- Napoles-Springer AM, Ortiz C, O’Brien H, Diaz-Mendez M, Perez-Stable EJ. Use of cancer support groups among Latina breast cancer survivors. Journal of cancer survivorship: research and practice. 2007;1(3):193–204. doi: 10.1007/s11764-007-0029-7. [DOI] [PubMed] [Google Scholar]
- Nenova M, Duhamel K, Zemon V, Rini C, Redd WH. Posttraumatic growth, social support, and social constraint in hematopoietic stem cell transplant survivors. Psychooncology. 2011 doi: 10.1002/pon.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen JE, Goldstein MS, Lee JH, Breen N, Rowland JH. Use of health- related and cancer-specific support groups among adult cancer survivors. Cancer. 2007;109(12):2580–2589. doi: 10.1002/cncr.22719. [DOI] [PubMed] [Google Scholar]
- Posluszny DM, Baum A, Edwards RP, Dew MA. Posttraumatic growth in women one year after diagnosis for gynecologic cancer or benign conditions. Journal of psychosocial oncology. 2011;29(5):561–572. doi: 10.1080/07347332.2011.599360. [DOI] [PubMed] [Google Scholar]
- Rand KL, Cripe LD, Monahan PO, Tong Y, Schmidt K, Rawl SM. Illness appraisal, religious coping, and psychological responses in men with advanced cancer. Support Care Cancer. 2011 doi: 10.1007/s00520-011-1265-y. [DOI] [PubMed] [Google Scholar]
- Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum. 2008;35(5):844–849. doi: 10.1188/08.ONF.844-849. [DOI] [PubMed] [Google Scholar]
- Schaefer FC, Blazer DG, Koenig HG. Religious and spiritual factors and the consequences of trauma: a review and model of the interrelationship. Int J Psychiatry Med. 2008;38(4):507–524. doi: 10.2190/PM.38.4.i. [DOI] [PubMed] [Google Scholar]
- Schou I, Ekeberg O, Karesen R, Sorensen E. Psychosocial intervention as a component of routine breast cancer care-who participates and does it help? Psychooncology. 2008;17(7):716–720. doi: 10.1002/pon.1264. [DOI] [PubMed] [Google Scholar]
- Schroevers MJ, Helgeson VS, Sanderman R, Ranchor AV. Type of social support matters for prediction of posttraumatic growth among cancer survivors. Psychooncology. 2010;19(1):46–53. doi: 10.1002/pon.1501. [DOI] [PubMed] [Google Scholar]
- Schwarzer R, Luszczynska A, Boehmer S, Taubert S, Knoll N. Changes in finding benefit after cancer surgery and the prediction of well-being one year later. Soc Sci Med. 2006;63(6):1614–1624. doi: 10.1016/j.socscimed.2006.04.004. S0277-9536(06)00202-4 [pii] [DOI] [PubMed] [Google Scholar]
- Scrignaro M, Barni S, Magrin ME. The combined contribution of social support and coping strategies in predicting post-traumatic growth: a longitudinal study on cancer patients. Psychooncology. 2011;20(8):823–831. doi: 10.1002/pon.1782. [DOI] [PubMed] [Google Scholar]
- Silva SM, Crespo C, Canavarro MC. Pathways for psychological adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychol Health. 2012 doi: 10.1080/08870446.2012.676644. [DOI] [PubMed] [Google Scholar]
- Silva SM, Moreira HC, Canavarro MC. Examining the links between perceived impact of breast cancer and psychosocial adjustment: the buffering role of posttraumatic growth. Psychooncology. 2011 doi: 10.1002/pon.1913. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62(3):355–360. doi: 10.1016/j.pec.2006.06.011. S0738-3991(06)00193-5 [pii] [DOI] [PubMed] [Google Scholar]
- Simoni JM, Franks JC, Lehavot K, Yard SS. Peer interventions to promote health: conceptual considerations. Am J Orthopsychiatry. 2011;81(3):351–359. doi: 10.1111/j.1939-0025.2011.01103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BW, Dalen J, Bernard JF, Baumgartner KB. Posttraumatic growth in non-Hispanic White and Hispanic women with cervical cancer. Journal of psychosocial oncology. 2008;26(4):91–109. doi: 10.1080/07347330802359768. [DOI] [PubMed] [Google Scholar]
- Steginga SK, Pinnock C, Gardner M, Gardiner RA, Dunn J. Evaluating peer support for prostate cancer: the Prostate Cancer Peer Support Inventory. BJU Int. 2005;95(1):46–50. doi: 10.1111/j.1464-410X.2005.05247.x. BJU5247 [pii] [DOI] [PubMed] [Google Scholar]
- Stevens MJ, Duttlinger JE. Correlates of participation in a breast cancer support group. J Psychosom Res. 1998;45(3):263–275. doi: 10.1016/s0022-3999(97)00296-1. [pii] [DOI] [PubMed] [Google Scholar]
- Storch EA, Roberti JW, Heidgerken AD, Storch JB, Lewin AB, Killiany EM, Geffken GR. The Duke Religion Index: a psychometric investigation. Pastoral Psychology. 2004;53(2):175–181. [Google Scholar]
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Till JE. Evaluation of support groups for women with breast cancer: importance of the navigator role. Health Qual Life Outcomes. 2003;1:16. doi: 10.1186/1477-7525-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychol. 2004;23(1):16–23. doi: 10.1037/0278-6133.23.1.16. [pii] [DOI] [PubMed] [Google Scholar]
- Vogel BA, Leonhart R, Helmes AW. Communication matters: the impact of communication and participation in decision making on breast cancer patients’ depression and quality of life. Patient Educ Couns. 2009;77(3):391–397. doi: 10.1016/j.pec.2009.09.005. S0738-3991(09)00421-2 [pii] [DOI] [PubMed] [Google Scholar]
- Zabalegui A, Sanchez S, Sanchez PD, Juando C. Nursing and cancer support groups. J Adv Nurs. 2005;51(4):369–381. doi: 10.1111/j.1365-2648.2005.03508.x. JAN3508 [pii] [DOI] [PubMed] [Google Scholar]