Abstract
In vitro, β-amyloid (Aβ) peptides form polymorphic fibrils, with molecular structures that depend on growth conditions, plus various oligomeric and protofibrillar aggregates. Detailed structural information about Aβ assemblies in the human brain has been lacking. Here, we investigate structures of brain-derived Aβ fibrils, using seeded fibril growth from brain extract and data from solid state nuclear magnetic resonance and electron microscopy. Experiments on tissue from two Alzheimer’s disease (AD) patients with distinct clinical histories indicate a single predominant 40-residue Aβ (Aβ40) fibril structure in each patient, but different structures in the two patients. A molecular structural model developed for Aβ40 fibrils from one patient reveals features that distinguish in vivo from in vitro fibrils. The data suggest that fibrils in the brain may spread from a single nucleation site, that structural variations may correlate with variations in AD, and that structure-specific amyloid imaging agents may be an important future goal.
Introduction
Aggregation of β-amyloid (Aβ) peptides in brain tissue is the likely cause of Alzheimer’s disease (AD) (Tanzi and Bertram, 2005; Yankner and Lu, 2009). The most abundant Aβ aggregates in AD brain tissue are amyloid fibrils, the end point of the aggregation process, which are contained in neuritic plaques, diffuse amyloid, and vascular amyloid. A variety of other aggregates have also been identified, including Aβ protofibrils and soluble oligomers of various sizes. In vitro structural studies, using solid state nuclear magnetic resonance (NMR) (Benzinger et al., 1998; Bertini et al., 2011; Lansbury et al., 1995; Paravastu et al., 2008; Petkova et al., 2005; Petkova et al., 2006; Qiang et al., 2011), electron microscopy (Goldsbury et al., 2005; Meinhardt et al., 2009; Zhang et al., 2009), and other techniques (Kheterpal et al., 2001; Kodali et al., 2010; Luhrs et al., 2005; Olofsson et al., 2007; Torok et al., 2002), show that Aβ fibrils are highly polymorphic, with molecular structures that depend on aggregation conditions. Detailed structural models for fibrils formed in vitro have been developed from experimental data, showing that fibril polymorphs can differ in specific aspects of peptide conformation and inter-residue interactions, as well as overall structural symmetry (Bertini et al., 2011; Luhrs et al., 2005; Paravastu et al., 2008; Petkova et al., 2006). Studies of certain non-fibrillar (Ahmed et al., 2010; Chimon et al., 2007; Lopez del Amo et al., 2012) and protofibrillar (Qiang et al., 2012; Scheidt et al., 2011) Aβ aggregates, also formed in vitro, provide evidence for peptide conformations similar to those in fibrils, but with reduced structural order and different supramolecular organizations.
Molecular structures of Aβ aggregates that develop in human brain tissue have not been characterized in detail, but evidence exists that structural variations may be biomedically important: (i) Structurally distinct fibrils can have different levels of toxicity in neuronal cell cultures (Petkova et al., 2005); (ii) Propagation of exogenous Aβ amyloid within transgenic mouse brains depends on the source of the exogenous Aβ-containing material (Langer et al., 2011; Meyer-Luehmann et al., 2006; Stohr et al., 2012); (iii) The binding stoichiometry of amyloid imaging agents, developed for positron emission tomography (PET), can differ substantially between Aβ fibrils formed in vitro and fibrils in AD brain tissue (Mathis et al., 2003). A precedent for the importance of molecular structural variations in a neurodegenerative disease is provided by transmissible spongiform encephalopathies (TSEs), in which variations in the molecular structures of mammalian prion protein (PrP) aggregates within brain tissue produce distinct, self-propagating TSE “strains” (Bessen and Marsh, 1994; Safar et al., 1998; Stohr et al., 2012). Analogous variations in the molecular structures of yeast prion fibrils produce prion strains in yeast (Toyama and Weissman, 2011).
Solid state NMR has been an especially powerful structural probe of Aβ aggregates formed in vitro (Ahmed et al., 2010; Benzinger et al., 1998; Bertini et al., 2011; Chimon et al., 2007; Lansbury et al., 1995; Lopez del Amo et al., 2012; Paravastu et al., 2008; Petkova et al., 2005; Petkova et al., 2006; Qiang et al., 2012; Qiang et al., 2011; Scheidt et al., 2011). Since solid state NMR measurements require milligram-scale quantities of 15N- and 13C-labeled fibrils, direct measurements on Aβ aggregates from brain tissue are not possible. However, in vitro studies show that Aβ fibrils grown from seeds (i.e., short fibril fragments, produced by sonication of existing fibrils) retain the molecular structures of the seeds (Kodali et al., 2010; Paravastu et al., 2008; Petkova et al., 2005). Thus, if amyloid-containing material is extracted from brain tissue and used as the source of seeds, seeded fibril growth can be used to amplify and label structures that develop in the human brain (Paravastu et al., 2009).
In this paper, we describe studies of fibril structures from brain tissue of two AD patients (patients I and II) with distinct clinical histories and neuropathology, using simplified amyloid extraction and seeding protocols. Solid state NMR and electron microscopy measurements on 40-residue Aβ (Aβ40) fibrils seeded with extract from two brain regions of patient I and three brain regions of patient II indicate that each patient developed a single predominant fibril structure. However, the predominant structures from the two patients are clearly different, as indicated by both NMR chemical shifts and fibril morphologies in electron microscopy. We develop a full molecular structural model for Aβ40 fibrils from patient I, which represents the first detailed, experimentally-determined structure of any brain-derived Aβ aggregate.
Given that Aβ aggregation is inherently polymorphic, the structural specificity of brain-seeded Aβ40 fibrils indicated by our data is remarkable. Possible implications for processes by which fibrils develop within the human brain, for the role of Aβ fibrils and the significance of their structures in AD, and for future developments of structure-specific imaging agents and aggregation inhibitors are discussed below.
Results
A single predominant Aβ40 fibril structure from patient I
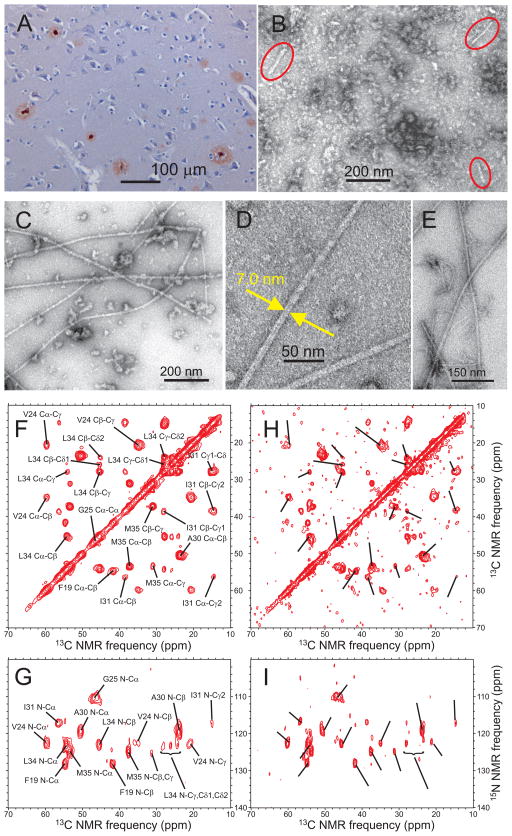
Patient I, a female who died at age 72, had tentative clinical diagnoses of Lewy body dementia (LBD) and primary progressive aphasia. Autopsy revealed neuritic Aβ plaques, diffuse amyloid, neurofibrillary tangles, and mild atrophy of frontal and parietal lobes indicative of AD, but few Lewy bodies. Starting with 1 g of tissue that contains abundant plaques (Fig. 1A), our amyloid extraction protocol (see Extended Experimental Methods) produced approximately 10 mg of amyloid-enriched material. Fibril fragments in this material were visible by transmission electron microscopy (TEM) (Fig. 1B). After addition of 0.8 mg of synthetic 15N,13C-labeled Aβ40, long fibrils developed within several hours (Fig. 1C, D). The fibrils have constant apparent diameters of 7 ± 1 nm, do not self-associate into thicker bundles, and appear morphologically homogeneous. Fibrils seeded with extract from occipital lobe tissue (Fig. 1C, D) are indistinguishable from fibrils seeded with extract from temporal/parietal lobe tissue (Fig. 1E). Brain-seeded fibrils from patient I are morphologically distinct from “striated ribbon” and “twisted” Aβ40 fibrils grown in vitro (without brain material) in our laboratory (Paravastu et al., 2008), as well as in vitro fibrils described by others (Goldsbury et al., 2005; Kodali et al., 2010; Meinhardt et al., 2009).
