Abstract
OBJECTIVES
Nonmedical prescription opiate use (NPOU) and nonmedical prescription sedative use (NPSU) are serious public health concerns. The objectives of this study were to determine the prevalence and emergency department (ED) visit characteristics and other correlates associated with past-year NPOU and NPSU among adolescents and young adults using the ED.
METHODS:
Participants aged 14 to 20 presenting to the ED at the University of Michigan Medical Center between September 2010 and September 2011 were systematically recruited. A computerized self-report screening survey with validated items measuring past-year NPOU, NPSU, substance use, and violence was delivered to participants, and a retrospective chart review was performed.
RESULTS:
Of the 2135 participants (86.0% response rate), 222 (10.4%) reported either NPOU or NPSU. Among the 185 (8.7%) participants that reported NPOU, 14.6% had a current home prescription for an opioid and among the 115 (5.4%) with NPSU, 12.3% had a current home prescription for a sedative. After controlling for demographics (age, gender, race, public assistance), correlates of NPOU or NPSU included other substance use, and drinking and driving or riding with a drinking driver. Additional correlates of NPOU included receiving an intravenous opioid in the ED and for NPSU, dating violence, presenting to the ED for a noninjury complaint, and previous ED visit in the past year.
CONCLUSIONS:
Nearly 1 in 10 young people who use the ED for care report NPOU or NPSU, and only 12.3% and 14.6% report having current home prescriptions for sedatives and opioids. The ED represents a key location for screening and intervention efforts.
Keywords: prescription drug misuse, emergency medicine, adolescent medicine
What’s Known on This Subject:
Unintentional overdose and emergency department visits secondary to nonmedical use of prescription drugs are on the rise with peak age of onset in midadolescence for these risk behaviors. Also, risk behaviors, such as substance use and violence, tend to cluster.
What This Study Adds:
Approximately 1 in 10 adolescents or young adults using the emergency department endorse nonmedical prescription opioid or sedative use in the past year. Rates of current opioid or sedative prescriptions are low among this group.
The Centers for Disease Control and Prevention describe abuse of prescription drugs as an epidemic, with ∼1 million emergency department (ED) visits related to prescription drug overdose, abuse, and misuse in 2008.1,2 However, for every 1 prescription opioid overdose, there are 35 ED visits and >400 reports of nonmedical use (use without a prescription or more than was prescribed or using to get high).3 Among adults, nonmedical use of prescription opioids4,5 and prescribed doses of >100 mg of morphine equivalents per day6–8 are associated with unintentional overdose. Currently, there are no studies that examine the prevalence of nonmedical prescription opioid use (NPOU) and nonmedical prescription sedative use (NPSU) among the ED population.
The peak age of onset for initiating NPOU is 16 years,9 and a sharp increase occurs in the number of ED visits involving NPOU and NPSU in late adolescence.1 Also, in 2011, of the 3.1 million persons aged ≥12 years who used drugs for the first time, approximately 1 in 5 initiated nonmedical use of prescription drugs.10 Among school samples, 80% of adolescents who reported NPOU previously obtained a prescription for opioids from a physician.11 Diversion is a common source of prescription drugs used for nonmedical reasons, and although rates of NPOU and NPSU are rising, prescribing rates for opioids and sedatives nearly doubled from 1994 to 2007.12 Among adolescents, risk behaviors tend to cluster,13 and in school-based samples, adolescents who report nonmedical prescription drug use have higher odds of alcohol misuse, marijuana use, and other drug use.11
Rates of nonmedical prescription drug use among adolescents in health care settings remain unknown. Pain is a common complaint among ED patients, and many patients leave the ED with an opioid prescription.14 Recently, the American College of Emergency Physicians published a clinical policy focused on critical issues in opioid prescribing for adult patients in the ED, but because of a lack of systematic research, did not comment on evidence-based screening or intervention strategies for NPOU.15 Given that emergency medicine providers are a source of prescription opioids and sedatives, a more thorough understanding of patient and ED visit characteristics associated with NPOU and NPSU is needed to inform screening and intervention initiatives.
The primary aim of this study was to determine the past-year prevalence of NPOU and NPSU among a systematic sample of adolescents and young adults using the ED. We examined correlates associated with past-year NPOU and NPSU to inform ED-based clinical practice.
Methods
Study Design
This study reports a secondary analysis of cross-sectional data collected during recruitment for a randomized controlled trial (UConnect: Optimizing Brief Alcohol Intervention for Underage Drinkers in the ER; http://clinicaltrials.gov/show/NCT01051141).
