Abstract
Aims
International studies provide an opportunity to compare treatment approaches and outcomes. The present study compares elderly hospitalized acute myocardial infarction (AMI) patients in Minneapolis/St. Paul, USA (MSP) and Göteborg, Sweden (GB).
Methods and results
A population-based sample of hospitalized AMI (ICD-9 410) patients aged ≥75 in MSP and GB in 2001–02 was abstracted by trained nurses. Mortality was ascertained from medical records and death certificates. Demographics, cardiovascular procedures, and prescription medications were compared using sex-specific generalized linear models. Adjusted hazard ratios (HR) were calculated with Cox regression. In MSP 839 (387 men, 452 women) and in GB 564 (275 men, 289 women) patients were identified. Age was similar (men: MSP 83 ± 7, GB 82 ± 5; women: MSP 84 ± 6, GB 84 ± 6) yet MSP patients had more previous cardiovascular comorbidities and procedures (PCI/CABG). Guideline-based medication use was high in both locations. MSP patients were significantly more likely to undergo PCI (men: MSP 33%, GB 7%; women: MSP 30%, GB 7%). Survival at 7.5 years was 27.8% among MSP patients (men: 26.6%, women: 28.8%) and 17.2% among GB patients (men: 17.5%, women: 17.0%). After adjustment for baseline characteristics and guideline-based therapies, survival was higher among MSP men [HR: 0.66, 95% confidence interval (CI): 0.50–0.88] and women (HR: 0.49, 95% CI: 0.36–0.67) compared with GB.
Conclusion
In MSP and GB, guideline-based therapy use was high. However, PCI use was markedly higher in MSP. Long-term survival was better among elderly men and women in MSP compared with GB possibly related to greater utilization of PCI.
Keywords: Acute myocardial infarction, Elderly, International comparison
See page 3171 for the editorial comment on this article (doi:10.1093/eurheartj/eht263)
Introduction
International studies of medical practice provide an opportunity to compare treatment approaches and outcomes. The USA and Sweden are two medically advanced countries each with guideline-based treatment strategies for acute myocardial infarction (AMI).1–4 Improvements in short- and long-term mortality among hospitalized AMI patients have been observed in both areas.5–8 Several hypotheses have been proposed to explain these improvements. An overall reduction in population risk factors as well as advances in individual treatment are important factors in the overall decline in mortality in both the USA and Sweden.5,6
Medical treatment and outcomes in population-based samples of hospitalized AMI patients aged 30–74 in Minneapolis–St. Paul, USA (MSP), and Göteborg, Sweden (GB) have been compared previously.9,10 Major differences in AMI treatment approaches were observed during each survey period, 1990–91 and 1995–96, nevertheless short- and long-term mortality were similar in MSP and GB. The most recent survey, 2001–02, included AMI patients aged 75 and older, providing an opportunity to study acute treatment and long-term survival among elderly AMI patients. We hypothesized that treatment and long-term outcomes for AMI patients differed between these developed countries.
Methods
Study population and sample
The seven-county metropolitan area of MSP had a 2000 census population of 2.6 million inhabitants, including 44 243 men and 81 249 women 75 years of age and older. The population of MSP is mainly white and predominantly of northern European descent (Norwegian, Swedish, and German). The city of GB, on Sweden's west coast, had a 2002 population of 474 572, mainly ethnic Swedes (81%) with diverse immigrants accounting for the remainder of the population; the population 75 years of age and older included 14 752 men and 26 024 women.
From July 2001 through June 2002 hospitalized AMI discharges among residents of MSP and GB who were 30 years of age and older were identified; the present analysis focuses on the elderly, those aged 75 years and older. In MSP, complete computerized discharge lists were provided by each hospital and a random sample of the 1226 AMI hospitalizations (ICD-9 code 410) was selected. Medical records for 50% of men and 100% of women were sampled. Repeat hospitalizations during the same year were excluded. The sampling frame was guided by planned over-sampling of women and budget constraints. In GB, medical records for all hospitalized AMI patients during the same time period were abstracted. Acute myocardial infarction patients were eligible for inclusion in this study if they had chest pain and at least one cardiac biomarker value (CK-MB or troponin) more than twice the upper limit of normal.