Fig. 1.
Evidence for a single predominant Aβ40 fibril structure in brain tissue of patient I. (A) Light microscope image of cortical tissue from patient I, with immunohistochemical staining for β-amyloid using monoclonal antibody 6E10. Amyloid deposits are red or pink. (B) Negatively stained TEM image of extract from occipital lobe tissue before addition of monomeric Aβ40. Fibril fragments are circled in red. (C, D) TEM images of isotopically labeled Aβ40 fibrils, recorded 24 hr after addition of monomeric Aβ40 to sonicated extract from occipital lobe tissue. Aβ40 was uniformly 15N,13C-labeled at F19, V24, G25, A30, I31, L34, and M35. (E) TEM image of fibrils prepared by seeding with sonicated extract from temporal/parietal lobe tissue. (F, G) 2D 13C-13C and 15N-13C solid state NMR spectra of Aβ40 fibrils, seeded with extract from occipital lobe tissue. Black lines and labels show site-specific crosspeak assignments. (H, I) 2D 13C-13C and 15N-13C solid state NMR spectra of Aβ40 fibrils, seeded with extract from temporal/parietal lobe tissue, with the same black lines as in panels F and H. See also Figs. S1 and S2.
Control experiments, detected by thioflavin T fluorescence and by TEM, showed rapid fibril growth when brain tissue from AD patients was used, but not when identical experiments were performed with non-AD tissue (Fig. S1). Thus, seeding of fibril growth is attributable to fibrils in the AD brain tissue, not to other components of brain tissue that survive the extraction protocol. Compared with protocols described previously (Paravastu et al., 2009), our current protocols involve fewer extraction steps, preserve more components of the brain tissue, and permit NMR samples to be created in a single seeding step from smaller quantities of tissue.
Two-dimensional (2D) solid state NMR spectra of Aβ40 fibrils seeded with extract of occipital lobe tissue (Fig. 1F, G) show remarkably sharp crosspeak signals, with a single set of 15N and 13C NMR chemical shifts for each 15N,13C-labeled residue (0.7–1.2 ppm and 1.3–1.8 ppm FWHM linewidths for 13C and 15N signals, respectively). Since chemical shifts are exquisitely sensitive to molecular structural variations, the observation of a single set of shifts implies a single predominant fibril structure, consistent with the morphological homogeneity in TEM images. 2D spectra of fibrils seeded with extract of temporal/parietal lobe tissue (Fig. 1H, I; Fig. S2F) are nearly identical, apart from differences in signal-to-noise ratio due to differences in sample sizes. Chemical shifts in spectra of these brain-seeded fibrils are significantly different from shifts reported previously for fibrils grown in vitro (Bertini et al., 2011; Paravastu et al., 2008; Petkova et al., 2005). The high signal-to-noise ratio in Fig. 1F allows us to place an upper limit of 10% on the mass of minor structural components relative to the predominant fibril structure in the occipital-seeded sample.
Different Aβ40 fibril structures from brain tissue of patients I and II
Patient II, a female who died at age 80, had a clinical diagnosis of probable AD. Autopsy revealed severe AD, including gross atrophy of the brain, loss of neurons, gliosis in the hippocampus and cortex, neurons with granulovacuolar degeneration and Hirano bodies, neuritic plaques, and neurofibrillary tangles. Brain-seeded Aβ40 fibrils prepared from occipital lobe (Fig. 2A, B) and frontal lobe (Fig. 2C) tissue of patient II show an apparent periodic twist in TEM images (minima and maxima in apparent width approximately equal to 11 nm and 5 nm; 85 ± 10 nm distance between minima) that is absent from images of fibrils from patient I (Fig. 1C–E). Solid state NMR spectra again show a single set of chemical shifts, indicating a single predominant fibril structure that is the same in samples seeded with occipital lobe, frontal lobe, or temporal lobe tissue (Fig. 2D–G; Fig. S2G, H) However, chemical shifts for brain-seeded fibrils from patients I and II are obviously different (Fig. 2D, E). Signals with the chemical shifts of fibrils from patient I are undetectable in spectra of fibrils from patient II, and vice versa. These data indicate that patients I and II developed structurally distinct fibrils in their brains.
Fig. 2.
Evidence for different Aβ40 fibril structures in brain tissue of patients I and II. (A, B) TEM images of Aβ40 fibrils, recorded 36 hr after addition of monomeric Aβ40 to sonicated extract from occipital lobe tissue of patient II. Blue arrows indicate minima in the apparent fibril diameter, associated with a periodic twist that is absent from fibril images in Fig. 1. Aβ40 was uniformly 15N,13C-labeled at F19, V24, G25, S26, A30, I31, L34, and M35. (C) TEM image of fibrils prepared by seeding with sonicated extract from frontal lobe tissue of patient II. (D, E) 2D 13C-13C and 15N-13C solid state NMR spectra of Aβ40 fibrils, seeded with extract from occipital lobe tissue of patient II (blue contours) or patient I (red contours). Black lines and labels show site-specific crosspeak assignments for spectra from patient II. (F, G) 2D 13C-13C and 15N-13C solid state NMR spectra of Aβ40 fibrils, seeded with extract from frontal lobe tissue of patient II, with the same black lines as in panels D and E. See also Figs. S2 and S6.
From the 2D spectrum in Fig. 2D, the mass of any minor structural components must be less than 10% relative to the predominant fibril structure. Although the twisted morphology in TEM images of fibrils derived from brain tissue of patient II is similar to the morphology of certain Aβ40 fibrils grown in vitro (Paravastu et al., 2008), the NMR chemical shifts are significantly different (Fig. S6).
Structural model for Aβ40 fibrils from patient I
The high quality of 2D solid state NMR spectra of Aβ40 fibrils derived from brain tissue of patient I encouraged us to pursue a full molecular structure determination. We prepared fibril samples with a variety of isotopic labeling patterns (Table 1). A uniformly 15N,13C-labeled sample (sample A) was generated by seeding recombinant Aβ40 with extract from occipital lobe tissue. Samples with other labeling patterns (samples C–G) were generated by seeding synthetic Aβ40 with aliquots of samples whose spectra appear in Fig. 1 (sample B). NMR chemical shifts are consistent in 2D spectra of all samples (Figs. 3 and S2), indicating that all samples contained the same fibril structure.
Table 1.