Setting
A large academic ED (the University of Michigan Emergency Department and Children’s Emergency Services) located in Ann Arbor, Michigan, served as the study site. Study procedures were approved by the institutional review board at the University of Michigan, and a Certificate of Confidentiality was obtained from the National Institutes of Health.
Selection of Participants
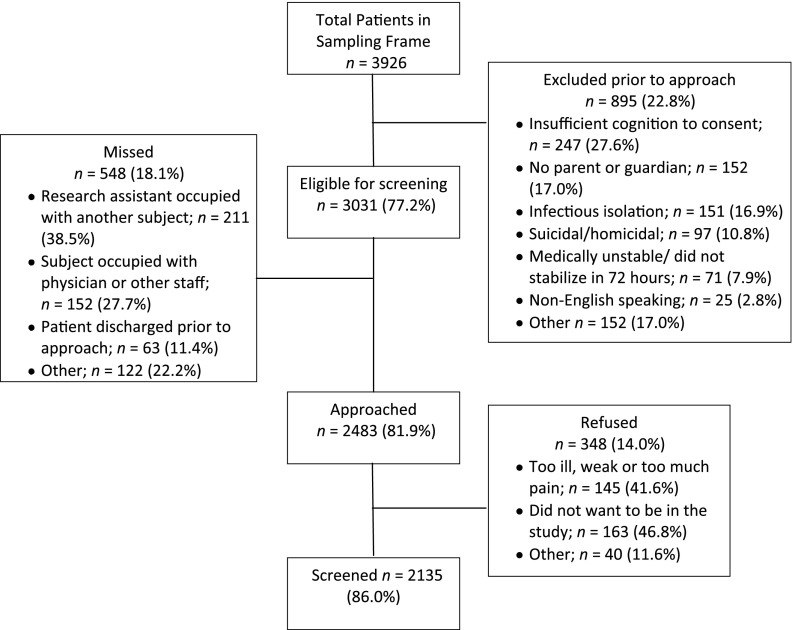
Patients aged 14 to 20 who presented to the ED for any reason (ie, fever, injury) were eligible for screening (see Fig 1 for exclusions and further details). Recruitment was conducted by research assistants and occurred systematically and sequentially during randomly selected day shifts (8:00 am–2:00 pm), overnight shifts (midnight–8:00 am) and all afternoon/evening shifts (2:00 pm–12:00 am), 7 days a week (excluding major holidays) between September 2010 and September 2011. Patients were identified through an Electronic Medical Record (EMR); those requiring emergent intervention (eg, intubation) in the ED were surveyed as an inpatient within 72 hours of admission if they stabilized. After obtaining informed consent (or parental consent and participant assent for patients <18 years) participants completed a self-administered computerized screening questionnaire lasting ∼15 minutes.
FIGURE 1.
Recruitment flow sheet.
Methods of Measurement
All questions were piloted to ensure comprehension, and all measures have been previously validated in adolescent and young adult samples.
Outcome Measures
Past-year nonmedical prescription drug use was assessed by using 2 yes/no questions from the National Institute on Drug Abuse Alcohol, Smoking, and Substance Involvement Screening Test.16 NPOU was measured with “Have you used any of the following substances (prescription opioids, such as fentanyl, oxycodone, hydrocodone, methadone, buprenorphine, suboxone) to get high, or taken them when they were prescribed to someone else, or taken more than what was prescribed to you?” NPSU was assessed with “Have you used any of the following substances (Valium, Serepax, Ativan, Xanax, Librium, Rohypnol, GHB, and so forth) to get high, or taken them when they were prescribed to someone else, or taken more than what was prescribed to you?”
Demographics
Demographic items (age, gender, race, school status, living situation) were selected from the National Study of Adolescent Health.17 Academic performance18 was collapsed into 2 categories encompassing failing grades (mostly Ds and Fs)/dropped out of school versus all others. Participants were asked “Do your parents, or the most important person raising you receive public assistance” to provide information on socioeconomic status.
Risk Factors
Dating violence over the past year was assessed by using a collapsed version of the Conflict in Adolescent Dating Relationships Inventory,19 asking about violence with “your dating partner (girlfriend/boyfriend, fiancée) or husband/wife.” Four questions regarding victimization by a partner (α = 0.87) and 4 parallel questions regarding aggression from a partner (α = 0.87) were collapsed to create a dichotomous variable reflecting any dating violence involvement (yes/no).
