Abstract
Objectives
To evaluate the real-life effect of an evidence-based Gold Standard Programme (GSP) for smoking cessation interventions in disadvantaged patients and to identify modifiable factors that consistently produce the highest abstinence rates.
Design
Observational prospective cohort study.
Setting
GSPs in pharmacies, hospitals and communities in Denmark, reporting to the national Smoking Cessation Database.
Participants
Disadvantaged patients, defined as patients with a lower level of education and those receiving unemployment benefits.
Interventions
6-week manualised GSP smoking cessation interventions performed by certified staff.
Main outcome measures
6 months of continuous abstinence, response rate: 80%.
Results
Continuous abstinence of the 16 377 responders was 34% (of all 20 588 smokers: 27%). Continuous abstinence was lower in 5738 smokers with a lower educational level (30% of responders and 23% of all) and in 840 unemployed (27% of responders and 19% of all). In respect to modifiable factors, continuous abstinence was found more often after programmes in one-on-one formats (vs group formats) among patients with a lower educational level, 34% (vs 25%, p=0.037), or among unemployed, 35% (vs 24%, p=0.099). The variable ‘format’ stayed in the final model of multivariable analyses in patients with a lower educational level, OR=1.31 (95% CI 1.05 to 1.63).
Conclusions
Although continuous abstinence was lower among disadvantaged smokers, the absolute difference was small. If the programme had been as effective in disadvantaged as in non-disadvantaged groups, there would have been an extra 46 or 8 quitters annually, respectively. Promoting individual interventions among those with a low education may increase the effectiveness of GSP.
Keywords: Smoking, smoking cessation intervention, health disparities, health inequalities, nationwide database
Introduction
Smoking rates are higher among individuals from lower socioeconomic groups. Access to preventive health services, such as smoking cessation programmes, is limited, and the success rate is reported to be even smaller.1–4 The efficacy of smoking cessation interventions in research settings has been described in randomised clinical trials.4–10 There have been few studies of the effectiveness of interventions implemented in real-life settings, thus results from efficacy trials might not reflect real-life conditions.11 12
The Danish Smoking Cessation Database (SCDB-DK) offers a unique opportunity to analyse the effectiveness of real-life smoking cessation interventions.13 14 This high-quality clinical database combines comprehensive information on 67 000 smoking interventions taking place at the smoking cessation intervention units. Smokers have been included from 2001 and are followed up to 6 months after the intervention. The SCDB-DK reflects a diversity of settings, formats and organisations. The main programme is the Gold Standard Programme (GSP).15–17 In order to further address smoking-related inequality in healthcare, we must know which programmes are most effective for the disadvantaged. The data set also allowed exploration of factors that might be modified in order to increase continuous abstinence among disadvantaged groups, such as the programme setting payment and modality, as well as more traditional factors such as age or gender which might affect outcome but are not modifiable. We were not aware of any current literature addressing these issues. In general, there is some evidence that group programmes are more effective7 18 and that incentives have a short effect but no consistent long-term effect.19 With regard to geography, Denmark is a very small country with a good infrastructure, and the capital is not far from the regions. The Danes travel back and forth between regions every day; therefore, another region for smoking cessation intervention could easily be chosen. Therefore, the geographical region was considered a potentially modifiable factor, although this might not always be the case.
Thus, the aim of this study was to identify the programme, setting, payment modality and geographic region with the highest rates of continuous abstinence in disadvantaged patients.
Methods
Design
This was an observational prospective cohort study using data from a national registry (Smoking Cessation Database).
Setting
During the study period, smoking cessation programmes were offered in all five Danish regions by more than 350 units in hospitals and primary care facilities, including pharmacies, municipality facilities and others.
Participants
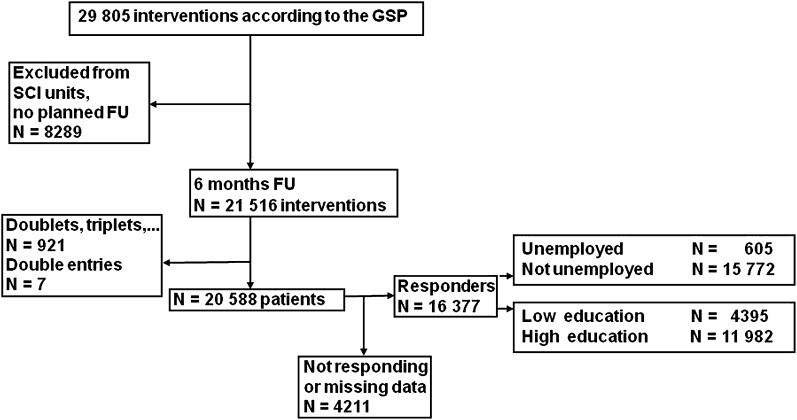
From the beginning of 2001 to the summer of 2011, approximately 67 000 smoking cessation interventions were registered in the Smoking Cessation Databank. Informed consent was obtained. From 2006, registration was performed using a unique 10 digit personal identification number (PIN), and 34 551 interventions were registered with a PIN at the end of January 2011. The PIN can be used to control for doublets. Individuals, who registered in the Smoking Cessation Database, were at least 18 years old, and participated in the GSP in Denmark were included. Patients younger than 18 years (411 patients); patients from Greenland (37 patients); patients without information on gender, age and smoking cessation unit (53 patients); patients with <7-month follow-up (1723 patients) and patients attending interventions other than the GSP (2522 patients) were excluded. Thereby, 29 805 smoking cessation interventions according to GSP were considered. Some smoking cessation units did not systematically follow their patients up to 6 months. Patients in those units were not included in the analysis of the primary outcome (trial profile: figure 1). Of the 21 516 databank entries finally included, seven were double entries and 921 were entries referring to courses of patients attending a programme more than one time (two to seven times). Therefore, 20 588 patients were finally included.
