Abstract
Anxiety disorders are prevalent in children with epilepsy. The purpose of this study was to evaluate the efficacy, adaptability, and feasibility of a manual-based, computer-assisted cognitive behavioral therapy (CBT) intervention for anxiety disorders in children with epilepsy. Fifteen anxious youth (aged 8–13 years) with epilepsy completed 12 weeks of manualized computer-assisted CBT. Children and parents completed a semi-structured interview at baseline, and questionnaires assessing symptoms of anxiety, depression, and behavior problems were completed prior to treatment, at treatment midpoint, after treatment completion, and three months post treatment. There were significant reductions in symptoms of anxiety and depression reported by the children at completion of the intervention and at the three-month follow-up. Similarly, parents reported fewer symptoms of anxiety and a reduction in behavior problems. No adverse events were reported. This CBT intervention for children with epilepsy and anxiety disorders is safe, effective, and feasible with a promising future.
Keywords: anxiety, cognitive behavior therapy, child, computer technology, pediatric, mental health, intervention, seizures
INTRODUCTION
Seizure disorders are the most common childhood neurologic condition, with 4–10% of children experiencing at least one seizure.[1] Children with epilepsy have higher rates of emotional and behavioral problems than their healthy peers.[2–5] More specifically, Pinquart and Shen[6] found that children with seizures are more likely to exhibit anxious symptoms than children in the general population. The prevalence rates of anxiety disorders in children with epilepsy, as assessed by studies employing standardized psychiatric interviews, range from 13.0–48.5%.[7–10] As part of a large population-based investigation utilizing parent report, the 2007 National Survey of Children’s Health found that children with a current seizure disorder were more likely to experience anxiety (17% v. 3%) and depression (8% v. 2%) than children without epilepsy.[11]
The unpredictability of seizures and the associated sense of vulnerability may place children with epilepsy at risk for exaggerated fears and anxiety, especially about seizures.[12,13] Psychosocial stress and the severity of epilepsy also appear to impact the expression of anxiety and depression.[14] Additionally, Kanner[15] described the complex relationship between anxiety disorders, mood disorders, and epilepsy which have all been linked to abnormalities in serotonin levels in the nervous system. This relationship may be further complicated by the potential adverse consequences of epilepsy medications. In children, anxiety can interfere with academic performance, social life, social skills, and general well-being.[6] Specifically, among children with epilepsy, Stevanovic et al.[16] reported that quality of life significantly decreases as symptoms of anxiety and depression increase. Symptoms of generalized anxiety, separation anxiety, and depression have a more significant impact on health-related quality of life than other anxiety symptoms (e.g., panic and somatic symptoms), demographic variables, and epilepsy-related variables.[16] Reilly et al.[17] suggested that epilepsy services should screen for anxiety and depression as part of a comprehensive assessment. Treatment of anxiety disorders in childhood might effectively prevent further serious mental illness. It might also reduce the societal costs of adverse health and social outcomes such as reduced educational attainment, marriage instability, and low occupational and financial status.[18] If left untreated, anxiety in childhood can persist into adulthood, as evidenced by high rates of anxiety, depression, and suicide in adults with epilepsy.[8]
Pharmacological and nonpharmacological interventions for psychiatric comorbidities in children with epilepsy are infrequent. When nonpharmacological interventions are introduced, the focus tends to be primarily on seizure reduction rather than on the reduction of symptoms of psychological disorders.[19] Understandably, the reduction of seizures is often the primary focus of contact with health care providers. Emotional and behavioral problems, including anxiety and depression, are often under-diagnosed and under-treated in children with epilepsy.[20] To date, only two pediatric epilepsy intervention studies have addressed psychosocial and mood-related symptoms. One study focused on promoting the self-management of epilepsy and improving related psychosocial functioning.[21] The second study targeted subthreshold depressive symptoms in order to try to prevent the onset of a depressive disorder.[22] To our knowledge, there are no published intervention studies aimed at treating anxiety disorders in children with epilepsy.[19]
Various studies have addressed the efficacy of cognitive behavioral therapy (CBT) in conjunction with medical comorbidities.[23] Keehn et al.[24] recently conducted a pilot study of children with autism and anxiety disorders, utilizing the Coping Cat, a manualized treatment protocol that has been demonstrated to be efficacious in randomized clinical trials.[25–27] The treatment protocol was modified for children with autism in ways that did not impact treatment fidelity. Keehn et al.[24] reported a clinically significant reduction in levels of anxiety in children with high functioning autism spectrum disorder. Hudson et al.[28] provided suggestions and case examples to demonstrate the suitability of Coping Cat for treating anxiety disorders in children with comorbid diagnoses. Their case examples included children with spina bifida, selective mutism, and attention deficit/hyperactivity disorder (ADHD).
Recent research in the general psychiatric literature has sought to develop cost-effective and transportable CBT intervention programs.[29–33] Such programs have been delivered in innovative settings such as primary care facilities, school, and camps, and have made use of computers and the internet.[34–40] These studies contribute to the widely recognized goal of disseminating evidence-based treatments from research to community settings.[41] Additional research is needed to reduce dissemination barriers and to improve the accessibility of CBT to children and adolescents.[42]
In an effort to identify a non-pharmacological, effective, and feasible treatment for anxiety in children with epilepsy, this study utilized a computer-assisted CBT program, Camp Cope-A-Lot. This program, adapted from the Coping Cat manualized program, has been shown to be efficacious in reducing anxiety in youth in the general population.[41] This is the first time this type of CBT intervention has been used in children with epilepsy and anxiety disorders. The primary aim of this study was to determine the efficacy, adaptability, and feasibility of a computer-assisted CBT intervention as a treatment for anxiety disorders in children with epilepsy. We hypothesized that children and their parents would report reduced symptoms of anxiety over the course of a 12-week intervention, and that this reduction in anxiety symptoms would be maintained at 3-month follow-up.
