Abstract
Background
Acute Respiratory Distress Syndrome (ARDS) is a devastating condition with an estimated mortality exceeding 30%. There are data suggesting risk factors for ARDS development in high-risk populations, but few data are available in lower incidence populations. Using risk-matched analysis and a combination of clinical and research datasets, we determined the incidence and risk factors for the development of ARDS in this general surgical population.
Methods
We conducted a review of common adult surgical procedures completed between January 1, 2005 and July 1, 2009 using an anesthesia information system. This dataset was merged with an ARDS registry and an institutional death registry. Preoperative variables were subjected to multivariate analysis. Matching and multivariate regression was used to determine intraoperative factors associated ARDS development.
Results
50,367 separate patient admissions were identified, 93 (0.2%) of these patients developed ARDS. Preoperative risk factors for ARDS development included American Society of Anesthesiologist status 3-5(odds ratio (OR) 18.96), emergent surgery (OR 9.34), renal failure (OR 2.19), chronic obstructive pulmonary disease (OR 2.16), number of anesthetics during the admission (OR 1.37), and male sex (OR 1.65). After matching, intraoperative risk factors included drive pressure (OR 1.17), fraction inspired oxygen (OR 1.02), crystalloid administration in liters (1.43) and erythrocyte transfusion (OR 5.36).
Conclusion
ARDS is a rare condition postoperatively in the general surgical population and is exceptionally uncommon in low American Society of Anesthesiologists status patients undergoing scheduled surgery. Analysis after matching suggests ARDS development is associated with median drive pressure, FiO2, crystalloid volume, and transfusion.
Introduction
Acute Respiratory Distress Syndrome (ARDS) is a clinical syndrome that is defined as the rapid onset of hypoxia with a PaO2/FiO2 (P/F) ratio ≤ 300 and bilateral pulmonary infiltrates in the absence of left atrial hypertension.1 The overall in-hospital mortality of patients with ARDS is commonly thought to exceed 30%.2, 3. A subset of patients undergoing operative procedures is at higher risk for postoperative ARDS. Cardiac, thoracic, vascular, and trauma surgeries are high-risk for the development of postoperative ARDS;4-7 however, the incidence and risk factors for new onset postoperative ARDS in the noncardiothoracic, vascular, and trauma surgical populations have not been well defined. In addition, intraoperative ventilator and fluid management may influence the incidence of ARDS after pneumonectomy and other intrathoracic procedures.7, 8. Hence, ventilator and fluid management may impact ARDS development in other populations.9
In our previous work, we demonstrated that patients with a low intraoperative P/F ratio were typically managed using increased FiO2 and peak airway pressures.10 We have also shown that patients with a preoperative diagnosis of ARDS are not typically managed using a lung protective ventilation strategy incorporating low tidal volumes (Vt) and levels of positive end expiratory pressure (PEEP) supported by the critical care literature.11 However, this prior work did not explicitly investigate patients without ARDS prior to their operation. Therefore, we sought to determine the incidence of new onset ARDS in what have traditionally been thought of as low-incidence cases in a broad surgical population. Furthermore, we sought to determine preoperative risk factors for the development of ARDS in this population, and if intraoperative management of patients that developed ARDS was fundamentally different from those patients that did not develop the condition. We tested the hypothesis that patients with known predictors of end-organ dysfunction, large volume resuscitations, and extended exposure to elevated ventilator settings would be at increased risk for the development of postoperative ARDS.
Materials and Methods
Institutional Review Board approval was obtained for this cohort study at The University of Michigan Health System (IRB-MED, Ann Arbor, Michigan), a large, tertiary care facility. All data were deidentified prior to analysis, and a waiver of consent was obtained for this study. All cases recorded in the anesthesia information management system (Centricity, General Electric Healthcare, Waukesha, WI) from June 1, 2004 to June 1, 2009 were screened for inclusion. All cases on the cardiac, thoracic, transplant, trauma, and vascular surgery services were excluded, as were cases with no recorded service.
Preoperative data were prospectively collected from routine clinical documentation that was entered into the anesthesia information management system at the point of care. The record includes a structured preoperative history and physical examination allowing for coded entry and free text where required. Data abstracted from the preoperative history included age, sex, primary surgical service, American Society of Anesthesiologists (ASA) classification, diabetes, hypertension, coronary artery disease, congestive heart failure, renal failure, liver disease, asthma, chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, smoking status, and height. Variables were selected for either their previous association with the development of ARDS, necessary for the management of patients with ARDS or high risk of organ dysfunction potentially requiring intensive care unit admission.5, 6, 12-15 Variables that may be associated with the development of ARDS but do not have a structured area of documentation in the anesthesia information management system were not included in the analysis. A detailed description of variable definitions is included in appendix 1. Free text entries were hand-coded by the research team for analysis. From the height variable, the predicted body weight was calculated for this study using the formula 50 + 2.3 (height (in) − 60) for men and 45.5 + 2.3 (height (in) − 60) for women.
Unique hospital admissions were considered as the base unit for analysis. In those admissions containing multiple anesthetic cases, data were analyzed from the last case of the admission or the last case prior to development of ARDS, as appropriate. Records from the final anesthetic of each admission were also used to determine preoperative comorbidities and ASA status. Based on preliminary data analysis, the ASA status recorded for this final case was collapsed into a binary variable reflecting whether a patient was considered ASA 1-2 or ASA 3-5. For those hospitalizations containing multiple surgical cases, the total number of surgical procedures during each admission was also calculated and included in analysis. After initial analysis, it was decided that multiple admissions in the seven days prior to an ARDS event would be managed by retaining the admission most proximal to the diagnosis and excluding the other admissions.