Trained nurses, supervised by physicians, abstracted information on medical history, signs and symptoms, cardiac procedures, cardiac enzyme levels, electrocardiograms, clinical complications, and treatment from patient medical records. Vital status at the time of hospital discharge was obtained from the medical record and after hospital discharge from computer linkage with death certificate files provided by the Minnesota Department of Health and the Swedish National Registry. In Minnesota, based on the previous unpublished work, we know that the Minnesota Department of Health has complete death certificate records. In Sweden, survival confirmation as well as date of death for those who died were obtained from the Swedish National Population Registry. All-cause mortality was ascertained through 7.5 years following hospitalization. The study protocol complies with the Declaration of Helsinki and the Institutional Review Board at each study site approved the protocol.
Hospital facilities
Of the 22 acute care hospitals in MSP 21 participated in this project (all except one small rural facility). All of the participating hospitals had intensive care units for AMI treatment, most had cardiologists providing care and 12 hospitals had angioplasty/PCI facilities. These 12 hospitals account for 76% of primary AMI admissions and transfer to these facilities is readily available.
The two acute care hospitals in GB (Sahlgren's Hospital and Östra Hospital), each serving half of the city, participated. Most patients were admitted to the coronary care unit and received treatment from fully trained cardiologists, cardiologists in training, or internal medicine physicians doing required 6-month cardiology training. Cardiac catheterization was performed at both facilities but only one provided those services 24 h a day, 7 days a week. Transfer to that hospital was readily available.
Statistical analysis
Patient characteristics, cardiovascular procedures, and in-hospital and discharge prescription medications were compared between MSP and GB AMI patients using sex-specific generalized linear regression models. The Kaplan–Meier survival analysis was used for an unadjusted comparison of mortality. Cox proportional hazards regression was utilized for adjusted survival analyses. Potential covariates include baseline characteristics and guideline-based treatments. All analyses were pre-specified sex-specific and weighted by the inverse of the sampling fraction. Reported P-values are two-tailed and an α level of 0.05 was used to assess statistical significance. All statistical analyses were performed with SAS software (version 9.2; SAS Institute, Inc, Cary, NC, USA).
Results
Baseline characteristics
A total of 3279 hospitalized AMIs, 2311 among MSP residents and 968 among GB residents were identified; overall 1403 hospitalized AMIs (MSP n = 839, GB n = 564) occurred among residents 75 years of age and older. Of the 1403 hospitalized AMIs, 662 occurred among men (MSP n = 387, GB n = 275) and 741 occurred among women (MSP n = 452, GB n = 289). The age distribution in MSP and GB was similar among men as well as among women. However, patients in MSP had significantly more prior cardiovascular comorbidities (Table 1). Notably, despite a similar prevalence of prior myocardial infarction among MSP and GB patients, more than twice as many MSP patients had had a previous coronary procedure (PCI/CABG).
Table 1.