METHODS
Participants
Children and their parents were recruited from a comprehensive epilepsy program in a pediatric neurology clinic at a tertiary care center. Selection criteria for children included: (a) a diagnosis of epilepsy for a minimum of 6 months, (b) chronological age between 8 and 13 years, (c) no MRI abnormalities other than atrophy, (d) no other developmental disabilities (e.g., intellectual disability or autism), (e) no other neurological disorders, (f) a current primary anxiety disorder, (g) no current non-pharmacological or pharmacological treatment of an anxiety disorder, and (h) a minimum of a first-grade reading level according to the Wide Range Achievement Test 4 (WRAT-4).
Twenty children met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)[43] criteria for an anxiety disorder as determined by a semi-structured interview, Kiddie-Schedule for Affective Disorders and Schizophrenia – Present and Lifetime Version (KSADS-PL).[44] The KSADS-PL has been utilized in several studies of children with epilepsy to identify rates of psychiatric comorbidity.[7–10] In the current study, two interviewers were specially trained to administer the clinical interview (JBB, JEJ).
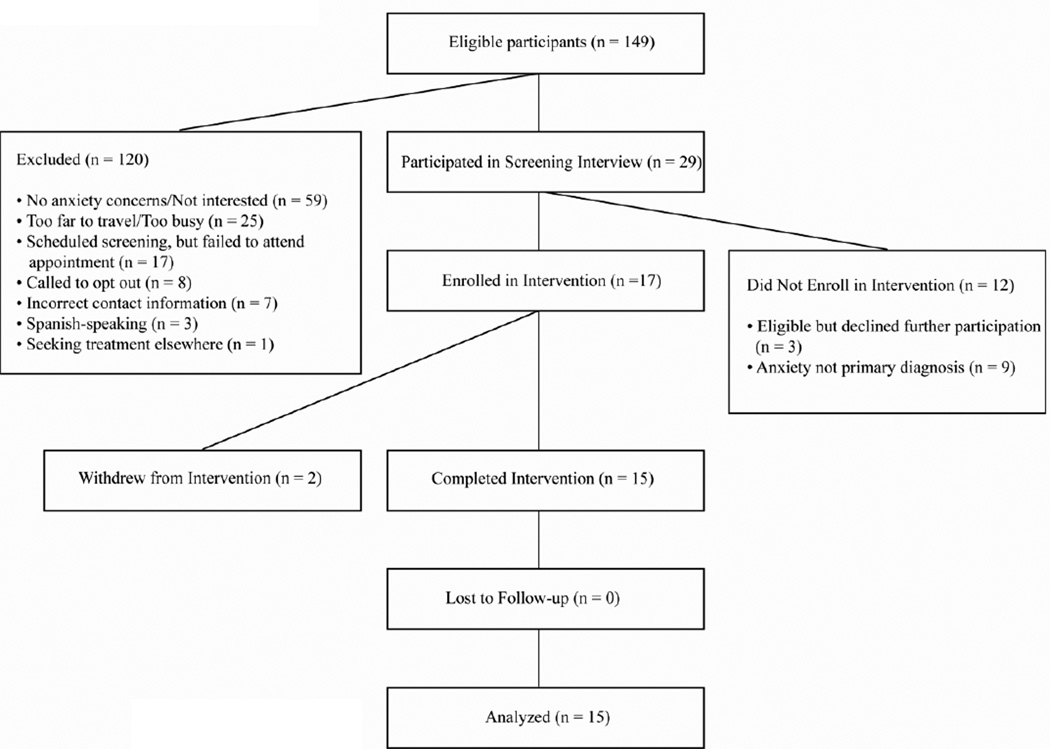
Three children qualified but declined to enroll, and two participants withdrew from the intervention due to scheduling conflicts. The remaining 15 children completed the 12-week intervention and the 3-month follow-up visit. One parent of each child participated in meetings with the child’s therapist during weeks 1, 3, 7, and 12, and the 3-month follow-up visit. Figure 1 is a flowchart depicting recruitment, enrollment, and follow-up.
Figure 1.
Flow chart depicting participant recruitment, screening, enrollment, and follow-up. Reasons for exclusion and failing to enroll are provided.
Measures
Anxiety and Depressive Symptoms
Children were assessed at baseline, week 7, week 12, and 3 months post treatment using reliable and valid self-report and parent proxy report measures. Anxiety self-report measures included the Multidimensional Anxiety Scale for Children (MASC)[45] and the Screen for Child Anxiety Related Emotional Disorders (SCARED).[46] Depressive symptoms were measured using the Children’s Depression Inventory (CDI).[47,48] Parents’ perceptions of their children’s anxiety were measured using the SCARED and the Child Behavior Checklist (CBCL)[49,50] was employed to measure parents’ perceptions of their children’s emotional and behavioral problems.
Parent and Child Satisfaction Measures
Satisfaction questionnaires were developed for this study to collect feedback from parents and children upon completing the intervention. The parent questionnaire consisted of 12 questions rated on a Likert scale from 1 to 5 (1=strongly disagree to 5=strongly agree). The questionnaire items included overall satisfaction, improvement in the child’s skills or knowledge, and the parent-therapist interaction. The child questionnaire consisted of two open-ended questions: (1) What did you like most about Camp Cope-A-Lot? and (2) What did you like least about Camp Cope-A-Lot? Additionally, the children were asked to rate their level of anxiety before and after the intervention on a 10-point scale (1=lowest level of anxiety to 10=highest level of anxiety).