Intraoperative physiologic and ventilator data were acquired using an automated, validated electronic interface from the anesthesia machine (Aisys, General Electric Healthcare) and physiologic monitors (Solar 9500; General Electric Healthcare).12, 13, 16, 17 Fraction inspired oxygen (FiO2), peak inspiratory pressure (PIP), exhaled Vt, PEEP, oxyhemoglobin saturation (SpO2), drive pressure(ΔP, defined as PIP-PEEP), respiratory rate were obtained and analyzed for median values to eliminate spurious and isolated values. Based on previous data, the duration of high pressure ventilation may be associated with development of ARDS.7 Considering this data, we chose to examine the number of 10-min epochs of median PIP >30 cmH2O, and number of 10-min epochs of median Vt > 12 cc/kg predicted body weight from the time of incision to the end of anesthesia.2 This technique has been used in prior to studies to eliminate artifact and spurious values over relatively short periods of time.12, 13
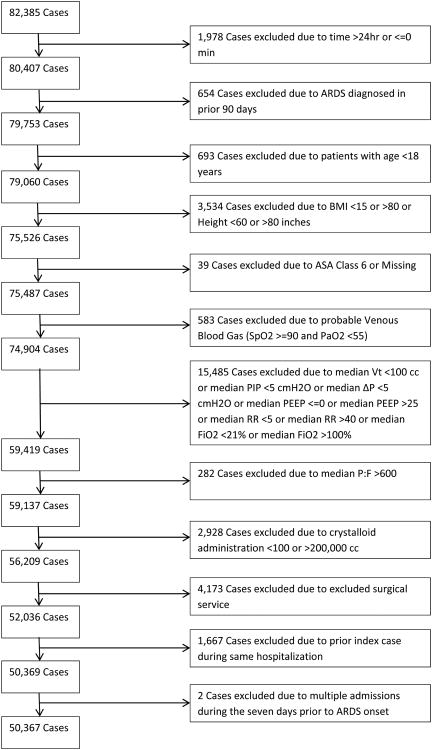
Case times were validated as having started and ended by having electronically documented heart rate from electrocardiogram or electronically documented start, incision, and end times in the event electrocardiogram data was not available. Cases with negative or undocumented times were excluded. Cases from patients graded as ASA classification 6 were also excluded as the ventilation strategy implemented may have been designed to favor perfusion to other organs. A summary of inclusion and exclusion criteria are presented in figure 1.
Figure 1. Method of case exclusion.
* Ventilator setting exclusion criteria include Vt < 100, PIP<5, driving pressure <5, 0>PEEP>25, 5>RR>40,21>FiO2>100
** Other exclusion criteria for which no additional patients were excluded were: 45mmHg>PaO2>600mmHg, PIP epochs<0, Vt Epochs<0, PRBC>200, FFP>200, Colloid<0, Cryoprecipiate <0
ARDS = acute respiratory distress syndrome; ASA = American Society of Anesthesiologists; BMI = body mass index; FFP = fresh frozen plasma;PaO2 = partial pressure of oxygen;P:F = PaO2/FiO2; PRBC = packed erythrocytes;SpO2 = hemoglobin saturation; PEEP = positive end expiratory pressure; PIP = peak inspiratory pressure; RR = risk ratio; Vt = tidal volume.
When available, we analyzed values for the intraoperative arterial blood gases that were manually entered by the anesthetic team into the structured electronic perioperative information system (Centricity, General Electric Healthcare). From the recorded intraoperative PaO2 values and FiO2 the P/F ratio was calculated for each available blood gas. Volumes of crystalloid, colloid, units of packed erythrocytes, units of fresh frozen plasma, and units of platelets were also obtained from the electronic anesthetic record.
To identify the subpopulation of patients who went on to develop ARDS, patients in the operative dataset were merged with a dedicated prospectively collected research dataset of all adult critical care patients on ventilators at the University of Michigan Medical Center who were screened for entry into ARDS studies. For the purposes of this investigation, only patients receiving mechanical ventilation after their anesthetic were screened for ARDS. In this research dataset, ARDS was diagnosed through analysis of the patient's ventilator status, arterial blood gases, chest x-ray, and clinical documentation. Patients were deemed positive for the primary outcome of ARDS if they were on a ventilator, had bilateral infiltrates on chest x-ray as determined by a clinician, had a P/F ratio ≤ 300, and had minimal evidence of left atrial fluid overload. Patients were included in the postoperative ARDS group if the date of ARDS onset was determined to be between postoperative days 0 and 7, inclusive. Patients who developed ARDS on the day of their operation were examined by one of the authors (JMB), and those with a diagnosis of ARDS prior to their anesthetic were excluded. Finally, mortality data was collected from an institutional death database to compare the mortality of the propensity matched groups both with and without ARDS in order to determine the risk presented to patients that develop ARDS. This database is constructed using multiple resources including in-hospital mortality, failed follow-up at clinic visits and the social security death master file.
Statistical Analysis
Statistical analysis was performed using R version 2.14 (R Foundation for Statistical Computing, Vienna, Austria). Population characteristics were examined using Student's t-test, Pearson's chi-square test, Mann-Whitney U test, or Fisher's exact test, as appropriate for the distribution of the data. Collinearity diagnostics were performed, and a condition index >30 was examined with a bivariate correlation matrix, with a pairwise correlation threshold of >0.70 for problematic collinearity. All variables that were significantly different between groups (p < 0.05) were entered into a logistic regression model. Bootstrap samples (R=1,000 replicates) were chosen and backward stepwise selection was used to fit a parsimonious regression model to each sample. It was determined a priori that those variables retained in ≥60% of all bootstrapped models would be retained for the final model.18 This parsimonious model was fit in R = 1000 bootstrap samples to determine percentile confidence intervals for the odds ratio (OR) and absolute risk difference for each variable.19, 20 The fit and predictive capability of the model was assessed using 10-fold cross-validation of the Hosmer-Lemeshow Goodness of Fit test and Receiver Operating Characteristic – Area Under the Curve (ROC-AUC).21
Controls were then matched to cases based on their preoperative likelihood of developing ARDS. All preoperative variables that were significantly different between groups were entered into an optimal matching algorithm, which is similar to a greedy algorithm but also minimizes the overall distance between groups.22, 23 The data analysis plan specified that all cases of ARDS were to be retained if the intra-variable difference between matched groups was reduced to <0.2 standard deviations. In the case of intra-variable differences >0.2 standard deviations, data would first be grouped into appropriate quantiles for those variables, and then matching would proceed within each quantile. After initial data analysis, the matching ratio was increased to 4:1, which would be sufficient to detect a between-group difference in ΔP of 2 cm H2O or Vt of 0.75 cc/kg with >80% power. Percent improvement in balance between the groups was examined, and population characteristics were again described using the appropriate statistical tests.
