Abstract
Background
In 2011, German hospitals treated approximately 205 000 patients suffering from acute poisoning. Change is seen over time both in the types of poisoning that occur and in the indications for specific treatment.
Methods
This article is based on a selective review of the literature, with special attention to the health reports of the German federal government, the annual reports of the GIZ-Nord Poisons Center (the poison information center for the four northwestern states of Germany, i.e. Bremen, Hamburg, Lower Saxony and Schleswig-Holstein), and the recommendations of international medical associations.
Results
From 1996 to 2011, the GIZ-Nord Poisons Center answered more than 450 000 inquiries, most of which involved exposures to medical drugs, chemicals, plants, foods, or cosmetics. Poisoning was clinically manifest in only a fraction of these cases. Ethanol intoxication is the commonest type of acute poisoning and suicide by medical drug overdose is the commonest type of suicide by poisoning. Death from acute poisoning is most commonly the result of either smoke inhalation or illegal drug use. Severe poisoning is only rarely due to the ingestion of chemicals (particularly detergents and cleaning products), cosmetics, or plant matter. Medical procedures that are intended to reduce the absorption of a poison or enhance its elimination are now only rarely indicated. Antidotes (e.g., atropine, 4-dimethylaminophenol, naloxone, toluidine blue) are available for only a few kinds of poisoning. Randomized clinical trials of treatment have been carried out for only a few substances.
Conclusion
Most exposures to poisons can be treated with general emergency care and, if necessary, with symptomatic intensive-care measures. Poison information centers help ensure that cases of poisoning are dealt with efficiently. The data they collect are a useful aid to toxicological assessment and can serve as a point of departure for research projects.
Poisoning has always been a part of human life. The causes and scientific understanding of poisoning change over time, and with them the opportunities for its correct diagnosis and treatment.
In earlier times, poisoning was thought of as a single clinical entity that could be prevented, or treated, in practically the same way for all agents: Standard “detoxifying measures” were used, and supposed universal antidotes such as mithridate and theriac were held to be able to counteract the effects of any and all poisons. Today, modern analytical toxicology and the rapid accessibility of support from poison information centers enable treating physicians to address each case individually, with much more accurate poisoning risk assessment. The specific treatment to be provided depends on the toxic substance and dose involved.
Clinical epidemiology
Health problems caused by longstanding tobacco and ethanol consumption can be thought of as types of chronic poisoning. Although such problems are by far the most common “intoxications” affecting our society in this broad sense of the term (1, 2), we will not discuss this matter in any further detail here and will restrict our topic to acute intoxications.
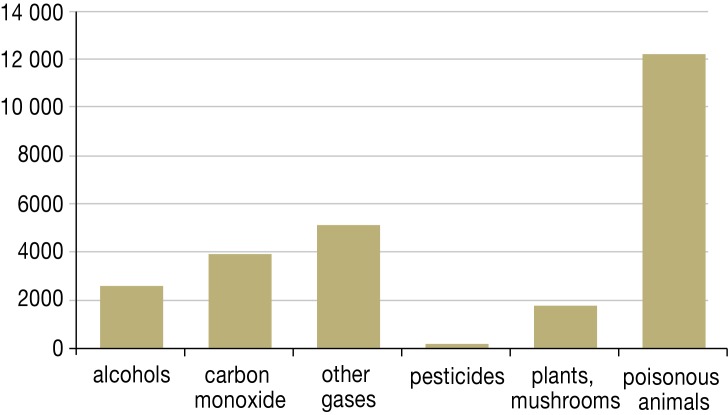
The causes of acute poisoning change over time. Some substances that were once very common causes of poisoning are now only rarely so: These include barbiturates, older types of rodenticide (thallium compounds), and alkyl phosphate insecticides such as parathion (see Figure 1, pesticides). Newer medications, illegal drugs, technical products such as cleaning agents and cosmetics, and new consuming habits (both intentional and unintentional) have also changed the overall picture substantially.
Figure 1.
Substances of mainly non-medical use that were most commonly involved in cases of acute poisoning treated in German hospitals in 2011 (4, 5). Alcohols by type: ethanol (1497), not further specified (1201), methanol (21), 2-propanol (39) (according to ICD-T51)
Chronic poisoning.
Health problems caused by longstanding tobacco and ethanol consumption can be thought of as types of chronic poisoning.
No detailed database on the frequency of various types of poisoning is currently available, even though intoxications are reportable illnesses under German law (§16e of the Chemikaliengesetz [Chemicals Act]).
The official cause-of-death statistics for Germany in the year 2011 included 1987 deaths (0.23% of all deaths) that were classified under the ICD-10 codes T36–50 (medications, illegal drugs, biologically active substances) and 1296 (0.15%) that were classified under codes T51–65 (substances of non-medical use) (3). 1410 deaths were classified as intentional self-intoxication with medications (X60–X64). In this article, we discuss the most common types of poisoning.
The German hospital diagnosis statistics for the year 2011 included 205 121 cases of treatment for acute intoxication (4, 5):
43 675 in-hospital treatments with the main diagnosis of poisoning with medications, illegal drugs, and biologically active substances (T36–50);
29 927 treatments for the toxic effects of substances of mainly non-medical use (T51–65);
131 519 treatments for mental and behavioral disturbances caused by acute intoxication with psychotropic substances (F10.0–19.0).
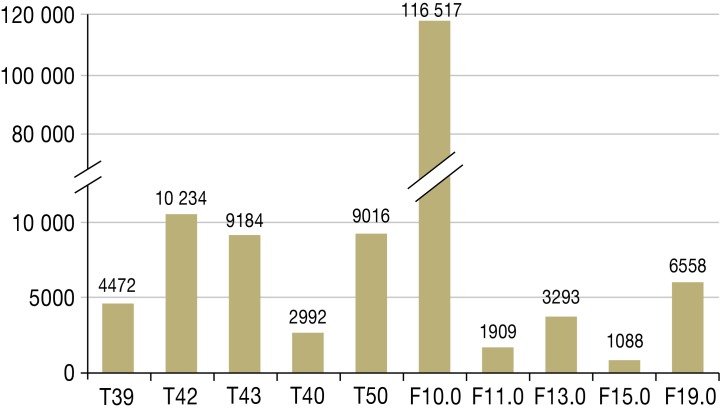
Acute alcohol poisoning was classified under the ICD-10 code T51 in a small minority of cases (2858 cases, cf. Figure 1) and under the code F10.0 in most cases (116 517 cases, cf. Figure 2) (4, 5).
Figure 2.