Summary of isotopic labeling patterns and solid state NMR measurements on Aβ40 fibrils derived from patient I.
| sample | uniformly 15N,13C-labeled residues | selectively 13C-labeled sites | NMR measurements1 |
|---|---|---|---|
| A | residues 1-40 | 2D fpRFDR, NCAX, NCOCX, RAD, PAR, and TEDOR; 3D NCACX and NCOCX; 15N- and 13C-BARE | |
| B | F19, V24, G25, A30, I31, L34, M35 | 2D fpRFDR, RAD, NCACX | |
| C | F20, D23, V24, K28, G29, A30, I31 | 2D fpRFDR, RAD, NCACX; fsREDOR | |
| D | H14, Q15, A21, V36, G37 | 2D fpRFDR, RAD, NCACX; 15N- and 13C-BARE | |
| E | K16, F19, A21, E22, I32, V36 | 2D fpRFDR, RAD, NCACX; 15N- and 13C-BARE | |
| F | A2 and A21 methyl; V12, F20, I31, G38 carbonyl | PITHIRDS-CT | |
| G | A30 methyl, V18 carbonyl | PITHIRDS-CT |
Definitions of acronyms: fpRFDR = finite-pulse radio-frequency-driven recoupling; NCACX = 15N-13Cα-13Cx chemical shift correlation; NCOCX = 15N-13CO-13Cx chemical shift correlation; RAD = radio-frequency-assisted diffusion; PAR = proton-assisted recoupling; TEDOR = transferred echo double resonance; BARE = backbone recoupling; fsREDOR = frequency-selective rotational echo double resonance; PITHIRDS-CT = constant-time π-pulse recoupling
Fig. 3.
The entire Aβ40 sequence is structurally ordered in fibrils from patient I. (A, B) 2D solid state 15N-13C NMR spectra of uniformly 15N,13C-labeled Aβ40 fibrils. Panel A is a NCACX spectrum, correlating backbone 15N chemical shifts of a given residue with 13C chemical shifts of the same residue. Panel B is a NCOCX spectrum, correlating backbone 15N chemical shifts of a given residue with 13C chemical shifts of the previous residue. Only the aliphatic 13C regions are shown. Asterisks in panel B denote intra-residue crosspeaks and crosspeaks involving sidechain 15N signals. (C) 2D 13C-13C spectrum, obtained with 50 ms RAD mixing (left) and 2.94 ms fpRFDR mixing (right). Black labels indicate CO/Cα (left) and Cα/Cβ (right) crosspeaks. Blue labels indicate additional intra-residue crosspeaks, including multiple-bond crosspeaks. Site-specific crosspeak assignments in these 2D spectra show that residues 1–40 contribute relatively strong, sharp signals, implying structural order. See also Table S1.
From 2D and 3D NMR spectra, we obtained unique assignments of all 15N and 13C chemical shifts (Table S1). As shown in Fig. 3, all residues in the Aβ40 sequence contribute strong and sharp signals to the solid state NMR spectra, except H14 and E22. Since dynamically disordered segments of a protein assembly are generally absent from such solid state NMR spectra and statically disordered segments yield broad signals, it appears that the entire Aβ40 sequence participates in the ordered and relatively rigid molecular structure.
We obtained structural restraints from a combination of solid state NMR and electron microscopy measurements. Structural restraints from solid state NMR, summarized in Table S2, include: (i) Conformation-dependent 13C and 15N chemical shifts (Fig. 4A), from which backbone torsion angle predictions (Table S1) were derived using the TALOS+ program (Shen et al., 2009); (ii) Intermolecular 13C-13C magnetic dipole-dipole couplings, measured with the PITHIRDS-CT technique (Tycko, 2007), which imply an in-register parallel β-sheet structure (Fig. 4B); (iii) 15N-13C dipole-dipole couplings between K28 Nε and D23 Cγ sites, measured with the fsREDOR technique (Jaroniec et al., 2001), which indicate a 0.35 ± 0.02 nm distance, consistent with a D23-K28 salt bridge (Fig. 4C). (iv) Intramolecular dipole-dipole couplings among backbone amide 15N nuclei and among backbone carbonyl 13C nuclei, measured with the 15N-BARE and 13C-BARE techniques (Hu et al., 2012), which serve as site-specific restraints on backbone conformation (Figs. 4D and S3); (v) Inter-residue distance restraints from 2D RAD (Morcombe et al., 2004; Takegoshi et al., 2001), PAR (De Paepe et al., 2008), band-selective fpRFDR (Bayro et al., 2009; Ishii, 2001), and band-selective TEDOR (Jaroniec et al., 2002) spectra (Fig. S4 and Table S3).
Fig. 4.
Structural restraints on Aβ40 fibrils from patient I. (A) Residue-specific secondary 13C NMR chemical shifts. Non-glycine residues with positive values for Cβ and negative values for CO and Cα are likely to have β-strand conformations. Open symbols indicate glycine residues. (B) Intermolecular 13C-13C dipole-dipole couplings among 13C-labeled methyl sites of A2 or A21 or 13C-labeled carbonyl sites of V12, F20, I31, or G38. Comparison with simulations for linear chains of 13C nuclei with various spacings indicates intermolecular distances of approximately 0.5 nm for all labeled sites, implying in-register parallel β-sheets. (C) 15N-13C dipole-dipole couplings between D23 Cγ and K28 Nζ sites indicate a 0.35 ± 0.02 nm interatomic distance, implying salt-bridge interactions between oppositely charged D23 and K28 sidechains. (D) 15N-15N dipole-dipole couplings among backbone amide nitrogens. Stronger couplings for F20 and A21 indicate non-β-strand conformations. (E) Dark-field TEM image of unstained fibrils. Mass-per-length (MPL) values are obtained from integrated intensities within 300 nm X 50 nm rectangles, centered on TMV (cyan) or Aβ40 (yellow) fibril segments, after subtraction of the average background intensity from similar rectangles on either side (dotted lines). TMV particles serve as in situ MPL standards. (F) MPL histogram, with light blue dashed lines indicating MPL values expected for structures comprised of 1–5 cross-β units. Dark blue line is a best-fit Gaussian function, centered at 28.4 ± 0.3 kDa/nm and with a full-width-at-half-maximum (FWHM) equal to 12.0 ± 0.8 kDa/nm. (G) Histogram of errors in MPL values due to noise in the dark-field images. The best-fit Gaussian function has FWHM equal to 12.8 ± 0.6 kDa/nm, showing that random noise accounts for the width in panel F. (H) MPL histogram for Aβ40 fibrils seeded with extract from occipital lobe tissue of patient II, with best-fit Gaussian function centered at 29.1 ± 1.2 kDa/nm and FWHM equal to 12.1 ± 0.8 kDa/nm. See also Fig. S3 and Table S2.
Dark-field TEM images of unstained samples (Fig. 4E) allow quantification of the mass-per-length (MPL) of individual fibrils (Chen et al., 2009; Goldsbury et al., 2005). Given that amyloid fibrils contain cross-β structural motifs with a 0.47–0.48 nm intermolecular distance along the fibril axis (supported by Fig. 4B) and that the molecular weight of Aβ40 is 4.3 kDa, a single cross-β unit would have MPL ≈ 9.0 kDa/nm. The observed MPL value of 28 ± 2 kDa/nm (Fig. 4F), together with the observation of a single set of NMR chemical shifts for all residues, implies a molecular structure comprised of three cross-β units, with three-fold symmetry about the long fibril axis.
Structure calculations were performed with the Xplor-NIH program (Schwieters et al., 2006), starting from nine well-separated Aβ40 molecules with random conformations. In addition to distance and conformational restraints from the NMR data, rotational and translational symmetry restraints were applied, as dictated by the MPL data, the solid state NMR spectra, and the fibrillar nature of the Aβ40 assemblies. Low-energy final structures consist of three copies of a three-fold-symmetric repeat unit, with translational symmetry along the fibril axis.
