Summary
The autistic phenotype in Down syndrome (DS) is marked by a characteristic pattern of stereotypies, anxiety and social withdrawal. Our aim was to study adaptive behaviour in DS with and without autistic comorbidity using the Vineland Adaptive Behaviour Scales (VABS), the Childhood Autism Rating Scales (CARS) and the DSM IV-TR criteria.
We assessed 24 individuals and established three groups: Down syndrome (DS), DS and autistic disorder (DS-AD), and autistic disorder (AD).
The DS and DS-AD groups showed statistically significantly similar strengths on the VABS (in receptive and domestic skills).
The DS and DS-AD subjects also showed similar strengths on the CARS (in imitation and relating), differing significantly from the AD group.
The profile of adaptive functioning and symptoms in DS-AD seemed to be more similar to that found in DS than to the profile emerging in AD. We suggest that the comorbidity of austistic symptoms in DS hampered the acquisition of adaptive skills more than did the presence of DS alone.
Keywords: adaptive behaviour , autism , comorbidity , Down syndrome
Introduction
The literature suggests that there is a high incidence (1–11%) of comorbidity of autism spectrum disorders in Down syndrome (DS) ( 1 – 4 ) . Although it is widely believed that social interaction is a special strength in DS ( 5 , 6 ) , difficulties in social referencing ( 7 ) , aberrations in mutual gaze ( 8 ) , and a deficit in basic motivation for learning new skills ( 9 ) have been reported. Moreover, in DS there is an overlap of autism and obsessive compulsive behaviour ( 10 ) . Autistic disorder (AD) in DS ( 11 ) appears to be comprised of a distinctive set of aberrant behaviours, marked by a characteristic pattern of stereotypies, anxiety and social withdrawal.
The diagnosis of autism in DS is difficult, an important bias resulting from the existence of strong stereotypes as regards the perceived behaviour of subjects with DS: although children with DS tend to be considered sociable, good humoured and friendly, they are also perceived as stubborn, resistant to change, and showing obsessive personality traits. As a result, parents are more likely to under-report social deficit items, whereas professionals tend to attribute pervasive behaviours to the chromosomal abnormality and to intellectual disability (ID), rather than to a comorbidity with AD ( 1 ) .
Distinguishing, in DS, between autistic-type behaviours and behaviour associated with ID is crucial but also difficult, as children with DS and AD (DS-AD) are reported to be more cognitively impaired than DS subjects without AD ( 2 – 4 ) , and the question of the extent to which increased severity of ID influences the emergence of AD has not been answered ( 2 , 12 ) .
Several studies have shown a high incidence of associated medical factors in DS that may contribute to the co-morbid presence of AD. This may refer not to a single medical condition, but rather to an increased total number of all associated medical conditions ( 13 ) . Children with DS-AD have been described to show an increased frequency of neurological abnormalities such as seizures ( 14 , 15 ) , dysfunctional swallowing, severe hypotonia and motor delay, congenital heart diseases, gastrointestinal tract anomalies, ophthalmological disorders, pneumonia, and sleep apnoea ( 13 , 16 ) .
In a recent neuroimaging study ( 17 ) , DS-AD showed, in comparison to DS alone, increased volumes of white matter in the cerebellum and in the brainstem, which were significantly associated with a higher frequency of stereotypies. In AD, the cerebellum has been shown to present hypoplasia of the vermis and the hemispheres and a decrease in Purkinje cells, which has been hypothesised to be associated with weak connectivity along the cerebello-thalamo-cortical circuit ( 18 ) .
Moreover, in DS-AD, positive family histories of autistic spectrum disorders, speech problems, ID, and communication and learning deficits have been found to be more frequent than in DS alone ( 19 ) .
Research has consistently demonstrated that children with autism display deficits in adaptive functioning that extend beyond their cognitive deficits ( 20 ) . In high-functioning autism adaptive behaviour strongly correlates with autistic symptoms, whereas in low-functioning autism it correlates with cognitive skills; this suggests that IQ handicaps adaptive skills globally, but that autistic symptoms correlate with a specific adaptive profile. Several studies have focused on adaptive behaviour in subjects with autism ( 21 ) compared with individuals with ID not otherwise specified. Subjects with AD obtained lower scores on communication and on social skills and lower total scores, but recorded higher levels in daily living. They also showed a more variable communication and socialisation profile ( 22 , 23 ) .
In AD, growth in communication and daily living skills seemed to be related to IQ but growth in socialisation was not ( 24 ) . Significantly lower socialisation scores emerged as the intrinsic feature of AD in all studies.
In comparisons of individuals with DS versus AD, data on adaptive behaviour are concordant only with regard to social skills (consistently found to differ between the two groups), and are therefore not concordant for the domains of daily living, communication, global adaptive level, or overall profiles ( 25 – 27 ) .
Children with DS show significantly more advanced receptive communication, socialisation, interpersonal relationships, and play and leisure time skills than children with AD.
Moreover, there are consistent differences between children with ID who do or do not present autistic comorbidity.
In a recent study ( 2 ) , DS-AD individuals, compared with subjects with DS alone, showed significantly lower scores in all domains and in the adaptive behaviour composite. The level of cognitive functioning contributed substantially to the high scores on the Autism Diagnostic Interview – Revised (ADI-R). However, when the authors adjusted for cognition (using only non-verbal items), the differences between DS-AD and DS remained significant.
The Childhood Autism Rating Scale (CARS) was designed as a screening tool for use in the initial assessment and classification of autism. Studies concur in finding that the CARS has good reliability and validity, even when used by raters who are relatively naïve to autistic spectrum disorders ( 28 ) .
