Abstract
Objective To evaluate the cost effectiveness of acupuncture in the management of chronic headache.
Design Cost effectiveness analysis of a randomised controlled trial.
Setting General practices in England and Wales.
Participants 401 patients with chronic headache, predominantly migraine.
Interventions Patients were randomly allocated to receive up to 12 acupuncture treatments over three months from appropriately trained physiotherapists, or to usual care alone.
Main outcome measure Incremental cost per quality adjusted life year (QALY) gained.
Results Total costs during the one year period of the study were on average higher for the acupuncture group (£403; $768; €598) than for controls (£217) because of the acupuncture practitioners' costs. The mean health gain from acupuncture during the one year of the trial was 0.021 quality adjusted life years (QALYs), leading to a base case estimate of £9180 per QALY gained. This result was robust to sensitivity analysis. Cost per QALY dropped substantially when the analysis incorporated likely QALY differences for the years after the trial.
Conclusions Acupuncture for chronic headache improves health related quality of life at a small additional cost; it is relatively cost effective compared with a number of other interventions provided by the NHS.
Introduction
Migraine and chronic tension headache represent a considerable societal burden in terms of both costs to the health service—for example, for prescription drugs and visits to general practitioners—and also the costs of lost productivity because of reduced effectiveness and time off work.1-4 We have not found recent estimates of the total economic burden of migraine for the United Kingdom. A decade ago the annual costs to the health service were estimated to be between £23m1 and £30m.2 Since these studies were published health service costs have probably increased, given the prescription of more expensive drugs (such as the triptans). The relatively modest observed costs to the health service are often attributed to low consultation rates, poor recognition of disease, and underprescribing.3 A much greater burden is the cost to the economy of lost productivity: in the early 1990s this was estimated to be between £250m2 and £611m4 annually.
Public and scientific interest is increasing in acupuncture as an approach for chronic headache disorders. Although several randomised studies have been conducted,5 few reliable data are available on the cost effectiveness of this intervention. We present a cost effectiveness analysis carried out alongside a randomised trial that seeks to assess the value for money of acupuncture for chronic headache (ISRCTN96537534).
Methods
In the trial 401 patients aged 18-65 who reported an average of at least two headaches per month were recruited from general practices in England and Wales and randomly allocated to receive either up to 12 acupuncture treatments over three months from appropriately trained physiotherapists or usual care alone.6
For the purposes of this evaluation we assume that the acupuncture intervention to be provided in the community by the NHS; hence we measure costs from both an NHS perspective and a societal perspective. We measured effectiveness in terms of the quality adjusted life years (QALYs) gained. For our base case, we have taken a conservative approach by excluding savings in productivity costs and by adopting a time horizon of 12 months, the length of the trial follow up. Given the time horizon, no need arose to discount costs or effects. We measured costs in UK prices (£) for 2002-3. We used the algorithm devised by Brazier et al,7 a single index measure of health related quality of life (HRQoL)—the SF-6D—to calculate for each patient at baseline, three months, and 12 months from patients' responses to the SF-36 at each of these time points.
The patients themselves reported unit costs associated with non-prescription drugs and private healthcare visits. We used the health component of the harmonised index of consumer prices to inflate these costs to 2003 levels.8 Table 1 details other unit costs. We used standard NHS costs for a specific service if these had been published.9 For NHS visits to practitioners of complementary or alternative medicine we used the mean cost of a private visit, as recorded in the trial. We recorded drug prescriptions for a subgroup of patients (n = 71) from the database of their general practitioner.
Table 1.