Sex-specific baseline characteristics of hospitalized acute myocardial infarction patients in Göteborg, Sweden and Minneapolis–St. Paul, USA
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| MSP (n = 387) | GB (n = 275) | P-value | MSP (n = 452) | GB (n = 289) | P-value | |
| Age (mean ± SD) | 82.6 ± 7.3 | 82.1 ± 5.1 | 0.34 | 84.4 ± 5.7 | 83.9 ± 5.6 | 0.19 |
| Current smoker (%) | 8.0 | 12.7 | 0.07 | 6.4 | 9.4 | 0.15 |
| Prior history (%) | ||||||
| Myocardial infarction | 41.1 | 44.9 | 0.39 | 31.6 | 33.8 | 0.54 |
| Hypertension | 70.0 | 48.4 | <0.0001 | 81.6 | 58.8 | <0.0001 |
| Diabetes mellitus | 30.2 | 21.1 | 0.02 | 22.6 | 18.3 | 0.17 |
| Heart failure | 49.1 | 40.0 | 0.04 | 46.5 | 37.4 | 0.01 |
| Stroke | 23.0 | 17.8 | 0.16 | 19.9 | 20.4 | 0.87 |
| Cancer | 18.9 | 20.4 | 0.67 | 16.2 | 14.2 | 0.47 |
| PCI/CABG | 37.2 | 13.5 | <0.0001 | 21.2 | 8.3 | <0.0001 |
| Presentation symptoms (mean ± SD) | ||||||
| Systolic blood pressure | 142.9 ± 46.8 | 144.2 ± 34.1 | 0.66 | 146.3 ± 35.0 | 149.7 ± 36.7 | 0.21 |
| Heart rate | 86.7 ± 35.4 | 87.0 ± 24.1 | 0.88 | 87.5 ± 24.1 | 89.2 ± 24.0 | 0.36 |
PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
Diagnostic and therapeutic procedures
During the index hospitalization, diagnostic and therapeutic procedures as well as medication use differed between MSP and GB (Table 2). The use of invasive procedures was substantially more common in MSP; diagnostic coronary angiography was significantly greater in MSP men (MSP: 49.4%, GB: 20.0%; P < 0.0001) and women (MSP: 43.1%, GB: 12.1%; P < 0.0001). Subsequently, large differences were observed in reperfusion treatment based on cardiac angiography. Utilization of PCI, following angiography, was more than four times as common among MSP men compared with GB men (MSP: 32.8%, GB: 7.3%; P < 0.0001). The differential use of PCI was similar among women (MSP: 29.4%, GB: 6.6; P < 0.0001). Guideline-based medication use was high but differed modestly between MSP and GB. β-Blockers were prescribed more often in GB, while aspirin and ACE inhibitors were more common in MSP. The differential use of duel anti-platelet therapy between men and women in MSP and GB paralleled the differences in PCI.
Table 2.
Diagnostic and therapeutic procedures during hospitalization with acute myocardial infarction in Göteborg, Sweden and Minneapolis–St. Paul, USA
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| MSP (n = 387) | GB (n = 275) | P-value | MSP (n = 452) | GB (n = 289) | P-value | |
| ST-elevation MI | 20.9 | 34.9 | 0.0002 | 32.5 | 41.2 | 0.02 |
| Diagnostic procedures (%) | ||||||
| Coronary angiography | 49.4 | 20.0 | <0.0001 | 43.1 | 12.1 | <0.0001 |
| Echocardiography | 52.2 | 48.7 | 0.43 | 60.8 | 38.8 | <0.0001 |
| Exercise test | 8.3 | 13.5 | 0.05 | 9.1 | 6.6 | 0.24 |
| Therapeutic procedures (%) | ||||||
| PCI | 32.8 | 7.3 | <0.0001 | 29.4 | 6.6 | <0.0001 |
| Primary PCI | 78.0 | 88.9 | 0.43 | 78.9 | 68.4 | 0.31 |
| CABG | 7.5 | 6.9 | 0.80 | 3.8 | 1.7 | 0.11 |
| Medication (%) | ||||||
| Thrombolysis | 3.6 | 6.9 | 0.07 | 4.6 | 8.0 | 0.06 |
| Aspirin | 93.3 | 86.5 | 0.01 | 93.4 | 87.2 | 0.004 |
| Anti-platelet agents | 48.3 | 12.0 | <0.0001 | 48.9 | 12.1 | <0.0001 |
| β-Blockers | 79.1 | 86.5 | 0.03 | 82.1 | 88.2 | 0.02 |
| Calcium-channel blockers | 34.4 | 17.1 | <0.0001 | 35.6 | 20.8 | <0.0001 |
| Nitrates | 86.6 | 56.0 | <0.0001 | 86.5 | 51.6 | <0.0001 |
| Digitalis | 21.2 | 21.1 | 0.98 | 20.1 | 26.0 | 0.06 |
| Diuretic | 68.2 | 68.7 | 0.90 | 72.3 | 73.0 | 0.84 |
| ACE-inhibitors | 57.6 | 41.5 | 0.0002 | 58.2 | 31.8 | <0.0001 |
| Heparin | 79.3 | 71.6 | 0.04 | 80.8 | 75.1 | 0.08 |
| Lidocaine | 5.7 | 0.7 | 0.01 | 5.3 | 0.0 | <0.0001 |
| Length of stay, daysa | 5.4 | 8.1 | <0.0001 | 5.7 | 7.6 | <0.0001 |
PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
aGeometric mean.