Figure 1.
Patient flow. FU, follow-up; GSP, Gold Standard Smoking Cessation Programme; SCI, smoking cessation intervention.
Intervention
The GSP has been the standard intervention in Denmark since 2001. It was developed with the guidance of the National Cancer Institute, which trained the Stop Smoking Centre.20 The programme consisted of manual-based teaching sessions together with nicotine replacement therapy.13 14 20 It consisted of five meetings over 6 weeks, with a clearly structured patient education programme, including a motivational conversation at the beginning, reflections on benefits and costs of continuous smoking versus cessation, date of cessation, teaching and training about risk situations and relapse prevention, withdrawal symptoms and medical support, and planning for the future. Nicotine replacement therapy was provided and adjusted to smoking severity, according to the Fagerström test21 score, the number of cigarettes (or gram of tobacco when smoking pipes or cigars) and patient preferences. The patients were free to choose different kinds of nicotine products and change their minds during the programme. A hotline was available during daytime hours on working days. GSP was delivered either in a group or in an individual format. The group size varied, with the median being 12 registered participants (range 2–26 participants). The allocation of a single patient to the group or individual programme was at the discretion of the smoking cessation units or the instructors, respectively. The programme was usually offered free of charge. Of the 20 588 patients, 19 185 (93%) received the course for free. Some patients received free medication, while others had to pay themselves.
According to the standard operating procedures defined by the Steering Committee, compliance was defined as attendance of 75% or more of the scheduled meetings.
Measures (including outcome and independent variables)
Outcomes
The primary outcome was continuous abstinence, defined as not smoking at all from the end of the programme to the 6-month follow-up, as reported in a telephone interview after 6 months ±1 month. Four attempts were made to reach the patient, and at least one attempt had to be in the evening.
Other variables
For every patient, the smoking cessation programme, the specific modifications (individual vs group format), the region (Capital of Copenhagen, Midtjylland, Nordjylland, Sjælland, Syddanmark), the payment modality (no free medication, free medication for a few days, free medication for <5 weeks or 5-week medication free of charge) and the setting (hospitals, pharmacies and county or municipality) were documented categorically. If there were missing data, for the purpose of the multivariable analyses, dummy variables were formed and the missing variables were summarised as shown in the first column of table 1.
Table 1.
Continuous abstinence rates; OR and 95% CI for the univariate, adjusted analysis and for the final multivariable model
| Variables | Lower educational level | Unemployment | ||||
| OR univariate (95% CI) | Adjusted OR (95% CI) | Final adjusted OR (95% CI) | OR univariate (95% CI) | Adjusted OR (95% CI) | Final adjusted OR (95% CI) | |
| Capital vs other regions | 0.88 (0.78 to 1.00) | 0.95 (0.83 to 1.11) | 1.11 (0.77 to 1.59) | 1.39 (0.90 to 2.15) | ||
| Setting | ||||||
| Pharmacy vs other | 1.08 (0.93 to 1.24) | 0.99 (0.84 to 1.17) | 0.89 (0.58 to 1.37) | 0.85 (0.52 to 1.41) | ||
| Hospital vs other | 0.97 (0.79 to 1.19) | 1.01 (0.79 to 1.30) | 0.64 (0.39 to 1.07) | 0.57 (0.30 to 1.09) | ||
| Individual format vs other | 1.25 (1.01 to 1.54) | 1.30 (1.03 to 1.63) | 1.31 (1.05 to 1.63) | 1.56 (0.92 to 2.66) | 2.02 (1.07 to 3.79) | |
| Free medication for <5 weeks | 1.14 (0.93 to 1.40) | 1.17 (0.92 to 1.48) | 0.64 (0.34 to 1.17) | 0.78 (0.38 to 1.62) | ||
| Men vs women | 1.18 (1.03 to 1.34) | 1.26 (1.09 to 1.45) | 1.25 (1.09 to 1.43) | 1.23 (0.85 to 1.79) | 1.39 (0.92 to 2.10) | |
| Age, each 10 years | 1.07 (1.02 to 1.12) | 1.03 (0.97 to 1.09) | 1.02 (0.89 to 1.18) | 0.99 (0.80 to 1.22) | ||
| Pack-year, each 10 years | 0.96 (0.93 to 0.99) | 1.00 (0.95 to 1.05) | 0.93 (0.85 to 1.01) | 0.95 (0.82 to 1.11) | ||
| Fagerström, each point | 0.88 (0.86 to 0.91) | 0.89 (0.86 to 0.92) | 0.88 (0.86 to 0.92) | 0.89 (0.81 to 0.96) | 0.92 (0.82 to 1.03) | 0.89 (0.82 to 0.98) |
| Earlier attempts | ||||||
| 1–3/missing vs no attempts | 1.06 (0.93 to 1.21) | 0.98 (0.85 to 1.13) | 1.19 (0.81 to 1.73) | 1.06 (0.71 to 1.609) | ||
| >3 attempts vs no attempt | 0.99 (0.78 to 1.27) | 0.83 (0.64 to 1.09) | 1.73 (0.90 to 3.31) | 1.43 (0.70 to 2.93) | ||
| Living with smoker | 0.94 (0.82 to 1.08) | 1.01 (0.88 to 1.16) | 1.10 (0.76 to 1.61) | 1.49 (0.98 to 2.26) | ||
| Compliant with the programme | 3.32 (2.86 to 3.86) | 3.26 (2.80 to 3.80) | 3.30 (2.84 to 3.84) | 4.60 (3.05 to 6.95) | 4.59 (2.99 to 7.05) | 4.58 (3.01 to 6.96) |
| Professional recommendation | 0.78 (0.69 to 0.89) | 0.79 (0.69 to 0.91) | 0.80 (0.70 to 0.92) | 0.70 (0.49 to 1.02) | 0.91 (0.60 to 1.37) | |
The continuous variables such as age, smoking (cigarettes per day, pack-years (years of smoking × cigarettes per day divided by 20)) and Fagerström Test for Nicotine dependence21 were categorised as shown in tables 2 and 3.