Intervention
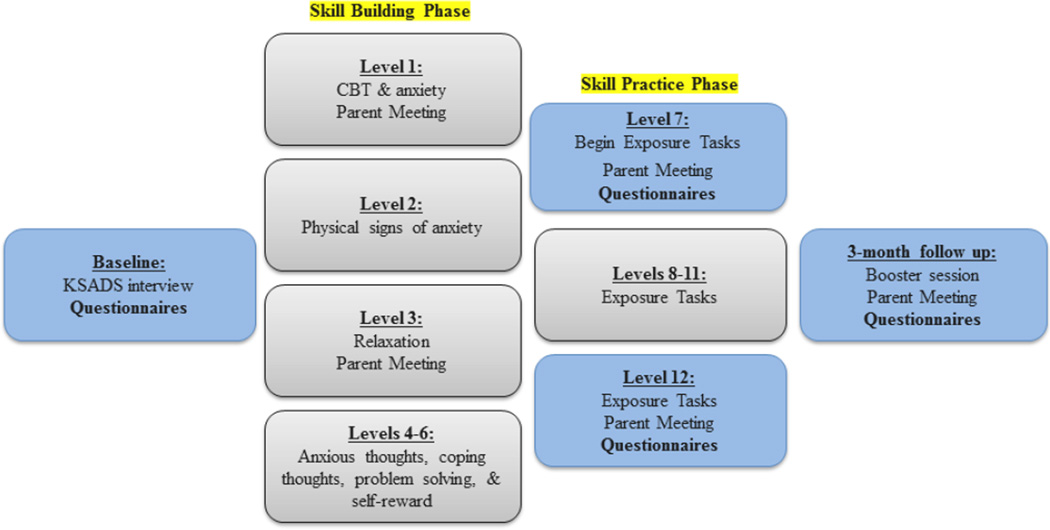
Camp Cope-A-Lot (CCAL) was developed as a manualized computer-assisted CBT treatment program for children (aged 7–13) with anxiety disorders.[51] In this study, the computer-assisted manualized intervention was delivered via computer and in the presence of a therapist in a medical center setting. The program is organized into 12 levels, one level administered per week, each lasting 50–60 minutes. CCAL is divided into two phases: skill building (Levels 1–6) and skill practice (Levels 7–12) (Figure 2). The skill-building phase introduces basic concepts such as relaxation training, identifying thoughts and feelings, problem solving, and self-reward. Approximately 30 minutes of the skill-building levels are delivered via computerized interactive activities. The therapist reinforces the concepts taught in the computer program with concrete examples and worksheets. The skill practice phase consists of exposure tasks in which the child implements the skills taught in the first six levels. Exposure tasks directly target the specific anxiety, worry, or fear that a child identifies. The levels in this phase consist of a 5-minute computer video demonstration of an exposure task. The child and therapist complete 1–2 exposure tasks together after each video. The child, parent, and therapist work together to plan and practice in-session and out-of-session exposure activities.
Figure 2.
Camp Cope-A-Lot intervention outline. Content of each appointment is shown, including when parent meetings occurred and when instruments were completed.
CCAL was modified, without compromising treatment fidelity, to make the intervention more flexible and more suitable to the needs of children with epilepsy. In particular, the program was adapted to accommodate different learning styles due to the high rates of learning problems in children with epilepsy.[25,52,53] Similar to protocol changes made by Keehn et al.,[24] the following modifications were made:
Appointment duration was lengthened to 60 minutes to allow the children to review content at an appropriate pace. Brief breaks were provided when needed.
Additional written materials were provided to the parents at weeks 1, 3, 7, and 12 to better inform parents of the content and skills learned at each level in order to increase children’s compliance and skill-building at home.
Additional written materials were developed for the children to reinforce their understanding of the program’s concepts.
More concrete language was used as needed.
Children who had difficulties with writing and spelling were aided by the therapist to reduce any writing-related burden.
The primary focus was on behavioral components, rather than cognitive components, if a child had difficulty with cognitive restructuring (i.e., learning to identify problematic or maladaptive thoughts).
Reinforcement activities were identified to match the child’s individual interests. If a child was not interested in computer games, other activities were provided (board games, drawing, stickers, etc.).
All sessions were videotaped. Fifty percent of the sessions were reviewed across participants and sessions in order to monitor treatment fidelity and protocol adherence. Importantly, at no point did the computer program or video games trigger seizures.
Procedures
The Health Sciences Institutional Review Board (IRB) at the University of Wisconsin School of Medicine and Public Health approved this protocol. The Comprehensive Epilepsy Program at the University of Wisconsin generated a log of children who fell within the target age range. An invitation letter was sent to the potential study participants (i.e., children and their parents) who did not meet exclusion criteria (i.e., intellectual disability, autism). The letter described the study and the participation requirements. Parents were then contacted by phone and were further screened to identify any potential symptoms related to anxiety. If parents indicated interest in the study, they were scheduled for an interview. One participant who had not been contacted by the study team was referred to the study by the child’s neurologist after reporting problematic behaviors (e.g., inattention, social problems, and problems in school or at home). Two participants received an invitation letter but did not contact study staff until another healthcare provider (i.e., nurse, neuropsychologist) referred them to the study. A screening interview was conducted with these parents and their children regardless of whether these problems were reported in an anxiety-related context. Prior to the interview, IRB consent forms were mailed for review. Consent was obtained from the parent or legal guardian, and the child signed an assent form.
Parents and children were screened separately using the K-SADS-PL interview. A consensus diagnosis was established between the two interviewers; if agreement could not be reached, the participant was excluded from the study (n=1). If the child met criteria for an anxiety disorder based on this interview, the child and parent were invited to participate in the intervention. Two children who had secondary depressive disorder diagnoses were monitored closely for suicidal ideation or increases in depressive symptoms. These children’s neurologists were consulted to determine if study participation should be terminated.