Discharge medications
Prescription of discharge medications paralleled in hospital use albeit at somewhat lower rates (Table 3). Guideline-based medication use was common among men and women in MSP and GB. Utilization of aspirin was high and similar in the two locations. The use of β-blockers was higher in GB, while the use of ACE inhibitors and lipid lowering agents was more common in MSP.
Table 3.
Prescription medications at discharge among hospitalized acute myocardial infarction patients in Göteborg, Sweden and Minneapolis–St. Paul, USA
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| MSP (n = 355) | GB (n = 235) | P-value | MSP (n = 424) | GB (n = 249) | P-value | |
| Medication (%) | ||||||
| Aspirin | 80.6 | 86.0 | 0.14 | 80.7 | 87.1 | 0.03 |
| Anti-platelet agents | 42.5 | 11.9 | <0.0001 | 42.0 | 12.9 | <0.0001 |
| β-Blockers | 73.8 | 85.1 | 0.01 | 74.5 | 86.7 | 0.0002 |
| Calcium-channel blockers | 22.0 | 14.5 | 0.05 | 21.5 | 16.9 | 0.15 |
| Nitrates | 66.5 | 47.2 | <0.0001 | 67.5 | 45.8 | <0.0001 |
| Digitalis | 15.5 | 12.3 | 0.35 | 15.1 | 16.5 | 0.64 |
| Diuretics | 45.1 | 62.6 | 0.002 | 50.9 | 67.9 | <0.0001 |
| ACE-inhibitors | 51.3 | 41.7 | 0.04 | 53.8 | 32.1 | <0.0001 |
| Lipid lowering agents | 51.8 | 35.9 | 0.001 | 44.8 | 23.7 | <0.0001 |
Mortality
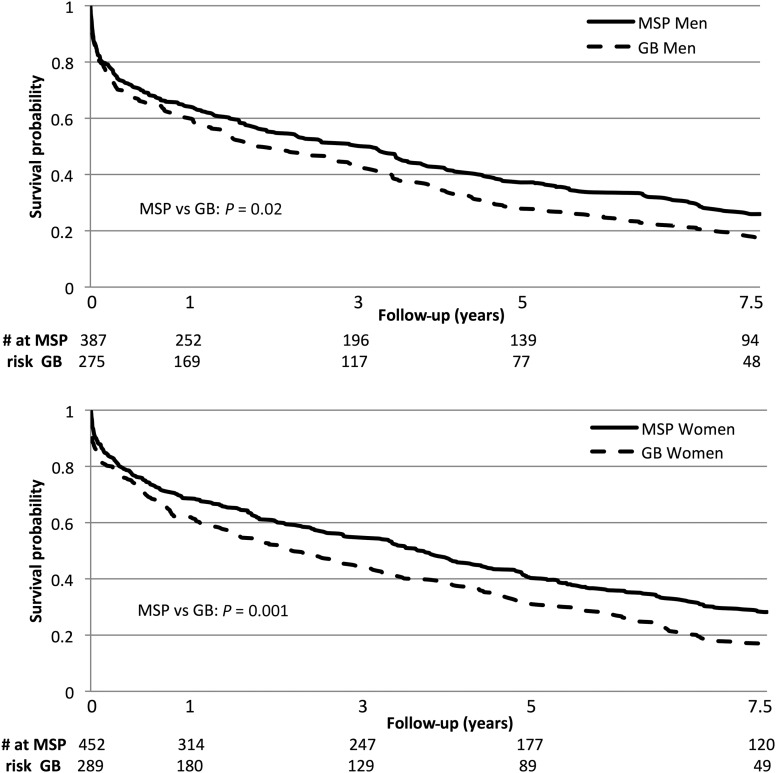
Survival at the end of the study, 7.5 years, was 27.8% among MSP patients (men: 26.6%, women: 28.8%) and 17.2% among GB patients (men: 17.5%, women: 17.0%) (Figure 1). Mortality during the index hospitalization was 8.3 and 14.6% among men in MSP and GB, respectively; among women, the corresponding values were 6.2 and 13.8%. Mortality at 28 days was high and similar among men in MSP and GB at roughly 16.5% (P = 0.95). Among women, 28-day mortality followed a similar pattern, mortality in MSP was 11.3% and in GB was 15.6% (P = 0.09).