Table 2.
Characteristics of all patients with low and high education and their continuous abstinence (given as % of all and of the responders, respectively)
| Low education | High education | |||||
| Characteristics | Continuous abstinence (%) | Characteristics | Continuous abstinence (%) | |||
| n (%) | All | Responders | n (%) | All | Responders | |
| All | 5738 (100) | 23 | 30 | 14 850 (100) | 28 | 35 |
| Setting | ||||||
| Hospital/midwifery | 686 (12) | 22 | 29 | 1613 (11) | 30 | 36 |
| Pharmacies | 1677 (29) | 24 | 31 | 3537 (24) | 30 | 37 |
| Municipality/county | 3320 (58) | 22 | 29 | 9571 (64) | 27 | 34 |
| Other | 55 (1) | 129 (1) | ||||
| Format | ||||||
| Individual | 601 (10) | 25 | 34 | 1240 (8) | 32 | 40 |
| Group | 5106 (89) | 22 | 29 | 13 536 (91) | 28 | 34 |
| Other | 31 (1) | 74 (0) | ||||
| Medication for free | ||||||
| No free medication | 3135 (55) | 23 | 30 | 7778 (52) | 30 | 36 |
| Free medication for a few days | 1979 (34) | 21 | 28 | 5806 (39) | 26 | 34 |
| Free medication for <5 weeks | 523 (9) | 23 | 31 | 1065 (7) | 27 | 33 |
| Free medication for 5 weeks | 101 (2) | 30 | 41 | 201 (1) | 33 | 39 |
| Region | ||||||
| Living in the capital | 2072 (36) | 21 | 28 | 6347 (43) | 26 | 33 |
| Living in other regions | 3666 (64) | 24 | 31 | 8503 (57) | 30 | 36 |
| Midtjylland | 1207 (21) | 25 | 31 | 2860 (19) | 30 | 36 |
| Nordjylland | 275 (5) | 23 | 30 | 539 (4) | 31 | 37 |
| Sjælland | 891 (16) | 24 | 31 | 2152 (14) | 29 | 35 |
| Syddanmark | 1293 (23) | 24 | 30 | 2952 (20) | 30 | 36 |
| Gender | ||||||
| Male | 2221 (39) | 24 | 32 | 5715 (38) | 31 | 38 |
| Female | 3517 (61) | 22 | 28 | 9135 (62) | 27 | 33 |
| Age (years) | ||||||
| 18–39 | 1756 (31) | 18 | 27 | 3588 (24) | 26 | 34 |
| 40–49 | 1237 (22) | 24 | 31 | 3845 (26) | 28 | 34 |
| 50–59 | 1359 (24) | 24 | 30 | 4007 (27) | 28 | 35 |
| 59–98 | 1386 (24) | 26 | 32 | 3410 (23) | 31 | 37 |
| Smoking | ||||||
| 0–20 pack-years | 2301 (40) | 23 | 31 | 5515 (37) | 30 | 39 |
| >20 pack-years | 3437 (60) | 23 | 29 | 9335 (63) | 27 | 33 |
| Fagerström 1–4 points | 1968 (34) | 28 | 36 | 5838 (39) | 33 | 40 |
| Fagerström 5–10 points | 3770 (66) | 20 | 26 | 9012 (61) | 25 | 32 |
| 0 to <10 cigarettes per day | 487 (8) | 26 | 35 | 1328 (9) | 36 | 45 |
| 10 to <20 | 1896 (33) | 26 | 34 | 5317 (36) | 30 | 37 |
| 20 to <30 | 2415 (42) | 22 | 28 | 6118 (41) | 26 | 32 |
| 30 to <40 | 647 (11) | 17 | 23 | 1460 (10) | 24 | 30 |
| 40+ | 293 (5) | 18 | 24 | 627 (4) | 23 | 29 |
| Compliance with programme | ||||||
| Compliant | 3200 (56) | 32 | 39 | 8970 (60) | 37 | 44 |
| Not compliant | 2418 (42) | 11 | 15 | 5588 (38) | 14 | 18 |
| Missing information | 120 (2) | 25 | 33 | 292 (2) | 29 | 39 |
| Living with a smoker | ||||||
| Yes | 2129 (37) | 22 | 29 | 4910 (33) | 28 | 34 |
| No | 3568 (62) | 23 | 30 | 9825 (66) | 29 | 36 |
| Missing information | 41 (1) | 29 | 44 | 115 (1) | 30 | 36 |
| Attempts to quit | ||||||
| Never attempting to quit | 2516 (44) | 22 | 29 | 5535 (37) | 28 | 34 |
| 1–3 | 2724 (47) | 23 | 30 | 7506 (51) | 28 | 34 |
| >3 | 438 (8) | 23 | 29 | 1488 (10) | 33 | 41 |
| Missing information | 60 (1) | 22 | 30 | 321 (2) | 23 | 32 |
| Professional recommendation | ||||||
| Yes | 3345 (58) | 21 | 28 | 8113 (55) | 27 | 33 |
| No | 2393 (42) | 25 | 33 | 6737 (45) | 30 | 37 |
| Education | ||||||
| Low level | 5738 (100) | 23 | 30 | |||
| High level | 14 082 (95) | 29 | 35 | |||
| Missing information | 768 (5) | 21 | 28 | |||
| Unemployment | ||||||
| Unemployed | 371 (6) | 16 | 24 | 469 (3) | 22 | 29 |
| Not unemployed | 5282 (92) | 23 | 30 | 13 951 (94) | 29 | 35 |
| Missing information | 85 (1) | 21 | 31 | 430 (3) | 23 | 31 |
Table 3.