Medications, illegal drugs, and biologically active substances most commonly involved in cases of acute poisoning treated in German hospitals in 2011 (4, 5)
T39 = analgesics (ca. 40% 4-aminophenol derivatives)
T42 = hypnotics (ca. 50% benzodiazepines) and antiepileptic drugs
T43 = antidepressants, neuroleptic drugs, psychotropic substances (not further classified)
T40 = narcotics, methadone, hallucinogens (especially morphine and codeine)
T50 = other medications, not further specified
Mental and behavioral disturbances due to acute intoxication with: F10.0 = alcohol (ethanol)
F11.0 = opioids
F13.0 = hypnotics, sedatives
F15.0 = stimulants
F19.0 = multiple substance use
Substances affecting the central nervous system were involved in most intoxications with medications (Figure 2).
The substances of non-medical use that were most commonly involved in intoxications were the following:
alcohols, mainly ethanol;
carbon monoxide and other gases and vapors, as well as other kinds of smoke and harmful substances;
substances ingested with food, including plants and mushrooms;
substances derived from contact with poisonous animals (insect bites in the vast majority of cases).
For the purpose of comparison, cf. pesticide poisoning (Figure 1).
Substances affecting the CNS.
Most intoxications with medications are due to substances affecting the central nervous system.
Treatment.
Most patients suffering from intoxication are treated purely symptomatically.
The statistics compiled by the German poison information centers (Giftinformationszentren, GIZ) are based on a more detailed classification and thus enable a finer analysis. About half of all inquiries to the GIZ-Nord Poisons Center (the responsible center for for the four northwestern states of Germany, i.e. Bremen, Hamburg, Lower Saxony and Schleswig-Holstein) come from doctors in a full range of outpatient and inpatient treatment settings (hospitals, practices, emergency medical services); the other half come from persons who had been exposed or thought they had been exposed to a toxic substance.
The approximately 456 173 inquiries that were received from 1996 to 2011 most commonly dealt with real or potential intoxication with medications, chemical products, plants, food items (especially products containing alcohol), or cosmetics. Data were collected in accordance with European legislation (6). The severity of poisoning was initially documented in terms of estimated risk with the Poisoning Severity Score (7) and was followed up in cases of severe poisoning.
Manifest intoxications often arose after the ingestion of medications, illegal drugs, and chemical products. In contrast, the ingestion of cosmetics or plants led to manifest intoxication in only a small percentage of exposures. There were only a few cases of severe poisoning from plants indigenous to Germany, including, for example, death cap mushrooms (Amanita phalloides) and wolfsbane (Aconitum napellus).
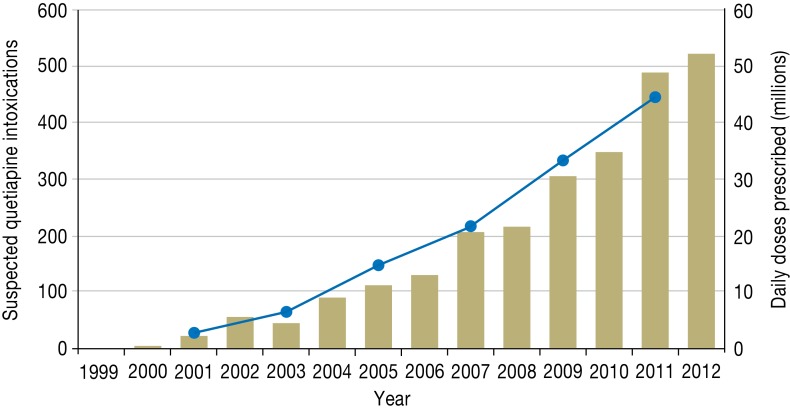
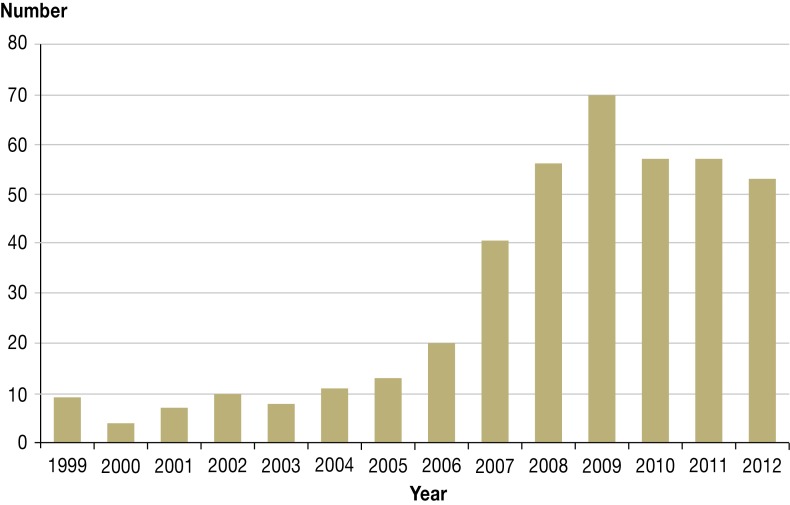
One of the tasks of poison information centers is to detect poisoning arising from any new medication by observing the increasing incidence of poisoning with it as the prescription frequency rises (pharmacovigilance). The case of quetiapine (8, 9) can serve as an illustration (Figure 3).
Figure 3.
Inquiries about suspected quetiapine intoxication that were addressed to the GIZ-Nord Poisons Center compared to annual volume of quetiapine prescriptions (8, 9)
Manifest intoxications.
Manifest intoxications often arise after the ingestion of medications, illegal drugs, and chemicals.
The poison information centers in Germany maintain an information-sharing system (Informationsverbund) so that cases of poisoning from various centers can be evaluated as a group. This enables rapid risk assessment for products that have recently appeared on the market (10).
The German Federal Institute for Risk Assessment (Bundesinstitut für Risikobewertung, BfR) collects and analyzes case reports and issues position statements as an aid to decision-making, with the aim of making foods and chemicals safer.
The treatment of poisoning: general aspects
Clinical trials in toxicology are often hard to carry out: The framework conditions are hardly ever the same from one case of poisoning to another, and, as a result, the assessment of any particular intervention may be problematic. The available data on various types of treatment have been taken into consideration in the position papers issued by the medical societies.
Pre-hospital measures for persons suffering from an intoxication generally consist of the usual emergency measures for securing vital bodily functions.
It is essential to take a detailed history from the patient and any other involved persons and to obtain samples of medications (and their packages), food remnants, vomitus, and any products that may have caused the intoxication. In particular, the samples obtained at the outset may turn out to be of major forensic importance.
Pre-hospital measures.
Pre-hospital measures for persons suffering from intoxication generally consist of the usual emergency measures for securing vital bodily functions.