Unit costs
| Cost component | Unit cost (£) | Source of unit cost | Details* |
|---|---|---|---|
| Acupuncture | |||
| Study acupuncture visit (per hour) | 43.00 | Netten and Curtis 20029 | Clinic visit to community physiotherapist |
| Non-study NHS acupuncture visit | 22.28 | Netten and Curtis 20029; trial data | £0.72×31 minutes |
| Private acupuncture visit | Various | Trial data | Patients reported individual costs |
| NHS visits | |||
| General practitioner | 27.00 | Netten and Curtis 20029 | Cost per clinic consultation |
| Outpatient | 82.00 | Netten and Curtis 20029 | Generic cost per outpatient attendance |
| Counsellor or psychotherapist | 35.75 | Netten and Curtis 20029 | Clinic visit to community based counsellor |
| Physiotherapy | 17.00 | Netten and Curtis 20029 | Clinic visit to community physiotherapist |
| Chiropractor or osteopath | 25.38 | Trial data | Mean cost of a private visit |
| Medical herbalist | 18.17 | Trial data | Mean cost of a private visit |
| Homoeopath | 31.46 | Trial data | Mean cost of a private visit |
| Hypnotherapist | 38.75 | Trial data | Mean cost of a private visit |
| Relaxation therapy | 6.92 | Trial data | Mean cost of a private visit |
| Other costs (base case) | |||
| Private health care visits | Various | Trial data | Patients reported individual costs |
| Over the counter medication | Various | Trial data | Patients reported individual costs |
| Other costs (sensitivity analysis) | |||
| General practitioner cost per hour | 118.00 | Netten and Curtis 20029 | Cost per hour of patient contact |
| Private acupuncture | 28.38 | Trial data | Mean cost of a private visit |
| Prescription drugs | Various | BNF September 200210 | Specified by dosage and pack size. |
| Cost of a day off sick | 88.05 | Office for National Statistics11 | Average earnings per hour×average working hours = £11.7411×7.512 |
All NHS visit costs include salary, on-costs, qualifications, overheads, and capital overheads.
To estimate the cost of the study intervention we took the standard cost (including overheads, capital, and training) for an NHS community physiotherapist9 and multiplied it by the contact time for each individual patient with the physiotherapist trained in acupuncture. We did not include the cost of needles and other consumables as these are negligible compared with staff time.13 We assumed that acupuncture sessions on the NHS, but not by a study acupuncturist, had a duration equal to the mean duration of a study session, 31 minutes.
We used using linear regression (analysis of covariance, ANCOVA) with age, sex, diagnosis (migraine or non-migraine headache), severity of headache at baseline, number of years of headache disorder, site, and baseline SF-6D as covariates to estimate differences between groups for cost and effectiveness on the intention to treat principle. Exact methods for estimating confidence intervals for incremental cost effectiveness ratios are not possible, and we therefore used the net benefit approach to estimate parametric cost effectiveness acceptability curves.14,15 Net benefit analysis usually requires any gain in outcome (for example, QALYs) from an intervention to be valued by using the ceiling ratio, λ, defined as the decision makers' willingness to pay for an additional unit of health outcome, and from this any additional costs are subtracted. A λ equal to £30 000 per QALY is a threshold of cost effectiveness consistent with decisions that have been taken by the National Institute for Clinical Excellence (NICE).16 The cost effectiveness acceptability curves show the probability that the incremental cost effectiveness is below λ, for a range of values of λ. We used SPSS for Windows, version 11.0.0, to perform statistical analysis and Microsoft Excel 2002 SP2 for the calculation of cost effectiveness acceptability curves.
For the base case we conducted no imputation for cases missing HRQoL data; therefore the cost effectiveness analysis sample was those patients who reported SF-36 completely in all three questionnaires and for whom QALYs could therefore be calculated. Data on use of resources and cost were available for a larger sample of cases, and for these variables we report statistics for all responding patients.
Economic evaluation is subject to uncertainty not just because of sample variation but also because of assumptions made and generalisability issues.17 We therefore conducted sensitivity analyses to test the robustness of the results to changes in the base case assumptions. We varied the staff time and grade associated with acupuncture treatment and used different strategies for missing data. We also added productivity costs by multiplying the number of days sick from work or other usual activity, as reported by the study patients, by the average earnings per day in England and Wales11 inflated to 2003 prices.12 The base case analysis does not project beyond the 12 months of observation. It is improbable that the difference in HRQoL observed at 12 months would disappear immediately. In the sensitivity analysis we assumed that, although the study acupuncture intervention was delivered as a one off package and not taken up again in subsequent years, the difference in costs (excluding acupuncture) and effectiveness would gradually subside at the same rate over varying periods of time. We discounted costs at 6% and QALYs at 1.5%, in keeping with the conventions of UK central government.18
Results
Table 2 shows the baseline characteristics for the patients who completed the SF-36 on all three occasions. This group forms our sample for our base case analysis of cost effectiveness. Tables 3 and 4 show resource use, HRQoL, and cost; for these tables we report the results from all responding individuals.
Table 2.