The role of intraoperative management was then examined through a second predictive model, constructed on the risk-matched patient population. Median ΔP, median respiratory rate, median FiO2, number of 10-min epochs of PIP ≥30 cmH20, number of 10-min epochs of Vt ≥12 cc/kg predicted body weight, transfusion of packed erythrocytes, transfusion of platelets, use of fresh frozen plasma, use of colloid, total volume of crystalloid, and duration of case were entered into a conditional logistic regression model, accounting for the matched nature of the data. Backward stepwise conditional logistic regression was used within bootstrap samples (R = 1000), as described above. Those variables that were significant predictors in ≥60% of samples comprised the final parsimonious predictive model. Bootstrap percentile confidence intervals were constructed for the ORs of each predictor. This model was examined using the Hosmer-Lemeshow Goodness of Fit statistic and the ROC-AUC. Calculation of absolute risk difference and cross-validation of the ROC-AUC were not performed, as conditional logistic regression models cannot be used for computing the predicted values necessary for these statistics.18, 19, 24
Due to the hierarchical nature of the study design, some patients contributed multiple cases to the data set. Intraclass correlation coefficients were estimated for each variable, to understand the degree to which repeated measures were likely to be correlated with prior measures. To quantify the effect of these correlations on the predictive models, a sensitivity analysis was performed in a dataset without multiple observations. Specifically, only those patients who had a single anesthetic during their first admission were included; any further admissions for those patients were excluded from the dataset. The analysis above was repeated with only these patients.
Furthermore, because a considerable number of cases did not have a recorded estimated blood loss (EBL), this variable was excluded from the initial model and considered in a separate sensitivity analysis. Cases were divided into EBL quintiles then matched within each quintile based on preoperative risk factors, as above. After thus controlling for surgical blood loss, the intraoperative parsimonious predictive model developed above was fit to these data and bootstrap percentile confidence intervals determined for the OR and absolute risk difference of each predictor.
Results
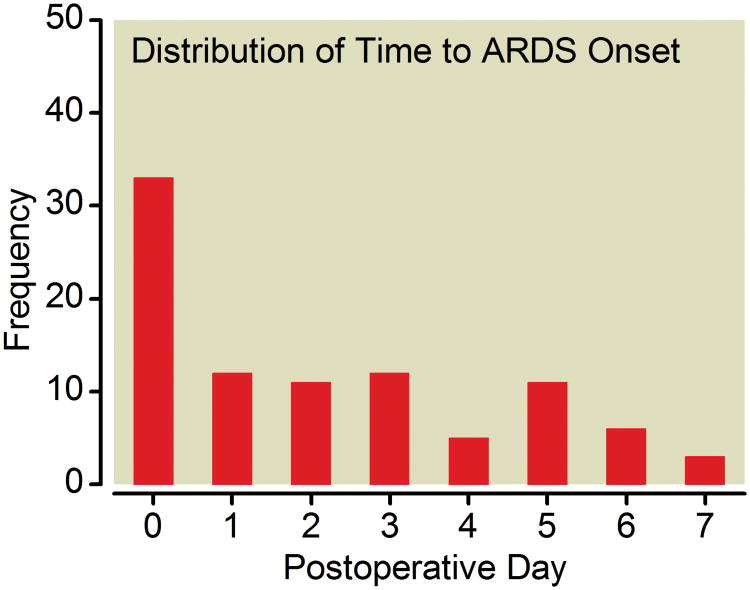
Data were reviewed for 82,385 anesthetic cases, and a summary of excluded cases is shown in figure 1. Of the 50,367 hospitalizations analyzed, 93 (0.2%) were complicated by postoperative ARDS. The median time to onset of postoperative ARDS was 2 days (fig. 2). There were several significant differences in patients who did and those who did not develop postoperative ARDS (table 1). Most patients were admitted only once during the study period (34,535 patients, 83.8%), although the number of admissions per patient ranged from 1 to 15 (table 2). The majority of hospitalizations contained only one anesthetic case during that admission (48,873 admissions, 97.0%), although the number of cases per admission ranged from 1 to 14 (table 2).
Figure 2. Postoperative Day of ARDS Onset.
ARDS = Acute Respiratory Distress Syndrome
Table 1. Patient Characteristics.
| ARDS (n = 93) Median | IQR | Control (n = 50,274) Median | IQR | p | |
|---|---|---|---|---|---|
|
|
|||||
| Age | 59 | (48.0, 73.0) | 51 | (39.0, 63.0) | <0.001 |
| BMI | 26.9 | (22.8, 34.8) | 27.6 | (24.0, 32.4) | 0.996 |
| Anesthetics per admission | 1 | (1, 1) | 1 | (1, 1) | <0.001 |
| n | % | n | % | ||
| Male | 62 | 67% | 23,210 | 46% | <0.001 |
| Emergent Case | 33 | 35% | 2,145 | 4% | <0.001 |
| ASA Class ≥ 3 | 86 | 92% | 15,759 | 31% | <0.001 |
| Former Smoker | 20 | 22% | 10,132 | 20% | 0.700 |
| Current Smoker | 18 | 19% | 8,242 | 16% | 0.403 |
| Ethanol Abuse | 6 | 6% | 1,667 | 3% | 0.133 |
| Diabetes | 25 | 27% | 6,558 | 13% | <0.001 |
| Hypertension | 50 | 54% | 18,204 | 36% | 0.001 |
| Coronary Artery Disease | 17 | 18% | 4,032 | 8% | 0.002 |
| Congestive Heart Failure | 12 | 13% | 1,534 | 3% | <0.001 |
| Renal Failure | 25 | 27% | 2,729 | 5% | <0.001 |
| Liver Disease | 3 | 3% | 954 | 2% | 0.260 |
| Asthma | 1 | 1% | 3,987 | 8% | 0.007 |
| COPD | 22 | 24% | 2,694 | 5% | <0.001 |
| Sleep Apnea | 10 | 11% | 4,378 | 9% | 0.460 |
ARDS = acute respiratory distress syndrome; ASA = American Society of Anesthesiologists; BMI = body mass index; COPD = chronic obstructive pulmonary disease; IQR = interquartile range.