Fig. 5A shows the repeat unit from the final structure with the lowest total restraint energy. Repeat units from 20 low-energy structures (PDB code 2M4J) are superimposed in Fig. 5B. This bundle of structures represents the full range of final structures that are fully consistent with the experimental data, defined by the absence of violations of backbone torsion angle predictions exceeding 7°, the absence of violations of distance restraints exceeding 0.06 nm, and good agreement with the 15N- and 13C-BARE data (Fig. S3). Structure calculation statistics appear in Table S4. Figs. 5C and 5D show an idealized representation of the full fibril structure. Attempts to calculate structures with two-fold rotational symmetry, using the same set of experimental restraints and the same Xplor-NIH protocols, produced no final structures that were fully consistent with the experimental data.
Fig. 5.
Molecular structure of Aβ40 fibrils from patient I. (A) Structure with the lowest total experimental restraint energy in Xplor-NIH calculations. The three-fold-symmetric repeat unit is shown, as viewed along the fibril growth axis. Backbone and sidechain carbon atoms are grey and green, respectively. (B) Superposition of 20 structures that are consistent with experimental restraints (PDB code 2M4J). Sidechains of the three Aβ40 molecules in the repeat unit are yellow, green, or orange. (C, D) Two views of the idealized fibril structure, created by repeating the trimeric unit 18 times with 0.48 nm displacements along the fibril axis. (E, F) Structural models for Aβ40 fibril polymorphs with three-fold and two-fold symmetry about the fibril growth axis, developed previously from solid state NMR and electron microscopy measurements on fibrils grown in vitro. Repeat units from these models are shown, calculated as regularized averages of structure bundles in PDB codes 2LMP and 2LMN, respectively. See also Figs. S4 and S6 and Tables S3 and S4.
Key distance restraints for the bundle of structures in Fig. 5B include intramolecular V24-K28, K28-I31, E11-V39, M35-G38, M35-V39, M35-V40, F19-L34, and H13-V39 distances, as well as intermolecular F4-V24, R5-V24, D7-S26, S8-V24, A30-V40, and I32-V39 distances (see Fig. S4 and Table S3). I31-V39, H13-V40, L17-I32, and F19-I32 contacts, observed in three-fold-symmetric fibrils formed in vitro (Paravastu et al., 2008), are not present in Aβ40 fibrils from patient I.
Further support for the structure in Fig. 5 comes from two additional experiments. First, we used 2D 15N-13C solid state NMR spectra to monitor site-specific hydrogen/deuterium (H/D) exchange rates during exposure of sample A to D2O buffer (Fig. 6). Only backbone amide sites of A2, F4, D7, S8, G9, G25, and S26, which are co-localized in the structure, exhibited significant H/D exchange over an 18 day period. These results suggest that the N-terminal segment undergoes transient unfolding events that also expose G25 and S26. (Continual large-amplitude motions are ruled out by NMR signal strengths and dipole-dipole couplings in Figs. 3, 4B, and S3.) Second, we measured site-specific enhancements of 15N spin-lattice relaxation rates induced by paramagnetic CuNa2-EDTA (Fig. S5). The smallest relaxation enhancements were observed for residues 30–40, consistent with their burial in the fibril core and with a narrow central pore that excludes the Cu-EDTA complex.
Fig. 6.
H/D exchange measurements on Aβ40 fibrils derived from occipital lobe tissue of patient I, detected through 2D 15N-13C solid state NMR spectra. (A) 2D NCA spectra of uniformly 15N,13C-labeled fibrils, before H/D exchange, after various periods of exchange, and after back-exchange. In all spectra, the highest contour level is normalized to the strongest crosspeak, and 16 contour levels are shown, decreasing by successive factors of 1.2. In the spectrum at 426–437 hr, arrows indicate positions of resolved or partially resolved crosspeaks that show clear reductions in intensity due to H/D exchange. (B) 2D NCACX spectra after various periods of exchange and after back-exchange, with contour levels as in panel A. (C) Structure from Fig. 5A with residues that exhibit significant H/D exchange colored magenta. See also Fig. S5.
Comparison with in vitro fibril structures
In-register parallel intermolecular alignment (Fig. 5C, D) also occurs in full-length Aβ fibrils formed in vitro without brain material (Benzinger et al., 1998; Luhrs et al., 2005; Paravastu et al., 2008; Petkova et al., 2005; Torok et al., 2002), although metastable intermediates (Qiang et al., 2012) and fibrils formed by certain Aβ fragments (Colletier et al., 2011; Lansbury et al., 1995) can contain antiparallel cross-β motifs. Three-fold symmetry occurs in certain in vitro Aβ40 fibrils with “twisted” morphologies (Goldsbury et al., 2005; Paravastu et al., 2008). (Fig. 5E), while other in vitro Aβ40 and Aβ42 fibrils exhibit two-fold symmetry (Bertini et al., 2011; Meinhardt et al., 2009; Petkova et al., 2006; Zhang et al., 2009) (Fig. 5F). D23–K28 salt bridge interactions have been observed in two-fold-symmetric (Petkova et al., 2006), but not three-fold-symmetric (Paravastu et al., 2008), Aβ40 fibrils formed in vitro. Residues 12–19 form a β-strand in all known Aβ40 structures, with sidechains of even-numbered residues exposed on the exterior surface, while residues 30–40 are buried in the fibril core. Close contacts between F19 and L34 sidechains occur in both in vitro Aβ40 (Bertini et al., 2011; Paravastu et al., 2008; Petkova et al., 2006) and in vitro Aβ42 (Ahmed et al., 2010) fibrils.
Novel conformational features in Aβ40 fibrils from patient I may provide a basis for the development of structure-specific inhibitors or imaging agents. These features include a twist in residues 19–23 that allows sidechains of either F20 or E22 to be buried within the structure, a kink at G33 that allows sidechains of I32 and L34 to point in opposite directions and make contacts with different sets of Aβ40 molecules, and a bend in glycine residues 37 and 38. In contrast, fibrils formed in vitro by Aβ40 and Aβ42 contain relatively simple strand-bend-strand conformations, as in Fig. 5E, F. A variety of experiments indicate N-terminal disorder in in vitro Aβ40 and Aβ42 fibrils (Kheterpal et al., 2001; Luhrs et al., 2005; Paravastu et al., 2008; Petkova et al., 2005). However, Aβ40 fibrils from patient I exhibit strong, sharp NMR signals (Fig. 3) and strong 13C-13C and 15N-15N dipole-dipole couplings for N-terminal residues (Figs. 4B and S3), indicating structural order.
MPL data for Aβ40 fibrils from patient II also indicate three-fold symmetry (Fig. 4H). F19–L34 sidechain contacts, which are clear in spectra of samples A and B from patient I (Fig. S4C), are not detected in fibrils from patient II. From chemical shifts (Fig. S6), TALOS+ predicts a continuous β-strand in residues 28–32 in fibrils from patient II, while structures in Fig. 5B have a non-β-strand conformation at G29. Thus, fibrils from patients I and II differ in both peptide backbone conformation and inter-residue interactions, but not overall symmetry.