Characteristics of patients for whom QALYs could be calculated (sample size: acupuncture=136, control=119)
| Acupuncture arm | Control arm | |
|---|---|---|
| Mean age in years (SD) | 46.7 (9.7) | 46.0 (11.0) |
| No of female participants (%) | 111 (82%) | 102 (85%) |
| Mean chronicity in years (SD) | 22.1 (14.8) | 21.8 (13.3) |
| Mean headache severity score at baseline (SD)* | 24.1 (14.0) | 27.0 (16.9) |
| No of participants with migraine (%) | 128 (94%) | 113 (95%) |
SD=standard deviation
Patients completed a 6 point Likert scale (0-5) four times a day for four weeks. The score is the weekly average.6
Table 3.
Use of resources and health related quality of life
|
Acupuncture arm
|
Control arm
|
|||
|---|---|---|---|---|
| Resource | Mean (SD) | n | Mean (SD) | n |
| No of acupuncture visits | ||||
| Acupuncture, study | 7.92 (3.76) | 205 | 0.10 (1.03) | 196 |
| Study hours of contact | 4.24 (2.31) | 205 | 0.06 (0.59) | 196 |
| Acupuncture, other NHS | 0.79 (2.31) | 177 | 0.01 (0.08) | 157 |
| Acupuncture, private | 0.34 (1.45) | 177 | 0.01 (0.16) | 157 |
| No of other healthcare visits | ||||
| General practitioner | 1.72 (2.54) | 177 | 2.65 (3.79) | 157 |
| Outpatient | 0.26 (0.93) | 177 | 0.15 (0.65) | 157 |
| Other, NHS | 0.10 (0.64) | 177 | 0.27 (1.57) | 157 |
| Other, private | 2.77 (8.70) | 177 | 2.71 (7.52) | 157 |
| Health related quality of life (SF-6D, score out of 100) | ||||
| Baseline | 69.3 (13.2) | 197 | 70.6 (12.8) | 189 |
| At 3 months | 71.2 (13.6) | 157 | 70.3 (13.1) | 143 |
| At 12 months | 73.9 (14.3) | 150 | 70.7 (13.3) | 133 |
n=sample size; SD=standard deviation.
Table 4.
Costs in £
|
Acupuncture arm
|
Control arm
|
||||
|---|---|---|---|---|---|
| Cost | Mean (SD) | n | Mean (SD) | n | Difference*Mean (95% CI) |
| Acupuncture | |||||
| Acupuncture, study | 201.49 (89.62) | 177 | 3.02 (28.60) | 157 | 198.97 (185.72 to 212.22) |
| Acupuncture, other NHS | 17.54 (51.55) | 177 | 0.14 (1.78) | 157 | 17.76 (9.65 to 25.86) |
| Acupuncture, private | 10.68 (46.27) | 177 | 0.38 (4.79) | 157 | 10.48 (3.08 to 17.89) |
| Other healthcare visits | |||||
| General practitioner | 46.40 (68.48) | 177 | 71.67 (102.34) | 157 | −21.38 (−39.89 to −2.87) |
| Outpatient | 21.68 (76.49) | 177 | 12.10 (53.32) | 157 | 10.24 (−4.15 to 24.63) |
| Other, NHS | 2.59 (18.80) | 177 | 6.63 (39.61) | 157 | −3.48 (−9.59 to 2.63) |
| Other, private | 73.15 (262.04) | 177 | 68.38 (369.97) | 157 | −5.00 (−62.61 to 52.61) |
| Medication | |||||
| Over the counter drugs | 39.07 (60.97) | 177 | 39.42 (50.67) | 157 | 0.00 (−11.87 to 11.87) |
| Complementary or alternative medication | 1.72 (10.00) | 177 | 5.68 (17.82) | 157 | −4.01 (−7.13 to −0.88) |
| Prescription drugs† | 160.98 (365.77) | 36 | 211.51 (484.15) | 35 | −32.04 (−231.27 to 167.18) |
n=sample size; SD=standard deviation; CI=confidence interval.
Adjusted for baseline variables.
Subsample only.
Patients in the acupuncture arm had on average 4.2 hours of contact with a study acupuncturist (table 3). Two patients in the control arm were treated by one of the study acupuncturists, and 18 patients in the acupuncture arm did not attend for acupuncture. Some patients (30 in the acupuncture arm and two in the control arm) visited an acupuncturist for further acupuncture (either NHS or private). Hence the cost of the study acupuncture sessions was augmented by the cost of additional acupuncture sessions (table 4).