Characteristics of the unemployed and not unemployed patients and their continuous abstinence (given as % of all and of the responders, respectively)
| Unemployed | Not unemployed | |||||
| Characteristics | Continuous abstinence (%) | Characteristics | Continuous abstinence (%) | |||
| n (%) | All | Responders | n (%) | All | Responders | |
| All | 840 (100) | 19 | 27 | 19 748 (100) | 27 | 34 |
| Setting | ||||||
| Hospital/midwifery | 145 (17) | 17 | 21 | 2154 (11) | 28 | 35 |
| Pharmacies | 219 (26) | 19 | 27 | 4995 (25) | 29 | 36 |
| Municipality/county | 473 (56) | 21 | 29 | 12 418 (63) | 26 | 33 |
| Other | 3 (0) | 181 (1) | ||||
| Format | ||||||
| Individual | 99 (12) | 24 | 35 | 1742 (9) | 30 | 38 |
| Group | 734 (87) | 19 | 26 | 17 908 (91) | 27 | 33 |
| Other | 7 (1) | 98 (0) | ||||
| Medication for free | ||||||
| No free medication | 444 (53) | 20 | 29 | 10 469 (53) | 28 | 35 |
| Free medication for a few days | 295 (35) | 20 | 27 | 7490 (38) | 25 | 33 |
| Free medication for <5 weeks | 92 (11) | 12 | 17 | 1496 (8) | 27 | 33 |
| Free medication for 5 weeks | 9 (1) | 33 | 38 | 293 (1) | 32 | 40 |
| Region | ||||||
| Living in the capital | 337 (40) | 21 | 28 | 8082 (41) | 25 | 32 |
| Living in other regions | 503 (60) | 18 | 26 | 11 666 (59) | 28 | 35 |
| Midtjylland | 208 (25) | 20 | 27 | 3859 (20) | 29 | 35 |
| Nordjylland | 41 (5) | 22 | 29 | 773 (4) | 29 | 35 |
| Sjælland | 113 (13) | 18 | 26 | 2930 (15) | 28 | 34 |
| Syddanmark | 141 (17) | 16 | 24 | 4104 (21) | 28 | 35 |
| Gender | ||||||
| Male | 304 (36) | 21 | 30 | 7632 (39) | 29 | 36 |
| Female | 536 (64) | 19 | 26 | 12 116 (61) | 26 | 32 |
| Age (years) | ||||||
| 18–39 | 361 (43) | 18 | 27 | 4983 (25) | 24 | 32 |
| 40–49 | 209 (25) | 20 | 28 | 4873 (25) | 27 | 34 |
| 50–59 | 233 (28) | 21 | 26 | 5133 (26) | 28 | 34 |
| 59–98 | 37 (4) | 19 | 23 | 4759 (24) | 29 | 36 |
| Smoking | ||||||
| 0–20 pack-years | 381 (45) | 19 | 30 | 7435 (38) | 28 | 37 |
| >20 pack-years | 459 (55) | 19 | 25 | 12 313 (62) | 26 | 32 |
| Fagerström 1–4 points | 227 (27) | 23 | 33 | 7579 (38) | 32 | 39 |
| Fagerström 5–10 points | 613 (73) | 178 | 25 | 12 169 (62) | 24 | 30 |
| 0 to <10 cigarettes per day | 60 (7) | 18 | 27 | 1755 (9) | 34 | 43 |
| 10 to <20 | 252 (30) | 27 | 39 | 6961 (35) | 29 | 36 |
| 20 to <30 | 360 (43) | 17 | 24 | 8173 (41) | 25 | 32 |
| 30 to <40 | 111 (13) | 14 | 18 | 1996 (10) | 22 | 29 |
| 40+ | 57 (7) | 14 | 16 | 863 (4) | 22 | 28 |
| Compliance with programme | ||||||
| Compliant | 396 (47) | 32 | 40 | 11 774 (60) | 36 | 43 |
| Not compliant | 426 (51) | 8 | 13 | 7580 (38) | 13 | 18 |
| Missing information | 18 (2) | 6 | 10 | 394 (2) | 29 | 38 |
| Living with a smoker | ||||||
| Yes | 292 (35) | 20 | 28 | 6747 (34) | 26 | 32 |
| No | 545 (65) | 19 | 26 | 12 848 (65) | 27 | 35 |
| Missing information | 3 (0) | 158 (1) | ||||
| Attempts to quit | ||||||
| Never attempted to quit | 418 (50) | 18 | 25 | 7633 (39) | 26 | 33 |
| 1–3 | 350 (42) | 20 | 28 | 9880 (50) | 27 | 33 |
| >3 attempts | 68 (8) | 25 | 36 | 1858 (9) | 31 | 38 |
| Missing information | 4 (0) | 377 (2) | 23 | 32 | ||
| Professional recommendation | ||||||
| Yes | 531 (63) | 18 | 24 | 10 927 (55) | 26 | 32 |
| No | 309 (37) | 21 | 32 | 8821 (45) | 29 | 36 |
| Education | ||||||
| Low level | 371 (44) | 16 | 24 | 5367 (27) | 23 | 30 |
| High level | 446 (53) | 23 | 30 | 13 636 (69) | 29 | 36 |
| Missing information | 23 (3) | 9 | 13 | 745 (4) | 22 | 28 |
| Unemployment | ||||||
| Unemployed | 840 (100) | 19 | 27 | |||
| Not unemployed | 19 233 (97) | 27 | 34 | |||
| Missing information | 515 (3) | 23 | 31 | |||