Table 2. Summary of Anesthetic Frequencies per Admission and Number of Admissions per Patient.
| Number of Anesthetics | Number of Admissions in Dataset (n, %) | Number of Admissions | Number of Patients | ||
|---|---|---|---|---|---|
| 1 | 48,873 | 97.0% | 1 | 34,535 | 83.8% |
| 2 | 1,118 | 2.2% | 2 | 5,008 | 12.2% |
| 3 | 228 | 0.5% | 3 | 1,121 | 2.7% |
| 4 | 79 | 0.2% | 4 | 341 | 0.8% |
| 5 | 33 | 0.1% | 5 | 106 | 0.3% |
| 6 to 10 | 30 | 0.1% | 6 to 10 | 72 | 0.2% |
| 11 to 14 | 6 | 0.0% | 11 to 15 | 6 | 0.0% |
In an attempt to reduce the impact of linked factors in the regression, a condition number of 13.8 was calculated, well below the threshold of 30, suggesting that no changes were necessary to address collinearity. Seven variables were retained in >60% of bootstrap samples: ASA physical status ≥3, emergent procedure, asthma, renal failure, COPD, male gender, and the number of anesthetics during admission (table 3). In 10-fold cross-validation, the Hosmer-Lemeshow Goodness of Fit test was non-significant in each validation sample and the mean ROC-AUC 0.886 (95% CI 0.785 to 0.979).
Table 3. Alternate – Absolute Risk Reduction and Odds Ratio.
| Number of models retaining variable | OR | Absolute Risk Difference | Significant at α =0.05 | |
|---|---|---|---|---|
|
|
||||
| ASA ≥3 | 1,000 | 18.96 (9.63, 61.39) | 0.40% (0.30, 0.50) | * |
| Emergent Procedure | 1,000 | 9.34 (5.69, 14.52) | 1.00% (0.61, 1.40) | * |
| Asthma | 969 | 0.13 (0.00, 0.52) | −0.17% (−0.23, −0.09) | |
| Renal Failure | 936 | 2.19 (1.28, 3.39) | 0.18% (0.04, 0.33) | * |
| COPD | 907 | 2.16 (1.24, 3.54) | 0.18% (0.04, 0.36) | * |
| Male | 837 | 1.65 (1.04, 2.55) | 0.09% (0.01, 0.16) | * |
| Number of anesthetics during admission | 797 | 1.37 (1.10, 1.61) | 0.05% (0.02, 0.07) | * |
| CAD | 471 | - | - | |
| Hypertension | 356 | - | - | |
| CHF | 245 | - | - | |
| Age | 223 | - | - | |
| Diabetes | 175 | - | - | |
ASA = American Society of Anesthesiologists; CAD = coronary artery disease; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; OR = odds ratio.
Matching resulted in a 99.2 % balance improvement, and all intravariable differences between matched groups were <0.2 standard deviations. No significant differences remained between the two matched groups following matching (table 4). After matching on preoperative risk, mortality remained significantly higher in the group that developed ARDS than in the control group, both at 28 days (22% vs. 7%, p < 0.001) and at 90 days (27% vs. 12%, p < 0.001).
Table 4. Post-Matching Demographics.
| ARDS n = 93 | Control n = 372 | p | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
|
|
|||||
| Age | 59 | (48, 73) | 59 | (47, 70) | 0.651 |
| Anesthetics per admission | 1 | (1, 1) | 1 | (1, 1) | 0.382 |
| n | % | n | % | ||
| Male | 62 | 67% | 233 | 63% | 0.547 |
| Emergent Case | 33 | 35% | 129 | 35% | 0.903 |
| ASA | 0.351 | ||||
| 1 | 0 | 0% | 11 | 3% | - |
| 2 | 7 | 8% | 18 | 5% | - |
| 3 | 48 | 52% | 179 | 48% | - |
| 4 | 37 | 40% | 160 | 43% | - |
| 5 | 1 | 1% | 4 | 1% | - |
| Former Smoker | 20 | 22% | 113 | 30% | 0.097 |
| Current Smoker | 18 | 19% | 61 | 16% | 0.537 |
| Ethanol Abuse | 6 | 6% | 23 | 6% | 1.000 |
| Diabetes | 25 | 27% | 100 | 27% | 1.000 |
| Hypertension | 50 | 54% | 184 | 49% | 0.488 |
| Coronary Artery Disease | 17 | 18% | 63 | 17% | 0.760 |
| Congestive Heart | |||||
| Failure | 12 | 13% | 51 | 14% | 1.000 |
| Renal Failure | 25 | 27% | 94 | 25% | 0.791 |
| Liver Disease | 3 | 3% | 12 | 3% | 1.000 |
| Asthma | 1 | 1% | 11 | 3% | 0.474 |
| COPD | 22 | 24% | 77 | 21% | 0.571 |
ARDS = acute respiratory distress syndrome; ASA = American Society of Anesthesiologists; COPD = chronic obstructive pulmonary disease; IQR = interquartile range.
To assess the impact of intraoperative management on subsequent ARDS development, a predictive model was built including several ventilator and transfusion settings. A summary of variables examined is provided in table 5. Five variables were retained in ≥60% of reverse selection bootstrap replicates: median ΔP, median FiO2, transfusion of packed erythrocytes, transfusion of platelets, and total volume of crystalloid administered (table 6). This model was well-fit by the Hosmer-Lemeshow test (p = 0.718). The ROC-AUC for this model was 0.851 (DeLong 95% CI 0.805 to 0.897).
Table 5. Intraoperative Characteristics.
| ARDS n = 93 | Control n = 372 | p | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
|
|
|||||
| Median Δ Pressure | 24 | (19, 28) | 18 | (15, 22) | <0.001 |
| Median PIP | 27 | (22, 33) | 21 | (17, 26) | <0.001 |
| Median PEEP | 4 | (2, 5) | 4 | (0, 5) | 0.233 |
| Median Tidal Volume | 580 | (479, 690) | 553 | (480, 616) | 0.003 |
| Median Tidal Volume (cc/kg PBW) | 9.0 | (7.5, 10.1) | 8.5 | (7.3, 9.7) | 0.053 |
| Epochs of PIP ≥30 | 1 | (0, 14) | 0 | (0, 0) | <0.001 |
| Epochs of Vt> 12 cc/kg PBW | 0 | (0, 1) | 0 | (0, 0) | <0.001 |
| Median RR | 12 | (10, 14) | 11 | (10, 12) | 0.02 |
| Median FiO2 | 76 | (52, 96) | 55 | (45, 93) | 0.001 |
| Case Length (minutes) | 251 | (189, 410) | 180 | (120, 268) | <0.001 |
| Crystalloid (L) | 3.2 | (2.0, 4.8) | 2.0 | (1.3, 3.0) | <0.001 |
| n | % | n | % | p | |
| Received Packed Erythrocytes | 38 | 41% | 54 | 15% | <0.001 |
| Received Platelets | 13 | 14% | 15 | 4% | 0.001 |
| Received Colloid | 37 | 40% | 67 | 18% | <0.001 |
| Received FFP | 13 | 14% | 17 | 5% | 0.003 |
ARDS = acute respiratory distress syndrome; FiO2 = fraction of inspired oxygen; FFP = fresh frozen plasma;IQR = interquartile range; PBW = predicted body weight; PEEP = positive end-expiratory pressure; PIP = peak inflation pressure;RR = risk ratio;Vt = low tidal volume.