Each child completed one level of the intervention each week for 12 weeks and a 3-month follow-up visit with his or her individual therapist. Children were rewarded for completing out-of-session tasks with game time at the end of every session. With parent collaboration, children also received rewards at home for completing exposure tasks (e.g., favorite treat, alone time with a parent, outing with a friend) and for completing the entire program (e.g., fishing day with dad, new video game, dinner at a favorite restaurant). Emphasis was placed on rewarding effort on the tasks versus correctly completing the tasks. During the 3-month follow-up visit, the child and therapist reviewed skills the child learned during the intervention (e.g., identifying thoughts and feelings, challenging anxious thoughts, and problem-solving) and applied the skills to a current issue of the child’s choice. Children were compensated with gift cards for completing the KSADS-PL interview, week 6, week 12, and the 3-month follow-up visit.
The parent of each child also met with the child’s assigned therapist to discuss the child’s progress and any concerns at weeks 1, 3, 7, 12, and the 3-month follow-up. Parents were given a handout at each parent meeting summarizing the concepts the children learned in each level of the intervention. Parents were made aware of their child’s out-of-session assignments, but the children were encouraged to complete the activities on their own. Parent meetings also gave parents an opportunity to give input on the creation of their child’s fear hierarchy and exposure tasks.
Data Analysis
Repeated measures one-way ANOVAs and post-hoc t-tests were used to analyze changes across all four treatment intervals (baseline, week 7, week 12, and 3-month follow-up) for child (CDI, MASC, SCARED) and parent (CBCL, SCARED) rating scales.
RESULTS
Sample Characteristics
Fifteen children completed the study (Table 1). The mean age of the sample was 11 years. Females and males were equally represented. Mean WRAT4 reading scores fell within the average range. Mean age of seizure onset was 7 years with average epilepsy duration of 4 years. The majority of children had localized epilepsy. Twelve children were taking one antiepilepsy medication (AED). The parents of three children made the decision not to place their children on an AED. No children were identified as seizure remitted. The children in this study had well-controlled epilepsy with monthly or yearly seizures.
Table 1.
Demographics and Epilepsy Variables
| Participants (N = 15) | Epilepsy Syndrome | ||
| Localized | 11 (73.3%) | ||
| Generalized | 4 (26.7%) | ||
| Age (M, SD) | 11.00 (1.51) | ||
| Gender | Seizure Frequency in past 12 months | ||
| Female | 8 (53.3%) | None | 2 (13.3%) |
| Male | 7 (46.7%) | Daily | 1 (6.7%) |
| Weekly | 1 (6.7%) | ||
| WRAT-4 Reading (M, SD) | 95.33 (10.59) | Monthly | 3 (20.0%) |
| Yearly | 8 (53.3%) | ||
| Age of Seizure Onset (M, SD) | 7.00 (3.00) | AEDs | |
| None | 3 (20.0%) | ||
| Mono | 12 (80.0%) | ||
|
Duration of Epilepsy yrs. (M, SD) |
4.12 (2.82) | ||
Anxiety Disorders
Before treatment, 15 children met DSM-IV criteria for a current primary anxiety disorder (Table 2). The most common diagnosis was generalized anxiety disorder (GAD), followed by separation anxiety and social phobia. Over half of the sample had more than one Axis I diagnosis, including a secondary anxiety disorder, a depressive disorder, or ADHD. None of the children had previously been prescribed a psychotropic medication or were currently in therapy. Two children were home-schooled due to significant functional impairments related to their anxiety disorders.
Table 2.
DSM-IV Disorders based on KSADS-PL
| KSADS Diagnosis | Number (%) |
|---|---|
| Primary Anxiety Disorder | |
| Generalized | 7 (46.7%) |
| Separation | 3 (20.0%) |
| Social Phobia | 3 (20.0%) |
| Specific Phobia | 1 (6.7%) |
| Anxiety NOS | 1 (6.7%) |
| Other Comorbidities | |
| 2nd Anxiety disorder | 4 (26.7%) |
| ADHD | 2 (13.3%) |
| Depressive dis. NOS | 2 (13.3%) |
| Selective Mutism | 1 (6.7%) |
| One Anxiety Disorder | 6 (40.0%) |
| Anxiety + comorbidities | 9 (60.0%) |
Child Post Treatment Outcomes
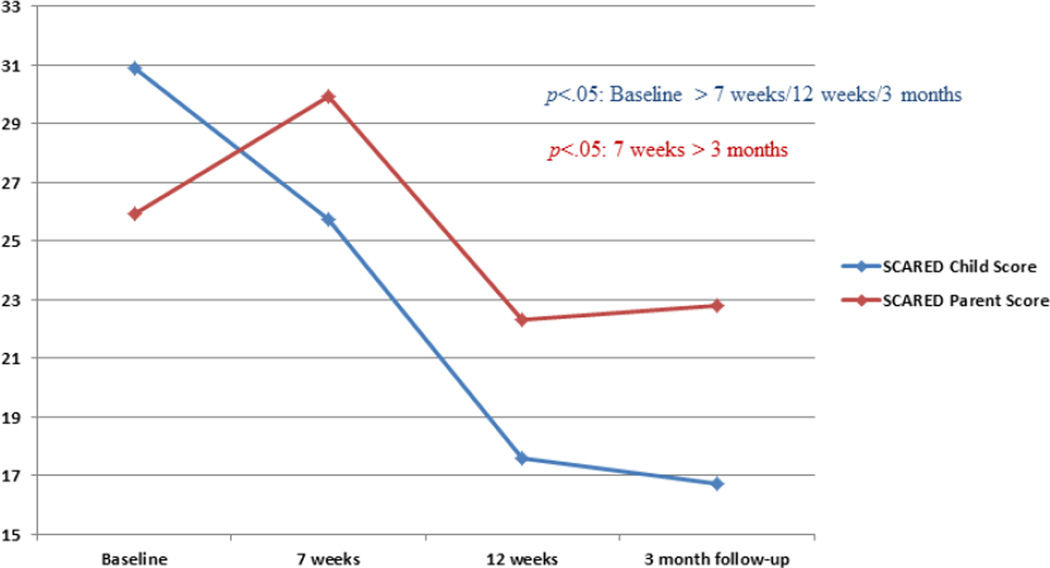
Child ratings of anxiety revealed significant change over time on the MASC (F1.773, 23.051]=4.669, p=0.023) and the SCARED (F1.332, 17.319]=5.873, p=0.019). Similarly, participants reported decreased anxiety from baseline (M=57.33, SD=15.21) to week 12 (M=47.93, SD=14.47) and from baseline to the 3-month follow-up (M=47.43, SD=12.28) on the MASC; p’s<0.05. In addition, child SCARED scores were significantly lowered from baseline (M=30.87, SD=18.22) to the successive treatment intervals: week 7 (M=25.73, SD=16.52), week 12 (M=17.60, SD=12.39), and the 3-month follow-up (M=16.71, SD=12.50) p’s<0.05 (Figure 3). Child ratings of depression revealed significant change over time on the CDI (F2.464, 32.037]=4.136, p=0.019). Post-hoc tests for the CDI indicated significant improvement relative to baseline scores (M=48.53, SD=11.34) at week 12 (M=42.87, SD=8.76) and at the 3-month follow-up (M=41.36, SD=7.11); p’s<0.01. Additionally, in terms of clinically significant outcomes, 73% of the participants did not have a clinically elevated score on the SCARED post-treatment.