Our aim was to describe the behavioural phenotype in DS-AD and to look for differences in the adaptive behaviour profile between DS with and without AD using the Vineland Adaptive Behaviour Scales (VABS), the CARS and the DSM IV-TR criteria.
Materials and methods
Participants
All the participants came from three different regional health-care services in Italy: the IRCCS Stella Maris Foundation, Division of Child Neurology and Psychiatry at the University of Pisa (Pisa and Livorno), AIAS (Pistoia), and CEPS (Bologna). All individuals with autism were referred to the Pervasive Developmental Disorders study centre at the Stella Maris Institute. The inclusion criteria were: presence of DS and/or autism, living with the family, and exclusion of dementia and uncorrected metabolic disorders. Informed consent to participate in the study was provided by relatives after written information had been distributed and discussed. Ethics approval was obtained from the relative regional research ethics committees.
All the individuals were matched for age, sociocultural background, gender and ethnic group.
Measures
All subjects underwent a semi-structured psychiatric interview, a detailed medical and neuropsychiatric history and a complete clinical and neurological examination to look for any other medical conditions.
The adapted Italian version of the VABS ( 29 ) was administered to all individuals as a structured interview, conducted in the presence of the caregivers. The VABS is divided into four key domains (each in turn divided into three subdomains) and, of these, we used: 1) Communication (Receptive, Expressive, Written), 2) Daily Living Skills (Personal, Domestic, Community), and 3) Socialisation (Interpersonal Relationships, Play and Leisure Time, Coping).
The CARS ( 30 ) scoring was based on the observations, in both structured and non-structured situations, of a trained child neuropsychiatrist (SB or AD); these observations took from 30 to 60 minutes for each child. The CARS assesses behaviour in 14 domains that are generally affected by severe problems in autism, plus one general item of impressions of autism.
The 15 items in the scale are: relating to people, imitative behaviour, emotional response, body use, object use, adaptation to change, visual response, listening response, perceptive response, fear or anxiety, verbal communication, non-verbal communication, activity level, level and consistency of cognitive relations, and general impressions.
All the subjects were clinically diagnosed according to DSM-IV TR criteria by a child neuropsychiatrist (SB or AD) using clinical interviews, each lasting 1.5 hours, with parents and child, in a room equipped with age-appropriate play material.
Autistic semiology was assessed using the criteria of the DSM-IV TR; all the individuals in the AD and DS-AD groups met at least seven of the DSM-IV TR diagnostic criteria.
Cognitive abilities were tested by an experienced child neuropsychologist (VP) using Raven’s Coloured Progressive Matrices and the Wechsler Intelligence Scales Revised (WISC-R). In cases in which these scales could not be applied, e.g. in the presence of limited verbal interaction, the non-verbal Griffiths’ and Leiter scales were used.
Sociocultural background was evaluated considering the completed schooling of each parent (elementary school, high school, university or college degree).
Procedures
We established three groups: Group 1: children with DS, Group 2: children with DS and AD (DS-AD), Group 3: children with AD.
Vabs
Total adaptive behaviour composite scores and age-equivalent scores were calculated for all individuals.
To calculate areas of strength and areas of weakness, the VABS raw scores were converted into three levels of functioning (above average, or strong; average; below average, or weak) in relation to the average for this age group and considering three levels of ID (mild, moderate and severe), as suggested in the VABS manual.
Cars
The examiner assigned a score of 1 to 4 for each item: 1 indicates behaviour appropriate for the subject’s age, while 4 indicates a severe deviance from age-appropriate behaviour. The total score classifies the child as: not autistic (below 30, cut-off for diagnosis of childhood autism), mild or moderately autistic (30–36.5), or severely autistic (above 36.5).
For the assessment of severe autism, we followed the advice of the authors of the scale ( 30 ) , counting the number of items in which the child obtained a score equal to or greater than 3. A diagnosis of severe autism is appropriate when there are at least five such items.
Statistical analysis
Statistical analysis was conducted using SPSS for Windows 14.0. One-way ANOVA was performed for group differences and the Bonferroni test was used for post hoc analysis. For non-parametric data, we used the Pearson chi-square with cross-tabs.
Results
Patient characteristics
Twenty-four individuals (11 males and 13 females) participated in the study. Their mean age was 21.86±6.44 years (range: 6.83 to 34).
All the DS-AD individuals showed a free trisomy 21; of the subjects with DS alone, six showed a free trisomy 21, one showed a mosaicism and one showed a translocation (p=0.319). No chromosomal anomalies were found in the individuals with AD.
Six individuals (25%) had mild mental retardation, eight (33.3%) had moderate mental retardation, and 10 (41.7%) had severe mental retardation.
In the DS group, mental retardation was mild in 37.5%, moderate in 50% and severe in 12.5%.
In the AD group, mental retardation was mild in 37.5%, moderate in 25%, and severe in 37.5%.
In the DS-AD group, no subject showed mild mental retardation (0%), whereas mental retardation was moderate in 25% and severe in 75%.
The frequency of mild ID was significantly higher in the DS group and the AD group than in the DS-AD subjects, while the frequency of severe ID was significantly lower (p<0.05).
Associated medical conditions
Congenital heart malformations were present in three individuals (12.5%): two DS-AD subjects and one DS subject (Pearson’s chi-square, p=0.319).
Corrected late-onset hypothyroidism (after 10 years of age) was present in two individuals (8.3%): one DS-AD subject and one DS subject (p=0.58).
Coeliac disease was present in just one subject, affected by DS-AD (4.2%) (p=0.352).
