Abstract
Noting inappropriate uses of piperacillin/tazobactam at their institution, the authors emphasize the need for antimicrobial stewardship efforts, as well as infection-control practices, to curtail drug resistance, reduce costs, and minimize adverse events.
INTRODUCTION
The increase in global antimicrobial resistance presents a major health concern and drastically affects patient outcomes.1–3 The frequency of inappropriate use of antimicrobial agents is often used as a surrogate marker for its impact on antimicrobial drug resistance.1 Several studies have focused on the inappropriate use of broad-spectrum antimicrobials. In a study by Thuong et al., piperacillin/tazobactam (Zosyn, Wyeth/Pfizer) was used inappropriately 17% of the time; vancomycin (Vancocin, ViroPharma), 7%, of the time; and ciprofloxacin (Cipro, Bayer), 60% of the time.4 In that study, appropriateness was assessed according to the following criteria: the initial antibiotic choice according to hospital guidelines, antibiotic selection according to the clinical situation and microbiological information, proper duration of therapy, and re-evaluation and adaptation of therapy.4 Inappropriate use of antibiotics, coupled with the decline in the emergence of new antimicrobial entities, has led to the need for more judicious use of antimicrobials.1,5
ANTIMICROBIAL STEWARDSHIP
The Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA) have published guidelines to improve antimicrobial stewardship. The goals of these stewardship programs is to optimize patient outcomes and to reduce collateral damage, such as Clostridium difficile infections and the emergence of antibiotic-resistant bacteria.1 Another aim is to lower health care costs without adversely affecting standards of care.1 Successfully implemented stewardship programs have achieved a decrease in antimicrobial use by 22% to 36%, with annual savings of $200,000 to $900,000.1,6,7
A multidisciplinary team approach to antimicrobial stewardship is recommended as follows. Core members should include an infectious-disease physician and a clinical pharmacist with training in this area; a clinical microbiologist; an infection-control specialist and a hospital epidemiologist; an information system specialist; and a hospital administrator.1,7 Infection control also plays a vital role in preventing the spread of resistant organisms. Examples of infection-control practices include hand hygiene; isolation of the patient; and cleaning procedures, including sterilization and disinfection of surgical equipment, patient rooms, and patient-care areas.1
Various strategies have been proposed for antimicrobial stewardship programs. Some of these include staff education, formulary restrictions, formulary substitutions, antimicrobial cycling, early parenteral-to-oral conversion, use of optimal antibiotic doses, and multidisciplinary development of evidence-based practice guidelines that take into account local microbiology and resistance patterns.1,7
Piperacillin/tazobactam is a beta-lactam/beta lactamase inhibitor with coverage against gram-negative organisms (including Pseudomonas aeruginosa), gram-positive organisms, and anaerobic bacterial organisms. P. aeruginosa is a gram-negative, non–lactose-fermenting rod that is resistant to multiple agents. Infections caused by this pathogen can be very challenging to treat.8 Few drugs have reliable activity against this pathogen. Piperacillin/tazobactam is one of these agents, and its appropriate use is essential to decrease the development of resistance.
Piperacillin/tazobactam use has been evaluated in several studies. Raveh et al. found that the appropriateness rate of piperacillin/tazobactam use in their study hospital was 90%.9 Appropriateness was defined as antibiotics that were prescribed according to institution guidelines, treatment targeted according to susceptibility data, and drug therapy recommended by an infectious-diseases consultant.9
Antoine et al. conducted a study to investigate the knowledge, attitudes, and behaviors of house staff and faculty concerning piperacillin/tazobactam use at four hospitals in Atlanta, Georgia.10 Reviewing 163 patient charts to determine the appropriateness of piperacillin/tazobactam use, they found that the medication was used correctly only 71% of the time. In this study, appropriateness was evaluated based on the FDA-approved indication. Inappropriate indications included penicillin allergy, contaminated culture, bacterial colonization (which might not cause infection), infection with a pathogen for which resistance to piperacillin/tazobactam has been documented, community-acquired pneumonia (CAP) without complications, community-acquired urinary tract infections (UTIs), uncomplicated pancreatitis, and suspected intra-abdominal infections of mild-to-moderate severity.
To use antibiotics judiciously, our institution has developed drug-use guidelines for several antibiotics, including vancomycin, aminoglycosides, tigecycline (Tygacil, Wyeth/Pfizer), micafungin (Mycamine, Astellas), and voriconazole (Vfend, Pfizer). Because of a lack of institution-specific guidelines for the use of piperacillin/tazobactam, we completed a medicationuse evaluation (MUE) of this broad-spectrum antimicrobial to determine how appropriately it was being used in our community health system.