When intoxication occurs in the workplace, safety data sheets may yield clues to the presence of toxic residues in the products that are used there.
Even for patients with no or only mild symptoms the situation may become life-threatening. Medical observation is therefore necessary until such a situation can be excluded by a reliable risk assessment based on clinical diagnosis and, where appropriate, additional laboratory testing.
Long latencies are characteristic of, for example, poisoning by mushrooms of the Cortinarius species (e.g., the fool’s webcap Cortinarius orellanus), death cap mushrooms, or paracetamol. There may be an oligosymptomatic interval lasting several days before life-threatening manifestations arise.
Poison information centers have comprehensive information about active substances and products and can help with the identification of the toxic substance and with an assessment of the risks and probable course of the episode.
The poison information centers offer assistance with the proper choice of laboratory tests, the selection and transport of samples (urine and serum samples taken early on in the patient’s course), determination of a laboratory that can perform the necessary tests at once, and logistical support so that the case can be dealt with rapidly.
Patients who have been exposed to poisonous substances in doses that are so small as to be clearly non-toxic need no further work-up or treatment. All other patients are initially treated with symptom-oriented management.
Treatments that lower absorption or enhance elimination are only rarely indicated; the same is true of pre-hospital treatment with antidote (i.e., at the site of poisoning). For patients who have ingested corrosive substances (e.g., acids or bases), rapid irrigation of the mucous membranes is indicated, while induced vomiting and the use of activated charcoal are contraindicated. The administration of milk to poisoning victims is hardly ever useful, despite a persistent traditional notion to this effect.
Milk for poisoning victims?
The administration of milk to poisoning victims is hardly ever useful, despite a persistent traditional notion to this effect.
The treatment of poisoning: specific treatments
Treatments that lower absorption
Early administration of a single dose of activated charcoal—Gastric lavage (“stomach pumping”) and provoked vomiting, once common measures for lowering the absorption of ingested poisons, have been largely abandoned in favor of the administration of activated charcoal in aqueous suspension. This method of lowering absorption is markedly less invasive and considerably less dangerous when performed for the proper indications.
Nonetheless, one should not administer activated charcoal before knowing the adsorptive properties of the ingested substance. Activated charcoal adsorbs many medications, alkaloids, and vitamin K antagonists well, but many other substances are not adsorbed to any useful extent.
Activated charcoal administration is contraindicated after the ingestion of corrosive substances (e.g., inorganic acids), surfactants, or liquid hydrocarbons, and whenever the respiratory tract has not been protected (by intubation) (e1, e2).
The main risk associated with the administration of an activated charcoal suspension is aspiration.
Experience in poison information centers has shown that activated charcoal is often given in an insufficient dose; 0.5–1 g/kg body weight is recommended. Suspension in adequate amounts of fluid is necessary to avoid provoking ileus.
The administration of a sufficient dose of activated charcoal is particularly important in overdoses of medications that have a delayed pharmacological effect (11, e2, e3). Some medications, when taken in large amounts, form bezoars in the gastrointestinal tract that can be the source of dangerously protracted resorption long after the initial ingestion.
Gastric lavage—The putative clinical benefit of gastric lavage has never been unequivocally demonstrated; on the other hand, the severe complications that have been observed in controlled trials include aspiration, hypoxia, pneumonia, perforation, and laryngospasm (12). As a result, after extensive discussion in specialty societies for clinical toxicology, the indications for gastric lavage as a means of reducing the absorption of poisonous substances have been substantially restricted (12, e4– e7). As a rule, this method should only be considered in life-threatening cases within 60 minutes of the ingestion. Contraindications include corrosive injuries with acids or bases, ingestions of liquid hydrocarbons of low viscosity such as gasoline, and loss of the protective airway reflexes (in patients who are not intubated). In the latest version of a relevant position paper, dated February 2013, it is recommended that gastric lavage should be performed only by a physician with experience in the technique (12).
Lowering absorption.
Gastric lavage and provoked vomiting, once common measures for lowering the absorption of ingested poisons, have been largely abandoned in favor of the administration of activated charcoal in aqueous suspension.
Induced vomiting—Ipecac syrup was used for many years to provoke vomiting in children after toxic ingestions; this is no longer considered an appropriate routine measure (13, e8).
Another historic method of inducing vomiting was with intramuscularly administered apomorphine. The administration of sodium chloride solution to induce vomiting is, likewise, an obsolete treatment: Particularly in children (14), this can cause hypernatremia if the patient, against expectation, does not vomit (e9). 3 grams of sodium chloride per kilogram of body weight is stated to be a lethal dose (15).
Anterograde intestinal lavage—Anterograde intestinal lavage is used in only a few kinds of poisoning, in which rapid removal of the intestinal contents is necessary to prevent the absorption of potentially lethal amounts of the toxic substance (e.g., overdoses of timed-release medications, or of illegal drugs transported within the gut in plastic bags or similar containers) (16).
Laxatives—Laxatives such as sorbitol or, more commonly, sodium sulfate were given in earlier years to treat acute poisoning, but their use is no longer recommended. The simultaneous administration of laxatives and activated charcoal lowers the efficacy of both (17).
Treatments that enhance elimination
Various methods can be used to enhance the elimination of toxic substances with a long half-life. The preferred method depends on the substance to be eliminated.
Repeated administration of activated charcoal
The administration of activated charcoal enhances the elimination of a toxic substance either by interrupting the enterohepatic circulation or else by lowering the concentration of free toxic substance in the intestinal lumen below its intravascular concentration, so that the intestinal wall functions as a dialysis membrane for the removal of the substance via the gastrointestinal tract.
The appropriate, effective use of activated charcoal to enhance elimination (like its use to reduce absorption) requires knowledge of the adsorptive properties and route of elimination of the toxic substance in question.
Urine alkalinization.
Alkalinization of the urine to pH values above 7.5 by the intravenous administration of sodium bicarbonate is recommended mainly for patients with salicylate intoxication.
Clinical trials have shown the benefit of repeated administration of activated charcoal in life-threatening cases of poisoning with one of a small group of medications (carbamazepine, theophylline, dapsone, phenobarbital, quinine) (18). The utility of giving activated charcoal repeatedly in other types of poisoning is doubtful: For example, one of the few pertinent randomized trials showed no clear benefit from this method in the treatment of phenytoin poisoning (19).
Urine alkalinization
Alkalinization of the urine to pH values above 7.5 by the intravenous administration of sodium bicarbonate is recommended mainly for patients with salicylate intoxication. The treatment is intended to enhance the elimination of the drug and thereby prevent acidosis. Although this would also be a simple, reasonable way to treat barbiturate poisoning, it is no longer recommended for this purpose because of the demonstrated superiority of activated charcoal administration (20, e10). Alkalinization of the urine was discussed at one time as a possible treatment for methotrexate poisoning but has become obsolete for this purpose, because such patients are now treated with folinic acid and, when indicated, glucarpidase.