A history of epilepsy was present in four individuals (16.7%): two DS-AD subjects, one DS subject and one AD subject (p=0.741). All of these individuals were seizure-free and not taking antiepileptic drugs; the seizures reported were complex partial seizures and no individual had shown infantile spasms.
A gastrointestinal tract disorder was present in one DS individual (4.2%) (p=0.352).
Other medical disorders were present in two individuals (8.3%): one DS-AD subject showed multiple dental agenesis and one DS subject had undergone tonsillectomy at the age of 5 years.
No focal neurological deficits were observed in any member of the entire series.
None of the DS subjects had a family history of an autism spectrum disorder.
As regards the total number of associated medical conditions, no disorder was present in 14 individuals (2 DS-AD, 5 DS and 7 AD), one disorder was present in seven individuals (5 DS-AD, 1 DS and 1 AD), and three disorders were present in three individuals (1 DS-AD and 2 DS). Significant differences in cross-tabs were only observed between DS-AD and AD (p=0.40), whereas DS-AD versus DS (p=0.117) and DS versus AD (p=0.311) did not show significant differences.
Ocular disorders (strabismus, astigmatism, myopia, hypermetropia and nystagmus) were observed only in subjects with DS: in four individuals with DS-AD and in five with DS alone (Pearson’s chi-square between DS and DS-AD p=0.614).
Cataract was present in four DS-AD subjects and in one DS individual (p=0.106).
VABS and CARS: group differences
Vineland Adaptive Behaviour Scales ( Table I , over)
Table I .
Vineland Adaptive Behaviour Scales: means of age-equivalent scores
| VABS n=24 | DS | p | DS-AD | p | AD | p |
|---|---|---|---|---|---|---|
|
| ||||||
| Mean age (years) ± SD | 21.68±8.30 | 20.78±9.9 | 20.06±3.25 | |||
| Gender M/F | 3/5 | Bonferroni | 4/4 | Bonferroni | 4/4 | Bonferroni |
|
Mean ± SD / p-values Post-hoc Bonferroni |
DS | DS vs DS-AD | DS-AD | DS-AD vs AD | AD | DS vs AD |
| Receptive | 6.93±2.49 | * 0.046 | 3.55±2.94 | – | 2.67±2.22 | ** 0.009 |
| Expressive | 5.60±1.94 | ** 0.001 | 1.58±0.67 | ** 0.016 | 4.53±2.56 | – |
| Written | 7.17±3.3 | – | 3.52±0.76 | – | 6.52±4.12 | – |
| COMMUNICATION | 6.78±2.84 | ** 0.009 | 2.16±0.95 | – | 5.07±3.80 | – |
| Personal | 5.90±2.18 | * 0.048 | 3.13±1.45 | – | 3.70±2.57 | – |
| Domestic | 10.63±3.26 | ** 0.001 | 5.40±2.43 | – | 4.5±1.32 | ** 0.000 |
| Community | 6.27±1.82 | * 0.002 | 2.85±0.61 | – | 4.57±2.37 | – |
| DAILY LIVING | 7.05±1.51 | ** 0.000 | 3.33±1.37 | – | 4.42±2.05 | * 0.014 |
| Interpers. relationships | 6.44±4.25 | ** 0.003 | 1.47±0.97 | – | 2.07±1.20 | ** 0.009 |
| Play and leisure | 6.48±3.81 | ** 0.004 | 1.65±0.85 | – | 2.66±2.43 | * 0.027 |
| Coping | 7.78±3.42 | ** 0.002 | 3.63±0.73 | – | 4.25±1.32 | * 0.011 |
| SOCIALISATION | 7.17±4.41 | ** 0.003 | 2.07±0.86 | – | 2.82±1.57 | * 0.014 |
| TOTAL VABS | 7.00±2.53 | ** 0.001 | 2.52±0.98 | – | 4.10±2.42 | * 0.035 |
The DS-AD subjects showed significantly lower scores than the DS individuals in all subdomains except written, where no group differences at all were found. Moreover, the DS-AD group recorded the lowest age-equivalent scores of all three groups in almost all subdomains; the only exceptions were receptive and domestic skills, where the individuals with AD showed lower scores, although these differences did not reach statistical significance. In the expressive subdomain, the DS-AD group scored significantly lower than the other two groups.
The DS group recorded significantly higher scores than the AD subjects in receptive, domestic, daily living, and in all the socialisation subdomains.
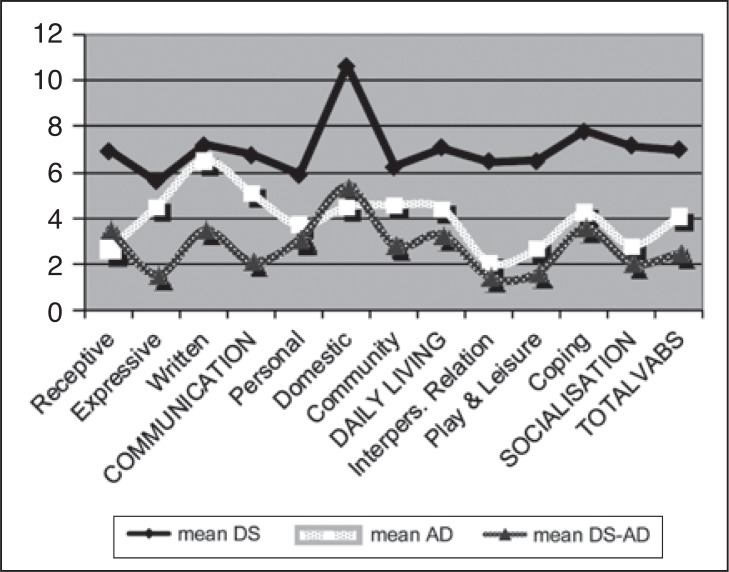
Adaptive Behaviour Profile ( figure 1 , over)
Figure 1 .