We found small but statistically significant reductions in expenditure on visits to general practitioners and complementary or alternative medications (table 4). Differences in other cost components did not reach significance. We obtained costs for prescription drugs from a subsample of 71 patients, and we had hoped to extrapolate results from these patients to the full study sample. However, regression models of these costs had poor properties: linear regression was heteroscedastic, and results differed depending on the various alternative regression methods used. We therefore excluded costs for prescription drug costs from the cost effectiveness analyses. As differences between groups were small (< £50 per patient) and tended to favour the acupuncture group, exclusion of the costs of prescription drugs is a conservative measure that is unlikely to have an important influence on cost effectiveness estimates.
Table 3 reports HRQoL as measured by the SF-6D. We noted an improvement in QALYs over the 12 months in the acupuncture group but not in controls, with the difference between groups reaching significance (P = 0.02). We estimated the mean health gain to be 0.021 QALYs, equivalent to eight quality adjusted days (table 5).
Table 5.
Cost effectiveness. Values are means (standard deviations) unless otherwise indicated
| Acupuncture arm n=136 | Control arm n=119 | Mean difference‡(95% CI) | |
|---|---|---|---|
| NHS cost (£)* | 289.65 (165.86) | 88.65 (130.28) | 205.34 (169.33 to 241.35) |
| Patient cost (£) | 113.75 (258.24) | 128.56 (426.56) | −15.91 (−86.24 to 54.42) |
| Total cost (£)† | 403.40 (356.69) | 217.20 (486.00) | 189.42 (102.24 to 276.61) |
| Quality adjusted life years (QALYs) | 0.727 (0.119) | 0.708 (0.112) | 0.021 (0.001 to 0.040) |
Incremental cost per QALY gained: £9951 (NHS cost); £9180 (total cost).
Excluding prescription drug costs.
Total cost (£)=NHS cost+patient cost.
Adjusted for baseline variables.
We estimated the mean incremental cost of the acupuncture intervention to the NHS to be £205 per patient, excluding the impact on prescription drugs (table 5). This was offset slightly by a small reduction in direct patient costs (over the counter medication and visits to practitioners of complementary and alternative medicine). Overall this equates to an additional cost of £9180 per QALY gained, including patient costs.
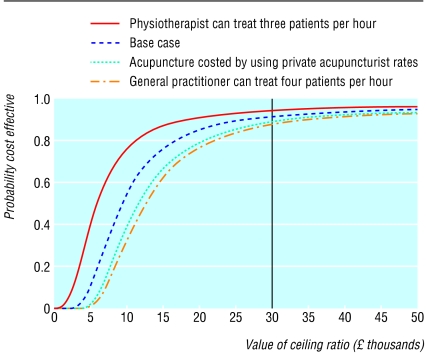
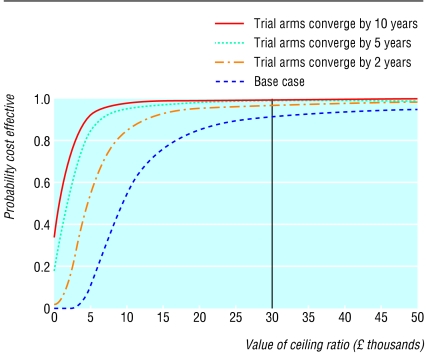
Figures 1 and 2 show the probability that the intervention is cost effective (under our base case assumptions) for a range of cost effectiveness ceilings. At a ceiling of £30 000 per QALY gained (a threshold of cost effectiveness consistent with decisions that have been taken by NICE16). the probability that acupuncture is cost effective is 92%. The figures also show how cost effectiveness changes for several different scenarios (details and further scenarios in table 6). Given the relative value of a general practitioner's time, acupuncture by physiotherapists represents better value for money. Even if a general practitioner can manage to treat four patients in an hour this is still less cost effective than a physiotherapist treating two per hour (the base case scenario).
Fig 1.
Cost effectiveness acceptability curve with sensitivity analysis for acupuncture unit cost
Fig 2.
Cost effectiveness acceptability curve with sensitivity analysis for duration of effect
Table 6.