Table 6. Intraoperative Predictors.
| Bootstraps Retaining Variable (#) | OR | Significant at α =0.05 | |
|---|---|---|---|
|
|
|||
| Median Drive Pressure | 914 | 1.17 (1.09, 1.31) | * |
| Packed Erythrocyte Transfusion | 869 | 5.36 (1.39, 11.11) | * |
| Median FiO2 | 797 | 1.02 (1.00, 1.05) | * |
| Crystalloid (L) | 704 | 1.43 (1.15, 1.93) | * |
| Platelet Transfusion | 621 | 5.36 (0.88, 64.75) | |
| Epochs of PIP ≥30 | 511 | - | |
| Median RR | 424 | - | |
| Case Duration | 361 | - | |
| Median Vt | 335 | - | |
| Colloid administration | 303 | - | |
| FFP Transfusion | 282 | - | |
| Epochs of Vt ≥12 cc/kg | 249 | - | |
FiO2 = fraction of inspired oxygen; FFP = fresh frozen plasma; OR = odds ratio;PIP = peak inflation pressure; RR = risk ratio;Vt = low tidal volume.
By identifying those patients who underwent only a single anesthetic during their first admission and excluding any further admissions for those patients, we constructed a cohort of 37,697 unique patients, of whom 62 (0.16%) developed postoperative ARDS. Analysis of this cohort found preoperative predictors identical to those selected the in larger population, with very similar OR, except for the logical removal of the number of cases per admission. Intraoperative predictors for this cohort were also quite similar, although only median ΔP (OR 1.15, 95% CI 1.05 to 1.31), packed erythrocyte transfusion (OR 4.05, 95% CI 1.29 to 17.55), and volume of crystalloid in L (OR 1.56, 95% 1.13 to 2.29) achieved statistical significance.
Valid estimates of surgical blood loss (EBL) were available for 30,234 cases, of which 71 (0.23%) resulted in postoperative ARDS. Within each EBL quintile, cases were matched to controls based on preoperative risk factors. After controlling for EBL, Median ΔP (OR 1.17, 95% CI 1.09 to1.27), platelet transfusion (OR 13.59, 95% CI 1.09 to 100) and volume of crystalloid in L (OR 1.43, 95% CI 1.02 to 2.26) remained significant risk factors for ARDS development.
Discussion
ARDS is among the most devastating postoperative complications and is associated with significant mortality.5, 25 The main results of this study are as follows: 1) In a general surgical population presenting to the operating room without ARDS, the overall incidence of new onset postoperative ARDS was approximately 0.2%; 2) The risk of ARDS was extremely low in ASA Class 1-2 patients; 3) Patients with ASA Class 3-5, emergency surgery, renal failure, COPD, and multiple anesthetics are at an increased risk of ARDS; 4) After controlling for patient comorbidities and risk factors, intraoperative ΔP, increased FiO2, volume of crystalloid, and transfusion are associated with the development of ARDS; 5) Development of ARDS greatly increases patient mortality, regardless of preoperative comorbidities.
Considerable research has helped ascertain preoperative risk factors for postoperative respiratory complications.26-30 Although there is some literature investigating the development of ARDS postoperatively, most of this work has focused on high-risk elective surgeries such as cardiac and thoracic interventions.3-7, 31 This study focused on a relatively common surgical population, a group of patients seen in hospitals throughout the world with a low incidence of ARDS that has precluded prospective study.
Preoperative univariate associations with the development of ARDS in our cohort were similar to prior studies, reflecting a greater number of comorbidities among the patients who developed ARDS.5, 7 In multivariate analysis, only ASA status, emergent surgical procedure, renal failure, COPD, and number of anesthetics were significant predictors of future ARDS. A history of being an active smoker and ethanol abuser did not meet statistical significance for predicting ARDS, although they have been associated with ARDS risk in other populations.7 This may be because such conditions are common in the surgical populations which prior have focused upon. The great importance of ASA status in predicting postoperative ARDS suggests that the actual comorbidities are less important, except for renal failure and COPD, than the preoperative medical optimization of comorbidities. From this data, ASA 1 and 2 patients are at low risk of the development of ARDS and patients undergoing emergency surgery may present a unique cohort deserving special attention.
The data from this study suggests asthmatic patients may be protected from ARDS. While a type I error is possible given the low incidence of asthma in our population, several asthma treatments have been suggested to be potentially effective in ARDS, despite sparse data.32-36 Prior studies have focused on the administration of agents after the onset of ARDS, whereas the patients in our study would have received treatment prophylactically. Although beyond the scope of the present investigation, this is an issue that we feel is worthy of future study.
After matching, it appears that intraoperative ventilator management may impact the development of postoperative ARDS. The finding that exposure to higher ΔP appears to increase the odds of ARDS development is consistent with the findings by other investigators in higher risk populations demonstrating that increased PIPs were similarly predictive of ARDS.5, 7 However, our data suggest that exposure to elevated PIP with a lack of PEEP is a component of the development of ARDS. This may be because such ventilator settings introduce barotrauma and atelectrauma, potentially compounding lung injury. The fact increased pressures but not increased Vt were predictive of future ARDS is interesting. Much of the work in the critical care community in preventing ARDS mortality has focused on the use of low Vt ventilation.2, 37-41 Previous perioperative literature suggests both pressure and volume may be important in preventing ARDS. Increased pressures appear to be consistent predictors of future ARDS,4-7, 31 while a protocol that focused on low Vt, and consequently, lower plateau pressures has shown a specific association with a reduction in the incidence of ARDS in thoracic surgery patients.8 Our current study appears to support that increased ΔP with low PEEP is associated with the development of ARDS to a greater degree than elevated Vt or PIP alone.