Profile of adaptive behaviour.
As regards the profile of adaptive behaviour in the three groups, the subdomain trajectories show that the DS and DS-AD children displayed largely same areas of strength (receptive and domestic skills) and weakness (expressive, interpersonal relationships, and community), even though the level of the profile was generally lower in the DS-AD children.
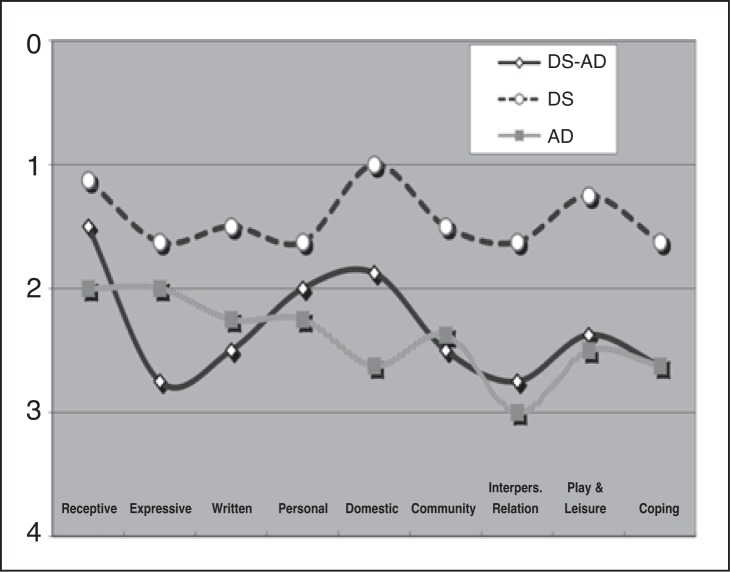
Adaptive functioning in different subdomains: areas of strength and weakness ( table II , fig. 2 , over)
Table II .
Adaptive functioning in different subdomains of the Vineland Adaptive Behaviour Scales: areas of strength and weakness
| DS | DS-AD | AD | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| in % | strong | average | weak | strong | average | weak | strong | average | weak |
| Receptive | 87.5 | 12.5 | 0.0 | 62.5 | 25 | 12.5 | 37.5 | 25 | 37.5 |
| Expressive | 50 | 37.5 | 12.5 | 0 | 25 | 75 | 37.5 | 25 | 37.5 |
| Written | 62.5 | 25 | 12.5 | 0 | 50 | 50 | 25 | 25 | 50 |
| Personal | 50 | 37.5 | 12.5 | 12.5 | 75 | 12.5 | 0 | 75 | 25 |
| Domestic | 100 | 0 | 0 | 50 | 12.5 | 37.5 | 0 | 37.5 | 62.5 |
| Community | 62.5 | 25 | 12.5 | 12.5 | 25 | 62.5 | 12.5 | 37.5 | 50 |
| Interpers. rel.s | 50 | 37.5 | 12.5 | 0 | 25 | 75 | 0 | 0 | 100 |
| Play & leisure | 75 | 25 | 0 | 12.5 | 37.5 | 50 | 12.5 | 25 | 62.5 |
| Coping | 37.5 | 62.5 | 0 | 0 | 37.5 | 62.5 | 0 | 37.5 | 62.5 |
Figure 2 .
Level of adaptive behaviour.
The majority of DS individuals, when adjusted for their IQ, showed above average scores (strengths) in almost all the subdomains (p<0.01, chi-square); only in coping was their adaptive functioning found to be average when adjusted for cognitive level.
The majority of DS-AD individuals showed strengths in the receptive and domestic subdomains (p<0.01, chi-square), average functioning in the written, expressive, community, and interpersonal relationships domains (p<0.01, chi-square), and below average functioning in play and coping (p<0.05, chi-square).
The majority of AD individuals showed average functioning in the receptive, expressive, and personal domains, whereas the written, domestic, community, interpersonal relationships (p<0.01, chi-square), play and coping domains (p<0.05, chi-square) were found to constitute areas of weakness.
Considering individual performances and not only means, in the personal subdomain no individual with AD showed above average adaptive functioning, whereas 12.5% of the DS-AD group did. Interpersonal relationships constituted an area of weakness for all individuals with AD, whereas 25% of the DS-AD subjects showed an average level of functioning in this domain.
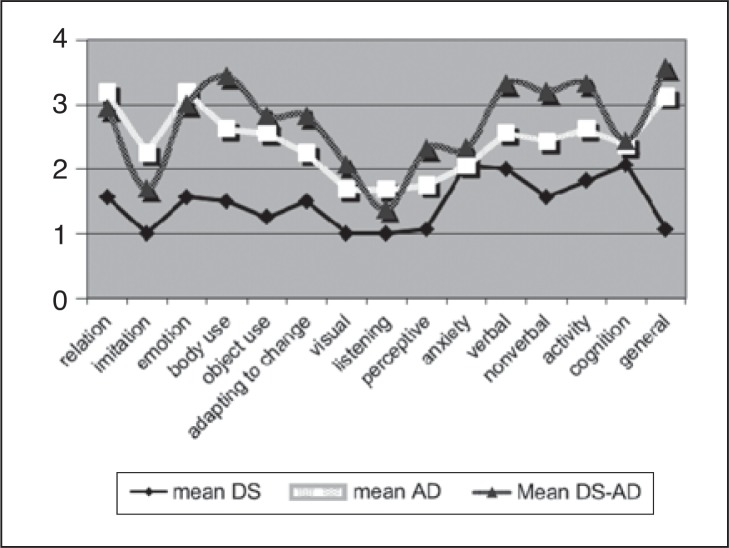
Cars ( table III , fig. 3 )
Table III .