METHODOLOGY
We conducted a retrospective chart review of patients who received piperacillin/tazobactam at our hospital health system. The health system comprises four acute-care hospitals, a medical group, a research institute, and a foundation. Computerized prescriber order entry (CPOE) and electronic medical records (EMRs) are used. Our study was exempt from investigational review board approval because it was considered a quality-improvement project.
Our study period covered the months of April 2011 through June 2011. We identified more than 500 patients who received piperacillin/tazobactam during this period. We evaluated 200 randomly selected patient charts, 50 charts at each hospital. We collected the following data by reviewing individual patient charts: patient demographics, empirical indication for piperacillin/tazobactam use (determined from physician progress notes), dose and duration of antibiotic therapy, culture and sensitivity results, concomitant antibiotics, total length of stay (LOS) in the hospital, and whether or not an infectious-diseases specialist was consulted. The primary endpoint of overall appropriateness was evaluated based on empirical indication, dose, and de-escalation of the antimicrobial regimen.
A chi-square test was used for the comparison of categorical variables (i.e., appropriateness among the four hospitals). A P value of less than 0.05 was regarded as statistically significant. We performed the statistical analysis using SAS software, version 9.2.
The following criteria were used to determine the appropriateness of piperacillin/tazobactam use:
- Adequacy of initial antibiotic choice. Empirical therapy with piperacillin/tazobactam was considered appropriate based on the following indications (IDSA disease-state guideline or prescribing information recommendations):11–14
- Late-onset hospital-acquired pneumonia (HAP), health care–associated pneumonia (HCAP), and ventilator-associated pneumonia (VAP)
- Community-acquired pneumonia (CAP) if P. aeruginosa is a consideration (e.g., in patients with bronchiectasis, chronic oral steroid use, or late HIV infection)
- Febrile neutropenia
- Intra-abdominal infections
- Septic shock
- Moderate-to-severe infections: appendicitis, skin and soft-tissue infections (SSTIs), peritonitis, pelvic inflammatory disease, and puerperal endometritis
Appropriate dose as recommended by the prescribing information. We evaluated the dose only if the empirical therapy with piperacillin/tazobactam was considered appropriate.
Re-evaluation and adaptation of therapy after cultures and sensitivities are obtained. The regimen was appropriately de-escalated, if necessary, or an alternative antibiotic was selected if the organism was not susceptible to piperacillin/tazobactam.
RESULTS
Baseline characteristics of the study population are shown in Table 1. Serum creatinine levels, white blood cell (WBC) counts, and temperature were obtained on the day of initiation of piperacillin/tazobactam therapy. The empirical indications for which piperacillin/tazobactam was prescribed are presented in Table 2. HCAP made up the majority (22.5%) of these indications.
Table 1.
Basic Characteristics of the Study Population (200 Patients) at Northshore University HealthSystem
| Mean patient age | 73.3 years |
Antibiotic allergies (No.)
|
|
| Sex | 53.5% male |
| Mean white blood cell count | 13.2 × 103 cells/mm3 |
| Mean temperature | 99.1°F |
| Mean height | 166.7 cm |
| Mean weight | 75.6 kg |
| Mean serum creatinine, excluding patients receiving peritoneal dialysis or hemodialysis | 1.4 mg/dL |
| Mean duration of piperacillin/tazobactam treatment | 4.8 days |
| Mean length of hospital stay | 10.2 days |
| Percentage of patients consulting an infection-disease specialist | 24% |
Table 2.
Empirical Indications for Which Piperacillin/Tazobactam Was Prescribed
| Indication | No. of Patients |
|---|---|
| Health care–associated pneumonia | 45 |
| Sepsis | 35 |
| Community-acquired/aspiration pneumonia | 23 |
| Hospital-acquired pneumonia | 22 |
| Intra-abdominal infection | 18 |
| Skin and soft-tissue infection | 13 |
| Organ perforation | 11 |
| Urinary tract infection | 9 |
| Fever of unknown origin | 7 |
| Diverticulitis | 4 |
| Other (preoperative diarrhea, sinusitis, and Ludwig’s angina) | 4 |
| Neutropenic fever | 2 |
| Empyema | 2 |
| Osteomyelitis | 1 |
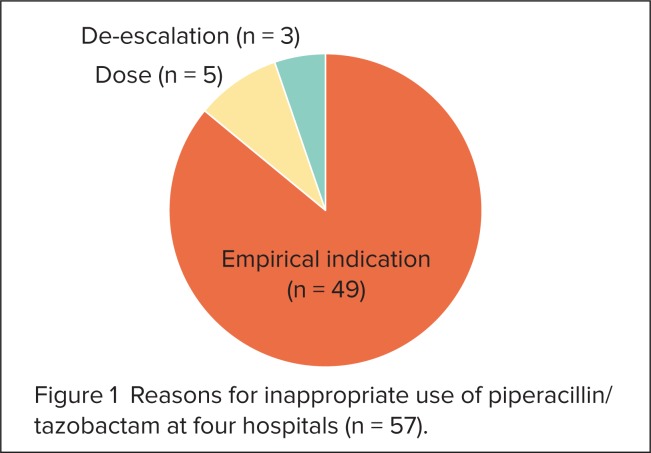
The three reasons for inappropriate use at all four hospitals (Figure 1) were empirical indication (86%), wrong dose (9%), concomitant antibiotics, and a failure to de-escalate the dose (5%).