Discussion
Significance of structural observations
Polymorphism is an inherent property of Aβ fibril formation (Colletier et al., 2011; Goldsbury et al., 2005; Kodali et al., 2010; Meinhardt et al., 2009; Paravastu et al., 2008; Petkova et al., 2005; Qiang et al., 2011), attributable to the coexistence of multiple nucleation processes (each leading to a different fibril structure), the comparably high thermodynamic stabilities of distinct polymorphs, and the low rates of dissociation of peptide monomers or soluble species from fibrils (Qiang et al., 2013). It is therefore surprising that Aβ40 fibrils derived from brain tissue of either patient I or patient II are not polymorphic. Possible explanations include: (i) The brain tissue environment permits only one nucleation process. The observation of distinct fibril structures from patients I and II contradicts this explanation unless unknown differences in their brain tissue selected different nucleation processes; (ii) Multiple fibril structures are nucleated, and all but one are eliminated by amyloid clearance mechanisms. Unknown differences in clearance mechanisms between patients I and II would be required to account for our data; (iii) The majority of fibrils that persist to the time of death arise from nucleation of one structure at a single site. This structure then spreads by physical or biologically-mediated processes of fragmentation and transport, possibly involving activated microglia (Majumdar et al., 2008). After transport to a new site, fibril fragments serve as seeds for the growth of structurally identical fibrils (Langer et al., 2011), as in the experiments described above. In this scenario, differences between patients I and II may be due entirely to the stochastic nature of the initial nucleation event.
Patients I and II differed in clinical history (initial diagnoses of LBD vs. AD) and neuropathology (mild vs. severe cortical atrophy), although both patients developed Aβ plaques and neurofibrillary tangles characteristic of AD. The observation of distinct Aβ40 fibril structures from the two patients, both in TEM images and in solid state NMR spectra, suggests that differences in fibril structure may correlate with differences in disease development. The analogy with TSE strains, in which self-propagating polymorphisms of PrP aggregates lead to distinct anatomical patterns of PrP deposition, disease incubation periods, and symptoms (Bessen and Marsh, 1994; Collinge, 2001; Safar et al., 1998), is obvious. Prior suggestive evidence for AD strains includes the observation of polymorph-specific differences in Aβ40 fibril toxicity in neuronal cell cultures (Petkova et al., 2005) and the observation that propagation efficiencies of exogenous Aβ42 fibrils in transgenic mice depend on the source of the exogeneous material (Meyer-Luehmann et al., 2006; Stohr et al., 2012). Further experiments are certainly required before AD strains can be considered a reality.
Role of fibrils in AD
Both the identity of Aβ aggregates that contribute most to neurodegeneration in AD and their pathogenic mechanisms are currently uncertain (Yankner and Lu, 2009). Various experiments point to non-fibrillar Aβ oligomers as neurotoxic species (Krafft and Klein, 2010; Lesne et al., 2006; Noguchi et al., 2009; Selkoe, 2008). Ongoing fibril growth or conversion of oligomers to fibrils may be required for neurotoxicity (Jan et al., 2011). Although mature amyloid fibrils are sometimes described as being non-toxic in cell cultures, experiments by us (Petkova et al., 2005; Qiang et al., 2012) and others (Chimon et al., 2007; Walsh et al., 1999) show that Aβ40 fibrils are indeed toxic in cell cultures. In brain tissue, Aβ fibrils may initiate inflammation (Cameron and Landreth, 2010; Glass et al., 2010), oxidative damage (Sultana et al., 2009; Tougu et al., 2011), or other pathogenic processes.
The severity of cognitive impairment in AD patients prior to death has been reported not to correlate with plaque density (Giannakopoulos et al., 1997). At least one study reached the opposite conclusion (Cummings et al., 1996); the quantity of brain amyloid has been found to correlate with the likelihood of progression from mild cognitive impairment to AD (Villemagne et al., 2011). Although asymptomatic elderly people develop amyloid plaques, the quantity of amyloid is generally less than in AD patients (Aizenstein et al., 2008). Fibrillar oligomers (which may be fibril fragments), but not non-fibrillar oligomers, have been reported to be elevated in AD patients (Tomic et al., 2009).
Thus, Aβ fibrils (along with oligomeric and protofibrillar species) remain as likely causative or contributing agents in AD. Our finding of specific fibril structures in AD patients suggests that certain structures may be more pathogenic than others. The weakness of correlations between total amyloid deposition and cognitive deficiency in AD patients may be due in part to differential effects of amyloid deposits comprised of different fibril structures. Similarly, amyloid deposits in brain tissue of asymptomatic elderly people may contain relatively inert structures. It is also conceivable that specific fibril structures coexist with specific oligomer structures, for example if the oligomers are “on-pathway” intermediates to fibril formation, or if the oligomers are produced by degradation of fibrils. Association of specific Aβ fibrils with AD may then arise indirectly, through their association with specific oligomers. Structural data for fibrils may then represent a window into the properties of oligomers, whose molecular structures are particularly challenging to characterize directly. Further experiments are required to test these possibilities.
Aβ40 and Aβ42
The 42-residue form of Aβ (Aβ42) is often considered particularly important in AD, because of its more rapid aggregation kinetics in vitro (Bitan et al., 2003; Jarrett et al., 1993), elevated levels in patients with some disease-associated mutations (Scheuner et al., 1996), and elevated levels in AD brain tissue (Kuo et al., 1996). However, depending on experimental conditions, differences in aggregation kinetics in vitro are not large. Aβ40 levels in humans are still roughly five-fold larger than Aβ42 levels, even with disease-associated mutations. Direct assessment of Aβ40/Aβ42 ratios in Aβ aggregates within brain tissue depends on monoclonal antibodies that recognize C-terminal epitopes (Iwatsubo et al., 1994). For Aβ40 fibrils with the structure in Fig. 5A, the C-terminus is not accessible to antibodies, suggesting that such assessments may not be reliable. Measurements on AD brain extract, after dissolution in formic acid, show a wide range of Aβ40/Aβ42 ratios (Gravina et al., 1995).
In our hands, polymorphic Aβ42 fibrils prepared in vitro do not seed the growth of Aβ40 fibrils. Therefore, our brain-seeded Aβ40 fibrils most likely arise from Aβ40 fibrils (not Aβ42 fibrils) in the brain tissue of patients I and II.
Implications for imaging agents and inhibitors
In vivo imaging of Aβ amyloid by positron emission tomography, based on compounds that bind preferentially to Aβ fibrils (Clark et al., 2011; Klunk et al., 2004), has become an important tool in AD research and diagnosis. Existing imaging agents were developed without detailed molecular structural information for fibrils that develop in brain tissue. Specific structural differences between brain-seeded and in vitro fibrils identified above may facilitate the development of imaging agents with improved specificity and structural selectivity.
Significant efforts have also been devoted to the development of inhibitors of Aβ aggregation, including both small-molecule (Yang et al., 2005) and peptide-based (Gordon et al., 2001) inhibitors. Compounds that inhibit formation of the specific Aβ structures that develop in AD brain tissue may be particularly valuable in AD prevention or treatment.
Experimental Methods
Amyloid extraction and seeding
Amyloid-enriched extract was produced by subjecting brain tissue to homogenization, ultracentrifugation in 1.2 M and 1.9 M sucrose, DNAse I digestion, and a brief treatment with 1% sodium dodecyl sulfate to remove residual lipids. After washing, this material was pelleted and stored at −20° C. Fibrils were grown at 24° C by adding synthetic or recombinant Aβ40, solubilized in dimethyl sulfoxide, to a 5 mg/ml suspension of sonicated brain extract in 10 mM phosphate buffer, pH 7.4, with a final Aβ40 concentration of 100 μM. For solid state NMR, fibrils (embedded in brain extract) were pelleted, lyophilized, packed into magic-angle spinning (MAS) rotors, and rehydrated by addition of H2O. Full details are given in Extended Experimental Methods.