Past-year alcohol misuse was assessed with the 3-item Alcohol Use Disorders Identification Test, Consumption (α = 0.89) using a cutoff of 3 indicating alcohol misuse for participants <18 and 4 or more for participants aged ≥18 years.20
Past-year driving after drinking was measured with 5 items (α = 0.91) from the Young Adult Driving Questionnaire.21 One item from the Youth Risk Behavior Survey22 assessed past-year riding in a car with a driver who had been drinking. Responses on these 6 items were dichotomized, reflecting any driving after drinking/riding with a drinking driver versus no report of these behaviors.
Past-year marijuana use (yes/no) was measured with 1 question from the National Institute on Drug Abuse Alcohol, Smoking, and Substance Involvement Screening Test.16 Participants were also asked “In the past 12 months have you used nonprescription cough or cold medicine (ie, robotripping, dextromethorphan [DXM], Delsum, Coricidin, and so forth) to get high” to assess nonmedical use of nonprescription cough or cold medicines.16,23
Chart Review
Research staff were trained on the classification of external causes of injuries, International Classification of Diseases, Ninth Revision, Clinical Modification24 and retrospectively abstracted the reason for the ED visit from the EMR and coded it as medical illness (eg, asthma, fever) or injury (ICD-9-CM E800–E999). The type and route of opioid medication provided during the index ED visit was recorded and separated into oral or intravenous. If participants received an opioid prescription on discharge, they were coded as “yes” for “received opioid prescription for home.” Any past-year ED visit before the index visit was also abstracted from the EMR.
The EMR was reviewed to determine each participant’s medication list at the time of the index ED visit. Participants reporting diazepam, alprazolam, triazolam, estazolam, clonazepam, chlordiazepoxide, tomazepam, zolpidem, zaleplon, or eszopiclone to a medical provider as a current medication were coded as having an active outpatient sedative prescription. Participants reporting codeine, hydrocodone, oxycodone, oxycontin, propoxyphene, hydromorphone, morphine, methadone, meperidine, or butorphanol as a current medication were coded as having an active outpatient opioid prescription.
To ensure reliability of all chart review data, research staff were blind to the outcome measure and abstracted data onto a standardized form. Discrepancies were assessed by 2 reviewers and a final decision was made by an emergency medicine physician (Dr Whiteside or Dr Cunningham). Audits were performed regularly on chart reviews and 20% of randomly selected charts were double-entered to ensure reliability. κ values for chart review items ranged from 0.82 to 1.00.25
Analysis
Data were analyzed by using SAS Version 9.2 (SAS Institute, Inc, Cary, NC). Descriptive statistics of nonmedical prescription drug use, demographics, risk factors, and ED visit characteristics were calculated for all participants. To evaluate bivariate associations with dependent measures, χ2 tests and ANOVAs were used to determine differences between NPOU and those without NPOU and NPSU and those without NPSU. To understand the relationship between multiple risk factors for drug use and NPOU and NPSU, 2 separate multivariate logistic regression models were constructed based on theory and previous research. All demographic variables (age, gender, race, public assistance) were controlled for in the final analyses predicting NPOU and NPSU. Also, risk factors and chart review variables that were significant in the bivariate analysis for each model depicting NPOU or NPSU were included in the final logistic regression for that respective outcome. However, for the model predicting NPOU, the variable “received opioids on discharge” was not included, given the association between this variable and the main outcome. Diagnostics, including a correlation matrix and variance inflation factors, were calculated for all variables retained in the final regression models and there was no evidence of multicollinearity.
Results
Of the 3926 patients presenting to the ED during the sampling frame, 3031 (77.2%) were potentially eligible and 2483 (81.9%) were approached for screening (Fig 1). χ2 analyses revealed that that male patients were more likely to be missed than female patients (χ2 = 16.31, P < .001) and 14- to 17-year-olds were more likely to be missed than 18- to 20-year-olds (χ2 = 9.14, P < .01). Among approached participants, 348 (14.0%) refused and 2195 were screened. There was no difference in gender or age between those who refused and those who completed the survey. The average age of the sample was 17.5 years (SD 2.0), 1206 (56.3%) were female, 1530 (71.7%) identified as white, and 627 (29%) received public assistance.
A total of 222 (10.4%) patients reported NPOU or NPSU. Of this subsample, 185 participants had NPOU, 115 participants had NPSU, and 78 engaged in both NPOU and NPSU. Of those with NPOU, only 27 had a current home prescription for an opioid with 2 receiving a prescription for opioids on discharge, and 12 receiving an intravenous opioid and 6 receiving an oral opioid during their ED visit. Among the 115 participants with NPSU, only 14 had a current home prescription for a sedative.