A Cochrane analysis concluded that urine alkalinization can also be considered in severe intoxication with dichlorophenoxyacetic acid herbicides (21, e10).
Hemodialysis
Hemodialysis is a suitable method for the rapid removal of short-chain alcohols such as methanol and ethylene glycol, particularly when the intoxication has already caused acidosis. Fomepizole, a well-tolerated and effective antidote, can often obviate the need for dialysis if given early enough (e11). Hemodialysis is also recommended for the treatment of poisoning with a variety of other substances including salicylates, valproate, lithium, carbamazepine, phenytoin, and metformin. In metformin poisoning, the lactic acidosis that arises because of the intoxication can be treated concomitantly (22).
Hemoperfusion
Hemoperfusion has substantial adverse effects and is therefore indicated only to treat types of poisoning that cannot be satisfactorily treated in other ways (e.g., by dialysis). It is now hardly ever used, as its scope of application is essentially the same as that of repetitive activated charcoal administration.
Induced vomiting.
Although ipecac syrup was used for many years to provoke vomiting in children after toxic ingestions, this is no longer considered an appropriate routine measure.
Antidotes
Now as in the past, the administration of an effective antidote is considered the ideal treatment of poisoning. Well-tolerated antidotes can be used safely and with ease: e.g., acetylcysteine for paracetamol intoxications (usually given intravenously in an amount depending on body weight), dimethicone for surfactant ingestions, and fomepizole for poisoning with methanol or glycols. Fomepizole inhibits alcohol dehydrogenase (14) and has replaced ethanol as an antidote with substantially higher toxicity.
As a consequence of recent improvements in symptom-oriented intensive care medicine, the use of certain antidotes that carry the risk of severe complications must be re-evaluated.
The physician using such antidotes needs to have detailed knowledge of the substances used (e.g., antisera, chelators) and their clinical effects. A list of historical and current antidotes and their clinical uses can be found, for example, on the GIZ-Nord website (23).
The “Bremen List” is a proposal for a minimal antidote kit, which was intended to serve as the basis for further discussions of this topic (Box) (24).
Box. Proposed minimal antidote kit: the “Bremen List” (cf. [24]).
Atropine 100 mg ampoule, indication: organophosphate intoxication
4-DMAP (dimethylaminophenol) 250 mg ampoule, indication: cyanide intoxication
Naloxone 0.4 mg ampoule, indication: opioid intoxication
Toluidine blue 300 mg ampoule, indication: poisoning with substances that cause methemoglobin formation
Medical activated charcoal 50 g, before arrival in hospital, only after consultation with poison center
Recently introduced antidotes include glucarpidase for methotrexate overdoses, icatibant for ACE-inhibitor– induced angioedema, uridine triacetate for fluorouracil overdoses, and deferasirox as a new chelator for iron overload.
New treatments for specific types of poisoning
Insulin therapy has not yet become established as a treatment for beta-blocker and calcium-antagonist poisoning because of the insufficient clinical experience to date (25).
Life-threatening poisoning with local anesthetics has been treated successfully with the administration of lipid emulsions, so-called lipid rescue therapy (26).
Selected individual types of poisoning
Psychotropic drugs
Tricyclic antidepressants and sedating neuroleptic drugs such as phenothiazines are often ingested with suicidal intent. When taken accidentally by a child, the normal therapeutic daily dose for an adult may suffice to cause overt signs of poisoning (e12). The main clinical manifestations are those of the anticholinergic syndrome. When a potentially lethal dose has been taken, the treatment consists of gastric lavage as soon as possible, or else a single administration of activated charcoal within an hour of ingestion. If sedation has already set in, activated charcoal administration is contraindicated because of the risk of aspiration.
Poisoning with tricyclic antidepressants.
When a potentially lethal dose has been taken, the treatment consists of gastric lavage as soon as possible, or else a single administration of activated charcoal within an hour of ingestion.
Attempts to enhance the elimination of tricyclic antidepressants are unlikely to succeed because of their large volume of distribution and their extensive binding to plasma proteins. Raising the blood pH with sodium bicarbonate lowers the free active substance concentration and simultaneously raises the serum sodium concentration, making cardiac arrhythmia less likely (27).
Flumazenil is now considered to be contraindicated for patients who are intoxicated with psychotropic drugs. The same is true of physostigmine, which was once commonly recommended as an antidote for the anticholinergic symptoms of tricyclic antidepressant overdose (e12).
The newer antidepressants (selective serotonin reuptake inhibitors, SSRI) are less cardiotoxic. Their effects can be potentiated, however, by simultaneous administration with other drugs that have a similar mechanism of action, such as appetite suppressants; the serotonin syndrome may result.
A further group of substances often involved in poisoning consists of opium, diamorphine (heroin), other opioids such as methadone, other synthetic narcotics, cocaine, and other (hallucinogenic) drugs. Now as in the past, treatment with an opioid antagonist (naloxone) is indicated to treat poisoning due to any substance that acts at the opiate receptor. Poisoning with other types of substances is best treated symptomatically.
Novel psychoactive substances
The newer designer drugs also belong to the class of “psychodysleptic” agents. Many substances in this large and diverse group are already explicitly covered by the German Narcotics Act (Betäubungsmittelgesetz) (28).
Substances that act at the opiate receptor.
Now as in the past, treatment with an opioid antagonist (naloxone) is indicated to treat poisoning due to any substance that acts at the opiate receptor.
Alongside substances that have been in use since the 1930s, such as metamphetamine (INN: metamfetamine), currently popular designer drugs (newer amphetamine and cathinone derivatives) are offered for sale over the Internet, often deliberately mislabeled as “bath salts,” “plant food,” or “research chemicals.” Some act mainly as stimulants, others mainly as hallucinogens (28– 30).
“Spice,” a substance that recently appeared on the market in Germany, was touted as a mixture of exotic plants that are little known here. Extensive toxicological analysis revealed that the plant material was doped with synthetic cannabinoid receptor agonists. These designer compounds (31) evade detection by the rapid tests for traditional illegal drugs that have been in common use up to the present. Now that the analytical identification of the offending substance has become possible in individual clinical cases, toxic side effects have been found to occur more commonly after the consumption of synthetic cannabinoids than after the consumption of tetrahydrocannabinol (32). Drug dependence has also been described (33).