Figure 1.
Unadjusted sex-specific survival among hospitalized acute myocardial infarction patients in Göteborg, Sweden and Minneapolis–St. Paul, USA.
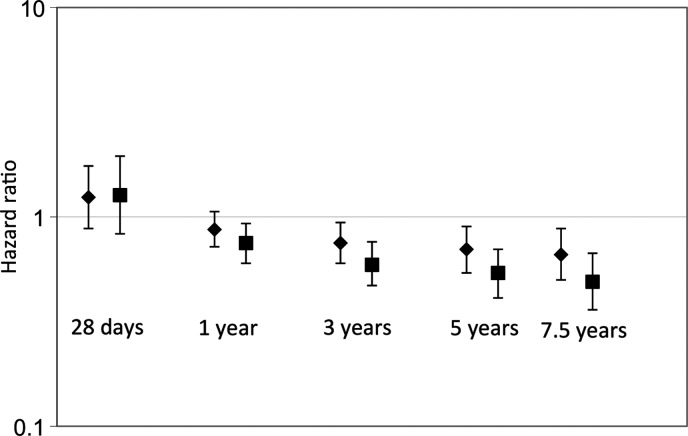
In an attempt to explain differences in mortality, multivariable adjusted models were created including covariates for baseline characteristics (age; history of hypertension, diabetes mellitus, heart failure, prior PCI/CABG) as well as guideline-based treatments (PCI; thrombolysis; in-hospital use of aspirin, β-blockers, and ACE inhibitors; discharge prescription of aspirin, β-blockers, ACE inhibitors, and lipid lowering agents) and type of AMI (STEMI or non-STEMI). The risk of death varied during follow-up between sites for men (P = 0.01) as well as women (P = 0.002) (Figure 2). After adjustment for covariates, at 7.5 years, mortality was superior among MSP men [hazard ratio (HR): 0.66, 95% confidence interval (CI): 0.50–0.88] and women (HR: 0.49, 95% CI: 0.36–0.67) compared with GB men and women, respectively. Further adjustment for in-hospital use and discharge prescription of anti-platelets yielded results consistent with the primary analysis. In a subgroup analysis, restricted to patients who underwent PCI, the multivariable adjusted hazard of mortality at 7.5 years was not statistically significantly different among men in MSP compared with GB (HR: 0.70, 95% CI: 0.37–1.34), or among women in MSP compared with GB (HR: 0.67, 95% CI: 0.32–1.41).
Figure 2.
Adjusted for age; history of hypertension, diabetes mellitus, heart failure, PCI/CABG; PCI; thrombolysis; in-hospital use of aspirin, β-blockers, and ACE inhibitors; discharge prescription of aspirin, β-blockers, ACE inhibitors, and lipid lowering agents. Reference: Göteborg, Sweden. Diamonds represent men and squares represent women.
Discussion
International comparisons can provide important information regarding medical therapy and outcomes, particularly when practices differ. The comparison of the USA and Sweden, each with sophisticated medical systems, offers unique insights into the treatment and long-term outcomes of hospitalized AMI patients.