Compared with those without NPOU, those reporting NPOU were older (18.0 years [SD = 2.0] vs 17.5 years [SD = 1.8], P < .001), more likely to receive public assistance (42.2% vs 28.2%, P < .001) and more likely to have poor academic performance (17.4% vs 5.1%, P < .001). There were no statistically significant differences in gender or race between these 2 groups (Table 1). Those with NPSU were more likely to identify as white (80.0% vs 71.2%, P < .05), receive public assistance (50.4% vs 28.2%, P < .001), and have poor academic performance (18.4% vs 5.4%, P < .001) compared with those without NPSU, but there were no differences in gender or age among these 2 groups (Table 2). Participants who reported either NPOU or NPSU had increased odds of all measured risk factors (P < .001) and were less likely to be in the ED for injury (P < .01) and more likely to have a previous ED visit in the past 12 months (P < .01) compared with those without NPOU or NPSU. There were no differences among those with NPSU compared with those without NPSU with regard to opioid administration in the ED. Compared with those without NPOU, those with NPOU were more likely to have received an intravenous opioid (27.6% vs 14.1%, P < .0001) or an oral opioid (10.8% vs 6.5%, P < .05) during their ED visit and more likely to receive a prescription opioid on discharge (10.8% vs 6.5%, P < .05).
TABLE 1.
Demographics and Risk Factors for Past-Year NPOU
| Past-Year NPOU, n = 185, 8.7% | No Past-Year NPOU, n = 1950, 91.3% | |
|---|---|---|
| Demographics | ||
| Age, mean (SD) | 18.0 (2.0) | 17.5 (1.8)** |
| Female, n (%) | 101 (54.6) | 1102 (56.5) |
| White, n (%) | 134 (72.4) | 1396 (71.6) |
| African American, n (%) | 21 (11.4) | 316 (16.2) |
| Other, n (%) | 30 (16.2) | 238 (12.2) |
| Public assistance (parent or self), n (%) | 78 (42.2) | 549 (28.2)*** |
| Failing grades, or dropped out of school, n (%) | 32 (17.4) | 98 (5.1)*** |
| Risk factors, n (%) | ||
| Dating violence | 63 (34.1) | 281 (14.4)*** |
| Drinking and driving or riding with a drinking driver | 120 (64.9) | 516 (26.5) *** |
| Alcohol misuse | 108 (58.4) | 485 (24.9)*** |
| Marijuana use | 122 (66.0) | 584 (30.0)*** |
| Nonprescription cough or cold medicine misuse | 74 (40.0) | 249 (12.8)*** |
| Visit characteristics and ED use, n (%) | ||
| In ED for injury | 49 (26.6) | 699 (35.9)** |
| Discharged from ED | 149 (80.5) | 1642 (84.2) |
| Previous ED visit in past 12 mo | 65 (35.1) | 484 (24.82)** |
| Received oral opioid in the ED | 20 (10.8) | 126 (6.5)* |
| Received intravenous opioid in the ED | 51 (27.6) | 275 (14.1)*** |
| Given prescription for narcotic on discharge | 20 (10.8) | 126 (6.5)* |
P < .05; **P < .0.01; ***P < .001.
TABLE 2.
Demographics and Risk Factors for Past-Year NPSU
| Past-Year NPSU, n = 115, 5.4% | No Past-Year NPSU, n = 2019, 94.6% | |
|---|---|---|
| Demographics | ||
| Age, mean (SD) , n (%) | 17.9 (1.6) | 17.5 (2.0) |
| Female, n (%) | 66 (57.4) | 1137 (56.3) |
| White, n (%) | 92 (80.0) | 1438 (71.2)* |
| African American, n (%) | 8 (7.0) | 329 (16.3)* |
| Other, n (%) | 15 (13.0) | 253 (12.5)* |
| Public assistance (parent or self) , n (%) | 58 (50.4) | 569 (28.2)*** |
| Failing grades, or dropped out of school, n (%) | 21 (18.4) | 109 (5.4)*** |
| Risk factors, n (%) | ||
| Dating violence | 51 (44.4) | 293 (14.5)*** |
| Drinking and driving or riding with a drinking driver | 80 (69.6) | 556 (27.5) *** |
| Alcohol misuse | 74 (64.4) | 519 (25.7)*** |
| Marijuana use | 92 (80.0) | 614 (30.4)*** |
| Nonprescription cough or cold medicine misuse | 50 (43.5) | 273 (13.5)*** |
| Visit characteristics and ED utilization, n (%) | ||
| In ED for injury | 27 (23.4) | 721 (35.8)** |
| Discharged from ED | 94 (81.7) | 1697 (84.0) |
| Previous ED visit in past 12 mo | 46 (40.0) | 503 (24.9)*** |
| Received oral opioid in the ED | 11 (9.6) | 135 (6.7) |
| Received intravenous opioid in the ED | 23 (20.0) | 303 (15.0) |
| Given prescription for narcotic on discharge | 11 (9.6) | 135 (6.7) |
P < .05; **P < .0.01; ***P < .001.