Our analysis also showed intraoperative fluid and transfusion of blood products to be significantly associated with the onset of ARDS. Transfusion related acute lung injury has been described in the literature.42 The use of blood products in our population may be an indicator of more aggressive resuscitation, and as such, this would support works that showed that increased volume resuscitation was predictive of future ARDS.5, 8, 9, 43 Given the observational nature of the current study, no recommendations can be made about the use of blood products or volume resuscitation intraoperatively for the prevention of ARDS, but this area certainly warrants further investigation.
ARDS is known to be associated with approximately 30 to 40% mortality at 90 days.2, 25, 44 In our previous work, patients that underwent an anesthetic at our institution with a preoperative diagnosis of ARDS had a 32% 90 day mortality, compared to 19% mortality for those who underwent an anesthetic with a P/F ratio < 300 without meeting criteria for ARDS.11 Fernandez-Perez found a 60-day mortality of 27% compared to 1% for patients that did not have pulmonary complications.5 In this study, after matching, we have shown 27% mortality at 90 days for those patients that develop ARDS after their anesthetics, compared to 12% for those that do not. The development of ARDS in this cohort is associated with an increase in mortality and is a worthwhile target for efforts at prevention.
This study has several limitations. First, the data were collected as part of routine clinical care and were not subject to the validation processes used in prospective trials. Although data is typically entered through a predefined selection process for each variable, there was no formal training on the definitions for each variable (appendix 1). In addition, free text is allowed in all fields and was to interpretation by the research team. Models from such data have become common in the literature and have correlated with models based on prospectively collected data by dedicated research staff.13, 45 Additionally, items that may be associated with the development of ARDS that are not provided with specific coded entry boxes such as sepsis and aspiration were not included in the model. Next, the data are from a single, large, tertiary care center, collected over several years. The patient population may have changed over time and may not represent the typical patient seen in other locations. The database used to determine if patients had ARDS required mechanical ventilation and hence may underestimate the true frequency of ARDS. The etiology of the ARDS, whether it was primary or secondary to another insult was not determined and may itself be predictive of outcome. Additionally, we cannot be completely confident the elevated ΔP and increased FiO2 requirements were not signs of ARDS that had developed since the last datapoint was obtained preoperatively. Intraoperatively, there was not collection of plateau pressures and hence analysis was limited to PIP. While PIP has been used in several intraoperative ARDS manuscripts, it is limited and can be considerably higher than plateau pressures based on a variety of factors. Finally, the mortality data is based on an internal death registry and may not capture potential mortality of patients that were discharged to another long-term facility for ongoing care.
Due to the observational nature of this study, we did not have specific protocols for the intraoperative and postoperative management of the patient population other than routine clinical care. There was no mandated ventilator or fluid protocol at any point during the care of the patients involved in this study, including the postoperative period. However, despite this, there were statistically significant predictors of future ARDS determined both preoperatively and intraoperatively. Furthermore, in observational studies using clinical databases, the problem of model overfitting can be particularly vexing. We used several different bootstrapping techniques to reduce the variance in our models and select robust predictors, thereby minimizing the risk of type I statistical error. However, no amount of statistical testing can replace prospective validation of the predictive model and further study of interventions to mitigate risk. Ideally, the best evidence supporting the role of high pressure ventilation and development of ARDS in the surgical population would be a randomized controlled trial. Using the preoperative predictors described, one could develop criteria for enrollment in such a trial. However, careful consideration must be given to the design and ethical implications of such a study.
Despite the limitations, this investigation provides new evidence for a poorly studied population. We again demonstrated the high attributable mortality associated with the diagnosis of postoperative ARDS. We documented an exceptionally low incidence of postoperative ARDS in a general surgical population, particularly in the ASA 1 and 2 patients. Postoperative ARDS was predicted with high reliability using a model based on preoperative ASA, emergent surgical case, COPD, renal failure, and multiple surgeries. After matching, additional intraoperative risk factors for the development of ARDS(ΔP, increased FiO2, fluid administration, and transfusion) were identified, potentially offering clinicians opportunities to reduce the risk of postoperative ARDS. However, further investigation is still required before causation can be firmly established.
MS #201204133 – Final Boxed Summary Statement.
What we already know about this topic
Isoflurane produces both experimental neuroprotective and neurotoxic effects on the developing brain, depending on the duration and level of exposure
What this article tells us that is new
Using a human neural progenitor cell line, the authors confirmed and extended the dual effect of isoflurane exposures, and demonstrated the pivotal role of differential regulation of intracellular calcium in the cellular and molecular mechanisms of these effects
Acknowledgments
Support was provided from National Institutes of Health/National Center for Research Resources (UL1RR024986), Bethesda, Maryland; the University of Michigan, Ann Arbor, Michigan, and the Department of Anesthesiology at the University of Michigan, Ann Arbor, Michigan.
Appendix 1. Anesthesia Information Management System Fields
Below are the fields available in the Centricity Anesthesia Information Management System that were coded as positive for each comorbidity examined. Fields that contained provider-entered free text were reviewed and hand-coded by the research team. Common free-text entries are also provided for relevant fields; while these are not exhaustive, they are representative of the data considered to indicate a positive response for each condition.