Accordingly, quit attempts (never, one to three attempts or at least three attempts or missing information), living with a smoker (vs not living with a smoker or missing information), compliance (attendance of 75% or more of the scheduled meetings), non-compliant with programme (<75%) or missing information on compliance were documented for every patient. All patients were asked whether they received a recommendation from a health professional (eg, doctor, nurse, midwife). There was no difference made between those with no professional recommendation and those not responding to the question concerning professional recommendation.
Lower educational level was defined as no education except school (up to 12 years) or only short work-related courses in contrast to all other levels of education. Unemployment was defined as being available for the labour market and receiving unemployment benefits from the state, the municipalities, insurance or the unions. People at home, retired patients or patients in school were not included in this group; the proportion of patients without information on unemployment and education (4% and 3%, respectively (tables 2 and 3) was considered small and acceptable for a real-life study.
Statistical analysis
Existing data were analysed and reported, including missing data, loss of follow-up and sensitivity analyses according to the STROBE22 recommendations. First, a general description of the sample was given together with a description of the non-responders and the responders. Then, continuous abstinence was reported based on the patients' responses. Most randomised studies addressing the effect of smoking cessation intervention usually report according to the Russell Standards,23 which assume that it is likely that non-responders have relapsed. Therefore, continuous abstinence was also reported in our study, assuming that non-responders had relapsed.
The estimate of the expected annual number of extra quitters was calculated by multiplying the absolute differences in continuous abstinence rate with the number of the responding patients in this subgroup and by dividing it with the number of years of observation (5 years).
The continuous variables mentioned above were used in the multivariable analyses. Age, pack-years and cigarettes per day were included in steps of 10 (years or cigarettes).
The χ2 test or exact methods were used in the analysis of categorical data. A two-sided p value of <0.05 was regarded as significant. The non-parametric Mann–Whitney U test for the comparison of continuous or almost continuous variables was used. Multivariable logistic regression analyses and analyses of variance were used to test for differences in continuous abstinence. Statistical significances of possible predictors of continuous abstinence were compared by calculating the OR and the corresponding 95% CIs. Multiple logistic regression analyses were performed by entering all predictors together, followed by a stepwise backward procedure p(in) <0.10.
Dummy variables were formed for the variables as outlined in table 1 for the purpose of multivariable analysis (eg, capital vs regions, individual programme format, payment modality, living with a smoker, compliance, etc). The items ‘other’ or ‘missing’ were added to the bigger group. These numbers were considered as small and acceptable for a real-life study.
All statistical calculations were done with PASW V.18 (IBM Corporation).
Results
The analysis at 6 months for continuous abstinence included both the 16 377 responders (80%) and the 20% of non-responders (4211 patients). As shown in table 4, responding patients differ mainly with respect to age and compliance from non-responding patients. Non-responders were 3 years younger (median 47.3 vs 50.4 years, p<0.001). Patients compliant with the programme were more likely to respond: proportion of non-responders were lower among compliant patients compared to non-compliant patients (16% vs 27%, p<0.001). Rates of non-responding were 23% for those with a lower educational level and 28% for the unemployed. The proportion of non-responders was between 18% and 23% for all other socio-demographic-, smoking- and intervention-related variables.
Table 4.
