Abstract
Pseudocysts of the spleen are very rare, found in <1% of the splenectomies done and usually develop secondary to trauma. Pseudocysts of spleen rarely grow to large size and most of these remain asymptomatic, they require exploration only in symptomatic cases and chances for spleen preservation in these cases are usually less. Here, we present two cases of this rare entity developing secondary to abdominal trauma in the past, both presented with complaints of pain and lump in the abdomen. After thorough investigations, laparotomy was done preserving spleen in one case and doing splenectomy in the other. On histopathological examination, diagnosis of splenic pseudocysts was confirmed by the absence of lining epithelium. We would like to report these two cases because of their rarity and as diagnostic dilemmas.
INTRODUCTION
Splenic cysts are rare with around 800 cases reported in the world literature [1]. Cysts of the spleen can be classified as parasitic and non-parasitic. Non-parasitic cysts can be further classified as true cysts and pseudocysts. True cysts are those with an epithelial lining and include epidermoid cyst, epithelial or congenital cysts. Pseudocysts do not have epithelial lining and are usually post-traumatic or inflammatory/degenerative [2]. It is important to distinguish pseudocyst of spleen from other benign/malignant splenic cysts, especially from hydatid cysts in order to follow the right treatment and management option. Splenic pseudocysts mostly remain asymptomatic and require treatment only when they become symptomatic. Usually, only large cysts produce symptoms and are surgically treated by splenectomy or in some cases by splenic preservation surgery as in our second case. Here, we would like to present two cases of splenic pseudocyst as they are rarely diagnosed and present diagnostic challenge to the clinician.
CASE REPORTS
Case 1
A 24-year-old cricketer presented with complaints of left upper abdomen pain, recurrent vomiting and enlarging mass in the same region. There was a history of injury by cricket ball over the rib cage on left side 8 months back. On examination, there was a well demarcated, immobile mass of size ∼30 × 20 cm in the left hypochondrium extending in umbilical and epigastrium, seems to be originating from spleen. The patient was advised for computed tomographic (CT) scanning which showed the presence of a large mass originating from the spleen of size 32 × 20 cm, suggesting some cyst, besides this serum CA 19-9 levels were slightly raised. A surgery was planned considering the diagnosis of splenic cyst and abdomen was explored, and complete splenectomy was done. The histopathological examination confirmed the diagnosis of pseudocyst by the absence of lining epithelium.
Case 2
A 47-year-old female presented with complaints of a small lump (Figs 1–5) in left upper abdomen and a past history of fall on ladders a year back. On examination, there was a small lump confined to the left hypochondrium, firm in consistency with rounded borders suggesting origin from the spleen. The patient underwent CT scan of the abdomen after abdomen sonography and CECT suggested the presence of a cystic lesion originating from the lower margin of spleen ∼12 × 8 cm in size. The patient underwent a surgery and cystic lesion was removed preserving the spleen (Figs 6–8). The cyst on histopathological examination was a pseudocyst.
Figure 1:

Lump in abdomen over left hypochondrium.
Figure 2:
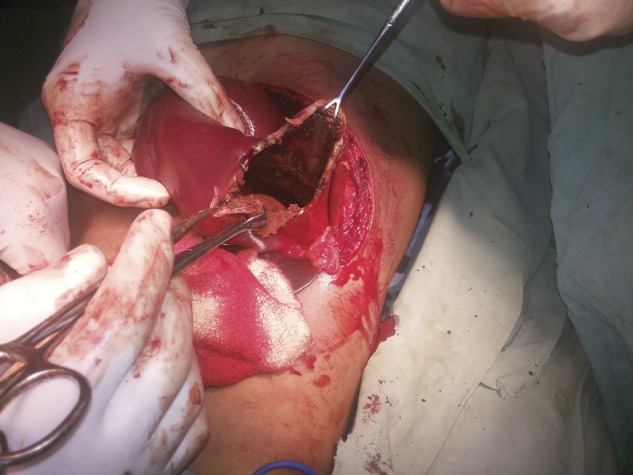
Intraoperative picture of the first patient.
Figure 3:
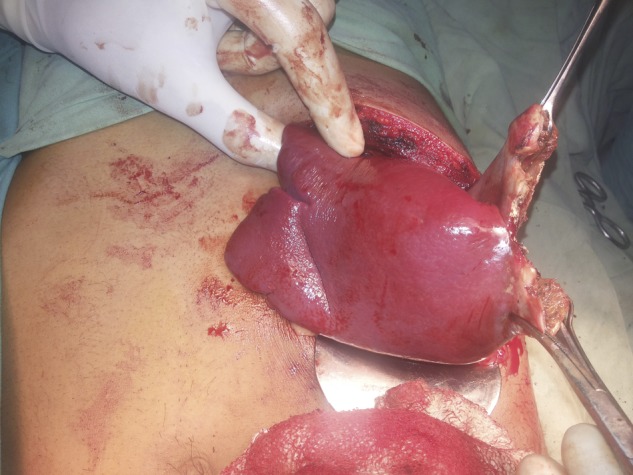
Intraoperative picture of the first patient.