Table 3 depicts correlates of NPOU in the multivariate model. Significant correlates included receipt of public assistance, poor academic performance, alcohol misuse, drinking and driving or riding with a drinking driver, marijuana use, nonprescription cough or cold medicine misuse, and receipt of intravenous opioid during the ED visit. Having a past-year ED visit and reason for the current ED visit (medical/injury) were not significantly associated with NPOU in this model.
TABLE 3.
Logistic Regression Predicting Past-Year NPOU
| NPOU OR (95% CI) | |
|---|---|
| Demographics | |
| Age | 0.99 (0.90–1.09) |
| Female | 0.90 (0.63–1.28) |
| White vs African American | 1.18 (0.73–1.92) |
| White vs other race | 0.73 (0.43–1.24) |
| Public assistance (parent or self) | 1.60 (1.11–2.32) |
| Failing grades or dropped out of school | 2.26 (1.42–3.61) |
| Risk factors (past year) | |
| Dating violence | 1.47 (1.00–2.17) |
| Alcohol misuse | 2.36 (1.59–3.50) |
| Drinking and driving or riding with a drinking driver | 2.40 (1.65–3.48) |
| Marijuana use | 1.92 (1.31–2.83) |
| Nonprescription cough or cold medicine misuse | 3.50 (2.43–5.02) |
| Chart review from index ED visit | |
| ED presentation for injury | 0.73 (0.50–1.07) |
| Previous ED visit in past 12 mo | 1.35 (0.94–1.94) |
| Received intravenous opioid in the ED | 2.44 (1.64–3.63) |
CI, confidence interval; OR, odds ratio.
In the multivariate model (Table 4), significant correlates of NPSU included receipt of public assistance, dating violence, alcohol misuse, drinking and driving/riding with a drinking driver, marijuana use, nonprescription cough or cold medicine misuse, and having a previous ED visit in the past year. Those with a current injury-related visit were less likely to endorse NPSU compared with those presenting for a medical complaint.
TABLE 4.
Logistic Regression Predicting Past-Year NPSU
| NPSU OR (95% CI) | |
|---|---|
| Demographics | |
| Age | 0.91 (0.81–1.03) |
| Female | 1.10 (0.70–1.71) |
| White vs African American | 0.66 (0.34–1.29) |
| White vs other race | 0.29 (0.13–0.64) |
| Public assistance (parent or self) | 2.32 (1.47–3.65) |
| Failing grades or dropped out of school | 1.67 (0.95–2.92) |
| Risk factors (past year) | |
| Dating violence | 2.19 (1.39–3.45) |
| Alcohol misuse | 2.38 (1.46–3.89) |
| Drinking and driving or riding with a drinking driver | 2.11 (1.31–3.42) |
| Marijuana use | 3.99 (2.35–6.82) |
| Nonprescription cough or cold medicine misuse | 3.58 (2.29–5.59) |
| Chart review from index ED visit | |
| ED presentation for injury | 0.56 (0.34–0.92) |
| Previous ED visit in past 12 mo | 1.63 (1.04–2.53) |
CI, confidence interval; OR, odds ratio.
Discussion
Approximately 1 in 10 ED patients (10.4%) aged 14 to 20, reported nonmedical use of prescription opioids or sedatives over the past year, with 8.7% reporting NPOU and 5.4% reporting NPSU, which is slightly higher than a school-based sample with annual prevalence rates of 7.9% for NPOU and 4.5% for NPSU in 2012.26 More than 80% of patients in this analysis were discharged from the ED, including those with past-year NPOU and NPSU and more than one-third of patients with NPOU or NPSU had been seen in the ED previously in the past year compared with only 25% of patients without NPOU or NPSU. Also, those with a previous ED visit in the past year had increased odds of NPSU after controlling for other risk factors. These high rates of at least 1 previous ED visit and discharge from the ED highlight the need for NPOU and NPSU screening and intervention within the ED.