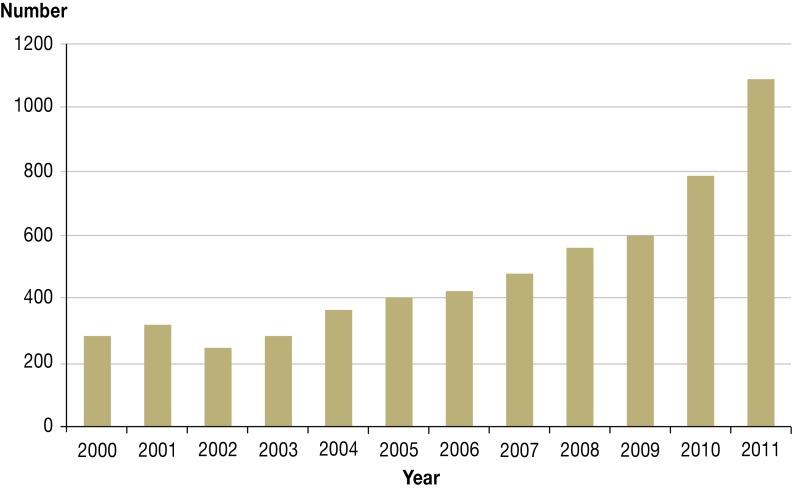
The figures in current drug reports reveal a marked rise in the consumption of designer drugs (34). The most prominent effects of such substances are often their sympathomimetic effects, which are especially evident in overdoses (Figure 4).
Figure 4.
Treatments in German hospitals, for intoxication with stimulants, F15.0 (4)
Because of the way they are manufactured, illegal drugs may contain neurotoxic by-products that can induce parkinsonism.
Beware: parkinsonism.
Because of the way they are manufactured, illegal drugs may contain neurotoxic by-products that can induce parkinsonism.
An analysis of substances being offered for sale over the Internet revealed a group of legal drugs of botanical origin that are commonly touted as “legal highs” and can be obtained without any difficulty:
diviner’s sage (Salvia divinorum, salvinorin A);
hallucinogenic mushrooms (ibotenic acid, muscimol);
kratom (Mitragyna speciosa, mitragynin), a botanical drug with an opiate receptor-agonist effect that is cultivated and consumed in a number of Asian and African countries despite being prohibited there;
Hawaiian baby woodrose (Argyreia nervosa, syn. Argyreia speciosa [L. f.], lysergic acid amide) (e13).
The hallucinogenic effect of these substances is treated purely symptomatically, if treatment is needed.
Analgesics
Among the non-opioid analgesics, paracetamol (= acetaminophen) is now taken less commonly with suicidal intent than was previously the case. The induction of cytochrome P450 isoenzyme 2E1 by alcohol or, less commonly, by prescription drugs potentiates the toxic effect of paracetamol by promoting the generation of toxic metabolites.
Acetylcysteine.
Acetylcysteine is a well-tolerated antidote whose main effect is to promote glutathione synthesis and thereby accelerate the inactivation of the toxic paracetamol metabolite N-acetyl-p-benzoquinone imine.
Acetylcysteine is a well-tolerated antidote whose main effect is to promote glutathione synthesis and thereby accelerate the inactivation of the toxic paracetamol metabolite N-acetyl-p-benzoquinone imine.
Poisoning with substances of mainly non-medical use
Alcohols
In recent years, the contamination of alcoholic drinks with methanol has repeatedly led to episodes of mass poisoning with lethal outcomes (e14).
A major problem in such cases is the delayed initiation of specific treatment, nearly always because of delayed diagnosis: Toxic products arise as a result of metabolism through the action of the enzyme alcohol dehydrogenase. On the other hand, patients treated early with fomepizole or with hemodialysis have a good prognosis. Rapid and reliable clinical diagnosis is now available by means of toxicological analysis (e15).
Ethylene glycol poisoning is often a suspected diagnosis in children. Swallowing even a single mouthful of antifreeze (which is often stored in beverage bottles) can produce overt signs of poisoning (14). Here, too, the treatment consists of early administration of fomepizole, and possibly hemodialysis if treatment is initiated late and the patient is already suffering from marked acidosis (e11).
Antifreeze poisoning.
Here, too, the treatment consists of early administration of fomepizole, and possibly hemodialysis if treatment is initiated late and the patient is already suffering from marked acidosis.
The last few years have seen a marked rise in the number of cases of severe ethanol intoxication among adolescents in Germany (cf. the German Drogensuchtbericht [Drug Addiction Report] for 2012, [34]). Ethanol poisoning and ethanol-related health impairment will not be discussed any further here (see Figures 1 and 2); ethanol accounts for about 60% of all hospital admissions for acute intoxication.
Gamma-hydroxybutyric acid (GHB), 1,4-butanediol, Gamma-butyrolactone (liquid ecstasy)
The consumption of gamma-hydroxybutyric acid (GHB, liquid ecstasy) has risen in recent years. This substance is approved as an intravenous anesthetic, and its sodium salt is approved for the symptomatic treatment of narcolepsy with cataplexy; it is covered by the German Law on Narcotics. In contrast, there are few if any legal restrictions on the sale and consumption of two toxicologically related substances, the common solvent gamma-butyrolactone and the chemical intermediate product 1,4-butanediol, both of which are metabolized to GHB in the body (e16) (Figure 5).
Figure 5.
Inquiries about gamma-hydroxybutyric acid (GHB) intoxications (data from the GIZ-Nord Poisons Center)
The detection of gamma-hydroxybutyric acid.
Exogenous GHB can be detected in the blood or urine for only about 6 (resp. 12) hours after ingestion, as the substance is rapidly metabolized and is also normally synthesized in the body in small amounts.
GHB is sold on the black market with powerfully associative advertising (e.g., as a putative “cattle anesthetic”) and taken by users with the intention of elevating mood; as it has no recognizable taste, it is also sometimes given surreptitiously to unsuspecting persons as a “date-rape” drug or knock-out preparation (35). It causes sudden loss of consciousness with amnesia afterward; its use can be highly dangerous, particularly in an overdose or in mixed intoxications. Exogenous GHB can be detected in the blood or urine for only about 6 (resp. 12) hours after ingestion, as the substance is rapidly metabolized and is also normally synthesized in the body in small amounts.