Figure 3.
Parent and child SCARED scores shown over time. Child means showed a significant reduction in anxiety symptoms across all three time points (p<.05: Baseline>7 weeks/12 weeks/ 3-month follow-up). Parent means showed a significant reduction in their child’s anxiety symptoms after the intervention and at follow-up (p<.05: 7 weeks> 12 weeks/3-month follow-up).
Parent Post Treatment Outcomes
Parent ratings (CBCL, SCARED) were analyzed in a similar fashion. Results revealed significant change over time on the CBCL Total Problems subscale (F1.811, 21.727]=3.889, p=0.040). These ratings were significantly lowered from baseline (M=60.20, SD=8.36) to week 12 (M=55.07, SD=9.57) and the 3-month follow-up (M=56.93, SD=8.18); p’s<0.05. CBCL Internalizing ratings showed a trend for improvement (F1.850, 22.203]=3.265, p=0.06). Post-hoc tests were conducted, which revealed that scores were significantly lowered from baseline (M=67.27, SD=5.57) to week 12 (M=62.07, SD=7.05); p=0.039. As anticipated, CBCL Externalizing ratings did not significantly change across the four time intervals (p=0.105).
SCARED parent ratings did not differ significantly from baseline to week 7, week 12, or the 3- month follow-up. As is visible in Figure 3, parent SCARED ratings revealed a trend (non-significant) of an increase from baseline to week 7 (p=0.054), suggesting an increase in parents’ awareness of the child’s anxiety. As a result, additional exploratory post-hoc tests focused on comparisons between parent SCARED ratings at week 7 and those at week 12 and the 3-month follow-up. When compared to ratings at week 7 (M=29.93, SD=10.95), significant treatment effects were seen at week 12 (M=22.29, SD=8.77; p=0.02) and at the 3-month follow-up (M=22.79, SD=12.84; p=0.018). Parent SCARED ratings at week 12 were not significantly different from those at the 3-month follow-up (p=0.484).
Parent and Child Satisfaction
Parents reported a high level of satisfaction with CCAL (Table 3). The majority of parents agreed or strongly agreed that the program was helpful for their child, was effective in reducing their child’s anxiety, and taught their child to identify physical signs of anxiety. All parents indicated that they would recommend the program to other parents. Children reported that they felt the intervention was helpful in reducing their anxiety symptoms (100%). A subset of children indicated that they did not like the number of questionnaires that they were required to complete throughout the intervention (30%). Additional comments included: (a) Camp Cope-A-Lot was good/fun (38%), and (b) it was difficult to talk about the fears/anxiety/worries at times and exposure tasks addressing fears were sometimes hard (23%).
Table 3.
Parent Ratings for Perceived Satisfaction
| Item | M | SD |
|---|---|---|
| 1. Program is helpful for my child | 4.73 | 0.46 |
| 2. Identifying physical signs of anxiety | 4.27 | 0.70 |
| 3. Reducing anxiety and worries | 4.40 | 0.63 |
| 4. Would recommend program to other parents | 4.80 | 0.41 |
Note: Ratings based on a scale ranging from 1 to 5 with 1 = strongly disagree and 5 = strongly agree.
DISCUSSION
Due to the high rates of coexisting anxiety disorders in children with epilepsy, it is important, as recently recommended in a report by the Institute of Medicine,[54] to identify efficacious treatments for anxiety in this population. This is the first study to evaluate a cognitive behavioral therapy (CBT) intervention for children with epilepsy and anxiety disorders. Since the feasibility of this type of intervention had not previously been demonstrated, only limited epilepsy-specific modifications were utilized. The data from this study suggest that the Camp Cope-A-Lot intervention program, developed for children in the general population, helps alleviate anxiety in children with epilepsy. Both parents and children report reduced anxiety symptoms after completing the intervention. The reduction of anxiety symptoms is also maintained 3 months post treatment. Although the children presented with a variety of anxiety disorders and other comorbidities (e.g., ADHD), all report a reduction in their anxiety symptoms. Parents report an overall reduction in their children’s total problems (CBCL) after completing the intervention and at the 3-month follow-up, suggesting that the intervention may help to reduce problematic behaviors by targeting anxiety. Although depression was not a primary focus of the intervention, the data also suggest that children’s depressive symptoms were reduced. Furthermore, parents and children express high levels of satisfaction, indicating a high level of acceptability for this intervention.