Patient characteristics with respect to response
| All | Non-responding (%) | Responding (%) | |
| N | 20 588 | 4211 (100%) | 16 377 (100%) |
| Setting | |||
| Hospital/midwifery | 2299 | 10 | 11 |
| Pharmacies | 5214 | 25 | 25 |
| Municipality/county | 12 891 | 64 | 62 |
| Other and missing information | 184 | 0 | 1 |
| Format | |||
| Individual | 1841 | 9 | 9 |
| Group | 18 642 | 90 | 91 |
| Other and missing information | 105 | 0 | 1 |
| Medication for free | |||
| No free medication | 10 913 | 50 | 54 |
| Free medication for a few days | 7785 | 41 | 37 |
| Free medication for <5 weeks | 1588 | 8 | 8 |
| Free medication for 5 weeks | 302 | 1 | 1 |
| Region | |||
| Living in the capital | 8419 | 45 | 40 |
| Living in other regions | 12 169 | 55 | 60 |
| Midtjylland | 4067 | 17 | 20 |
| Nordjylland | 814 | 4 | 4 |
| Sjælland | 3043 | 15 | 15 |
| Syddanmark | 4245 | 19 | 21 |
| Gender | |||
| Male | 7936 | 39 | 39 |
| Female | 12 652 | 61 | 61 |
| Age (years) | |||
| 18–39 | 5344 | 32 | 24 |
| 40–49 | 5082 | 25 | 25 |
| 50–59 | 5366 | 24 | 27 |
| 59–98 | 4796 | 20 | 24 |
| Smoking | |||
| 0–20 pack-years | 7816 | 43 | 37 |
| >20 pack-years | 12 772 | 57 | 63 |
| Fagerström 1–4 points | 7806 | 36 | 38 |
| Fagerström 5–10 points | 12 782 | 64 | 62 |
| 0 to <10 cigarettes per day | 1815 | 9 | 9 |
| 10 to <20 | 7213 | 34 | 35 |
| 20 to <30 | 8533 | 41 | 42 |
| 30 to <40 | 2107 | 11 | 10 |
| 40+ | 920 | 5 | 4 |
| Compliance with programme | |||
| Compliant | 12 170 | 47 | 62 |
| Not compliant | 8006 | 51 | 36 |
| Missing information | 412 | 2 | 2 |
| Living with a smoker | |||
| Yes | 7039 | 33 | 35 |
| No | 13 393 | 66 | 65 |
| Missing information | 156 | 1 | 1 |
| Attempts to quit | |||
| Never attempted to quit | 8051 | 40 | 39 |
| 1–3 attempts | 10 230 | 49 | 50 |
| >3 attempts | 1926 | 9 | 10 |
| Missing information | 381 | 2 | 2 |
| Professional recommendation | |||
| Yes | 11 458 | 54 | 56 |
| No | 9130 | 46 | 44 |
| Education | |||
| Low level | 5738 | 32 | 27 |
| High level | 14 082 | 64 | 70 |
| Missing information | 768 | 4 | 4 |
| Unemployment | |||
| Unemployed | 840 | 6 | 4 |
| Not unemployed | 19 233 | 91 | 94 |
| Missing information | 515 | 3 | 2 |
Overall, 34% (5503 of 16 377 patients) reported 6 months of continuous abstinence. Continuous abstinence was 27%, when all non-responders were considered to be smokers. Of the 16 377 responding to follow-up, 27% had a lower level of education and 4% were unemployed (figure 1). The characteristics of all of the patients with respect to unemployment or level of education are shown in tables 2 and 3.
Continuous abstinence was significantly lower for the patients with a lower education level (30%) compared with those with a higher education level (35%, p<0.001) in those responding (of all registered: 23% vs 28%, table 2). Continuous abstinence was also significantly lower for the unemployed patients (27%) compared with those who were employed (34%, p<0.001), corresponding to 19% versus 27% of all registered (table 3).
The overall difference in continuous abstinence between disadvantaged and non-disadvantaged patients was 5% (with respect to education) and 7% (with respect to unemployment). The difference was up to 11% (with respect to high vs low education in patients with three or more quit attempts) or 15% with respect to unemployment (vs non-unemployed) in patients receiving free medication for <5 weeks and 12% in the patients 59 years and older as well as in those smoking <10 cigarettes per day (16%) or more than 40 cigarettes per day (12%). Comparing disadvantaged patients with non-disadvantaged patients, the most striking difference was observed in respect to employment in the hospital setting: continuous abstinence was 14% higher in non-unemployed patients compared with unemployed patients.
The characteristics and percentage of the disadvantaged patients with continuous abstinence are shown in tables 2 and 3. The results of the univariate and multivariable analyses for the 6-month continuous abstinence rate are shown in table 1. The final model revealed that the lower Fagerström Test for Nicotine Dependence Score21 (per point) and compliance with the programme were the only consistent predictors associated with continuous abstinence in both groups of disadvantaged patients.
For patients with the lower educational level, the variable ‘individual format’ of the GSP was a predictor of success in smoking cessation (OR=1.31, 95% CI 1.05 to 1.63), but for unemployed patients, it did not remain in the final model.
In the group of patients with a lower educational level, male gender or not having received a recommendation to quit by a health professional were also predictors for continuous abstinence.
Discussion
Among disadvantaged smokers participating in the Danish GSP for smoking cessation, we can report relatively high continuous abstinence rates of those responding (27%–30%) and 19%–23% of all registered for treatment. However, this is still 5%–7% lower than non-disadvantaged smokers. In absolute terms, there would be eight extra quitters per year if the programme was as effective for the unemployed group as it was for the employed smokers and 46 extra quitters per year for the patients with a lower level of education. Nine of 10 patients received group GSP, but continuous abstinence was somewhat higher among the one-tenth of patients who participated in a programme with an individual format, regardless of being disadvantaged. No other potentially modifiable component of greater effectiveness for disadvantaged patients was identified. It was impossible to draw firm conclusions about the effect of payment for medication, as there were too few patients in the subgroup that received free medication for <5 weeks or longer. In nearly all subgroups, there was a consistent and varying lower rate of continuous abstinence in disadvantaged patients. Interestingly, in the hospital setting, continuous abstinence was 14% lower in unemployed patients compared with non-unemployed patients.