Solid state NMR and electron microscopy
NMR measurements were performed at magnetic field strengths of 9.4 T, 14.1 T, and 17.5 T using Varian Infinity and InfinityPlus spectrometers and triple-resonance MAS probes from the group of Dr. Ago Samoson (Tallinn University of Technology, Estonia) and from Varian. Full details are given in Extended Experimental Methods and Table S2.
TEM images of negatively stained and unstained samples were obtained with an FEI Morgagni microscope, operating at 80 keV. Dark-field images for MPL determination were obtained and analyzed as described previously (Chen et al., 2009).
Structure calculations
Three stages of simulated annealing within Xplor-NIH were used to arrive at final structures that satisfy all experimental restraints, consisting of 15 distance restraints per molecule from PITHIRDS-CT, fsREDOR, 15N-BARE, and 13C-BARE data, 60 torsion angle restraints per molecule from TALOS+ predictions, 50 torsion angle potential surfaces per molecule from 15N-BARE and 13C-BARE data, and 72 inter-residue distance restraints per molecule from 2D PAR, RAD, band-selective fpRFDR, and TEDOR spectra. Full details are given in Extended Experimental Methods and Table S4.
Supplementary Material
Research Highlights.
detailed study of molecular structures of β-amyloid aggregates in the human brain
one predominant β-amyloid fibril structure in brain tissue of each AD patient
two distinct fibril structures from two AD patients with distinct clinical histories
full structure of brain-derived fibrils reveals differences from in vitro fibrils
Acknowledgments
Supported by the Intramural Research Programs of the National Institute of Diabetes and Digestive and Kidney Diseases and the Center for Information Technology of the National Institutes of Health, and by N.I.H. grant R01 NS042852 (to S.C.M.). We thank Dr. Reed Wickner for assistance with gene sequencing and Dr. Peter Pytel for assistance with histopathology. Calculations were performed on the Biowulf Linux cluster at the N.I.H.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmed M, Davis J, Aucoin D, Sato T, Ahuja S, Aimoto S, Elliott JI, Van Nostrand WE, Smith SO. Structural conversion of neurotoxic amyloid-β(1–42) oligomers to fibrils. Nat Struct Mol Biol. 2010;17:561–U556. doi: 10.1038/nsmb.1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizenstein HJ, Nebes RD, Saxton JA, Price JC, Mathis CA, Tsopelas ND, Ziolko SK, James JA, Snitz BE, Houck PR, et al. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol. 2008;65:1509–1517. doi: 10.1001/archneur.65.11.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayro MJ, Maly T, Birkett NR, Dobson CM, Griffin RG. Long-range correlations between aliphatic 13C nuclei in protein MAS NMR spectroscopy. Angew Chem-Int Edit. 2009;48:5708–5710. doi: 10.1002/anie.200901520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzinger TLS, Gregory DM, Burkoth TS, Miller-Auer H, Lynn DG, Botto RE, Meredith SC. Propagating structure of Alzheimer’s β-amyloid(10-35) is parallel β-sheet with residues in exact register. Proc Natl Acad Sci U S A. 1998;95:13407–13412. doi: 10.1073/pnas.95.23.13407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertini I, Gonnelli L, Luchinat C, Mao JF, Nesi A. A new structural model of Aβ40 fibrils. J Am Chem Soc. 2011;133:16013–16022. doi: 10.1021/ja2035859. [DOI] [PubMed] [Google Scholar]
- Bessen RA, Marsh RF. Distinct PrP properties suggest the molecular basis of strain variation in transmissible mink encephalopathy. J Virol. 1994;68:7859–7868. doi: 10.1128/jvi.68.12.7859-7868.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitan G, Kirkitadze MD, Lomakin A, Vollers SS, Benedek GB, Teplow DB. Amyloid β-protein (Aβ) assembly: Aβ40 and Aβ42 oligomerize through distinct pathways. Proc Natl Acad Sci U S A. 2003;100:330–335. doi: 10.1073/pnas.222681699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron B, Landreth GE. Inflammation, microglia, and Alzheimer’s disease. Neurobiol Dis. 2010;37:503–509. doi: 10.1016/j.nbd.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B, Thurber KR, Shewmaker F, Wickner RB, Tycko R. Measurement of amyloid fibril mass-per-length by tilted-beam transmission electron microscopy. Proc Natl Acad Sci U S A. 2009;106:14339–14344. doi: 10.1073/pnas.0907821106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimon S, Shaibat MA, Jones CR, Calero DC, Aizezi B, Ishii Y. Evidence of fibril-like β-sheet structures in a neurotoxic amyloid intermediate of Alzheimer’s β-amyloid. Nat Struct Mol Biol. 2007;14:1157–1164. doi: 10.1038/nsmb1345. [DOI] [PubMed] [Google Scholar]
- Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, Pontecorvo MJ, Hefti F, Carpenter AP, Flitter ML, et al. Use of florbetapir-PET for imaging β-amyloid pathology. JAMA-J Am Med Assoc. 2011;305:275–283. doi: 10.1001/jama.2010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colletier JP, Laganowsky A, Landau M, Zhao ML, Soriaga AB, Goldschmidt L, Flot D, Cascio D, Sawaya MR, Eisenberg D. Molecular basis for amyloid-β polymorphism. Proc Natl Acad Sci U S A. 2011;108:16938–16943. doi: 10.1073/pnas.1112600108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinge J. Prion diseases of humans and animals: Their causes and molecular basis. Annu Rev Neurosci. 2001;24:519–550. doi: 10.1146/annurev.neuro.24.1.519. [DOI] [PubMed] [Google Scholar]
- Cummings BJ, Pike CJ, Shankle R, Cotman CW. β-amyloid deposition and other measures of neuropathology predict cognitive status in Alzheimer’s disease. Neurobiol Aging. 1996;17:921–933. doi: 10.1016/s0197-4580(96)00170-4. [DOI] [PubMed] [Google Scholar]
- De Paepe G, Lewandowski JR, Loquet A, Bockmann A, Griffin RG. Proton assisted recoupling and protein structure determination. J Chem Phys. 2008;129:245101. doi: 10.1063/1.3036928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannakopoulos P, Hof PR, Michel JP, Guimon J, Bouras C. Cerebral cortex pathology in aging and Alzheimer’s disease: A quantitative survey of large hospital-based geriatric and psychiatric cohorts. Brain Res Rev. 1997;25:217–245. doi: 10.1016/s0165-0173(97)00023-4. [DOI] [PubMed] [Google Scholar]
- Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH. Mechanisms underlying inflammation in neurodegeneration. Cell. 2010;140:918–934. doi: 10.1016/j.cell.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsbury C, Frey P, Olivieri V, Aebi U, Muller SA. Multiple assembly pathways underlie amyloid-β fibril polymorphisms. J Mol Biol. 2005;352:282–298. doi: 10.1016/j.jmb.2005.07.029. [DOI] [PubMed] [Google Scholar]
- Gordon DJ, Sciarretta KL, Meredith SC. Inhibition of β-amyloid(40) fibrillogenesis and disassembly of β-amyloid(40) fibrils by short β-amyloid congeners containing N-methyl amino acids at alternate residues. Biochemistry. 2001;40:8237–8245. doi: 10.1021/bi002416v. [DOI] [PubMed] [Google Scholar]