Carbon monoxide
Carbon monoxide poisoning due to the use of coal gas now belongs to the realm of history. At present, domestic carbon monoxide poisoning can result from the improper use of wood-charcoal grills, from defective heaters (36), or from smoke inhalation. Carbon monoxide poisoning is also an important topic in occupational medicine surveys (e17). It is treated by the administration of oxygen at normobaric pressure, or at hyperbaric pressure for severe cases in order to transport more physically dissolved oxygen. The indications for hyperbaric oxygenation differ from one country to another. The carbon monoxide poisoning guideline of the German Society for Occupational and Environmental Medicine (Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V., DGAUM) was revised in 2011: Hyperbaric oxygenation is stated to be a reasonable treatment for patients with moderate or severe manifestations of carbon monoxide poisoning, if a suitable pressure chamber is available, because it may lower the risk of late neurological complications. On the other hand, a Cochrane review of 2011 comes to no definitive conclusion about hyperbaric oxygenation (37).
Gases, smoke
Exposures to airborne particulate matter are associated with many diseases that can be considered types of chronic poisoning (tobacco smoke, exhaust fumes, fiber dust) (e18).
Gases and smoke.
Exposures to airborne particulate matter are associated with many diseases that can be considered types of chronic poisoning (tobacco smoke, exhaust fumes, fiber dust).
Smoke inhalation is a common cause of acute poisoning. Its victims may have inhaled not only carbon monoxide, but also other toxic substances, such as hydrogen cyanide. These two gases work synergistically, on the one hand lowering the oxygen-transporting capacity of hemoglobin by forming carboxyhemoglobin, and on the other hand impairing electron transport by forming cyanide complexes with the trivalent iron atom of cytochrome oxidase. Treating hydrogen cyanide poisoning with 4-dimethylaminophenol (4-DMAP) is contraindicated when the patient has been simultaneously exposed to carbon monoxide: The methemoglobin formation induced by 4-DMAP would additionally impair the oxygen-transporting capacity of the blood. In such cases, hydroxocobalamin can be used as an antidote (38– 40).
Poisonous animals
Poisoning by insect bites (e19) is common. Bites of the poisonous common European adder (Vipera berus L.) are rare and can in most cases be treated symptomatically, i.e., without antivenom.
Conclusion
Most intoxications can be treated symptomatically and with intensive-care measures as needed. Specific, effective measures directed against the particular offending substance can be used to treat only a small minority of patients. Poison information centers can help with therapeutic decision-making and planning in individual cases. These centers have extensive data on many types of products, offer advice, and can help organize suitable toxicological testing if necessary (e20). The ongoing collection of data by poison information centers is useful for the refinement of surveillance measures and also serves as a point of departure for research projects whose findings can be incorporated into future treatment recommendations.
Further information on CME.
This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education. Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire. See the following website: cme.aerzteblatt.de.
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
The present CME unit can be accessed until 12 January 2014.
The CME unit “Shortness of breath and cough in palliative-care patients”
(Issue 33-34/2013) can be accessed until 17 November 2013.
The CME unit “Degenerative lumbar spinal canal stenosis in the elderly”
(Issue 37/2013) can be accessed until 8 December 2013.
For Issue 45/2013, we plan to offer the topic “The febrile child: diagnosis and treatment.”
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What antidote inhibits alcohol dehydrogenase in the treatment of methanol and ethylene glycol poisoning?
fomepizole
thiamine
4-dimethylaminophenol (4-DMAP)
toluidine blue
hydroxocobalamin
Question 2
What is the usual adult dose of activated charcoal to lessen absorption?
3 tablets
5 g
10 g
0.5–1 g/kg body weight
2 g/kg body weight
Question 3
Which of the following substances is not adsorbed by activated charcoal in large amounts?
plant alkaloids
vitamin K antagonists in rodenticides
inorganic acids
tricyclic antidepressants
barbiturates
Question 4
Which of the following classes of drugs is commonly taken with suicidal intent?
protease inhibitors
tricyclic antidepressants
antihelminthic agents
hormones (glucocorticoids, contraceptives)
antibiotics
Question 5
In what type of poisoning should one consider giving a single dose of activated charcoal within one hour of the ingestion to lessen absorption?
tricyclic antidepressant overdose
swallowing of two yew seed cones
swallowing a small amount of common dishwashing detergent
swallowing a teaspoonful of hair gel
swallowing a containerful of ant bait whose active substance is a toxic organophosphate compound
Question 6
Which drugs can potentiate the effect of appetite suppressants?
benzodiazepines
selective serotonin reuptake inhibitors (SSRI)
calcium antagonists
antacids
cannabis
Question 7
What types of subtances, other than medical drugs, are most commonly involved in severe intoxications?
carbon monoxide, other gases, smoke
food and drinking water
pesticides and cleaning agents
methanol and ammonia
death-cap and webcap mushrooms
Question 8
How long after its ingestion is gamma-hydroxybutyric acid detectable in serum?
1–2 hours
2–4 hours
6–12 hours
24–48 hours
72–96 hours
Question 9
What means of reducing absorption is most commonly indicated?
gastric lavage
anterograde intestinal lavage
laxatives
activated charcoal
ipecac syrup
Question 10
Glucarpidase is indicated as an antidote for overdoses of what drug?
methotrexate
digitoxin
propofol
azathioprine
fluorouracil
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Dr. Desel has received payment for serving as a consultant for the International Association for Soaps, Detergents and Maintenance Products (AISE, Brussels) and an expert for the Henkel company. The Industrieverband Körperpflege und Waschmittel (German Personal Care Products and Detergents Industry Association, Frankfurt/Main) has sponsored a multicenter research project coordinated by the GIZ-Nord Poisons Center, managed by Dr. Desel.
Dr. Müller states that he has no conflict of interest.