There were no significant differences in parent ratings on the SCARED from baseline across all time points. In the literature from the general population comparing parent-child ratings of anxiety, a low correspondence between parent and child is frequently reported, with the parent reporting fewer symptoms than the child.[55–57] It has been postulated that anxiety may be less identifiable by external evaluation, particularly since anxiety is an internalizing disorder. Given the heritability of anxiety, parents may be anxious themselves and may normalize the anxiety present in their children.[58] Muris et al.[59] reported low to moderate correlations between SCARED parent-child ratings, ranging from .20-.47 depending on the subscale. Similarly, Cosi et al.[60] reported low to moderate correlations between parent and child SCARED ratings in a Spanish speaking population, indicating similar results across cultures.
This intervention has several limitations. Due to the small sample size, the generalizability of the results is limited. A larger sample size is needed to determine the impact of additional psychiatric comorbidities (e.g., ADHD, depression) on intervention outcomes. Furthermore, a larger sample could help to determine mediating and moderating variables that may impact the intervention results, such as type of epilepsy, medication, and duration of epilepsy. Additionally, no control group was obtained due to recruitment difficulties and time limitations, and as a result, a randomized controlled study is needed to attribute the reduction of anxiety symptoms to the specific intervention. In future studies, it will be important to include not only measures of treatment outcomes but measures of clinical significance as indicated by post treatment diagnostic status. No epilepsy-specific educational materials were provided to the children unless requested. Specific intervention components that target seizure education and seizure-specific worries may also enhance intervention outcomes. Finally, the majority of the children in this study had well-controlled seizure disorders and were of average cognitive ability. Results may not be generalizable to children with more severe epilepsy or who are cognitively impaired.
CONCLUSION
An intervention for children with anxiety and epilepsy using a manual-based, computer-assisted CBT treatment (Camp Cope-A-Lot) appears to be safe, effective, and feasible with a promising future. This study provides evidence for applying cognitive behavioral interventions, developed in the general population, to children with epilepsy. Modifications will likely be required, but the general treatment literature continues to encourage the flexibility of these treatment modalities.[28,52] Kendall and colleagues have disseminated the results of their research by providing easy access to training and materials for interventions that reduce the impact of anxiety disorders in children. The current study speaks to the importance of their work.
As part of a larger movement to encourage the transportability and dissemination of evidenced-based treatment modalities,[41,42,61] this study demonstrates success in adapting and applying an intervention that can be introduced into clinical practice in comprehensive epilepsy centers. The computer-assisted technology allows for portability to various settings. In this pilot study, all therapists (1 doctoral-level clinician, 1 master’s-level clinician, and 1 bachelor’s-level research specialist) underwent cognitive behavioral training (CBT 4 CBT) developed by Kendall and Khanna.[62] While familiarity with cognitive behavioral techniques is necessary in order for a clinician to implement this program, it is possible for nurses or allied health professionals to undergo training and gain the skills needed to successfully deliver the program. Future multicenter randomized controlled studies are needed to further understand how to best treat children with epilepsy and anxiety disorders. This study is an encouraging step that should provide an incentive for the development of future interventions to reduce the impact of anxiety disorders on the lives of children with epilepsy, and ultimately to improve their overall quality of life as they move into adolescence and adulthood.[18]
Highlights.
First published intervention trial for anxiety disorders in children with epilepsy
Evaluation of manualized, computer-assisted CBT for anxious children with epilepsy
Children reported reductions in symptoms of anxiety and depression
Parents reported fewer behavior problems and symptoms of anxiety in their child
This CBT intervention for anxious children with epilepsy is effective and feasible
ACKNOWLEDGMENTS
The authors would like to thank NIH and PACE for providing much needed funding. We would also like to thank all the children and parents who participated in this project. They are the motivation for the work that we do. Please contact Jana E. Jones (jejones@neurology.wisc.edu) for further details regarding specific adaptations to the CCAL intervention.
DISCLOSURES
This study was supported by in part by NIH 1KL2RR025012-01 (JEJ) and People Against Childhood Epilepsy (PACE).
JBB, MF, CS, DCJ, and JEJ report no disclosures.