- Gravina SA, Ho LB, Eckman CB, Long KE, Otvos L, Younkin LH, Suzuki N, Younkin SG. Amyloid-β protein (Aβ) in Alzheimer’s disease brain: Biochemical and immunocytochemical analysis with antibodies specific for forms ending at Aβ40 or Aβ42(43) J Biol Chem. 1995;270:7013–7016. doi: 10.1074/jbc.270.13.7013. [DOI] [PubMed] [Google Scholar]
- Hu KN, Qiang W, Bermejo GA, Schwieters CD, Tycko R. Restraints on backbone conformations in solid state NMR studies of uniformly labeled proteins from quantitative amide 15N-15N and carbonyl 13C-13C dipolar recoupling data. J Magn Reson. 2012;218:115–127. doi: 10.1016/j.jmr.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishii Y. 13C-13C dipolar recoupling under very fast magic angle spinning in solid state nuclear magnetic resonance: Applications to distance measurements, spectral assignments, and high-throughput secondary-structure determination. J Chem Phys. 2001;114:8473–8483. [Google Scholar]
- Iwatsubo T, Odaka A, Suzuki N, Mizusawa H, Nukina N, Ihara Y. Visualization of Aβ42(43) and Aβ40 in senile plaques with end-specific Aβ monoclonals: Evidence that an initially deposited species is Aβ42(43) Neuron. 1994;13:45–53. doi: 10.1016/0896-6273(94)90458-8. [DOI] [PubMed] [Google Scholar]
- Jan A, Adolfsson O, Allaman I, Buccarello AL, Magistretti PJ, Pfeifer A, Muhs A, Lashuel HA. Aβ42 neurotoxicity is mediated by ongoing nucleated polymerization process rather than by discrete Aβ42 species. J Biol Chem. 2011;286:8585–8596. doi: 10.1074/jbc.M110.172411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaroniec CP, Filip C, Griffin RG. 3d TEDOR NMR experiments for the simultaneous measurement of multiple carbon-nitrogen distances in uniformly 13C,15N-labeled solids. J Am Chem Soc. 2002;124:10728–10742. doi: 10.1021/ja026385y. [DOI] [PubMed] [Google Scholar]
- Jaroniec CP, Tounge BA, Herzfeld J, Griffin RG. Frequency selective heteronuclear dipolar recoupling in rotating solids: Accurate 13C-15N distance measurements in uniformly 13C,15N -labeled peptides. J Am Chem Soc. 2001;123:3507–3519. doi: 10.1021/ja003266e. [DOI] [PubMed] [Google Scholar]
- Jarrett JT, Berger EP, Lansbury PT. The carboxy terminus of the β-amyloid protein is critical for the seeding of amyloid formation: Implications for the pathogenesis of Alzheimer’s disease. Biochemistry. 1993;32:4693–4697. doi: 10.1021/bi00069a001. [DOI] [PubMed] [Google Scholar]
- Kheterpal I, Williams A, Murphy C, Bledsoe B, Wetzel R. Structural features of the Aβ amyloid fibril elucidated by limited proteolysis. Biochemistry. 2001;40:11757–11767. doi: 10.1021/bi010805z. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Engler H, Nordberg A, Wang YM, Blomqvist G, Holt DP, Bergstrom M, Savitcheva I, Huang GF, Estrada S, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh compound B. Ann Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- Kodali R, Williams AD, Chemuru S, Wetzel R. Aβ1-40 forms five distinct amyloid structures whose β-sheet contents and fibril stabilities are correlated. J Mol Biol. 2010;401:503–517. doi: 10.1016/j.jmb.2010.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krafft GA, Klein WL. ADDLs and the signaling web that leads to Alzheimer’s disease. Neuropharmacology. 2010;59:230–242. doi: 10.1016/j.neuropharm.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Kuo YM, Emmerling MR, VigoPelfrey C, Kasunic TC, Kirkpatrick JB, Murdoch GH, Ball MJ, Roher AE. Water-soluble Aβ(n-40, n-42) oligomers in normal and Alzheimer disease brains. J Biol Chem. 1996;271:4077–4081. doi: 10.1074/jbc.271.8.4077. [DOI] [PubMed] [Google Scholar]
- Langer F, Eisele YS, Fritschi SK, Staufenbiel M, Walker LC, Jucker M. Soluble Aβ seeds are potent inducers of cerebral β-amyloid deposition. J Neurosci. 2011;31:14488–14495. doi: 10.1523/JNEUROSCI.3088-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansbury PT, Costa PR, Griffiths JM, Simon EJ, Auger M, Halverson KJ, Kocisko DA, Hendsch ZS, Ashburn TT, Spencer RGS, et al. Structural model for the β-amyloid fibril based on interstrand alignment of an antiparallel-sheet comprising a C-terminal peptide. Nat Struct Biol. 1995;2:990–998. doi: 10.1038/nsb1195-990. [DOI] [PubMed] [Google Scholar]
- Lesne S, Koh MT, Kotilinek L, Kayed R, Glabe CG, Yang A, Gallagher M, Ashe KH. A specific amyloid-β protein assembly in the brain impairs memory. Nature. 2006;440:352–357. doi: 10.1038/nature04533. [DOI] [PubMed] [Google Scholar]
- Lopez del Amo JM, Dasari M, Fink U, Grelle G, Wanker EE, Bieschke J, Reif B. Structural analysis of Alzheimer disease β-amyloid oligomers induced by the green tea compound epigallocatechin-3-gallate (EGCG) J Mol Biol. 2012;421:517–524. doi: 10.1016/j.jmb.2012.01.013. [DOI] [PubMed] [Google Scholar]
- Luhrs T, Ritter C, Adrian M, Riek-Loher D, Bohrmann B, Doeli H, Schubert D, Riek R. 3D structure of Alzheimer’s amyloid-β(1–42) fibrils. Proc Natl Acad Sci U S A. 2005;102:17342–17347. doi: 10.1073/pnas.0506723102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar A, Chung HY, Dolios G, Wang R, Asamoah N, Lobel P, Maxfield FR. Degradation of fibrillar forms of Alzheimer’s amyloid β-peptide by macrophages. Neurobiol Aging. 2008;29:707–715. doi: 10.1016/j.neurobiolaging.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathis CA, Wang YM, Holt DP, Huang GF, Debnath ML, Klunk WE. Synthesis and evaluation of 11C-labeled 6-substituted 2-arylbenzothiazoles as amyloid imaging agents. J Med Chem. 2003;46:2740–2754. doi: 10.1021/jm030026b. [DOI] [PubMed] [Google Scholar]
- Meinhardt J, Sachse C, Hortschansky P, Grigorieff N, Fandrich M. Aβ1-40 fibril polymorphism implies diverse interaction patterns in amyloid fibrils. J Mol Biol. 2009;386:869–877. doi: 10.1016/j.jmb.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL, et al. Exogenous induction of cerebral β-amyloidogenesis is governed by agent and host. Science. 2006;313:1781–1784. doi: 10.1126/science.1131864. [DOI] [PubMed] [Google Scholar]
- Morcombe CR, Gaponenko V, Byrd RA, Zilm KW. Diluting abundant spins by isotope edited radio frequency field assisted diffusion. J Am Chem Soc. 2004;126:7196–7197. doi: 10.1021/ja047919t. [DOI] [PubMed] [Google Scholar]