Childhood Autism Rating Scales: mean scores and group differences
|
Mean±SD / p-values Bonferroni |
DS | DS vs DS-AD | DS-AD | DS-AD vs AD | AD | DS vs AD |
|---|---|---|---|---|---|---|
| CARS TOTAL | 21.81±2.01 | ** 0.000 | 40,37±4,94 | – | 36.56±3.86 | ** 0.000 |
| CARS relating | 1.56±0.32 | ** 0.000 | 2.93±0.62 | – | 3.19±0.25 | ** 0.000 |
| CARS imitation | 1.0±0 | ** 0.002 | 1.68±0.37 | * 0.011 | 2.25±0.46 | ** 0.000 |
| CARS emotion | 1.56±0.42 | ** 0.000 | 3.00±0.54 | – | 3.18±0.26 | ** 0.000 |
| CARS body use | 1.5±0.37 | ** 0.000 | 3.44±0.417 | * 0.002 | 2.62±0.44 | ** 0.000 |
| CARS object use | 1.25±0.37 | ** 0.000 | 2.81±1.03 | – | 2.56±0.42 | ** 0.003 |
| CARS change | 1.5±0.38 | ** 0.000 | 2.81±0.45 | * 0.035 | 2.25±0.38 | ** 0.004 |
| CARS visual | 1.0±0 | ** 0.000 | 2.06±0.62 | – | 1.68±0.25 | ** 0.006 |
| CARS listening | 1.0±0 | * 0.022 | 1.38±0.36 | – | 1.35±0.38 | ** 0.000 |
| CARS perceptive | 1.06±0.17 | ** 0.001 | 2.31±0.99 | – | 1.75±0.26 | – |
| CARS anxiety | 2.31±0.70 | – | 2.06±4.95 | – | 2.06±0.17 | – |
| CARS verbal | 2.0±0.53 | ** 0.000 | 3.31±0.17 | * 0.023 | 2.56±0.82 | ** 0.007 |
| CARS non-verbal | 1.56±0.32 | ** 0.001 | 3.18±0.53 | – | 2.43±0.62 | – |
| CARS activity | 1.81±0.53 | ** 0.000 | 3.31±0.37 | * 0.012 | 2.62±0.35 | ** 0.003 |
| CARS cognition | 2.06±0.17 | – | 2.43±0.17 | – | 2.37±0.69 | – |
| CARS general | 1.06±0.17 | ** 0.000 | 3.56±0.32 | * 0.022 | 2.37±0.69 | ** 0.000 |
Figure 3 .
Mean scores on CARS.
All the individuals with DS-AD and AD had a CARS score above 30 (cut-off for diagnosis of childhood autism), therefore the sensitivity of CARS was 100%.
All the DS individuals showed scores below 30 (mean 21.81±2.01). Within the other two groups the distribution of mild-to-moderate autism (scores between 30 and 36.5) and severe autism (scores above 36.5) was equal. In our sample, all children (n=8) with a total score greater than 36.5 also had more than five items with scores above or equal to 3. The DS-AD subjects had the highest scores in almost all domains.
The DS children scored lowest in almost all domains; only in anxiety did they score the highest.
The DS-AD group recorded significantly higher scores than the AD group in body use, adaptation to change, verbal communication, activity level and general impression (p<0.05).
The AD subjects had the highest scores only in relating, imitation (p<0.05), and emotion.
The DS differed from the AD group only in anxiety, cognition and non-verbal communication.
No differences were seen in cognition on the CARS. In all three groups the scores for anxiety symptoms and level of cognition were high.
Considering the group profiles, lower scores in relating, imitation, emotion, and visual response might be phenotypic for DS, given that the DS-AD showed a pattern similar to that of the DS subjects.
In the DS-AD subjects, body use, object use, adapting to change, listening response, perceptive response, verbal and non-verbal communication, and activity level seem to be more influenced by autistic symptoms than the other items.
Discussion
A specific pattern of functioning, phenotypic for DS and for DS-AD but different from AD alone, seemed to exist. Our results in AD were consistent with literature data reporting an area of weakness in socialisation and communication, a relative strength in daily living skills, and a more variable pattern than in DS ( 22 , 23 ) .
The DS-AD group exhibited significantly more autistic symptoms than the other groups, and the adaptive profile of these subjects seemed to be more similar to that of DS than to that of AD, albeit at a lower level. Areas of strength and weakness were by definition adjusted for cognitive levels, after which strengths in reception and in domestic skills persisted; in all other domains the DSAD subjects showed lower scores than those with AD or DS alone. The DS group showed higher scores overall than the AD group, and consistent with the literature, reception emerged as an area of strength, significantly different from AD ( 25 – 27 ) .
In reception, the AD group displayed the poorest performance of all three groups, with the greatest standard deviation.
In domestic skills, the DS-AD subjects showed a better performance than AD, probably due to higher skills in imitation and better relational skills (also observed in the CARS).
This confirmed our clinical impression that the DS-AD subjects were much more similar to the DS than to the AD subjects, especially in the CARS items relating and imitation. We suggest the comorbidity of autistic symptoms and DS hampered the acquisition of adaptive skills more than did the presence of DS alone.
The VABS investigates actual relationships with peers and these seemed to be more compromised in DS-AD, contrary to what the results of the CARS might suggest, where individuals with DS-AD performed better than those with AD.