Approximately 1 in 7 participants with NPOU received an opioid prescription at discharge compared with 1 in 15 participants without NPOU. In addition to developing screening and intervention protocols, information-sharing technology could assist providers in improving and monitoring safe prescribing practices.27 Statewide prescription monitoring programs (PMPs)28 are now widely available to providers as a tool to potentially limit prescription drug misuse and diversion, and states that have integrated the PMP with a hospital EMR note ease of use and clinical relevance.29 In North Carolina, a community-based program that includes safe prescribing practices and use of the statewide PMP has decreased mortality from overdose.30 Additionally, patients who require intravenous opioids are at high risk for NPOU and providers should be careful to balance treating pain complaints with this increased risk for NPOU.
Among adolescents, risk behaviors, such as drug use, alcohol misuse, and violence tend to co-occur.13 Fatal overdose from prescription opioids is associated with previous history of illicit drug use and alcohol use4,5 among adults, and simultaneous use of multiple substances is a known risk factor for unintentional overdose death.4 This analysis highlights that alcohol misuse, marijuana use, and nonmedical cough and cold medicine use were independent correlates for both NPOU and NPSU. Abuse of over-the-counter cough and cold medications, such as DXM, has been increasing with a peak age of abuse of 15 to 16 years.31 Although it is known that alcohol and illicit drug use is associated with nonmedical use of DXM,31 this is the first analysis to highlight nonmedical DXM use as an independent risk factor for both NMOU and NPSU. Given that over-the-counter DXM is easier to obtain than prescription sedatives or opioids, further research should explore the temporal relationship between the nonmedical use of these substances.
NPOU and NPSU were both also associated with drinking and driving or riding in a car with a drinking driver. This relationship has been previously demonstrated in adult samples, but not in adolescent samples.32 Alcohol use at a young age is a risk factor for both drinking and driving and nonmedical use of prescription drugs.33,34 Given these associations, adolescent alcohol interventions should consider addressing drug use in general and nonmedical use of prescription drugs in particular.
Adolescents involved in dating violence had more than 2-times increased odds of NPSU. Although there is a known association between adolescent dating violence and alcohol and marijuana use,35 this is the first analysis to demonstrate a correlation between dating violence and NPSU among ED patients. Of note, the causal relationship between the violence and NPSU was beyond the scope of this analysis and requires further study. However, dating violence was not related to NPOU in the multivariate model, which could be explained by differences in reasons for NPOU versus NPSU. Reasons for nonmedical use of prescription drugs are likely multifactorial36,37; those with NPOU may be trying to relieve pain or “get high,” whereas those with NPSU may be trying to relieve stress or anxiety. Different motivations for use may relate to this different risk factor profile.
Although this analysis provides novel information regarding NMOU and NPSU among young people seeking care in the ED, there are some inherent limitations. The cross-sectional nature of the data does not allow for causal conclusions. The definition of NPOU and NPSU for this study was broad, not allowing for targeted study on specific reasons for nonmedical use of these substances or differentiation of subpopulations (ie, medical misusers with a prescription; nonmedical users without a prescription) and thus is an area of future inquiry. This study includes data from participants recruited at a single ED and thus may not be generalizable to settings containing different sociodemographic groups. Additionally, data from the chart review were limited to the University of Michigan system and do not capture use of nonaffiliated EDs. Although self-reported data could be viewed as a limitation, several reviews support the reliability and validity of self-report of risk behaviors among this population when privacy is assured and assessments are self-administered and computerized.38–42
Conclusions
Approximately 10% of 14- to 20-year-old ED patients report past-year NPOU or NPSU. Additionally, young people using the ED had increased odds of NPOU if they received an intravenous opioid during their visit, or engaged in past-year substance abuse, whereas those with NPSU were more likely to have a history of dating violence and substance use, as increased ED use over the past year compared with those without NPOU or NPSU, respectively. These results suggest the ED is an ideal location for both screening and intervention given this risk factor profile and ED visit characteristics associated with both NPOU and NPSU. Future directions include developing screening and intervention protocols to assist in identifying ED patients at risk for nonmedical use of prescription drugs regardless of their reason for ED presentation.
Acknowledgments
The authors acknowledge Linping Duan for statistical support, Carrie Smolenski for project management, and the UConnect study staff for project assistance. Also, a special thanks is owed to the patients and staff of the University of Michigan Department of Emergency Medicine and Children’s Emergency Services.