Geographic variability in cardiovascular resource utilization is a well-documented phenomenon. A comparison of USA and Canadian patients in the GUSTO-1 trial found that revascularization rates during index hospitalization were nearly three times higher in the USA compared with Canada (angioplasty: USA 30.5% vs. 11.4%; bypass: USA 13.1% vs. 4.0%; P < 0.01 for both). After adjustment for baseline characteristics, enrolment in Canada was associated with a mortality HR of 1.17 (95% CI: 1.07–1.28; P = 0.001).11 The PURSUIT trial enrolled 10 948 patients with acute coronary syndromes, including 585 in Latin America and 4358 in North America.12 An invasive approach, including coronary angiogram, angioplasty, and bypass surgery, was utilized significantly more often in North America. After adjustment for baseline characteristics, enrolment in Latin America remained an independent predictor for death at 30 days and persisted at 6 months (odds ratio: 2.5; 95% CI: 1.8–3.4).12 In the ASSENT-2 trial, countries were grouped into tertiles based on revascularization rates (<15, 15–39, >39%) and the association with 30-day and 1-year mortality rates were compared. After adjustment for baseline patient characteristics, 30-day and 1-year mortality were significantly lower in the countries with the highest revascularization rates; the HR for 1-year mortality in the intermediate tertile compared with the highest was 1.45 (95% CI: 1.08–1.95; P = 0.013) and for the lowest tertile compared with the highest was 1.32 (95% CI: 1.06–1.63; P = 0.012).13
Other international comparisons have described geographic differences in cardiovascular procedures but similar patient outcomes. The combined GUSTO-I and GUSTO-III analysis of US and Canadian acute ST-elevation MI patients documented a higher revascularization rate in the USA with comparable 30-day and 1-year mortality rates.14 While a study conducted in six countries found the rate of invasive cardiac procedures, catheterization and revascularization, to be highest in Brazil and the USA, intermediate in Canada and Australia, and lowest in Hungary and Poland. Despite wide variation in use of invasive procedures, mortality and myocardial infarction were similar in all countries. Higher rates of invasive procedures were associated with lower rates of refractory angina or readmission for unstable angina but with higher rates of stroke.15
In prior publications, we reported differences in baseline characteristics, with MSP patients being younger but reporting more prior cardiovascular comorbidities and coronary procedures (PCI/CABG), and utilization of different treatment approaches, with GB favouring β-blockers and MSP utilizing invasive reperfusion (PCI/CABG). However, short- and long-term mortality were similar.9,10 The differences in baseline characteristics and AMI management strategies persisted during the present survey among the young (data not shown) as well as the elderly.
Despite the fact that patients 75 years of age and older comprise between 27 and 34% of non-ST-elevation acute coronary syndrome registries, they comprise only approximately 10% of patients enrolled in clinical trials.1,16 As a result, clinical trials rarely report results in the elderly. Guideline-based care, including medications and invasive procedures, is known to be lower among elderly ACS patients.17 The Euroheart study, an international cohort study including ACS patients from 25 European countries, found that elderly ACS patients were less intensively treated than young ACS patients and had higher in-hospital mortality.18 However, there is evidence of benefit of an early invasive approach among patients 75 years of age and older.19,20 Moreover, a pooled analysis of PCI and CABG clinical registries in the USA indicated a simultaneous improvement in outcomes as the use of coronary revascularization among those 75 years and older increased.21 In a Canadian study of AMI patients at least 80 years of age, the use of PCI and CABG as well as guideline-based prescription medication increased over the study period. One-year mortality improved over time but only among those who underwent revascularization.22 An international comparison of care among ACS patients reported that among elderly participants, enrolment in a non-US region was associated with a lower likelihood of cardiac catheterization compared with enrolment in the USA.23 However, even after adjustment for patient region and additional covariates, the multivariable adjusted odds of catheterization for each year of advancing age were 0.85 (95% CI: 0.82–0.88).23
In the present study, elderly AMI patients in MSP had a higher prevalence of prior cardiovascular disease comorbidities and treatments. Guideline-based medication use was high but somewhat higher during hospitalization than at discharge. This finding could be due to the discovery of side effects or intolerance during hospitalization or a pre-existing prescription. Notably, the prescription of lipid-lowering agents at discharge was much higher in MSP compared with GB. During hospitalization, the use of diagnostic coronary angiography and PCI were drastically higher in MSP than GB for both men and women. Diagnostic angiography was uncommon among elderly GB patients and even fewer received angioplasty. The use of thrombolysis was slightly higher in GB compared with MSP. Long-term mortality was lower among MSP men and women compared with GB men and women, respectively.