Hypertension: Duration: <Any>
Hypertension: Control: <Any>
Hypertension: Reported Usual BP: Any
- -Common text responses coded as positive:
- “Borderline”
- “Treated with diet/exercise”
Diabetes: Type: <Any>
Diabetes: Treatment: <Any>
Diabetes: Onset: <Any>
- -Common text responses coded as positive:
- “Prediabetes”
- “Insulin resistance”
- “Glucose intolerance”
- “Gestational diabetes”
CAD: Class: <Any>
CAD: Treatment: <Any>
CAD: CABG
CAD: Angioplasty
CAD: “CAD recorded, no symptoms”
CAD: Stability: <Any>
- -Common text responses coded as positive:
- “CABG”
- “Coronary stent(s)”
- “History of MI (myocardial infarction)”
CHF: Chronicity: <Any>
CHF: Class: <Any>
CHF: Etiology: <Any>
Renal Failure: Type: <Any>
Renal Failure: Etiology: <Any>
Renal Failure: Chronic insufficiency
Renal Failure: Complications: <Any>
Renal Failure: CRI
Renal Failure: Cr <Any>
Renal Failure: Last Dialyzed: <Any>
- -Common text responses coded as positive:
- “S/P Renal transplant”
Liver Disease: Hepatitis Type: <Any>
Liver Disease: Ascites
Liver Disease: Cirrhosis
- -Common text responses coded as positive:
- “Autoimmune hepatitis”
- “Wilson's Disease”
- “Steatohepatitis”
Asthma: Classification: <Any>
Asthma: Symptom Frequency: <Any>
Asthma: ER Visits: <Any>
Asthma: Hospitalization: <Any>
COPD: Type: <Any>
COPD: Severity: <Any>
Sleep Apnea: “Treated by BIPAP/CPAP”
Sleep Apnea: “Snores loud enough to wake themselves/others up”
Sleep Apnea: “Symptomatic, untreated”
Sleep Apnea: “Stops breathing at night”
Sleep Apnea: “Tested positive for sleep apnea”
Sleep Apnea: “Treated by surgery”
Alcohol: Abuse History: Current abuser
Alcohol: Drinks Per Day: <Any number greater or equal to two>
Alcohol: Amount: High
BIPAP = Bilevel Positive Airway Pressure; BP = blood pressure; CAD = coronary artery disease; CABG = coronary artery bypass graft; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; CPAP = continuous positive airway pressure; Cr = Creatinine; CRI = chronic renal insufficiency; ER = emergency room; MI = myocardial infarction; S/P = status post.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–24. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 2.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–8. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 3.Dulu A, Pastores S, Park B, Riedel E, Rusch V, Halpern N. Prevalence and mortality of acute lung injury and ARDS after lung resection. Chest. 2006;130:73–8. doi: 10.1378/chest.130.1.73. [DOI] [PubMed] [Google Scholar]
- 4.Fernandez-Perez ER, Keegan MT, Brown DR, Hubmayr RD, Gajic O. Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Anesthesiology. 2006;105:14–8. doi: 10.1097/00000542-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez-Perez ER, Sprung J, Afessa B, Warner DO, Vachon CM, Schroeder DR, Brown DR, Hubmayr RD, Gajic O. Intraoperative ventilator settings and acute lung injury after elective surgery: A nested case control study. Thorax. 2009;64:121–7. doi: 10.1136/thx.2008.102228. [DOI] [PubMed] [Google Scholar]
- 6.Gajic O, Dabbagh O, Park PK, Adesanya A, Chang SY, Hou P, Anderson H, 3rd, Hoth JJ, Mikkelsen ME, Gentile NT, Gong MN, Talmor D, Bajwa E, Watkins TR, Festic E, Yilmaz M, Iscimen R, Kaufman DA, Esper AM, Sadikot R, Douglas I, Sevransky J, Malinchoc M. Early identification of patients at risk of acute lung injury: Evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183:462–70. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Licker M, de Perrot M, Spiliopoulos A, Robert J, Diaper J, Chevalley C, Tschopp JM. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth Analg. 2003;97:1558–65. doi: 10.1213/01.ANE.0000087799.85495.8A. [DOI] [PubMed] [Google Scholar]
- 8.Licker M, Diaper J, Villiger Y, Spiliopoulos A, Licker V, Robert J, Tschopp JM. Impact of intraoperative lung-protective interventions in patients undergoing lung cancer surgery. Crit Care. 2009;13:R41. doi: 10.1186/cc7762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughes CG, Weavind L, Banerjee A, Mercaldo ND, Schildcrout JS, Pandharipande PP. Intraoperative risk factors for acute respiratory distress syndrome in critically ill patients. Anesth Analg. 2010;111:464–7. doi: 10.1213/ANE.0b013e3181d8a16a. [DOI] [PubMed] [Google Scholar]
- 10.Blum JM, Fetterman DM, Park PK, Morris M, Rosenberg AL. A description of intraoperative ventilator management and ventilation strategies in hypoxic patients. Anesth Analg. 2010;110:1616–22. doi: 10.1213/ANE.0b013e3181da82e1. [DOI] [PubMed] [Google Scholar]
- 11.Blum JM, Maile M, Park PK, Morris M, Jewell E, Dechert R, Rosenberg AL. A description of intraoperative ventilator management in patients with acute lung injury and the use of lung protective ventilation strategies. Anesthesiology. 2011;115:75–82. doi: 10.1097/ALN.0b013e31821a8d63. [DOI] [PubMed] [Google Scholar]
- 12.Kheterpal S, O'Reilly M, Englesbe MJ, Rosenberg AL, Shanks AM, Zhang L, Rothman ED, Campbell DA, Tremper KK. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110:58–66. doi: 10.1097/ALN.0b013e318190b6dc. [DOI] [PubMed] [Google Scholar]
- 13.Kheterpal S, Tremper KK, Englesbe MJ, O'Reilly M, Shanks AM, Fetterman DM, Rosenberg AL, Swartz RD. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology. 2007;107:892–902. doi: 10.1097/01.anes.0000290588.29668.38. [DOI] [PubMed] [Google Scholar]
- 14.Levitt JE, Matthay MA. The utility of clinical predictors of acute lung injury: Towards prevention and earlier recognition. Expert Rev Respir Med. 2010;4:785–97. doi: 10.1586/ers.10.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park JS, Kim HK, Kim K, Kim J, Shim YM, Choi YS. Prediction of acute pulmonary complications after resection of lung cancer in patients with preexisting interstitial lung disease. Thorac Cardiovasc Surg. 2011;59:148–52. doi: 10.1055/s-0030-1250644. [DOI] [PubMed] [Google Scholar]
- 16.Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96. doi: 10.1097/ALN.0b013e318216e7f4. [DOI] [PubMed] [Google Scholar]
- 17.Mhyre JM, Ramachandran SK, Kheterpal S, Morris M, Chan PS. Delayed time to defibrillation after intraoperative and periprocedural cardiac arrest. Anesthesiology. 2010;113:782–93. doi: 10.1097/ALN.0b013e3181eaa74f. [DOI] [PubMed] [Google Scholar]
- 18.Austin P, Tu J. Bootstrap methods for developing predictive models. Am Stat. 2004;58:131–7. [Google Scholar]