Glossary
- DXM
dextromethorphan
- ED
emergency department
- EMR
electronic medical record
- PMP
prescription monitoring program
- NPOU
nonmedical prescription opiate use
- NPSU
nonmedical prescription sedative use
Footnotes
Drs Whiteside and Cunningham assisted with conceptualization and study design, helped to design the chart review abstraction tool, were involved with data interpretation, assisted with drafting the initial manuscript, and contributed to revisions for important intellectual content; Drs Walton and Bohnert assisted with conceptualization and study design, were involved with data interpretation, and contributed substantially to revisions for important intellectual content; Drs Blow and Ehrlich assisted with study design, were involved with data interpretation, and contributed substantially to revisions for important intellectual content; Dr Bonar assisted with data interpretation, assisted with drafting the initial manuscript, and contributed substantially to revisions for important intellectual content; and all authors had a chance to approve the final manuscript to be published.
FINANCIAL DISCLOSURE: Dr Walton is the principal investigator on a randomized controlled trial funded by the National Institute of Alcohol Abuse and Alcoholism, which provided data for this analysis; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by National Institute of Alcohol Abuse and Alcoholism grant 5 R01 AA018122 04 (PI: Dr Walton). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention (CDC) . Emergency department visits involving nonmedical use of selected prescription drugs—United States, 2004-2008. MMWR Morb Mortal Wkly Rep. 2010;59(23):705–709 [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) . Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492 [PubMed] [Google Scholar]
- 3.Paulozzi L, Baldwin G, Centers for Disease Control and Prevention (CDC) . CDC grand rounds: prescription drug overdoses—a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61(1):10–13 [PubMed] [Google Scholar]
- 4.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620 [DOI] [PubMed] [Google Scholar]
- 5.Johnson EM, Lanier WA, Merrill RM, et al. Unintentional prescription opioid-related overdose deaths: description of decedents by next of kin or best contact, Utah, 2008-2009. J Gen Intern Med. 2013;28(4):522–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321 [DOI] [PubMed] [Google Scholar]
- 7.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–691 [DOI] [PubMed] [Google Scholar]
- 8.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meier EA, Troost JP, Anthony JC. Extramedical use of prescription pain relievers by youth aged 12 to 21 years in the United States: national estimates by age and by year. Arch Pediatr Adolesc Med. 2012;166(9):803–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012 [Google Scholar]
- 11.McCabe SE, West BT, Teter CJ, Boyd CJ. Medical and nonmedical use of prescription opioids among high school seniors in the United States. Arch Pediatr Adolesc Med. 2012;166(9):797–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortuna RJ, Robbins BW, Caiola E, Joynt M, Halterman JS. Prescribing of controlled medications to adolescents and young adults in the United States. Pediatrics. 2010;126(6):1108–1116 [DOI] [PubMed] [Google Scholar]
- 13.Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. J Adolesc Health. 1991;12(8):597–605 [DOI] [PubMed] [Google Scholar]
- 14.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78 [DOI] [PubMed] [Google Scholar]
- 15.Cantrill SV, Brown MD, Carlisle RJ, et al. American College of Emergency Physicians Opioid Guideline Writing Panel . Clinical policy: critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60(4):499–525 [DOI] [PubMed] [Google Scholar]
- 16.Ali R, Awwad E, Babor TF, et al. WHO ASSIST Working Group . The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194 [DOI] [PubMed] [Google Scholar]
- 17.Harris KM, Florey F, Tabor J, Bearman PS, Jones J, Udry JR. The National Longitudinal Study of Adolescent Health: Research Design (WWW document). 2003. Available at: www.cpc.unc.edu/projects/addhealth/design. Accessed May 21, 2008
- 18.Zimmerman MA, Copeland LA, Shope JT, Dielman TE. A longitudinal study of self-esteem: implications for adolescent development. J Youth Adolesc. 1997;26(2):117–141 [Google Scholar]
- 19.Wolfe DA, Scott K, Reitzel-Jaffe D, Wekerle C, Grasley C, Straatman AL. Development and validation of the Conflict in Adolescent Dating Relationships Inventory. Psychol Assess. 2001;13(2):277–293 [PubMed] [Google Scholar]