Figure 1.
Reasons for inappropriate use of piperacillin/tazobactam at four hospitals (n = 57).
Empirical indication was a large contributor to the inappropriate use of piperacillin/tazobactam. For appropriate dose, there was no difference among the four hospitals (P = 0.681). However, differences in appropriate de-escalation and initial empirical therapy were statistically significant among the hospitals (P < 0.0001 and P = 0.0294, respectively).
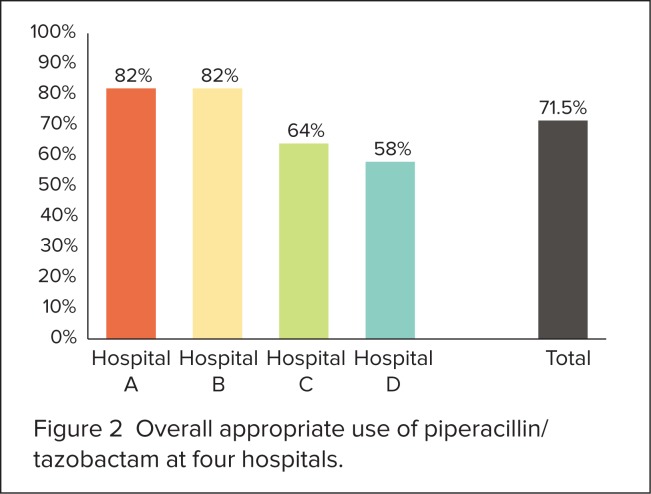
Overall rates of inappropriateness of antibiotic use differed among the four hospitals (P = 0.010); these rates are shown in Figure 2. The results are summarized in Table 3.
Figure 2.
Overall appropriate use of piperacillin/tazobactam at four hospitals.
Table 3.
Rates of Overall Appropriate Use of Piperacillin/Tazobactam at Four Hospitals
| Appropriateness Criteria | Hospital A | Hospital B | Hospital C | Hospital D | P Value |
|---|---|---|---|---|---|
| Empirical therapy | 43/50 (86%) | 42/50 (84%) | 34/50 (68%) | 33/50 (66%) | 0.0294 |
| Initial dose | 41/43 (95%) | 41/42 (98%) | 32/34 (94%) | 33/33 (100%) | 0.681 |
| Dose de-escalation | 31/31 (100%) | 22/22 (100%) | 25/25 (100%) | 10/18 (56%) | <0.0001 |
| Overall | 41/50 (82%) | 41/50 (82%) | 32/50 (64%) | 29/50 (58%) | 0.010 |
DISCUSSION
We sought to evaluate the appropriate use of piperacillin/tazobactam at a community health system. Our methods included a retrospective chart review of 200 randomly selected charts among four hospitals (i.e., 50 charts from each hospital). Appropriate use of piperacillin/tazobactam was based on three criteria: initial empirical therapy, dose, and appropriate targeted therapy.
We found that the overall appropriate use of piperacillin/tazobactam at all four hospitals was 71.5%. This rate differed among the hospitals (P = 0.010) and was lower than the benchmark study that we used (83%).4 Appropriateness rates for Hospitals A and B (82%) were higher than those for Hospital C (64%) and Hospital D (58%). When microbiology results were available, appropriate de-escalation of the microbial regimen was evident.
The IDSA and SHEA guidelines on antimicrobial stewardship recommend several elements to complement core antimicrobial stewardship strategies to optimize prescribing, including staff education, implementation of evidence-based order sets and clinical pathways, dose optimization, streamlined therapy, and parenteral-to-oral conversion.1 At our institution, approximately 86% of the inappropriate use of piperacillin/tazobactam was a result of its initial empirical selection. The high number of instances of inappropriate initial empirical selection of this agent is concerning.
Our university health system does not currently have guidelines for physicians and pharmacists regarding appropriate indications for the use of piperacillin/tazobactam. In addition to educating staff members about the appropriateness of this antimicrobial agent, creating and implementing guidelines for its use would be feasible interventions. Another medication-use evaluation could be performed a few months after these steps are implemented to assess the impact of these interventions.