We confirm that research performed on human subjects was in compliance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and the standards established by the granting agencies and the Institutional Review Board at the University of Wisconsin School of Medicine and Public Health. Informed consent was obtained for participants after the nature of the procedures was explained.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Friedman MJ, Sharieff GQ. Seizures in children. Pediatr Clin North Am. 2006;53(2):257–277. doi: 10.1016/j.pcl.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 2.Berg AT, Caplan R, Hesdorffer DC. Psychiatric and neurodevelopmental disorders in childhood-onset epilepsy. Epilepsy behav. 2011;20(3):550–555. doi: 10.1016/j.yebeh.2010.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Austin JK, Fastenau PS. Are seizure variables related to cognitive and behavior problems? Dev Med Child Neurol. 2010;52(1):5–6. doi: 10.1111/j.1469-8749.2009.03412.x. [DOI] [PubMed] [Google Scholar]
- 4.Loney JC, Wirrell EC, Sherman EMS, Hamiwka LD. Anxiety and depressive symptoms in children presenting with a first seizure. Pediatr Neurol. 2008;39(4):236–240. doi: 10.1016/j.pediatrneurol.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Freilinger M, Reisel B, Reiter E, Zelenko M, Hauser E, Seidl R. Behavioral and emotional problems in children with epilepsy. J Child Neurol. 2006;21(11):939–945. doi: 10.1177/08830738060210110501. [DOI] [PubMed] [Google Scholar]
- 6.Pinquart M, Shen Y. Anxiety in children and adolescents with chronic physical illnesses: a meta-analysis. Acta Paediatrica (Oslo, Norway: 1992. 2011;100(8):1069–1076. doi: 10.1111/j.1651-2227.2011.02223.x. [DOI] [PubMed] [Google Scholar]
- 7.Alwash RH, Hussein MJ, Matloub FF. Symptoms of anxiety and depression among adolescents with seizures in Irbid, Northern Jordan. Seizure. 2000;9(6):412–416. doi: 10.1053/seiz.2000.0427. [DOI] [PubMed] [Google Scholar]
- 8.Caplan R, Siddarth P, Gurbani S, Hanson R, Sankar R, Shields WD. Depression and Anxiety Disorders in Pediatric Epilepsy. Epilepsia. 2005;46(5):720–730. doi: 10.1111/j.1528-1167.2005.43604.x. [DOI] [PubMed] [Google Scholar]
- 9.Jones JE, Watson R, Sheth R, Caplan R, Koehn M, Seidenberg M, et al. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007;49(7):493–497. doi: 10.1111/j.1469-8749.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- 10.Ott D, Caplan R, Guthrie D, Siddarth P, Komo S, Shields WD, et al. Measures of psychopathology in children with complex partial seizures and primary generalized epilepsy with absence. J Am Acad Child Adolesc Psychiatry. 2001;40(8):907–914. doi: 10.1097/00004583-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129(2):256–264. doi: 10.1542/peds.2010-1371. [DOI] [PubMed] [Google Scholar]
- 12.Hamid H, Ettinger AB, Mula M. Anxiety symptoms in epilepsy: Salient issues for future research. Epilepsy behav. 2011;22(1):63–68. doi: 10.1016/j.yebeh.2011.04.064. [DOI] [PubMed] [Google Scholar]
- 13.Hesdorffer DC, Caplan R, Berg AT. Familial clustering of epilepsy and behavioral disorders: Evidence for a shared genetic basis. Epilepsia. 2012;53(2):301–307. doi: 10.1111/j.1528-1167.2011.03351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barry JJ, Ettinger AB, Friel P, Gilliam FG, Harden CL, Hermann B, et al. Consensus statement: The evaluation and treatment of people with epilepsy and affective disorders. Epilepsy behav. 2008;13(Suppl 1):S1–S29. doi: 10.1016/j.yebeh.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Kanner AM. Psychiatric issues in epilepsy: The complex relation of mood, anxiety disorders, and epilepsy. Epilepsy behav. 2009;15(1):83–87. doi: 10.1016/j.yebeh.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 16.Stevanovic D, Jancic J, Lakic A. The impact of depression and anxiety disorder symptoms on the health? related quality of life of children and adolescents with epilepsy. Epilepsia. 2011;52(8):e75–e78. doi: 10.1111/j.1528-1167.2011.03133.x. [DOI] [PubMed] [Google Scholar]
- 17.Reilly C, Agnew R, Neville BGR. Depression and anxiety in childhood epilepsy: A review. Seizure. 2011;20(8):589–597. doi: 10.1016/j.seizure.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Ruscio AM, Shear K, Wittchen H-U. Epidemiology of anxiety disorders. In: Stein MB, Steckler T, editors. Behavioral neurobiology of anxiety and its treatment. New York, NY US: Springer Science + Business Media; 2010. pp. 21–35. [Google Scholar]
- 19.Ramaratnam S, Baker GA, Goldstein LH. Psychological treatments for epilepsy. Cochrane Database Syst Rev. 2008;(3):CD002029. doi: 10.1002/14651858.CD002029.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Wagner JL, Smith G. Psychological services in a pediatric epilepsy clinic: Referral patterns and feasibility. Epilepsy behav. 2007;10(1):129–133. doi: 10.1016/j.yebeh.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Wagner JL, Smith G, Ferguson P, Van Bakergem K, Hrisko S. Pilot study of an integrated cognitive-behavioral and self-management intervention for youth with epilepsy and caregivers: Coping Openly and Personally with Epilepsy (COPE) Epilepsy behav. 2010;18(3):280–285. doi: 10.1016/j.yebeh.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Martinović Ž, Simonović P, Djokić R. Preventing depression in adolescents with epilepsy. Epilepsy behav. 2006;9(4):619–624. doi: 10.1016/j.yebeh.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Thompson RD, Delaney P, Flores I, Szigethy E. Cognitive-behavioral therapy for children with comorbid physical illness. Child Adolesc Psychiatr Clin N Am. 2011;20(2):329–348. doi: 10.1016/j.chc.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 24.Keehn RHM, Lincoln AJ, Brown MJ, Chavira DA. The Coping Cat Program for Children with Anxiety and Austism Spectrum Disorder: A Pilot Randomized Controlled Trial. J Autism Dev Disord. 2012 doi: 10.1007/s10803-012-1541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kendall PC, Hedtke KA. Cognitive-behavioral Therapy for Anxious Children: Therapist Manual. Ardmore, PA: Workbook Publishing; 2006. [Google Scholar]
- 26.Kendall PC, Hedtke KA. Coping Cat Workbook. Ardmore, PA: Workbook Publishing; 2006. [Google Scholar]
- 27.Mor N, Meijers J. Cognitive behavioral therapy in childhood anxiety. Israel J Psychiat. 2009;46(4):282–289. [PubMed] [Google Scholar]