References
- 1.Deutsche Hauptstelle für Suchtfragen e.V. Tabak. www.dhs.de/datenfakten/tabak.html. (last accessed on 8 July 2013)
- 2.Deutsche Hauptstelle für Suchtfragen e.V. Alkohol. www.dhs.de/datenfakten/alkohol.html. (last accessed on 8 July 2013)
- 3.Gesundheitsberichterstattung des Bundes. Sterbefälle, Sterbeziffern (from 1998) www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=38752000&nummer=6&p_sprache=D&p_indsp=-&p_aid=15523324. (last accessed on 8 July 2013)
- 4.DIMDI - ICD-10-GM. Version 2013. www.dimdi.de/static/de/klassi/icd-10-gm/kodesuche/onlinefassungen/htmlgm2013/block-t36-t50.htm. (last accessed on 8 July 2013)
- 5.Statistisches Bundesamt. www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Krankenhaeuser/TiefgegliederteDiagnosedaten. html (last accessed on 8 July 2013)
- 6.EUR-Lex - Official Journal - 1990 - C 329. eur-lex.europa.eu/JOHtml.do?uri=OJ:C:1990:329:SOM:EN:HTML. (last accessed on 8 July 2013)
- 7.Persson HE, Sjöberg GK, Haines JA, Pronczuk de Garbino J. Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36:205–213. doi: 10.3109/15563659809028940. [DOI] [PubMed] [Google Scholar]
- 8.Eyer F, Pfab R, Felgenhauer N, Strubel T, Saugel B, Zilker T. Clinical and analytical features of severe suicidal quetiapine overdoses—a retrospective cohort study. Clin Toxicol (Phila) 2011;49:846–853. doi: 10.3109/15563650.2011.624100. [DOI] [PubMed] [Google Scholar]
- 9.Schwabe U, Paffrath D. Berlin, Heidelberg: Springer; 2012. Arzneimittelverordnungs-Report 2012; 862 pp. [Google Scholar]
- 10.Ebbecke M, Schaper A, Kotseronis N. Hentschel H, Klöcking HP, et al., editors. „Nano-Epidemie“ 2006 - Toxikovigilanz deutscher Giftinformationszentren am Beispiel einer Epidemie von Vergiftungen, verursacht durch zwei neuartige Versiegelungssprays: Vergiftungsgefahren im Alltag. Erfurt: Acta Academiae Scientiarum. 2009:47–50. [Google Scholar]
- 11.Isbister GK, Kumar VV. Indications for single-dose activated charcoal administration in acute overdose. Current Opinion in Critical Care. 2011;17:351–357. doi: 10.1097/MCC.0b013e328348bf59. [DOI] [PubMed] [Google Scholar]
- 12.Benson BE, Hoppu K, Troutman WG, et al. Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol (Phila) 2013;51:140–146. doi: 10.3109/15563650.2013.770154. [DOI] [PubMed] [Google Scholar]
- 13.Höjer J, Troutman WG, Hoppu K, et al. Position paper update: ipecac syrup for gastrointestinal decontamination. Clin Toxicol (Phila) 2013;51:134–139. doi: 10.3109/15563650.2013.770153. [DOI] [PubMed] [Google Scholar]
- 14.Mühlendahl KE. Stuttgart, New York: Thieme; 2007. Vergiftungen im Kindesalter. [Google Scholar]
- 15.Klasco RK, editor. Truven Health Analytics, Greenwood Village. Colorado: Sodium Chloride (Management/Treatment Protocol)Poisindex® System. (Edition expires [03/2013]) [Google Scholar]
- 16.Position paper: whole bowel irrigation. J Toxicol Clin Toxicol. 2004;42:843–854. doi: 10.1081/clt-200035932. [DOI] [PubMed] [Google Scholar]
- 17.Positionc paper: athartics. J Toxicol Clin Toxicol. 2004;42:243–253. doi: 10.1081/clt-120039801. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. Position statement and practice guidelines on the use of multi-dose activated charcoal in the treatment of acute poisoning. J Toxicol Clin Toxicol. 1999;37:731–751. doi: 10.1081/clt-100102451. [DOI] [PubMed] [Google Scholar]
- 19.Skinner CG, Chang AS, Matthews AS, et al. Randomized controlled study on the use of multiple-dose activated charcoal in patients with supratherapeutic phenytoin levels. Clin Toxicol (Phila) 2012;50:764–769. doi: 10.3109/15563650.2012.716159. [DOI] [PubMed] [Google Scholar]
- 20.Roberts DM, Buckley NA. Enhanced elimination in acute barbiturate poisoning - a systematic review. Clin Toxicol (Phila) 2011;49:2–12. doi: 10.3109/15563650.2010.550582. [DOI] [PubMed] [Google Scholar]
- 21.Roberts DM, Buckley NA. Urinary alkalinisation for acute chlorophenoxy herbicide poisoning. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD005488.pub2. CD005488. [DOI] [PubMed] [Google Scholar]
- 22.Rifkin SI, McFarren C, Juvvadi R, Weinstein SS. Prolonged hemodialysis for severe metformin intoxication. Ren Fail. 2011;33:459–461. doi: 10.3109/0886022X.2011.568132. [DOI] [PubMed] [Google Scholar]
- 23.Desel H. Antidote - umfassende Liste. www.giz-nord.de/cms/index.php/informationen-zur-therapie-von-vergiftungen-/284-antidote-umfassende-liste-antidotes-comprehensive-list.html. (last accessed on 8 July 2013) [Google Scholar]
- 24.Schaper A, Bandemer G, Callies, et al. Vorhaltung von Antidota im Notarztdienst. Der Notarzt. 2012;28:114–148. [Google Scholar]
- 25.Levine MD, Boyer E. Hyperinsulinemia-euglycemia therapy: a useful tool in treating calcium channel blocker poisoning. Crit Care. 2006;10 doi: 10.1186/cc4964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Presley JD, Chyka PA. Intravenous lipid emulsion to reverse acute drug toxicity in pediatric patients. Ann Pharmacother. 2013;47:735–743. doi: 10.1345/aph.1R666. [DOI] [PubMed] [Google Scholar]
- 27.Woolf AD, Erdman AR, Nelson LS, et al. Tricyclic antidepressant poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila) 2007;45:203–233. doi: 10.1080/15563650701226192. [DOI] [PubMed] [Google Scholar]
- 28.Gibbons S. ’Legal highs’-novel and emerging psychoactive drugs: a chemical overview for the toxicologist. Clin Toxicol (Phila) 2012;50:15–24. doi: 10.3109/15563650.2011.645952. [DOI] [PubMed] [Google Scholar]
- 29.Carvalho M, Carmo H, Costa VM, et al. Toxicity of amphetamines: an update. Arch Toxicol. 2012;86:1167–1231. doi: 10.1007/s00204-012-0815-5. [DOI] [PubMed] [Google Scholar]
- 30.Coppola M, Mondola R. Synthetic cathinones: chemistry, pharmacology and toxicology of a new class of designer drugs of abuse marketed as “bath salts” or “plant food”. Toxicol Lett. 2012;211:144–149. doi: 10.1016/j.toxlet.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 31.Huffman JW, Szklennik PV, Almond A, et al. 1-Pentyl-3-phenylacetylindoles, a new class of cannabimimetic indoles. Bioorg Med Chem Lett. 2005;15:4110–4113. doi: 10.1016/j.bmcl.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Hermanns-Clausen M, Kneisel S, Szabo B, et al. Acute toxicity due to the confirmed consumption of synthetic cannabinoids: clinical and laboratory findings. Addiction. 2013;108:534–544. doi: 10.1111/j.1360-0443.2012.04078.x. [DOI] [PubMed] [Google Scholar]