STUDY LIMITATIONS
As in many retrospective studies, our study had several limitations. For one, we evaluated the appropriateness of piperacillin/tazobactam use retrospectively according to predefined criteria instead of assessing the appropriateness of its use at the time of clinical decision-making.
The criteria that we used to evaluate appropriateness were narrow; we could have also evaluated bacterial colonization, duration of therapy, and infection with a pathogen for which resistance to piperacillin/tazobactam had been documented. Length of therapy is difficult to assess, because antibiotic treatment should be tailored to each patient and the duration is dictated by the clinical course. However, incomplete therapy can lead to the re-emergence of infection and to patient re-admissions, whereas prolonged therapy can lead to unintended consequences such as C. difficile infection and the emergence of resistant bacteria.
Care should be exercised when these results are extrapolated to other practice settings because of differences in baseline antimicrobial stewardship practices.
CONCLUSION
Our results confirmed the tendency toward the inappropriate use of piperacillin/tazobactam at our institution, especially when the selection of treatment was based on initial empirical therapy. Given the concerns about the increasing occurrence of antimicrobial resistance, coupled with the decline in the emergence of new antimicrobial products, it is critical that broad-spectrum antibiotics, such as piperacillin/tazobactam, be used appropriately. Antimicrobial stewardship efforts, in addition to infection-control strategies (e.g., hand hygiene and isolation of the patient), present the best chance for curtailing drug resistance, for reducing costs, and for minimizing adverse events.
Footnotes
Disclosure: The authors report that they have no commercial or financial relationships in regard to this article.
REFERENCES
- 1.Dellit TH, Owens RC, McGowan JE, Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 2.Goff DA, Bauer KA, Reed EE, et al. Is the ‘low-hanging fruit’ worth picking for antimicrobial stewardship programs? Clin Infect Dis. 2012;55(4):587–592. doi: 10.1093/cid/cis494. [DOI] [PubMed] [Google Scholar]
- 3.Camins BC, King MD, Wells JB, et al. The impact of an antimicrobial utilization program on antimicrobial use at a large teaching hospital: A randomized controlled trial. Infect Control Hosp Epidemiol. 2009;30(10):931–938. doi: 10.1086/605924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thuong M, Shortgen F, Zazempa V, et al. Appropriate use of restricted antimicrobial agents in hospitals: The importance of empirical therapy and assisted re-evaluation. J Antimicrob Chemother. 2000;46:501–508. doi: 10.1093/jac/46.3.501. [DOI] [PubMed] [Google Scholar]
- 5.Armeni T. Antimicrobial stewardship. Pharmacist Lett Prescriber Lett. 2010;26(6):260613. [Google Scholar]
- 6.Ansari F, Gray K, Nathwani D, et al. Davey P. Outcomes of an intervention to improve hospital antibiotic prescribing: Interrupted time series with segmented regression analysis. J Antimicrob Chemother. 2003;52:842–848. doi: 10.1093/jac/dkg459. [DOI] [PubMed] [Google Scholar]
- 7.Ruttimann S, Keck B, Hartmeier C, et al. Long-term antibiotic cost savings from a comprehensive intervention program in a medical department of a university-affiliated teaching hospital. Clin Infect Dis. 2004;38(3):348–356. doi: 10.1086/380964. [DOI] [PubMed] [Google Scholar]
- 8.Fatima A, Nagvi SB, Khalig SA, et al. Antimicrobial susceptibility pattern of clinical isolates of Pseudomonas aeruginosa isolated from patients of lower respiratory tract infections. Springerplus. 2012;1(70):1–4. doi: 10.1186/2193-1801-1-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raveh D, Muallem-Zilcha E, Greenberg A, et al. Prospective drug utilization evaluation of three broad-spectrum antimicrobials: Cefepime, piperacillin–tazobactam, and meropenem. QJ Med. 2006;99:397–406. doi: 10.1093/qjmed/hcl050. [DOI] [PubMed] [Google Scholar]
- 10.Antoine TL, Curtis AB, Blumberg HM, et al. Knowledge, attitudes, and behaviors regarding piperacillin–tazobactam prescribing practices: Results from a multicenter study. Infect Control Hosp Epidemiol. 2006;27(11):1273–1277. doi: 10.1086/507973. [DOI] [PubMed] [Google Scholar]
- 11.Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: Guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:133–164. doi: 10.1086/649554. [DOI] [PubMed] [Google Scholar]
- 12.Niederman MS, Craven DE, Bonten MJ, et al. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 13.Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guidelines for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):e56–e93. doi: 10.1093/cid/cir073. [DOI] [PubMed] [Google Scholar]
- 14.Piperacillin/tazobactam (Zosyn), prescribing information. Philadelphia: Wyeth/Pfizer; 2012. [Google Scholar]