- 28.Hudson JL, Krain AL, Kendall PC. Expanding horizons: Adapting manual-based treatments for anxious children with comorbid diagnoses. Cogn Behav Pract. 2001;8(4):338–345. [Google Scholar]
- 29.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: a controlled trial. J Consult Clin Psychol. 1996;64(2):333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- 30.Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. J Am Med Assoc. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khanna MS, Kendall PC. Computer-assisted CBT for child anxiety: The coping cat CDROM. Cogn Behav Pract. 2008;15(2):159–165. [Google Scholar]
- 32.Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. J Consult Clin Psychol. 2010;78(5):737–745. doi: 10.1037/a0019739. [DOI] [PubMed] [Google Scholar]
- 33.Treatment for Adolescents with Depression Study Team. Fluoxetine, Cognitive- Behavioral Therapy, and Their Combination for Adolescents With Depression: Treatment for Adolescents With Depression Study (TADS) Randomized Controlled Trial. J Am Med Assoc. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 34.Galla BM, Wood JJ, Chiu AW, Langer DA, Jacobs J, Ifekwunigwe M, et al. One year follow-up to modular cognitive behavioral therapy for the treatment of pediatric anxiety disorders in an elementary school setting. Child Psychiatry Hum Dev. 2012;43(2):219–226. doi: 10.1007/s10578-011-0258-x. [DOI] [PubMed] [Google Scholar]
- 35.Ginsburg GS, Becker KD, Drazdowski TK, Tein J-Y. Treating anxiety disorders in inner city schools: Results from a pilot randomized controlled trial comparing CBT and usual care. Child Youth Care For. 2012;41(1):1–19. doi: 10.1007/s10566-011-9156-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manassis K, Wilansky-Traynor P, Farzan N, Kleiman V, Parker K, Sanford M. The feelings club: Randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress Anxiety. 2010;27(10):945–952. doi: 10.1002/da.20724. [DOI] [PubMed] [Google Scholar]
- 37.March S, Spence SH, Donovan CL. The efficacy of an Internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J Pediatr Psychol. 2009;34(5):474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- 38.Santucci LC, Ehrenreich JT, Trosper SE, Bennett SM, Pincus DB. Development and preliminary evaluation of a one-week summer treatment program for separation anxiety disorder. Cogn Behav Pract. 2009;16(3):317–331. doi: 10.1016/j.cbpra.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spence SH, Donovan CL, March S, Gamble A, Anderson RE, Prosser S, et al. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J Consult Clin Psychol. 2011;79(5):629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- 40.Weersing VR, Gonzalez A, Campo JV, Lucas AN. Brief behavioral therapy for pediatric anxiety and depression: Piloting an integrated treatment approach. Cogn Behav Pract. 2008;15(2):126–139. [Google Scholar]
- 41.Kendall PC, Khanna MS, Edson A, Cummings C, Harris SM. Computers and psychosocial treatment for child anxiety: Recent advances and ongoing efforts. Depress Anxiety. 2011;28(1):58–66. doi: 10.1002/da.20757. [DOI] [PubMed] [Google Scholar]
- 42.Elkins RM, McHugh RK, Santucci LC, Barlow DH. Improving the transportability of CBT for internalizing disorders in children. Clin Child Fam Psychol Rev. 2011;14(2):161–173. doi: 10.1007/s10567-011-0085-4. [DOI] [PubMed] [Google Scholar]
- 43.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: 1994. [Google Scholar]
- 44.Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 45.March JS, Parker JDA, Sullivan K, Stallings P. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 46.Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 47.Kovacs M. Children's Depression Inventory (CDI) Manual. New York: Multi-Health Systems, Inc.; 1992. [Google Scholar]
- 48.Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatr. 1981;46(56):305–315. [PubMed] [Google Scholar]
- 49.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 50.Achenbach TM. Manual for Child Behavior Checklist/4-18 and-1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 51.Kendall PC, Khanna MS. Camp Cope-A-Lot DVD. Ardmore, PA: Workbook Publishing; 2008. [Google Scholar]
- 52.Beidas RS, Benjamin CL, Puleo CM, Edmunds JM, Kendall PC. Flexible applications of the Coping Cat program for anxious youth. Cogn Behav Pract. 2010;17(2):142–153. doi: 10.1016/j.cbpra.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pavlou E, Gkampeta A. Learning disorders in children with epilepsy. Childs Nerv Syst. 2011;27(3):373–379. doi: 10.1007/s00381-010-1321-9. [DOI] [PubMed] [Google Scholar]
- 54.Institute of Medicine (IOM) Epilepsy across the spectrum: Promoting health and understanding. Washington, DC: 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Engel NA, Rodrigue JR, Geffken GR. Parent-child agreement on ratings of anxiety in children. Psychol Rep. 1994;75(3, Pt 1):1251–1260. doi: 10.2466/pr0.1994.75.3.1251. [DOI] [PubMed] [Google Scholar]
- 56.Barbosa J, Tannock R, Manassis K. Measuring anxiety: Parent-child reporting differences in clinical samples. Depress Anxiety. 2002;15(2):61–65. doi: 10.1002/da.10022. [DOI] [PubMed] [Google Scholar]
- 57.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101(2):213–232. [PubMed] [Google Scholar]
- 58.Comer JS, Kendall PC. A Symptom-Level Examination of Parent-Child Agreement in the Diagnosis of Anxious Youths. J Am Acad Child Adolesc Psychiatry. 2004;43(7):878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- 59.Muris P, Merckelbach H, Van Brakel A, Mayer B. The revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R): Further evidence for its reliability and validity. Anxiety, Stress Coping. 1999;12(4):411–425. doi: 10.1080/10615809908249319. [DOI] [PubMed] [Google Scholar]
- 60.Cosi S, Canals J, Hernández-Martinez C, Vigil-Colet A. Parent–child agreement in SCARED and its relationship to anxiety symptoms. J Anxiety Disord. 2010;24(1):129–133. doi: 10.1016/j.janxdis.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 61.Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following pediatric brain injury. J Consult Clin Psychol. 2006;74(3):445–454. doi: 10.1037/0022-006X.74.3.445. [DOI] [PubMed] [Google Scholar]
- 62.Kendall PC, Khanna MS. CBT4CBT: Computer-Based Training to Become a Cognitive-Behavioral Therapist DVD. Ardmore, PA: Workbook Publishing Inc.; 2008. [Google Scholar]