The proportion of patients not responding to follow-up was moderate, and the sensitivity analysis revealed relatively robust findings. It should be emphasised again that the Russell criteria23 were not applicable in this registry-based cohort study.
To our knowledge, continuous abstinence of disadvantaged patients, with regard to the format, the setting, the region and payment modality, have not been reported in randomised clinical trial or in cohort studies. Most of the evidence about smoking cessation derives from randomised trials, but it is regrettable that up to six of 10 patients with nicotine dependence were not eligible for these studies because they fulfilled at least one exclusion criteria.12 In contrast to studies applying stricter inclusion criteria,11 12 24 25 our study included patients aged 18 years or older undergoing the GSP in Denmark, regardless of smoking severity, motivation to quit, comorbidity or whether a quit date were set.
In the UK, smoking cessation services have been successfully implemented in deprived areas, but low long-term cessation rates in the range of 5%–11% were reported, even though these studies included quitters at 4 weeks, exclusively.2 6 24 In the UK, only 3% of all patients were in group programmes,9 24–26 which had a higher success rate.9 24 26 Many obstacles to attendance have been identified in the UK, for example, difficulties in finding adequate transport in rural areas or reported time constraints. All of this does not seem to play a major role for Danish patients. Patients who participated in a programme with an individual format showed a favourable outcome regardless of being disadvantaged. It remains unclear whether this finding is primarily related to patient preferences or staff competencies. Those 10%–12% entering the individual format might be a selected subgroup benefiting substantially from the individualised approach. Other factors not sufficiently addressed, such as comorbidity, patient resources or motivation or the patient's ability to recall events in the past, such as a health professional's recommendation to quit, might be also important in the context of continuous abstinence after the programme.
This is a real-life nationwide evaluation of continuous abstinence in disadvantaged smokers undergoing the GSP. It has been estimated that the Smoking Cessation Database includes about 90% of all registered smoking cessation activities in Denmark, and more than 5% of all Danish smokers have been registered in the database to date.27
The proportion of unemployed patients included in our study (4%) can be considered representative for Denmark (3%–6%),28 suggesting that they were sufficiently reached.
However, patients with a lower educational level seemed to have been under-represented: in our study, there were 27% compared with 37% in the Danish population.29
The definition of disadvantaged in the present study can only be seen in the context of Danish society, and caution is needed if conclusions are drawn for societies with a different social system to that of Denmark. The discrepancies between disadvantaged and higher social classes might be more pronounced in other societies, as the degree of social consensus is relatively high in Denmark. One has to keep in mind that all outcome data rely on self-reporting, thus estimates of continuous abstinence may be too high. The difference between co-validated and self-reported continuous abstinence is reported to be between 3% and 6%.8 24 25 30
It seems that the GSP might overcome at least, to some degree, the inequity related to disadvantaged smokers. The major implication for clinicians would be to refer more disadvantaged patients to the GSPs. It is important for policy makers to ensure that disadvantaged patients do get access to these successful programmes. Promoting individual interventions among those with low education may increase the effectiveness of GSP. Future research should focus on how to bring more patients into smoking cessation intervention programmes. The dominating predictor for continuous abstinence was compliance for the disadvantaged as well as for the non-disadvantaged patient; however, the direction of causality for compliance cannot be addressed by this approach. Future research should also address the improvement of compliance and the role of pharmacies in the care of disadvantaged smokers.
What is already known on this subject.
Lower socioeconomic groups have higher smoking rates and less often access to preventive health services such as smoking cessation intervention programmes.
What this study adds.
The GSP is effective in disadvantaged patients almost to the same degree as in non-disadvantaged patients. Minor improvements may be achieved through modifications of the programme that is a change from a group to an individual format.
Footnotes
Contributors: HT and TN were responsible for the study concept and design. Staff from the smoking cessation units in Denmark collected the data. MR coordinated the data collection and processing. TN, BLH, NG and HT did the statistical analyses. All authors contributed to the interpretation of the analyses and the results. TN and HT wrote the article. BLH, MR and NG revised it. All authors approved the final edition. All authors had full access to all the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. TN and HT are guarantors for the study.
Funding: Funding was provided by the Danish National Board of Health and the Danish Ministry of Interior and Health. The funders finance the daily function of the Danish Smoking Cessation Database. The funders have not been involved in the research project.
Competing interests: None.
Patient consent: Obtained.
Ethics approval: This project was approved by the Danish Data Protection Agency (J.-Nr. 2010-41-5463) and registered at the Scientific Ethical Committee (Prot.-Nr. H-C-FSP-2010-049). All patients gave written informed consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Technical appendix is available on http://www.rygestopbasen.dk. Participants gave no informed consent for data sharing.