Sensitivity analyses
| Sample size | Incremental cost (£) | QALYs gained | Incremental cost per QALY gained (£) | |
|---|---|---|---|---|
| Base case (see table 5) | 255 | 189.42 | 0.021 | 9180 |
| Alternative unit costs associated with acupuncture* | ||||
| Using average cost of a private acupuncture session | 255 | 234.72 | 0.021 | 11375 |
| Physiotherapist can treat three patients per hour | 255 | 117.64 | 0.021 | 5701 |
| General practitioner instead of physiotherapist (treating four patients per hour) | 255 | 254.50 | 0.021 | 12333 |
| Strategy for handling of missing values | ||||
| Include only patients completing all cost questionnaires | 220 | 201.52 | 0.018 | 11474 |
| Imputation of QALYs and cost† | 401 | 164.59 | 0.015 | 10836 |
| Inclusion of additional cost component | ||||
| Productivity costs (days off sick) | 255 | 67.34 | 0.021 | 3263 |
| Projection of results into the future | ||||
| Trial arms converge by 2 years | 255 | 183.33 | 0.039 | 4730 |
| Trial arms converge by 5 years | 255 | 166.39 | 0.092 | 1807 |
| Trial arms converge by 10 years | 255 | 142.10 | 0.177 | 801 |
All analyses adjust for baseline variables.
Assumes same health outcome as the base case.
Using linear regression to predict missing values from baseline parameters.
We saw a marked improvement in cost effectiveness associated with the inclusion of productivity costs. However, this represents an underestimate of the cost per QALY since the quality of life measure will in part reflect this improved productivity, especially with respect to increased leisure time. Estimated cost effectiveness was also improved by the projection of effects beyond one year and the assumption that acupuncturists could improve their throughput by dealing with patients simultaneously. Cost effectiveness was not markedly different when we used private acupuncture costs. Similarly, imputing values for cases with missing data did not greatly influence the results, although the explanatory power of the imputation regressions was weak. Under none of the scenarios did the central estimate of cost indicate overall cost savings.
Discussion
Acupuncture lead to increases in both QALYs and health service costs. We estimated the incremental cost effectiveness to be £9180 per QALY gained. The estimated improvement in quality of life correlates with the observed reductions in headache severity and frequency.
We consider that the base case is likely to be conservative as it excludes cost savings associated with prescription drugs and productivity gains. More importantly, our base case analysis considers only the 12 months of the trial. The effects of acupuncture appear to be persistent as differences between groups were slightly larger at one year than immediately post-treatment. If we include likely QALY differences for subsequent years, then acupuncture appears even better value for money.
Acupuncture by medical general practitioners (as well as by specialist physiotherapists) appears to be reasonably cost effective compared with usual care, however, given the relative value of a general practitioner's time, acupuncture by physiotherapists represents better value for money, unless general practitioners can achieve substantially better outcomes and or much shorter contact times.
The probability that the programme is cost effective at a ceiling of £30 000 was estimated to be 92% for the base case. This does not take into account the uncertainty owing to imputing missing values, which means that this probability is a slight overestimate. When only complete responders are included in the analysis the probability falls to 84%, but this estimate is biased conservatively. This study, like most economic evaluations,19 was not powered to detect a difference in cost effectiveness and therefore the lack of statistical significance at the 5% level should not be interpreted as evidence of non-cost effectiveness—few if any economic evaluations attain such levels of significance.
What is already known on this topic
Acupuncture is widely used for chronic pain
A number of small trials, and recently a larger more rigorous trial, indicate that acupuncture is of benefit for chronic headache disorders
No rigorous cost effectiveness assessments of acupuncture have been previously undertaken
What this study adds
Acupuncture improves health related quality of life (HRQoL), but increases costs to the health service
Cost effectiveness was estimated to be £9180 per QALY gained, or less if analysis incorporated likely QALY differences for the years after the trial
If decision makers are willing to pay up to £30 000 to gain one QALY then acupuncture in the treatment of chronic headache is highly likely to be cost effective
To our knowledge, this is the first rigorous economic evaluation of acupuncture. Prior economic studies on acupuncture for pain have typically been conducted by acupuncture advocates and have used questionable methods. For example, studies have claimed cost savings on the basis of hypothetical interventions that would have been necessary had acupuncture not been administered.13,20 Other studies have used before-after comparisons21 or non-randomised controls.22 Cost savings have been shown by retrospective studies of acupuncture for other conditions, but similar methodological problems have been described.23
Our study, with a relatively large sample size, a randomised comparison arm, and prospective evaluation of costs, has not found such overall cost savings for headache patients: we can be fairly certain from our results that acupuncture adds to health service costs for these patients. Therefore the pertinent question is whether this additional cost is justified by the associated health gains. Even when we use our conservative base case estimate of £9180 per QALY gained, acupuncture for migraine seems to be better value for money than several interventions that have been recommended by NICE.16 To our knowledge, a cost per QALY analysis has only been performed for one other antimigraine intervention—sumatriptan compared with oral caffeine and ergotamine—which had a cost per QALY of $C29 366 (£16 000).24 Acupuncture therefore compares favourably.