These phenotypic strengths emerged, even at the low level of adaptive functioning, in domestic skills, emotional abilities, imitation, interpersonal relationships and coping. Through our diagnostic screening, we also observed that DS individuals without autism showed peculiar behavioural patterns, language stereotypes, rituals and specific interests in parts of objects and specific body use that could easily be mistaken for autistic symptoms, but are in our opinion part of a specific behavioural pattern in DS. We state that, for this reason, the dual diagnosis of AD in DS must take phenotypic behavioural features into account.
Specific autistic features in DS, as reported recently by the group of Capone and coworkers ( 11 , 31 ) can also be readily detected through widely used screening tools, such as the CARS. To use a screening tool in addition to the DSM IV-TR criteria seems to be important, as it is more accessible to a larger population in routine clinical practice.
Children with DS often have a considerable delay in diagnosis of AD ( 13 ) . Early diagnosis of AD increases successful therapies ( 32 ) , but diagnosis may be achieved later in DS-AD than in AD alone, as regression occurs later, with an onset between 3–8 years ( 33 ) ; this may result in inappropriate educational strategies.
We hypothesise that the early diagnosis of autism in DS is important for early operative strategies and interventions as described in the literature ( 13 , 20 ) , and that the main goals of early rehabilitation programmes in ID should be to prevent the overlap of symptoms of autistic spectrum disorders; the early appearance of stereotypical behaviour, isolation and a delay in communicative skills may lead towards an autistic spectrum disorder, particularly in children with DS.
For this reason, rehabilitation strategies for individuals with DS and the comorbidity with AD must address primarily autistic features rather than ID alone. In addition, to establish a meaningful rehabilitation goal, physical limitations and cognitive impairments must be considered together in all children, so that the relative interventions can be performed in tandem, as postulated in the literature ( 34 ) .
Moreover, we postulate that DS-AD subjects might be more stimulated through peers and social contact and that isolation in these individuals might be more easily broken by a stimulating environment. This relative strength in personal relationships has also been reported as a bias in diagnosis of autistic comorbidity in DS ( 1 ) .
To our knowledge, this study is the first attempt to compare the three groups: DS, DS-AD and AD.
A strength of our sample was the exclusion of other neuropsychiatric disorders such as dementia and uncorrected metabolic conditions. We confirmed literature data showing that no single medical condition is over-represented in DS-AD, and that DS-AD has the highest number of associated medical conditions ( 13 , 16 ) , significantly different only versus AD alone.
Seizure disorders were present in all three groups, but infantile spasms which are characterised by an age-dependent early onset and which have been described to play a crucial role in the development of autism in DS and in AD, were not present ( 14 , 35 ) . In accordance with literature data ( 36 ) , the incidence of ocular and refractive errors was high in both DS groups; cataract was higher in DS-AD, but without reaching statistical significance.
In the literature, instability of fixation and continuous changes in saccadic velocity have been described in autistic children ( 37 ) . In our AD group, however, these features were not observed.
The karyotype was not statistically different between the two DS groups, perhaps due to the small numbers. Previously we described better adaptive behaviour in domestic skills in DS individuals with mosaicism of chromosome 21 ( 38 ) .
Limitations are that this was a pilot study and that the study group was quite small. DS-AD individuals showed significantly poorer cognitive abilities, as reported in the literature ( 2 , 4 , 39 ) , but when we adjusted adaptive behaviour for cognitive level in calculating points of strength and points of weakness, the differences remained and levels of adaptive functioning were in this way comparable.
We suggest that greater cognitive disability is one of the main risk factors, in DS, for the development of autistic pathology, as proposed in the literature ( 2 , 31 , 39 ) .
A common mechanism underlying ID across multiple genetic syndromes is an abnormal development of neuronal network connectivity resulting in a deficit in information processing ( 40 ) , and AD ( 41 ) also represents a developmental disconnection syndrome. A recent study explains, in this way, the relatively high prevalence of AD in DS subjects who already show a neural network disconnectivity ( 2 ) .
In conclusion, an early diagnosis of AD in DS is important so that appropriate educational and therapeutic programmes and strategies can be offered, allowing children to achieve the best possible outcomes.
Children with a dual diagnosis of DS and AD may acquire abilities differently from children with DS alone and also show unusual and sometimes challenging behaviour.
Adaptive skills must be integrated into the diagnostic workup of patients with ID, as cognitive abilities alone cannot fully explain behaviour, and treatment strategies must be individualised according to actual functioning.
In order to evaluate, in DS-AD, the interaction of adaptive behaviour, cognitive abilities, and other associated medical conditions with functional treatment and psychiatric comorbidity we need to increase our study group and follow up our individuals over time.
Acknowledgments
We gratefully acknowledge the participation of the children and their families.