- 19.Austin P. Absolute risk reductions, relative risks, relative risk reductions, and numbers needed to treat can be obtained from a logistic regression model. J Clin Epidemiol. 2010;63:2–6. doi: 10.1016/j.jclinepi.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Bender R, Kruss O. Methods to calculate relative risks, risk differences, and numbers needed to treat from logistic regression. J Clin Epidemiol. 2010;63:7–8. doi: 10.1016/j.jclinepi.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Fushiki T. Estimation of prediction error by using k-fold cross-validation. Stat Comput. 2009;21:137–46. [Google Scholar]
- 22.Hansen B, Klopfer S. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;1107:1–27. [Google Scholar]
- 23.Ho D, Imai K, King G, Stuart E. Matchit: Nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42 [Google Scholar]
- 24.Breslow NE, Day NE. Statistical methods in cancer research Volume I - The analysis of case-control studies. IARC Sci Publ. 1980:5–338. [PubMed] [Google Scholar]
- 25.Phua J, Badia J, Adhikari NKJ, Friedrich J, Fowler R, Singh J, Scales D, Stather D, Li A, Jones A, Gattas D, Hallett D, Tomlinson G, Stewart T, Ferguson N. Has mortality from acute respiratory distress syndrome decreased over time?: A systematic review. Am J Respir Crit Care Med. 2009;179:220–7. doi: 10.1164/rccm.200805-722OC. [DOI] [PubMed] [Google Scholar]
- 26.Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232:242–53. doi: 10.1097/00000658-200008000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson RG, Arozullah AM, Neumayer L, Henderson WG, Hosokawa P, Khuri SF. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: Results from the patient safety in surgery study. J Am Coll Surg. 2007;204:1188–98. doi: 10.1016/j.jamcollsurg.2007.02.070. [DOI] [PubMed] [Google Scholar]
- 28.Lawrence VA, Cornell JE, Smetana GW. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann Intern Med. 2006;144:596–608. doi: 10.7326/0003-4819-144-8-200604180-00011. [DOI] [PubMed] [Google Scholar]
- 29.Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, Smetana GW, Weiss K, Owens DK, Aronson M, Barry P, Casey DE, Jr, Cross JT, Jr, Sherif KD, Weiss KB. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: A guideline from the American College of Physicians. Ann Intern Med. 2006;144:575–80. doi: 10.7326/0003-4819-144-8-200604180-00008. [DOI] [PubMed] [Google Scholar]
- 30.Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann Intern Med. 2006;144:581–95. doi: 10.7326/0003-4819-144-8-200604180-00009. [DOI] [PubMed] [Google Scholar]
- 31.Jeon K, Yoon JW, Suh GY, Kim J, Kim K, Yang M, Kim H, Kwon OJ, Shim YM. Risk factors for post-pneumonectomy acute lung injury/acute respiratory distress syndrome in primary lung cancer patients. Anaesth Intensive Care. 2009;37:14–9. doi: 10.1177/0310057X0903700110. [DOI] [PubMed] [Google Scholar]
- 32.Lee JW. Beta2 adrenergic agonists in acute lung injury? The heart of the matter. Crit Care. 2009;13:1011. doi: 10.1186/cc8171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matthay MA, Brower RG, Carson S, Douglas IS, Eisner M, Hite D, Holets S, Kallet RH, Liu KD, MacIntyre N, Moss M, Schoenfeld D, Steingrub J, Thompson BT. Randomized, placebo-controlled clinical trial of an aerosolized beta-agonist for treatment of acute lung injury. Am J Respir Crit Care Med. 2011;184:561–8. doi: 10.1164/rccm.201012-2090OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, Gibson M, Umberger R. Methylprednisolone infusion in early severe ARDS: Results of a randomized controlled trial. Chest. 2007;131:954–63. doi: 10.1378/chest.06-2100. [DOI] [PubMed] [Google Scholar]
- 35.Perkins GD, McAuley DF, Thickett DR, Gao F. The beta-agonist lung injury trial (BALIT): A randomized placebo-controlled clinical trial. Am J Respir Crit Care Med. 2006;173:281–7. doi: 10.1164/rccm.200508-1302OC. [DOI] [PubMed] [Google Scholar]
- 36.Smith A, Brown R, Jugg B, Platt J, Mann T, Masey C, Jenner J, Rice P. The effect of steroid treatment with inhaled budesonide or intravenous methylprednisolone on phosgene-induced acute lung injury in a porcine model. Mil Med. 2009;174:1287–94. doi: 10.7205/milmed-d-09-00050. [DOI] [PubMed] [Google Scholar]
- 37.Brochard L, Roudot-Thoraval F, Roupie E, Delclaux C, Chastre J, Fernandez-Mondejar E, Clementi E, Mancebo J, Factor P, Matamis D, Ranieri M, Blanch L, Rodi G, Mentec H, Dreyfuss D, Ferrer M, Brun-Buisson C, Tobin M, Lemaire F. Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The multicenter trail group on tidal volume reduction in ARDS. Am J Respir Crit Care Med. 1998;158:1831–8. doi: 10.1164/ajrccm.158.6.9801044. [DOI] [PubMed] [Google Scholar]
- 38.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 39.Brower RG, Shanholtz CB, Fessler HE, Shade DM, White P, Jr, Wiener CM, Teeter JG, Dodd-o JM, Almog Y, Piantadosi S. Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med. 1999;27:1492–8. doi: 10.1097/00003246-199908000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, Davies AR, Hand LE, Zhou Q, Thabane L, Austin P, Lapinsky S, Baxter A, Russell J, Skrobik Y, Ronco JJ, Stewart TE. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2008;299:637–45. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 41.Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, Gervais C, Baudot J, Bouadma L, Brochard L. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2008;299:646–55. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 42.Stubbs JR. Transfusion-related acute lung injury, an evolving syndrome: The road of discovery, with emphasis on the role of the Mayo Clinic. Transfus Med Rev. 2011;25:66–75. doi: 10.1016/j.tmrv.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 43.Stewart RM, Park PK, Hunt JP, McIntyre RC, Jr, McCarthy J, Zarzabal LA, Michalek JE. Less is more: Improved outcomes in surgical patients with conservative fluid administration and central venous catheter monitoring. J Am Coll Surg. 2009;208:725–35. doi: 10.1016/j.jamcollsurg.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 44.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guerin C, Prat G, Morange S, Roch A. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–16. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 45.Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, Campbell DA., Jr Development and validation of an acute kidney injury risk index for patients undergoing general surgery: Results from a national data set. Anesthesiology. 2009;110:505–15. doi: 10.1097/ALN.0b013e3181979440. [DOI] [PubMed] [Google Scholar]