Figure 4:
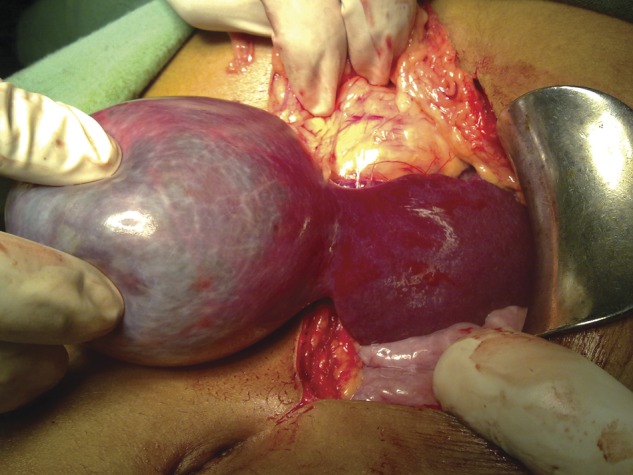
Intraoperative picture of the second patient.
Figure 5:
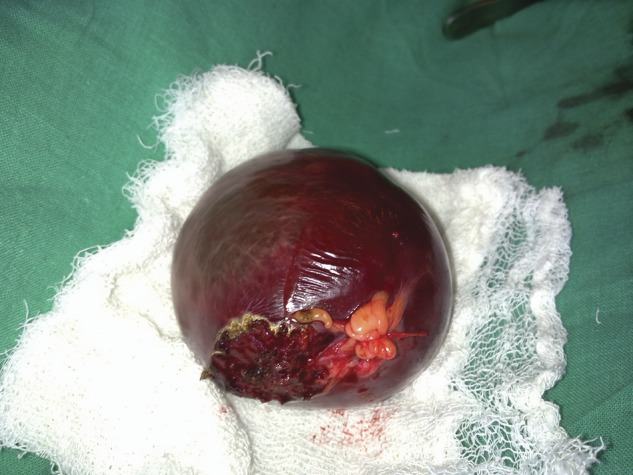
Specimen of the cyst removed from the second patient.
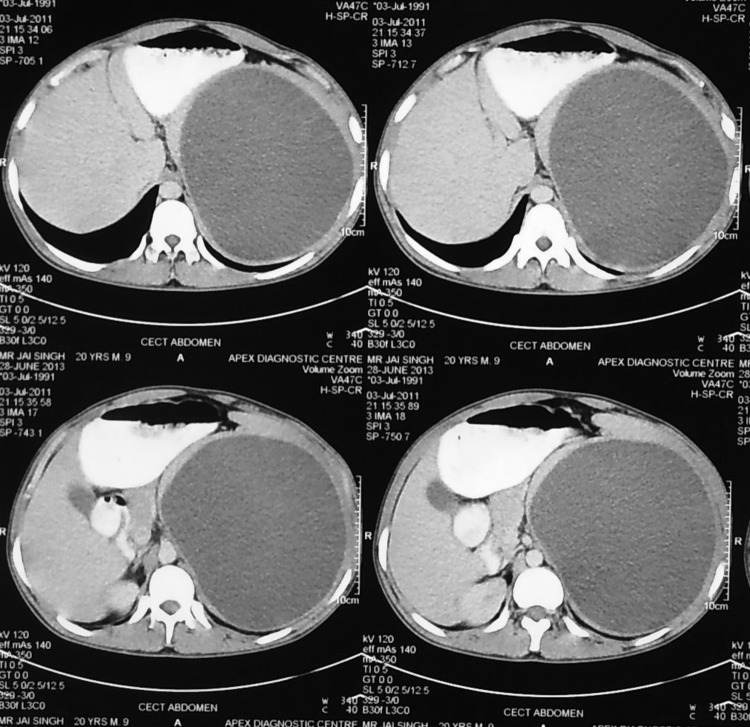
Figure 6:
CECT abdomen showing a huge splenic mass.
Figure 7:
CECT abdomen showing huge splenic mass compressing surrounding structures.