There are several limitations of this study. First, it is a retrospective study with the potential for incomplete data collection. For example, our AMI algorithm included cardiovascular symptoms and cardiac biomarkers without the inclusion of ECG criteria. However, based on previous work, where ECGs were analysed, few additional cases were identified.9 This finding is corroborated by other studies showing that ECG findings only modestly contribute to AMI diagnosis in the absence of confirming enzymes.24 Second, medical history data are based on self-report. Compared with medical record review, self-report is known to result in over-reporting of some medical conditions, including hypertension.25 Third, in examining long-term mortality, we have no information on compliance with discharge medications or the medical care that patients received after their index hospitalization because of privacy regulations. As a result, in-hospital and discharge therapies are being used as a proxy for subsequent medical care. Fourth, as with most epidemiologic studies, the effect of residual or unmeasured confounding might explain our results.
In a population-based study comparing elderly AMI patients in MSP and GB, there were pronounced differences in the treatment of AMI, especially the use of invasive strategies (PCI) in MSP compared with a more conservative approach in GB. Long-term survival post-AMI hospitalization was superior among elderly men and women in MSP compared with GB possibly related to more patients undergoing PCI in MSP.
Conflict of interest: none declared.
Funding
This work was supported by National Institute of Health (R01 HL023727 to R.V.L. and A.K.B.; K08 HL083611 to A.K.B.; T32 HL07779 to L.G.S.).
References
- 1.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger D, Bax JJ, Auricchio A, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Knuuti J, Kolh P, McDonagh T, Moulin C, Poldermans D, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Torbicki A, Vahanian A, Windecker S, Achenbach S, Badimon L, Bertrand M, Botker HE, Collet JP, Crea F, Danchin N, Falk E, Goudevenos J, Gulba D, Hambrecht R, Herrmann J, Kastrati A, Kjeldsen K, Kristensen SD, Lancellotti P, Mehilli J, Merkely B, Montalescot G, Neumann FJ, Neyses L, Perk J, Roffi M, Romeo F, Ruda M, Swahn E, Valgimigli M, Vrints CJ, Widimsky P. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 2.Kushner FG, Hand M, Smith SC, Jr, King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 3.Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van 't Hof A, Widimsky P, Zahger D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 4.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Jr, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP, Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Zidar JP. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;57:e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Bjorck L, Rosengren A, Bennett K, Lappas G, Capewell S. Modelling the decreasing coronary heart disease mortality in Sweden between 1986 and 2002. Eur Heart J. 2009;30:1046–1056. doi: 10.1093/eurheartj/ehn554. [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 7.Kesteloot H, Sans S, Kromhout D. Dynamics of cardiovascular and all-cause mortality in Western and Eastern Europe between 1970 and 2000. Eur Heart J. 2006;27:107–113. doi: 10.1093/eurheartj/ehi511. [DOI] [PubMed] [Google Scholar]
- 8.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herlitz J, McGovern P, Dellborg M, Karlsson T, Duval S, Karlson BW, Lee S, Luepker RV. Comparison of treatment and outcomes for patients with acute myocardial infarction in Minneapolis/St. Paul, Minnesota, and Goteborg, Sweden. Am Heart J. 2003;146:1023–1029. doi: 10.1016/S0002-8703(03)00531-3. [DOI] [PubMed] [Google Scholar]
- 10.McGovern PG, Herlitz J, Pankow JS, Karlsson T, Dellborg M, Shahar E, Luepker RV. Comparison of medical care and one- and 12-month mortality of hospitalized patients with acute myocardial infarction in Minneapolis-St. Paul, Minnesota, United States of America and Goteborg, Sweden. Am J Cardiol. 1997;80:557–562. doi: 10.1016/s0002-9149(97)00421-9. [DOI] [PubMed] [Google Scholar]