References
- 1. Kent L , Evans J , Paul M , Sharp M . Comorbidity of autistic spectrum disorders in children with Down syndrome . Dev Med Child Neurol . 1999 ; 41 : 153 – 158 . doi: 10.1017/s001216229900033x. [DOI] [PubMed] [Google Scholar]
- 2. Molloy CA , Murray DS , Kinsman A , et al. Differences in the clinical presentation of Trisomy 21 with and without autism . J Intellect Disabil Res . 2009 ; 53 : 143 – 151 . doi: 10.1111/j.1365-2788.2008.01138.x. [DOI] [PubMed] [Google Scholar]
- 3. Lowenthal R , Paula CS , Schwartzman JS , Brunoni D , Mercadante MT . Prevalence of pervasive developmental disorder in Down’s syndrome . J Autism Dev Disord . 2007 ; 37 : 1394 – 1395 . doi: 10.1007/s10803-007-0374-4. [DOI] [PubMed] [Google Scholar]
- 4. DiGuiseppi C , Hepburn S , Davis JM , et al. Screening for autism spectrum disorders in children with Down syndrome: population prevalence and screening test characteristics . J Dev Behav Pediatr . 2010 ; 31 : 181 – 191 . doi: 10.1097/DBP.0b013e3181d5aa6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carr J . Long-term-outcome for people with Down’s syndrome . J Child Psychol Psychiatry . 1994 ; 35 : 425 – 439 . doi: 10.1111/j.1469-7610.1994.tb01732.x. [DOI] [PubMed] [Google Scholar]
- 6. Harris S , Kasari C , Sigman MD . Joint attention and language gains in children with Down syndrome . Am J Ment Retard . 1996 ; 100 : 608 – 619 . [PubMed] [Google Scholar]
- 7. Gibbs MV , Thorpe JG . Personality stereotype of noninstitutionalized Down syndrome children . Am J Ment Defic . 1983 ; 87 : 601 – 605 . [PubMed] [Google Scholar]
- 8. Sinson JC , Wetherick NE . Mutual gaze in pre-school Down’s and normal children . J Ment Defic Res . 1982 ; 26 : 123 – 129 . doi: 10.1111/j.1365-2788.1982.tb00138.x. [DOI] [PubMed] [Google Scholar]
- 9. Wishart JG . Learning difficulties in infants with Down’s syndrome . Int J Rehabil Res . 1991 ; 14 : 251 – 255 . doi: 10.1097/00004356-199109000-00011. [DOI] [PubMed] [Google Scholar]
- 10. Prasher VP , Day S . Brief report: obsessive-compulsive disorder in adults with Down’s syndrome . J Autism Dev Disord . 1995 ; 25 : 453 – 458 . doi: 10.1007/BF02179379. [DOI] [PubMed] [Google Scholar]
- 11. Carter JC , Capone GT , Gray RM , Cox CS , Kaufmann WE . Autistic-spectrum disorders in Down syndrome: further delineation and distinction from other behavioral abnormalities . Am J Med Genet B Neuropsychiatr Genet . 2007 ; 144B : 87 – 94 . doi: 10.1002/ajmg.b.30407. [DOI] [PubMed] [Google Scholar]
- 12. Howlin P , Wing L , Gould J . The recognition of autism in children with Down syndrome--implications for intervention and some speculations about pathology . Dev Med Child Neurol . 1995 ; 37 : 406 – 414 . doi: 10.1111/j.1469-8749.1995.tb12024.x. [DOI] [PubMed] [Google Scholar]
- 13. Rasmussen P , Börjesson O , Wentz E , Gillberg C . Autistic disorders in Down syndrome: background factors and clinical correlates . Dev Med Child Neurol . 2001 ; 43 : 750 – 754 . doi: 10.1017/s0012162201001372. [DOI] [PubMed] [Google Scholar]
- 14. Eisermann MM , DeLaRaillère A , Dellatolas G , et al. Infantile spasms in Down syndrome--effects of delayed anticonvulsive treatment . Epilepsy Res . 2003 ; 55 : 21 – 27 . doi: 10.1016/s0920-1211(03)00088-3. [DOI] [PubMed] [Google Scholar]
- 15. Goldberg-Stern H , Strawsburg RH , Patterson B , et al. Seizure frequency and characteristics in children with Down syndrome . Brain Dev . 2001 ; 23 : 375 – 378 . doi: 10.1016/s0387-7604(01)00239-x. [DOI] [PubMed] [Google Scholar]
- 16. Reilly C . Autism spectrum disorders in Down syndrome: A review . Research in Autism Spectrum Disorders . 2009 ; 3 : 829 – 839 . [Google Scholar]
- 17. Carter JC , Capone GT , Kaufmann WE . Neuroanatomic correlates of autism and stereotypy in children with Down syndrome . Neuroreport . 2008 ; 19 : 653 – 656 . doi: 10.1097/WNR.0b013e3282faa8d8. [DOI] [PubMed] [Google Scholar]
- 18. Boso M , Emanuele E , Prestori F , Politi P , Barale F , D’Angelo E . Autism and genius: is there a link? The involvement of central brain loops and hypotheses for functional testing . Funct Neurol . 2010 ; 25 : 15 – 20 . [PubMed] [Google Scholar]
- 19. Ghaziuddin M . Autism in Down’s syndrome: a family history study . J Intellect Disabil Res . 2000 ; 44 : 562 – 566 . doi: 10.1046/j.1365-2788.2000.00271.x. [DOI] [PubMed] [Google Scholar]
- 20. Liss M , Harel B , Fein D , et al. Predictors and correlates of adaptive functioning in children with developmental disorders . J Autism Dev Disord . 2001 ; 31 : 219 – 230 . doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- 21. Kraijer D . Review of adaptive behavior studies in mentally retarded persons with autism/pervasive developmental disorder . J Autism Dev Disord . 2000 ; 30 : 39 – 47 . doi: 10.1023/a:1005460027636. [DOI] [PubMed] [Google Scholar]