References
- 1. Browning KK, Ferketich AK, Salsberry PJ, et al. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob Res 2008;10:55–61 [DOI] [PubMed] [Google Scholar]
- 2. Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation? J Public Health (Oxf) 2010;33:39–47 [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization WHO Report On The Global Tobacco Epidemic, 2009: Implementing Smoke-Free Environments. 2009. http://www.who.int/tobacco/mpower/en/ [Google Scholar]
- 4. Amos A, Amos A, Bauld L, et al. 2011. Tobacco Control, Inequalities In Health And Action At A Local Level. York: Public Health Research Consortium, 2011 [Google Scholar]
- 5. Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2010;(4):CD006103. [DOI] [PubMed] [Google Scholar]
- 6. Kotz D, West R. Explaining the social gradient in smoking cessation: it's not in the trying, but in the succeeding. Tob Control 2009;18:43–6 [DOI] [PubMed] [Google Scholar]
- 7. Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev 2005;(2):CD001292. [DOI] [PubMed] [Google Scholar]
- 8. Lumley J, Chamberlain C, Dowswell T, et al. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2009;(3):CD001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2005;(2):CD001007. [DOI] [PubMed] [Google Scholar]
- 10. Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2008;(2):CD000165. [DOI] [PubMed] [Google Scholar]
- 11. Prochaska JO, Evers KE, Prochaska JM, et al. Efficacy and effectiveness trials: examples from smoking cessation and bullying prevention. J Health Psychol 2007;12:170–8 [DOI] [PubMed] [Google Scholar]
- 12. LeStrat Y, Rehm J, LeFoll B. How generalisable to community samples are clinical trial results for treatment of nicotine dependence: a comparison of common eligibility criteria with respondents of a large representative general population survey. Tob Control 2011;20:338–43 [DOI] [PubMed] [Google Scholar]
- 13. Kjaer NT, Evald T, Rasmussen M, et al. The effectiveness of nationally implemented smoking interventions in Denmark. Prev Med 2007;45:12–14 [DOI] [PubMed] [Google Scholar]
- 14. Olsen KR, Bilde L, Juhl HH, et al. Cost-effectiveness of the Danish smoking cessation interventions: subgroup analysis based on the Danish smoking cessation database. Eur J Health Econ 2006;7:255–64 [DOI] [PubMed] [Google Scholar]
- 15. Borglykke A, Pisinger C, Jorgensen T, et al. The effectiveness of smoking cessation groups offered to hospitalised patients with symptoms of exacerbations of chronic obstructive pulmonary disease (COPD). Clin Respir J 2008;2:158–65 [DOI] [PubMed] [Google Scholar]
- 16. Moller AM, Villebro N, Pedersen T, et al. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002;359:114–17 [DOI] [PubMed] [Google Scholar]
- 17. Tonnesen H. Surgery and smoking at first and second hand: time to act. Anesthesiology 2011;115:1–3 [DOI] [PubMed] [Google Scholar]
- 18. Bauld L, Chesterman J, Ferguson J, et al. A comparison of the effectiveness of group-based and pharmacy-led smoking cessation treatment in Glasgow. Addiction 2009;104:308–16 [DOI] [PubMed] [Google Scholar]
- 19. Cahill K, Perera R. Competitions and incentives for smoking cessation. Cochrane Database Syst Rev 2008;(3):CD004307. [DOI] [PubMed] [Google Scholar]
- 20. Danish Cancer Society Manual for individual smoking cessaton intervention. In: Lind M, ed. Manual For Smoking Cessation Intervention In Groups. 2nd edn Copenhagen: Internet Communication, 2008. http://www.cancer.dk/fagfolk/forebyggelse/rygning/Rygestopraadgivere/grundkurser_til_rygestopraadgivere/ (accessed 11 Nov 2011). [Google Scholar]
- 21. Heatherton TF, Kozlowski LT, Frecker RC, et al. The Fagerstrom test for nicotine dependence: a revision of the fagerstrom tolerance questionnaire. Br J Addict 1991;86:1119–27 [DOI] [PubMed] [Google Scholar]
- 22. Von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. West R, Hajek P, Stead L, et al. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction 2005;100:299–303 [DOI] [PubMed] [Google Scholar]
- 24. Ferguson J, Bauld L, Chesterman J, et al. The English smoking treatment services: one-year outcomes. Addiction 2005;100(Suppl 2):59–69 [DOI] [PubMed] [Google Scholar]
- 25. Judge K, Bauld L, Chesterman J, et al. The English smoking treatment services: short-term outcomes. Addiction 2005;100(Suppl 2):46–58 [DOI] [PubMed] [Google Scholar]
- 26. Bauld L, Bell K, McCullough L, et al. The effectiveness of NHS smoking cessation services: a systematic review. J Public Health 2010;32:71–82 [DOI] [PubMed] [Google Scholar]
- 27. OECD OECD Health data 2010. How Does Denmark Compare. 2011. http://www.oecd.org/dataoecd/46/32/38979778.pdf [Google Scholar]
- 28. Statistics Denmark Seasonally Adjusted Figures By Seasonal Adjustment And Actual Figures, Region And Time. 2011. http://www.dst.dk/HomeUK/Statistics/focus_on/focus_on_show.aspx?sci=203 [Google Scholar]
- 29. Statistics Denmark Educational Attainment Of The Population By Age, Education And Time. 2011. http://www.dst.dk/HomeUK/Statistics/focus_on/focus_on_show.aspx?sci=569 [Google Scholar]
- 30. Pisinger C, Vestbo J, Borch-Johnsen K, et al. Smoking cessation intervention in a large randomised population-based study. The inter99 study. Prev Med 2005;40:285–92 [DOI] [PubMed] [Google Scholar]