Abstract
Retroareolar cysts are a rare condition of the adolescent female breast and their reported incidence in the literature is scarce. Arising from obstruction of the terminal channels that drain Montgomery's areolar tubercles retroareolar cysts comprise two different pathological entities; symptomatic and asymptomatic. We report on a case of a symptomatic retroareolar cyst in a 15-year-old girl and review the literature. We highlight the subtle clinical differences from other adolescent breast masses, describe the natural course of the condition and with respect to diagnosis detail the correlation between clinical features and characteristic sonographic findings. Finally, we highlight the importance of preserving the developing breast bud by adopting a conservative approach to the management of retroareolar cysts.
INTRODUCTION
Retroareolar cysts are a condition of adolescent women [1]. Their true incidence is largely unknown and published literature on the disease is scarce [1]. In comparison with the presentation of other adolescent breast masses, retroareolar cysts have subtle clinical differences and must be considered a distinct entity whose management correlates with the clinical course of the condition. In this paper, we report a case of retroareolar cyst, review the literature and suggest the optimal management.
CASE REPORT
A healthy 15-year-old girl presented to her GP with mastalgia and periareolar cellulitis of her right breast. She was initially treated with a course of oral flucloxacillin but after 2 days there was no improvement and an emergency hospital referral was organized. Physical examination identified periareolar erythema in the presence of a tender subareolar inflammatory mass and a mild pyrexia. A provisional diagnosis of retroareolar abscess was made and an ultrasound scan (USS) was requested. The USS revealed three focal fluid collections or cysts located behind the nipple which were in direct communication with each other. The cysts contained echogenic fluid with surrounding hyperaemia and subcutaneous oedema. After conversation with a consultant breast surgeon, it was decided not to aspirate the mass but to discharge the patient on an additional course of amoxicillin and follow her up 3 days later with consultant review.
Subsequent review revealed a mild improvement in symptoms and an alternative diagnosis of retroareolar cyst established. Follow-up with repeat USS 2 days later revealed a well-defined anechoic lesion cystic in nature rather than abscess. The lesion had decreased in size, and clinical examination revealed no existing erythema and decreased tenderness on palpation of the inflammatory mass.
DISCUSSION
Retroareolar cysts are thought to arise from obstruction of the terminal channel that drains Montgomery's areolar tubercles [1, 2]. First described in 1719 by Morgagni, areolar tubercles are small papular projections on the edge of the areola and consist of sebaceous glands and mammary lactiferous structures [1, 2]. The tubercles are related to Montgomery's glands which themselves are postulated to be involved in lactation [2].
Several mechanisms behind the obstruction and subsequent dilatation of the terminal channel that drains Montgomery's tubercle have been suggested. These include ineffective absorption of the ducts secretions, squamous metaplasia of the duct lining, autoimmune primary dilatation of the duct and hormonally induced relaxation of the areolar muscle leading to galactophorus dilatation [1]. Pathological obstruction, regardless of cause, subsequently leads to distension of the small terminal channels and associated acini thus forming a retroareolar cyst [1].
Huneeus et al. [1], in the largest reported series of retroareolar cysts, describe two distinct presentations of the disease. Over a period of 2 years 46 girls between 10 and 20 years of age were categorized either as having inflammatory (67%) or asymptomatic (33%) retroareolar cysts [1]. Asymptomatic retroareolar cyst presents due to the identification of a palpable mass in the subareolar region but in the absence of any inflammatory changes [1, 3]. Inflammatory retroareolar cysts characteristically present with sudden acute mastalgia and periareolar erythema. Clinical examination reveals tenderness, swelling in the areolar and periareolar region and a painful palpable but non-fluctuant mass [1]. Occasionally, inflammatory retroareolar cysts have also been associated with serous areolar discharge [1, 3].
Sonography is the radiological modality that best characterizes retroareolar cysts [1, 4–6]. Garcia et al. [4] in a review of USS in the adolescent breast describe asymptomatic retroareolar cysts presenting as anechoic masses in the breast tissue. The cysts can be multiple in number, round or lobular in shape and contain internal septations or isolated echoes (Fig. 1; [4, 5]). Garcia et al. [4] further describe inflammatory retroareolar cysts to contain echogenic debris, fluid filled levels, internal septations and increased peripheral vascularity [4]. This correlates with our sonographic findings (Fig. 2) and Huneeus et al.'s [1] series who noted the enhanced vascularity only in the symptomatic cyst [1]. Interestingly, Huneeus et al. [1] also reported the presence of bilateral asymptomatic cysts in almost half of their patients.
Figure 1:
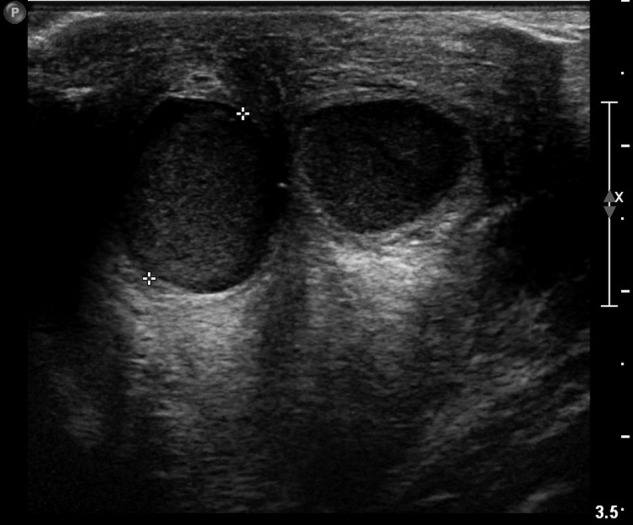
Retroareolar cysts in ultrasonography of the breast.