- 20.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67–73 [DOI] [PubMed] [Google Scholar]
- 21.Donovan JE. Young adult drinking-driving: behavioral and psychosocial correlates. J Stud Alcohol. 1993;54(5):600–613 [DOI] [PubMed] [Google Scholar]
- 22.Eaton D, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2009. MMWR Surveill Summ. 2010;59(5):1–142 [PubMed] [Google Scholar]
- 23.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses from the Nation's High School Seniors 2009. Ann Arbor, MI: Institute for Social Research; 2010 [Google Scholar]
- 24.Public Health Service and Health Care Financing Administration. International Classification of Diseases, 9th Revision, Clinical Modification. 6th ed. Washington, DC: Public Health Service; 1998. [Google Scholar]
- 25.Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27(3):305–308 [DOI] [PubMed] [Google Scholar]
- 26.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Results on Adolescents Drug Use: Overview of Key Findings, 2011. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012 [Google Scholar]
- 27.Baehren DF, Marco CA, Droz DE, Sinha S, Callan EM, Akpunonu P. A statewide prescription monitoring program affects emergency department prescribing behaviors. Ann Emerg Med. 2010;56(1):19–23.e1–3. [DOI] [PubMed]
- 28.Clark T, Eadie J, Knue P, Kreiner P, Strickler G. Prescription Drug Monitoring Programs: An Assessment of the Evidence for Best Practices. 2012. Available at: www.pdmpexcellence.org/sites/all/pdfs/Brandeis_PDMP_Report.pdf. Accessed July 1, 2013
- 29.MITRE Corporation. Integrating an emergency department with a prescription drug monitoring program: a pilot study. Enhancing access to prescription drug monitoring programs using health information technology. 2012. Available at: www.healthit.gov/sites/default/files/indiana-1_pdmp_pilot_study_0.pdf. Accessed July 1, 2013
- 30.Albert S, Brason FW, II, Sanford CK, Dasgupta N, Graham J, Lovette B. Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med. 2011;12(suppl 2):S77–S85 [DOI] [PubMed] [Google Scholar]
- 31.Bryner JK, Wang UK, Hui JW, Bedodo M, MacDougall C, Anderson IB. Dextromethorphan abuse in adolescence: an increasing trend: 1999-2004. Arch Pediatr Adolesc Med. 2006;160(12):1217–1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hermos J, Winter M, Heeren T, Hingson R. Alcohol-related problems among younger drinkers who misuse prescription drugs: results from the national epidemiologic survey of alcohol and related conditions (NESARC). Subst Abus. 2009;30(2):118–126 [DOI] [PubMed] [Google Scholar]
- 33.Hermos JA, Winter MR, Heeren TC, Hingson RW. Early age-of-onset drinking predicts prescription drug misuse among teenagers and young adults: results from a national survey. J Addict Med. 2008;2(1):22–30 [DOI] [PubMed] [Google Scholar]
- 34.Hingson RW, Zha WX. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics. 2009;123(6):1477–1484 [DOI] [PubMed] [Google Scholar]
- 35.Eaton DK, Davis KS, Barrios L, Brener ND, Noonan RK. Associations of dating violence victimization with lifetime participation, co-occurrence, and early initiation of risk behaviors among US high school students. J Interpers Violence. 2007;22(5):585–602 [DOI] [PubMed] [Google Scholar]
- 36.McCabe SE, Boyd CJ, Cranford JA, Teter CJ. Motives for nonmedical use of prescription opioids among high school seniors in the United States: self-treatment and beyond. Arch Pediatr Adolesc Med. 2009;163(8):739–744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rigg KK, Ibañez GE. Motivations for non-medical prescription drug use: a mixed methods analysis. J Subst Abuse Treat. 2010;39(3):236–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gray TA, Wish ED. Substance Abuse Need for Treatment among Arrestees (SANTA) in Maryland. College Park, MD: Center for Substance Abuse Research; 1998 [Google Scholar]
- 39.Thornberry TP, Krohn MD. The self-report method of measuring delinquency and crime. In: Duffee D, ed. Measurement and Analysis of Crime and Justice: Criminal Justice 2000. Washington, DC: US Department of Justice, Office of Justice Programs; 2000:33–83 [Google Scholar]
- 40.Buchan BJ, L Dennis M, Tims FM, Diamond GS. Cannabis use: consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction. 2002;97(suppl 1):98–108 [DOI] [PubMed] [Google Scholar]
- 41.Dennis M, Titus JC, Diamond G, et al. C.Y.T. Steering Committee . The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002;97(suppl 1):16–34 [DOI] [PubMed] [Google Scholar]
- 42.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33(6):436–457 [DOI] [PubMed] [Google Scholar]