- 22. Volkmar FR , Carter A , Sparrow SS , Cicchetti DV . Quantifying social development in autism . J Am Acad Child Adolesc Psychiatry . 1993 ; 32 : 627 – 632 . doi: 10.1097/00004583-199305000-00020. [DOI] [PubMed] [Google Scholar]
- 23. Stone WL , Ousley OY , Hepburn SL , Hogan KL , Brown CS . Patterns of adaptive behavior in very young children with autism . Am J Ment Retard . 1999 ; 104 : 187 – 199 . doi: 10.1352/0895-8017(1999)104<0187:POABIV>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24. Freeman BJ , Del’Homme M , Guthrie D , Zhang F . Vineland Adaptive Behavior Scale scores as a function of age and initial IQ in 210 autistic children . J Autism Dev Disord . 1999 ; 29 : 379 – 384 . doi: 10.1023/a:1023078827457. [DOI] [PubMed] [Google Scholar]
- 25. Rodrigue JR , Morgan SB , Geffken GR . A comparative evaluation of adaptive behavior in children and adolescents with autism, Down syndrome, and normal development . J Autism Dev Disord . 1991 ; 21 : 187 – 196 . doi: 10.1007/BF02284759. [DOI] [PubMed] [Google Scholar]
- 26. Loveland KA , Kelley ML . Development of adaptive behavior in preschoolers with autism or Down syndrome . Am J Ment Retard . 1991 ; 96 : 13 – 20 . [PubMed] [Google Scholar]
- 27. Dykens EM , Hodapp RM , Evans DW . Profiles and development of adaptive behavior in children with Down syndrome . Am J Ment Retard . 1994 ; 98 : 580 – 587 . [PubMed] [Google Scholar]
- 28. Rellini E , Tortolani D , Trillo S , Carbone S , Montecchi F . Childhood Autism Rating Scale (CARS) and Autism Behavior Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism . J Autism Dev Disord . 2004 ; 34 : 703 – 708 . doi: 10.1007/s10803-004-5290-2. [DOI] [PubMed] [Google Scholar]
- 29. Sparrow SS , Balla DA , Cicchetti DV , et al. In: Vineland adaptive behavior scales intervista, forma completa, manuale, adattamento italiano . Balboni G , Pedrabissi L , editors. Florence : Os ; 2003 . [Google Scholar]
- 30. Schopler E , Reichler RJ , DeVellis RF , Daly K . Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS) . J Autism Dev Disord . 1980 ; 10 : 91 – 103 . doi: 10.1007/BF02408436. [DOI] [PubMed] [Google Scholar]
- 31. Capone GT , Grados MA , Kaufmann WE , Bernad-Ripoll S , Jewell A . Down syndrome and comorbid autism-spectrum disorder: characterization using the aberrant behavior checklist . Am J Med Genet A . 2005 ; 134 : 373 – 380 . doi: 10.1002/ajmg.a.30622. [DOI] [PubMed] [Google Scholar]
- 32. Greenspan SI , Brazelton TB , Cordero J , et al. Guidelines for early identification, screening, and clinical management of children with autism spectrum disorders . Pediatrics . 2008 ; 121 : 828 – 830 . doi: 10.1542/peds.2007-3833. [DOI] [PubMed] [Google Scholar]
- 33. Castillo H , Patterson B , Hickey F , et al. Difference in age at regression in children with autism with and without Down syndrome . J Dev Behav Pediatr . 2008 ; 29 : 89 – 93 . doi: 10.1097/DBP.0b013e318165c78d. [DOI] [PubMed] [Google Scholar]
- 34. Rigoldi C , Galli M , Condoluci C , Carducci F , Onorati P , Albertini G . Gait analysis and cerebral volumes in Down’s syndrome . Funct Neurol . 2009 ; 24 : 147 – 152 . [PubMed] [Google Scholar]
- 35. Saemundsen E , Ludvigsson P , Rafnsson V . Risk of autism spectrum disorders after infantile spasms: a population-based study nested in a cohort with seizures in the first year of life . Epilepsia . 2008 ; 49 : 1865 – 1870 . doi: 10.1111/j.1528-1167.2008.01688.x. [DOI] [PubMed] [Google Scholar]
- 36. Creavin AL , Brown RD . Ophthalmic abnormalities in children with Down syndrome . J Pediatr Ophthalmol Strabismus . 2009 ; 46 : 76 – 82 . doi: 10.3928/01913913-20090301-06. [DOI] [PubMed] [Google Scholar]
- 37. Pensiero S , Fabbro F , Michieletto P , Accardo A , Brambilla P . Saccadic characteristics in autistic children . Funct Neurol . 2009 ; 24 : 153 – 158 . [PubMed] [Google Scholar]
- 38. Dressler A , Perelli V , Feucht M , Bargagna S . Adaptive behaviour in Down syndrome: a cross-sectional study from childhood to adulthood . Wien Klin Wochenschr . 2010 ; 122 : 673 – 680 . doi: 10.1007/s00508-010-1504-0. [DOI] [PubMed] [Google Scholar]
- 39. Capone GT , Goyal P , Grados M , Smith B , Kammann H . Risperidone use in children with Down syndrome, severe intellectual disability, and comorbid autistic spectrum disorders: a naturalistic study . J Dev Behav Pediatr . 2008 ; 29 : 106 – 116 . doi: 10.1097/DBP.0b013e318165c100. [DOI] [PubMed] [Google Scholar]
- 40. Dierssen M , Ramakers GJ . Dendritic pathology in mental retardation: from molecular genetics to neurobiology . Genes Brain Behav . 2006 ; 5 ( Suppl 2 ): 48 – 60 . doi: 10.1111/j.1601-183X.2006.00224.x. [DOI] [PubMed] [Google Scholar]
- 41. Geschwind DH , Levitt P . Autism spectrum disorders: developmental disconnection syndromes . Curr Opin Neurobiol . 2007 ; 17 : 103 – 111 . doi: 10.1016/j.conb.2007.01.009. [DOI] [PubMed] [Google Scholar]