Figure 2:
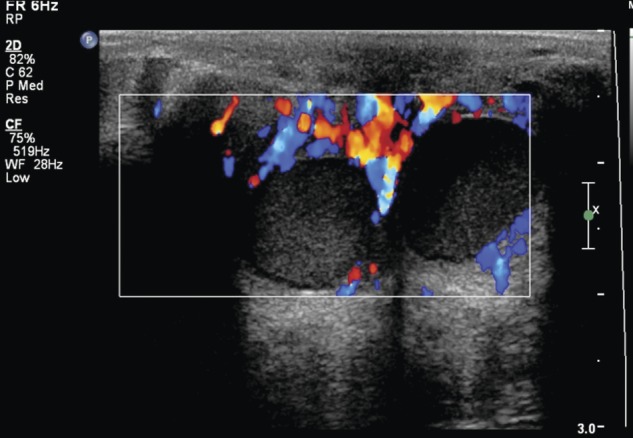
Infected retroareolar cyst with increased peripheral flow.
Successful management of retroareolar cysts is dependent on recognizing it as a distinct clinical entity and, in particular, distinguishing inflammatory retroareolar cysts from a breast abscess. Through this distinction you can avoid unnecessary needle aspiration and thus trauma to the developing breast bud.
Clinically abscesses are more fluctuant or indurated than inflamed retroareolar cysts with a greater propensity to cause more systemic sequelae [5]. The clinical evolution of the disease process also differs. Symptomatic retroareolar cysts follow a relatively benign clinical course and respond quickly to oral antibiotics and non-steroidal anti-inflammatories whereas abscesses often require more traumatic intervention. It is accepted that inflammatory cysts can develop into an abscess but it is rare [1, 4]. Of the 46 patients Huneeus et al. [1] followed up, only one required hospital admission for sepsis and even then traumatic intervention to the developing breast bud was avoided with the abscess responding to intravenous antibiotics.
In the absence of sepsis or severe pain, patients with inflammatory retroareolar cysts can be managed as outpatients [1]. Close clinical and sonographic follow-up is recommended with most inflammatory changes resolving after 7 days with a significant reduction or even absence of the cyst on USS [1, 2]. Interestingly sonographic follow-up of the asymptomatic cysts identify a similar long-term evolution with regression or complete disappearance of the cyst [1].
CONCLUSION
Retroareolar cysts are largely underreported in the literature and as such their development, histopathological characteristics and correlation with normal development of the adolescent breast remain unknown. Symptomatic cysts are managed successfully with oral antibiotics and frequent clinical and ultrasonographic follow-up. Asymptomatic cysts require the same monitoring and reassurance to the patient. Given the relatively benign course of the condition, every effort should be made to preserve the developing breast bud with needle aspiration or incision and drainage considered only in the rare presence of abscess formation unresponsive to antibiotics.
Further reporting of retroareolar cysts is required to identify the true incidence of the condition whilst further studies are required in order to appropriately identify the disease process pathologically and characterize its presence with respect to the normal development of the breast.
ACKNOWLEDGEMENTS
I would like to acknowledge Professor Graham Layer, Chairman of the Trustees of the Breast Unit Fund, for Education and Research (BUFFER).
REFERENCES
- 1.Huneeus A, Schilling A, Hovarth E, Pinochet M, Carrasco D. Retroareolar cysts in the adolescent. J Pediatr Adolesc Gynaecol. 2003;16:45–9. doi: 10.1016/s1083-3188(02)00238-3. doi:10.1016/S1083-3188(02)00238-3. [DOI] [PubMed] [Google Scholar]
- 2.De Silva NK, Brandt ML. Disorders of the breast in children and adolescents, Part 2: breast masses. J Pediatr Adolesc Gynaecol. 2006;19:415–8. doi: 10.1016/j.jpag.2006.09.002. doi:10.1016/j.jpag.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Watkins F, Giacomantonio M, Salisbury S. Nipple discharge and breast Lump related to Montgomery's tubercles in adolescent females. J Pediatr Surg. 1988;23:718–20. doi: 10.1016/s0022-3468(88)80409-3. doi:10.1016/S0022-3468(88)80409-3. [DOI] [PubMed] [Google Scholar]
- 4.Garcia CJ, Espinoza A, Dinamarca V, Navarro O, Daneman A, Garcia H, et al. Breast US in children and adolescents. Radiographics. 2000;20:1605–12. doi: 10.1148/radiographics.20.6.g00nv171605. [DOI] [PubMed] [Google Scholar]
- 5.West KW, Rescorla FJ, Scherer LR, Grosfeld JL. Diagnosis and treatment of symptomatic breast masses in the pediatric population. J Pediatr Surg. 1995;30:182–7. doi: 10.1016/0022-3468(95)90557-x. doi:10.1016/0022-3468(95)90557-X. [DOI] [PubMed] [Google Scholar]
- 6.Bock K, Duda VF, Peyman H, Ramaswamy A, Schulz-Wendtland R, Klose KJ, et al. Pathologic breast conditions in childhood and adolescence: evaluation by sonographic diagnosis. J Ultrasound Med. 2005;24:1347–54. doi: 10.7863/jum.2005.24.10.1347. [DOI] [PubMed] [Google Scholar]