- Noguchi A, Matsumura S, Dezawa M, Tada M, Yanazawa M, Ito A, Akioka M, Kikuchi S, Sato M, Ideno S, et al. Isolation and characterization of patient-derived, toxic, high mass amyloid β-protein (Aβ) assembly from Alzheimer disease brains. J Biol Chem. 2009;284:32895–32905. doi: 10.1074/jbc.M109.000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olofsson A, Lindhagen-Persson M, Sauer-Eriksson AE, Ohman A. Amide solvent protection analysis demonstrates that amyloid-β(1–40) and amyloid-β(1–42) form different fibrillar structures under identical conditions. Biochem J. 2007;404:63–70. doi: 10.1042/BJ20061561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paravastu AK, Leapman RD, Yau WM, Tycko R. Molecular structural basis for polymorphism in Alzheimer’s β-amyloid fibrils. Proc Natl Acad Sci U S A. 2008;105:18349–18354. doi: 10.1073/pnas.0806270105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paravastu AK, Qahwash I, Leapman RD, Meredith SC, Tycko R. Seeded growth of β-amyloid fibrils from Alzheimer’s brain-derived fibrils produces a distinct fibril structure. Proc Natl Acad Sci U S A. 2009;106:7443–7448. doi: 10.1073/pnas.0812033106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petkova AT, Leapman RD, Guo ZH, Yau WM, Mattson MP, Tycko R. Self-propagating, molecular-level polymorphism in Alzheimer’s β-amyloid fibrils. Science. 2005;307:262–265. doi: 10.1126/science.1105850. [DOI] [PubMed] [Google Scholar]
- Petkova AT, Yau WM, Tycko R. Experimental constraints on quaternary structure in Alzheimer’s β-amyloid fibrils. Biochemistry. 2006;45:498–512. doi: 10.1021/bi051952q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiang W, Kelley K, Tycko R. Polymorph-specific kinetics and thermodynamics of β-amyloid fibril growth. J Am Chem Soc. 2013 doi: 10.1021/ja311963f. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiang W, Yau WM, Luo YQ, Mattson MP, Tycko R. Antiparallel β-sheet architecture in Iowa mutant β-amyloid fibrils. Proc Natl Acad Sci U S A. 2012;109:4443–4448. doi: 10.1073/pnas.1111305109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiang W, Yau WM, Tycko R. Structural evolution of Iowa mutant β-amyloid fibrils from polymorphic to homogeneous states under repeated seeded growth. J Am Chem Soc. 2011;133:4018–4029. doi: 10.1021/ja109679q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safar J, Wille H, Itrri V, Groth D, Serban H, Torchia M, Cohen FE, Prusiner SB. Eight prion strains have PrPsc molecules with different conformations. Nat Med. 1998;4:1157–1165. doi: 10.1038/2654. [DOI] [PubMed] [Google Scholar]
- Scheidt HA, Morgado I, Rothemund S, Huster D, Fandrich M. Solid state NMR spectroscopic investigation of Aβ protofibrils: Implication of a β-sheet remodeling upon maturation into terminal amyloid fibrils. Angew Chem-Int Edit. 2011;50:2837–2840. doi: 10.1002/anie.201007265. [DOI] [PubMed] [Google Scholar]
- Scheuner D, Eckman C, Jensen M, Song X, Citron M, Suzuki N, Bird TD, Hardy J, Hutton M, Kukull W, et al. Secreted amyloid β-protein similar to that in the senile plaques of Alzheimer’s disease is increased in vivo by the presenilin 1 and 2 and APP mutations linked to familial Alzheimer’s disease. Nat Med. 1996;2:864–870. doi: 10.1038/nm0896-864. [DOI] [PubMed] [Google Scholar]
- Schwieters CD, Kuszewski JJ, Clore GM. Using Xplor-NIH for NMR molecular structure determination. Prog Nucl Magn Reson Spectrosc. 2006;48:47–62. [Google Scholar]
- Selkoe DJ. Soluble oligomers of the amyloid β-protein impair synaptic plasticity and behavior. Behav Brain Res. 2008;192:106–113. doi: 10.1016/j.bbr.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y, Delaglio F, Cornilescu G, Bax A. TALOS+: A hybrid method for predicting protein backbone torsion angles from NMR chemical shifts. J Biomol NMR. 2009;44:213–223. doi: 10.1007/s10858-009-9333-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stohr J, Watts JC, Mensinger ZL, Oehler A, Grillo SK, DeArmond SJ, Prusiner SB, Giles K. Purified and synthetic Alzheimer’s amyloid β (Aβ) prions. Proc Natl Acad Sci U S A. 2012;109:11025–11030. doi: 10.1073/pnas.1206555109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana R, Perluigi M, Butterfield DA. Oxidatively modified proteins in Alzheimer’s disease (AD), mild cognitive impairment and animal models of AD: Role of Aβ in pathogenesis. Acta Neuropathol. 2009;118:131–150. doi: 10.1007/s00401-009-0517-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takegoshi K, Nakamura S, Terao T. 13C-1H dipolar-assisted rotational resonance in magic-angle-spinning NMR. Chem Phys Lett. 2001;344:631–637. [Google Scholar]
- Tanzi RE, Bertram L. Twenty years of the Alzheimer’s disease amyloid hypothesis: A genetic perspective. Cell. 2005;120:545–555. doi: 10.1016/j.cell.2005.02.008. [DOI] [PubMed] [Google Scholar]
- Tomic JL, Pensalfini A, Head E, Glabe CG. Soluble fibrillar oligomer levels are elevated in Alzheimer’s disease brain and correlate with cognitive dysfunction. Neurobiol Dis. 2009;35:352–358. doi: 10.1016/j.nbd.2009.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torok M, Milton S, Kayed R, Wu P, McIntire T, Glabe CG, Langen R. Structural and dynamic features of Alzheimer’s Aβ peptide in amyloid fibrils studied by site-directed spin labeling. J Biol Chem. 2002;277:40810–40815. doi: 10.1074/jbc.M205659200. [DOI] [PubMed] [Google Scholar]
- Tougu V, Tiiman A, Palumaa P. Interactions of Zn(II) and Cu(II) ions with Alzheimer’s amyloid-β peptide. Metal ion binding, contribution to fibrillization and toxicity. Metallomics. 2011;3:250–261. doi: 10.1039/c0mt00073f. [DOI] [PubMed] [Google Scholar]
- Toyama BH, Weissman JS. Amyloid structure: Conformational diversity and consequences. Annu Rev Biochem. 2011;80:557–585. doi: 10.1146/annurev-biochem-090908-120656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tycko R. Symmetry-based constant-time homonuclear dipolar recoupling in solid state NMR. J Chem Phys. 2007;126:064506. doi: 10.1063/1.2437194. [DOI] [PubMed] [Google Scholar]
- Villemagne VL, Pike KE, Chetelat G, Ellis KA, Mulligan RS, Bourgeat P, Ackermann U, Jones G, Szoeke C, Salvado O, et al. Longitudinal assessment of Aβ and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69:181–192. doi: 10.1002/ana.22248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh DM, Hartley DM, Kusumoto Y, Fezoui Y, Condron MM, Lomakin A, Benedek GB, Selkoe DJ, Teplow DB. Amyloid β-protein fibrillogenesis: Structure and biological activity of protofibrillar intermediates. J Biol Chem. 1999;274:25945–25952. doi: 10.1074/jbc.274.36.25945. [DOI] [PubMed] [Google Scholar]
- Yang FS, Lim GP, Begum AN, Ubeda OJ, Simmons MR, Ambegaokar SS, Chen PP, Kayed R, Glabe CG, Frautschy SA, et al. Curcumin inhibits formation of amyloid-β oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem. 2005;280:5892–5901. doi: 10.1074/jbc.M404751200. [DOI] [PubMed] [Google Scholar]
- Yankner BA, Lu T. Amyloid β-protein toxicity and the pathogenesis of Alzheimer disease. J Biol Chem. 2009;284:4754–4758. doi: 10.1074/jbc.R800018200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R, Hu XY, Khant H, Ludtke SJ, Chiu W, Schmid MF, Frieden C, Lee JM. Interprotofilament interactions between Alzheimer’s Aβ1-42 peptides in amyloid fibrils revealed by cryoEM. Proc Natl Acad Sci U S A. 2009;106:4653–4658. doi: 10.1073/pnas.0901085106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.