- 11.Kaul P, Armstrong PW, Chang WC, Naylor CD, Granger CB, Lee KL, Peterson ED, Califf RM, Topol EJ, Mark DB. Long-term mortality of patients with acute myocardial infarction in the United States and Canada: comparison of patients enrolled in Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO)-I. Circulation. 2004;110:1754–1760. doi: 10.1161/01.CIR.0000142671.06167.91. [DOI] [PubMed] [Google Scholar]
- 12.Cohen MG, Pacchiana CM, Corbalan R, Perez JE, Ponte CI, Oropeza ES, Diaz R, Paolasso E, Izasa D, Rodas MA, Urrutia CE, Harrington RA, Topol EJ, Califf RM. Variation in patient management and outcomes for acute coronary syndromes in Latin America and North America: results from the Platelet IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy (PURSUIT) trial. Am Heart J. 2001;141:391–401. doi: 10.1067/mhj.2001.113216. [DOI] [PubMed] [Google Scholar]
- 13.Gupta M, Chang WC, Van de Werf F, Granger CB, Midodzi W, Barbash G, Pehrson K, Oto A, Toutouzas P, Jansky P, Armstrong PW. International differences in in-hospital revascularization and outcomes following acute myocardial infarction: a multilevel analysis of patients in ASSENT-2. Eur Heart J. 2003;24:1640–1650. doi: 10.1016/s0195-668x(03)00433-0. [DOI] [PubMed] [Google Scholar]
- 14.Chang WC, Fu Y, Ohman EM, Gupta M, Morris A, Roth SN, Granger CB, Califf RM, Topol EJ, Mark DB, Armstrong PW. Temporal evolution in the management of acute ST elevation myocardial infarction: the seven-year GUSTO experience from Canada and the United States. The North American GUSTO-I and GUSTO-III investigators. Can J Cardiol. 2000;16:1231–1239. [PubMed] [Google Scholar]
- 15.Yusuf S, Flather M, Pogue J, Hunt D, Varigos J, Piegas L, Avezum A, Anderson J, Keltai M, Budaj A, Fox K, Ceremuzynski L. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators. Lancet. 1998;352:507–514. doi: 10.1016/s0140-6736(97)11162-x. [DOI] [PubMed] [Google Scholar]
- 16.Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, Rich MW, Van de Werf F, White HD, Weaver WD, Naylor MD, Gore JM, Krumholz HM, Ohman EM. Acute coronary care in the elderly, part I: non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2549–2569. doi: 10.1161/CIRCULATIONAHA.107.182615. [DOI] [PubMed] [Google Scholar]
- 17.Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, Eagle KA, White K, Mehta RH, Knobel E, Collet JP. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2005;149:67–73. doi: 10.1016/j.ahj.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, Hasdai D. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 19.Bach RG, Cannon CP, Weintraub WS, DiBattiste PM, Demopoulos LA, Anderson HV, DeLucca PT, Mahoney EM, Murphy SA, Braunwald E. The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. Ann Intern Med. 2004;141:186–195. doi: 10.7326/0003-4819-141-3-200408030-00007. [DOI] [PubMed] [Google Scholar]
- 20.Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, Neumann FJ, Robertson DH, DeLucca PT, DiBattiste PM, Gibson CM, Braunwald E. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344:1879–1887. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 21.Peterson ED, Alexander KP, Malenka DJ, Hannan EL, O'Conner GT, McCallister BD, Weintraub WS, Grover FL. Multicenter experience in revascularization of very elderly patients. Am Heart J. 2004;148:486–492. doi: 10.1016/j.ahj.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 22.Page M, Doucet M, Eisenberg MJ, Behlouli H, Pilote L. Temporal trends in revascularization and outcomes after acute myocardial infarction among the very elderly. CMAJ. 2010;182:1415–1420. doi: 10.1503/cmaj.092053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexander KP, Newby LK, Bhapkar MV, White HD, Hochman JS, Pfisterer ME, Moliterno DJ, Peterson ED, Van de Werf F, Armstrong PW, Califf RM. International variation in invasive care of the elderly with acute coronary syndromes. Eur Heart J. 2006;27:1558–1564. doi: 10.1093/eurheartj/ehl067. [DOI] [PubMed] [Google Scholar]
- 24.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Smith B, Chu LK, Smith TC, Amoroso PJ, Boyko EJ, Hooper TI, Gackstetter GD, Ryan MA. Challenges of self-reported medical conditions and electronic medical records among members of a large military cohort. BMC Med Res Methodol. 2008;8:37. doi: 10.1186/1471-2288-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]