Figure 8:
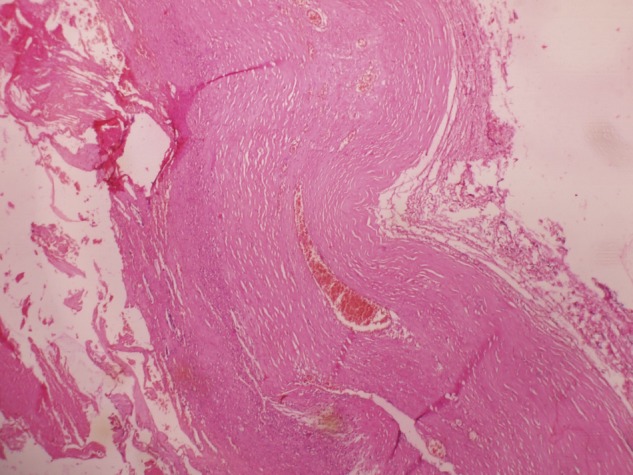
Histopathological slide showing the absence of lining epithelium.
DISCUSSION
A hemmorhagic cyst of the spleen is classified as a secondary (pseudo) non-parasitic cyst and is frequently caused by previous trauma. Symptoms correlate with the size and location of the cyst [3]. Most of the splenic pseudocysts (30–60%) are asymptomatic and cause problems as they enlarge. Common clinical presentation includes abdominal pain, nausea and vomiting due to compression of stomach by a large splenic cyst. Complications include rupture of spleen, intracapsular hemmorhage and infection [1].
The wall of a pseudocyst is composed of dense fibrous tissue with no epithelial lining and occasionally contains hemosiderin. To our knowledge, serum CA 19-9 levels are high in most true cysts but are rarely high in hemmorhagic pseudocysts because of the absence of epithelial lining [4]. CA 19-9 levels were raised in one of our cases.
Cystic lesions of the spleen rarely cause clinical symptoms, they are usually diagnosed incidentally by abdominal imaging for another purpose. When a benign cyst is considered as a preoperative diagnosis, preservation of spleen is the aim of surgical treatment and can prevent the risk of overwhelming post-splenectomy sepsis, especially in children and young patients [5]. Percutaneous drainage with or without injection of a chemical agent may decrease the size of large cysts, but this procedure is associated with a high rate of recurrence [6]. Total splenectomy is suggested only for huge cysts as well as cysts covered with splenic parenchyma or, cysts located near the hilum [7].
Recently, spleen preserving techniques like watchful waiting, percutaneous drainage, marsupialisation, splenic decapsularization and complete cystectomy with partial splenectomy have been tried, still the gold standard remains splenectomy [8].
REFERENCES
- 1.Geraghty M, Khan IZ, Conlon KC. Large primary splenic cyst: a laparoscopic technique. J Minim Access Surg. 2009;5:14–6. doi: 10.4103/0972-9941.51315. doi:10.4103/0972-9941.51315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fowler RH. Non parasitic benign cystic tumours of the spleen. Int Abstr Surg. 1953;96:209–27. [PubMed] [Google Scholar]
- 3.Balzan SM, Riedner CE, Santos LM, Pazzinatto CM, Fontes PR. Post traumatic splenic cysts and partial splenectomy: report of a case. Surg Today. 2001;31:262–5. doi: 10.1007/s005950170183. doi:10.1007/s005950170183. [DOI] [PubMed] [Google Scholar]
- 4.Madia C, Lumachi F, Veroux M, Fiamingo P, Gringeri E, Brolese A, et al. Giant splenic epithelial cyst with elevated serum markers CEA and CA 19–9 levels: an incidental association. Anticancer Res. 2003;23:773–6. [PubMed] [Google Scholar]
- 5.Eraklis AJ, Kevy SV, Diamond LK, Gross RE. Hazard of overwhelming infection after splenectomy in children. N Engl J Med. 1967;276:1225–9. doi: 10.1056/NEJM196706012762203. doi:10.1056/NEJM196706012762203. [DOI] [PubMed] [Google Scholar]
- 6.Moir C, Guttman F, Jequier S, Sonnino R, Youssef S. Splenic cysts: aspiration, sclerosis, or resection. J Pediatr Surg. 1989;24:646–8. doi: 10.1016/s0022-3468(89)80711-0. doi:10.1016/S0022-3468(89)80711-0. [DOI] [PubMed] [Google Scholar]
- 7.Stoidis CN, Spyropoulos BG, Missiakos EP, Fountzilas CK, Paraskeva PP, Fotiadis CI. Spontaneous regression of a splenic cyst: a case report and review of literature. Cases J. 2009;2:8730. doi: 10.4076/1757-1626-2-8730. doi:10.4076/1757-1626-2-8730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu HM, Kortbeek JB. Management of splenic pseudocysts following trauma: a retrospective case series. Am J Surg. 2006;191:631–4. doi: 10.1016/j.amjsurg.2006.01.034. doi:10.1016/j.amjsurg.2006.01.034. [DOI] [PubMed] [Google Scholar]