Clinicians, commissioners, and patients should consider acupuncture for migraine and chronic headache as it seems to reduce the severity of headache and improves HRQoL at a small additional cost. It is an intervention that is relatively cost effective compared with a number of interventions provided by the NHS.
Contributors: DW undertook the economic analyses and is the study guarantor; AJV conceived and designed the randomised trial and advised on statistical aspects of the economic analyses; RG advised on the analyses; RM contributed to design of resource outcome assessment.
Funding: NHS R&D National Coordinating Centre for Health Technology Assessment (NCCHTA) Grant: 96/40/15.
Competing interests: None declared.
Ethical approval was received from South West Multi-centre Research Ethics Committee and appropriate local ethics committees.
References
- 1.Blau JN, Drummond MF. Migraine. London: Office of Health Economics, 1991.
- 2.Bosanquet N, Zammit-Lucia J. Migraine: prevention or cure? Br J Med Econ 1992;2: 81-91. [Google Scholar]
- 3.Solomon GD, Price KL. Burden of migraine: a review of its socioeconomic impact, PharmacoEconomics 1997;11(suppl 1): 1-10. [DOI] [PubMed] [Google Scholar]
- 4.Cull RE, Wells NE, Moiechevich ML. The economic cost of migraine. Br J Med Econ 1992;2: 81-91. [Google Scholar]
- 5.Melchart D, Linde K, Fischer P, Berman B, White A, Vickers A, et al. Acupuncture for idiopathic headacnes. Cochrane Database Syst Rev 2001;(1): CD001218. [DOI] [PubMed]
- 6.Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith C, Ellis N, et al. Acupuncture for migraine and chronic tension headache in primary care: a large, pragmatic, randomised trial. BMJ 2004;328: 000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21(2): 271-92. [DOI] [PubMed] [Google Scholar]
- 8.Office for National Statistics. First release: consumer prices indices May 2003. London: ONS, 2003.
- 9.Netten A, Curtis L. Unit costs of health and social care. Canterbury: Personal Social Services Research Unit, University of Kent and Canterbury, 2002.
- 10.Joint Formulary Committee. British National Formulary. 44 ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2002.
- 11.Office for National Statistics. Average earnings index 1963-2003 London: ONS, 2003. www.statistics.gov.uk/statbase (accessed 14 May 2003).
- 12.Office for National Statistics. Labour market statistics May 2003. London: ONS, 2003.
- 13.Downey P. Acupuncture in the normal general practice consultation: an assessment of clinical and cost-effectiveness. Acupuncture Med 1995;13: 45-7. [Google Scholar]
- 14.Van Hout BA, Al MJ, Gordon GS, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994;3: 309-19. [DOI] [PubMed] [Google Scholar]
- 15.Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18(2 suppl): S68-80. [DOI] [PubMed] [Google Scholar]
- 16.Raftery J. NICE: faster access to modern treatments? Analysis of guidance on health technologies. BMJ 2001;323: 1300-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briggs AH, Gray AM. Handling uncertainty in economic evaluations of healthcare interventions. BMJ 1999;319: 635-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.HM Treasury. Appraisal and evaluation in central government. London: Stationery Office, 1997.
- 19.Willan AR. Analysis, sample size, and power for estimating incremental net health benefit from clinical trial data. Control Clin Trials. 2001;22: 228-37. [DOI] [PubMed] [Google Scholar]
- 20.Lindall S. Is acupuncture for pain relief cost-effective? Acupuncture Med 1999;17: 97-100. [Google Scholar]
- 21.Myers CP. Acupuncture in general practice: effect on drug expenditure. Acupuncture Med 1991;9: 71-2. [Google Scholar]
- 22.Ballegaard M D, Johannessen A, Karpatschof B, Nyboe J. Addition of acupuncture and self-care education in the treatment of patients with severe angina pectoris may be cost beneficial: an open, prospective study. J Altern Complement Med 1999;5: 405-13. [DOI] [PubMed] [Google Scholar]
- 23.White AR, Ernst E Economic analysis of complementary medicine: a systematic review. Complement Ther Med 2000. 8; 111-8. [DOI] [PubMed] [Google Scholar]
- 24.Evans KW, Boan JA, Evans JL, Shuaib A. Economic evaluation of oral sumatriptan compared with oral caffeine/ergotamine for migraine. Pharmacoeconomics 1997;12: 565-77. [DOI] [PubMed] [Google Scholar]