- 33.Zimmermann US, Winkelmann PR, Pilhatsch M, et al. Withdrawal phenomena and dependence syndrome after the consumption of “spice gold”. Dtsch Arztebl Int. 2009;106(27):464–467. doi: 10.3238/arztebl.2009.0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.BMG. Die Drogenbeauftragte der Bundesregierung: Drogensuchtbericht 2012. http://drogenbeauftragte.de/fileadmin/dateien-dba/Presse/Downloads/12-05-22_DrogensuchtBericht_2012.pdf. (last accessed on 28 February 2013)
- 35.Madea B, Musshoff F. Knock-out drugs: their prevalence, modes of action, and means of detection. Dtsch Arztebl Int. 2009;106(20):341–347. doi: 10.3238/arztebl.2009.0341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bundesinstitut für Risikobewertung. Kohlenmonoxid. www.bfr.bund.de/de/a-z_index/kohlenmonoxid-30286.html. (last accessed on 8 July 2013)
- 37.Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD002041.pub3. CD002041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zilker T, Sefrin P, Scherer G, et al. Rauchgasinhalations-Intoxikation. Der Notarzt. 2010;26:95–102. [Google Scholar]
- 39.Desel H, Flemming A, Zilker T, et al. Ergänzende Stellungnahme zur Publikation „Rauchgasinhalations-Intoxikation - Ursachen, Primär- versorgung und Handlungsempfehlungen. Der Notarzt. 2010;27 [Google Scholar]
- 40.Kaiser G Research in Legal Medicine. (in press) Vol. 39. Lübeck: Schmidt-Römheld; 2013. Zyanwasserstoffintoxikationen durch Brandrauch. [Google Scholar]
- e1.Chyka PA, Seger D. Position statement: single-dose activated charcoal. American Academy of Clinical Toxicology. European Association of Poisons Centres and Clinical Toxicologists. J Toxicol Clin Toxicol. 1997;35:721–741. doi: 10.3109/15563659709162569. [DOI] [PubMed] [Google Scholar]
- e2.Chyka PA, Seger D, Krenzelok EP, Vale JA. American Academy of Clinical Toxicology. European Association of Poisons Centres and Clinical Toxicologists: Position paper: Single-dose activated charcoal. Clin Toxicol (Phila) 2005;43:61–87. doi: 10.1081/clt-200051867. [DOI] [PubMed] [Google Scholar]
- e3.Chyka PA. Multiple-dose activated charcoal and enhancement of systemic drug clearance: summary of studies in animals and human volunteers. J Toxicol Clin Toxicol. 1995;33:399–405. doi: 10.3109/15563659509013748. [DOI] [PubMed] [Google Scholar]
- e4.Krenzelok EP. New developments in the therapy of intoxications. Toxicol Lett. 2002;127:299–305. doi: 10.1016/s0378-4274(01)00512-4. [DOI] [PubMed] [Google Scholar]
- e5.Good AM, Kelly CA, Bateman DN. Differences in treatment advice for common poisons by poisons centres—an international comparison. Clin Toxicol (Phila) 2007;45:234–239. doi: 10.1080/15563650601031601. [DOI] [PubMed] [Google Scholar]
- e6.Vale JA, Kulig K. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists: Position paper: gastric lavage. J Toxicol Clin Toxicol. 2004;42:933–943. doi: 10.1081/clt-200045006. [DOI] [PubMed] [Google Scholar]
- e7.Buckley NA, Eddleston M. The revised position papers on gastric decontamination. Clin Toxicol (Phila) 2005;43:129–130. doi: 10.1081/clt-200050420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e8.Position paper: Ipecac syrup. J Toxicol Clin Toxicol. 2004;42:133–143. doi: 10.1081/clt-120037421. [DOI] [PubMed] [Google Scholar]
- e9.Türk EE, Schulz F, Koops E, Gehl A, Tsokos M. Fatal hypernatremia after using salt as an emetic—report of three autopsy cases. Leg Med (Tokyo) 2005;7:47–50. doi: 10.1016/j.legalmed.2004.06.005. [DOI] [PubMed] [Google Scholar]
- e10.Proudfoot AT, Krenzelok EP, Vale JA. Position Paper on urine alkalinization. J Toxicol Clin Toxicol. 2004;42:1–26. doi: 10.1081/clt-120028740. [DOI] [PubMed] [Google Scholar]
- e11.Brent J. Fomepizole for the treatment of pediatric ethylene and diethylene glycol, butoxyethanol, and methanol poisonings. Clin Toxicol (Phila) 2010;48:401–406. doi: 10.3109/15563650.2010.495347. [DOI] [PubMed] [Google Scholar]
- e12.Antidepressants tricyclic (Management/Treatment Protocol) Poisindex® System. In: Klasco RK, editor. Truven Health Analytics, Greenwood Village. Colorado: (Edition expires [03/2013]) [Google Scholar]
- e13.Schmidt MM, Sharma A, Schifano F, Feinmann C. “Legal highs” on the net-Evaluation of UK-based Websites, products and product information. Forensic Sci Int. 2011;206:92–97. doi: 10.1016/j.forsciint.2010.06.030. [DOI] [PubMed] [Google Scholar]
- e14.Celik S, Karapirli M, Kandemir E, et al. Fatal ethyl and methyl alcohol-related poisoning in Ankara: A retrospective analysis of 10,720 cases between 2001 and 2011. J Forensic Leg Med. 2013;20:151–154. doi: 10.1016/j.jflm.2012.05.009. [DOI] [PubMed] [Google Scholar]
- e15.Kruse JA. Methanol and ethylene glycol intoxication. Crit Care Clin. 2012;28:661–711. doi: 10.1016/j.ccc.2012.07.002. [DOI] [PubMed] [Google Scholar]
- e16.Brailsford AD, Cowan DA, Kicman AT. Pharmacokinetic properties of ?-hydroxybutyrate (GHB) in wholeblood, serum, and urine. J Anal Toxicol. 2012;36:88–95. doi: 10.1093/jat/bkr023. [DOI] [PubMed] [Google Scholar]
- e17.Centers for Disease Control. Workplace safety: Carbon Monoxide. www.cdc.gov/niosh/topics/co-comp/ (last accessed on 8 July 2013)
- e18.GIZ-Nord Fremdstoffexpositionen. http://helike.giz–nord.de/php/index.php?option=com_content&task=view&id=184&Itemid=85. (last accessed on 8 July 2013)
- e19.Przybilla B, Ruëff F. Insect stings: clinical features and management. Dtsch Arztebl Int. 2012;109(13):238–248. doi: 10.3238/arztebl.2012.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e20.Maurer HH. How can analytical diagnostics in clinical toxicology be successfully performed today? Ther Drug Monit. 2012;34:561–564. doi: 10.1097/FTD.0b013e31826a622d.. [DOI] [PubMed] [Google Scholar]